Abstract
Nodular fasciitis (NF) is an uncommon and benign tumour-like fibroblastic proliferation that is difficult to distinguish from sarcoma both clinically and histologically. In addition, it is a type of lesion characterised by having a potential for spontaneous regression. NF is frequently misdiagnosed due to its rapid growth, rich cellularity, and mitotic figure. Although NF is only rarely diagnosed in children, the head and neck represent the most common locations for NF among this population. The cause of NF remains unknown, however trauma is believed to be an important triggering factor. We describe an unusual case of NF in the posterior ethmoid sinus in a six-year-old boy with no history of trauma. The NF was incidentally noted on a computed tomography scan after the patient complained of a squint. The diagnosis of NF was also supported by histopathology and specific immunohistological staining. A surgical biopsy was performed, and no recurrence was observed after one year.
Keywords: Nodular fasciitis, maxillary sinus, histopathology, endoscopy
ÖZ
Nodüler fasiit (NF), klinik ve histolojik olarak sarkomdan ayırt edilmesi zor olan, nadir görülen ve iyi huylu tümör benzeri bir fibroblastik proliferasyondur. Ayrıca, kendiliğinden gerileme potansiyeli olan bir lezyon türüdür. NF hızlı büyümesi, zengin hücreselliği ve mitotik biçimi nedeniyle sıklıkla yanlış teşhis edilmektedir. Çocuklarda nadiren teşhis edilmekle beraber, baş ve boyun bölgesi bu popülasyonda en yaygın NF konumunu temsil etmektedir. Travmanın önemli bir tetikleyici etken olduğuna inanılmasına rağmen, NF’nin nedeni bilinmemektedir. Travma öyküsü olmayan altı yaşında bir çocukta posterior etmoid sinüste nadir görülen bir NF vakası tanımlanmıştır. Hasta şaşılıktan şikâyet ettikten sonra bilgisayarlı tomografi taramasında NF tesadüfen kaydedilmiştir. NF tanısı histopatoloji ve spesifik immünohistolojik boyama ile de desteklenmiştir. Cerrahi biyopsi yapılmıştır ve bir yıl sonra nüks gözlenmemiştir.
Keywords: Nodüler fasiit, maksiller sinüs, histopatoloji, endoskopi
Introduction
Nodular fasciitis (NF) is a rarely seen benign tumour. More specifically, it is a fibroblastic proliferation of subcutaneous tissue that mimics sarcoma due to its aggressive features1. However, unlike sarcoma, spontaneous regression is possible in NF. NF was initially described in 1955, when it was identified as subcutaneous pseudosarcomatous fibromatosis2, however the nomenclature was changed to NF during the 1960s3.
Most cases of NF were diagnosed in young and middle-aged adults between 20 to 40 years of age. Neither sex nor race has been noted to impact the incidence of NF3. NF accounts for 0.025% of all pathologic cases4. Only approximately 4 to 10 % of NF lesions occur in children with boys being more commonly affected5, 6. The exact etiology of NF remains unknown, although it is believed to be triggered by an antecedent trauma or by a localised nonspecific inflammatory process7.
Two cases of NF originating in the maxillary sinus have been previously reported in a two-year-old boy and an adult lady in Saudi Arabia and India, respectively7,8. The posterior ethmoid sinus has not been previously reported as the origin of NF.
Case Report
A six-year-old boy initially presented to the ophthalmologist with a squint in the left eye, which was associated with facial asymmetry. The patient had the squint since the age of two. A computed tomography (CT) scan of the patient’s brain and orbit revealed non-enhancing soft-tissue density arising from the left posterior ethmoid sinus that breached the lamina papyracea (Figure 1a) and extended into the maxillary infundibulum (Figure 1b). The left fovea ethmoidalis was also eroded. The left orbital rim was slightly smaller when compared with the right one. There were no neck swelling, nasal symptoms, eye symptoms, constitutional symptoms or fever. Further, the patient had not experienced any preceding trauma or previously undergone an operation. Upon examination, the ranges of movement of the left eye toward the upper outer gaze were found to be reduced. No neck node was detected.
Figure 1.
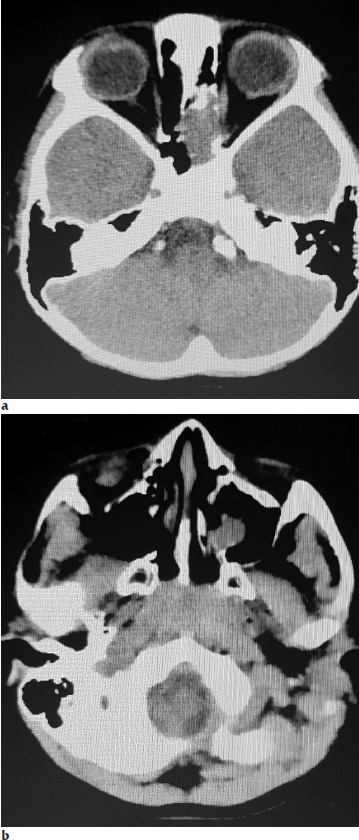
(a) A CT scan axial cut soft tissue setting showing the non-enhancing soft-tissue density from the left posterior ethmoid sinus breached the lamina papyracea. (b) The mass extended downward into the maxillary infundibulum.
The patient was subsequently referred for a nasoendoscopy, during which a bulging over the lateral wall of the left middle meatus, posterior to the uncinate process with a non-pulsatile prominent vessel was noted. Both fossae of Rosenmüller were normal.
The patient underwent an endoscopic biopsy. A whitish, friable, and non-vascularised mass was found to be bulging from the posterior ethmoid air cells. The parts of the mass attached to the lamina papyracea and the skull base were left undisturbed.
A microscopic examination of the specimen identified tumour tissue composed of spindle cells with variable cellularity that was embedded within a fibromyxoid stroma. The cells were arranged in storiform, C- and S-shaped patterns (Figure 2). They had plump stellate (ovoid) vesicular nuclei with visible nucleoli. Mitotic figures were only rarely seen (Figure 3). Blood vessels in different sizes characterised by perivascular hyalinization with scattered lymphocytes, eosinophils, and multinucleated giant cells were also identified (Figure 2). The immunohistochemical staining with vimentin and smooth muscle actin (SMA) revealed positive results, while the staining with S100, desmin, h-caldesmon, CD34, and CK revealed negative results. The Ki-67 proliferative index was absent (0-1%). A pathological diagnosis of NF was made. The patient was placed on regular follow-up for almost one year, no evidence of recurrence was seen clinically during this time. We planned to repeat CT scan of the paranasal sinus at postoperatively first year.
Figure 2.
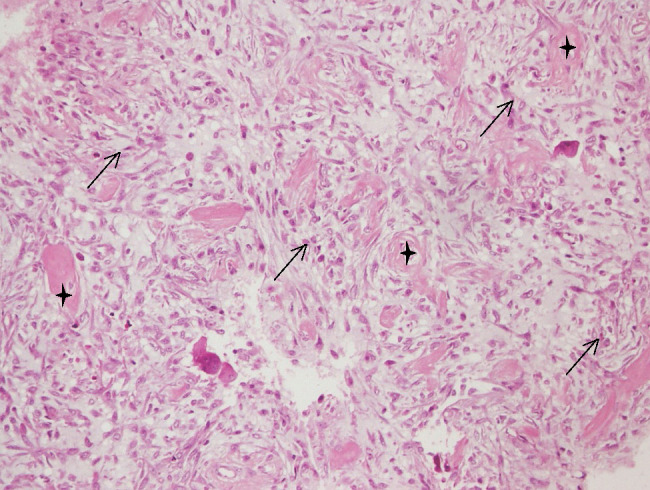
(H&E, x200) Spindle cells (→) arranged in storiform, C and S shaped embedded within a fibromyxoid stroma. Perivascular hyalinization (*) with scattered lymphocytes, eosinophils and multinucleated giant cells.
Figure 3.
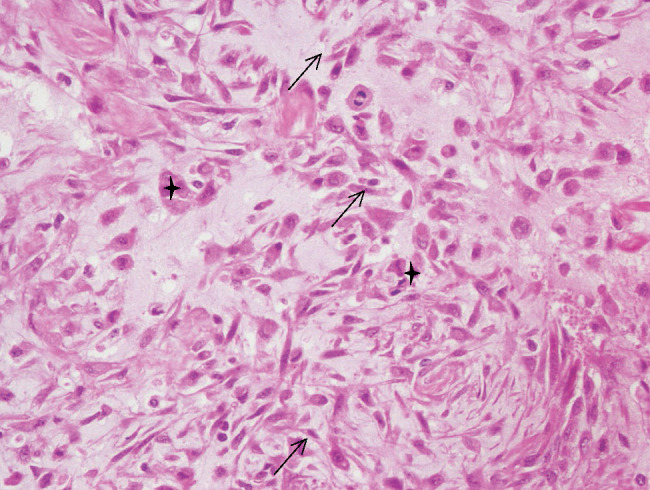
(H&E, x400) Spindle cells (→) are shown more clear. Slightly mitotic figures were seen (*).
Discussion
NF is the result of a benign reactive process. The lesions are frequently misdiagnosed as malignant lesions due to their rapid growth. Additionally, the abundant cellular and mitotic activities of NF have been shown histologically. The nonspecific clinical presentation of NF as well as the variations in the associated histological findings lead to its misdiagnosis1.
NF can also be referred to as pseudosarcomatous fasciitis, pseudosarcomatous fibromatosis, proliferative fasciitis, infiltrative fasciitis, productive fasciitis or subcutaneous fibromatosis9. Moreover, NF can be divided into three subtypes based on its relationship with the fascia, namely the subcutaneous, intramuscular, and fascial types7.
NF has been found to occur in all age groups; however, it is rarely seen in the pediatric population. No specific gender distribution has been noted in relation to NF in general, although it is more commonly seen in boys5,6. NF can occur anywhere in the body, but it is most frequently seen in the upper extremities (48%), particularly in the volar aspect of the forearm. NF is also typically found in the trunk (20%), head and neck (15-20%), and lower extremities (15%)8. The head and neck represent the most common locations for NF in infants and children. Among the cases of NF reported in children younger than 18 years old between 2010 and 2012, three out of five patients were males who had NF in the upper extremities1. From a total of 28 cases of NF reported in the head and neck regions of children, 14 were located over the skull, six at the mandible, three over the neck, two at the cheek, and one for each on the parotid gland, submandibular gland, and nose, with no lesions being reported over the forehead or paranasal sinus5.
The pathophysiology of NF is not yet fully understood, although it is believed to stem from a reactive process triggered in response to an injury or inflammatory process. Furthermore, its histological characteristics bear a close resemblance to those of granulation tissue8. In addition, many documented cases of NF (<15%) had a prior history of trauma. However, there was no history of trauma in this case. The two cases of maxillary sinus NF previously reported in the literature also did not have a documented history of trauma7,8. In fact, no antecedent trauma has been reported in the case series featuring pediatric NF patients1. Yet, in a study conducted in South Korea, which focused on the face, it was found that nine out of 16 patients had a history of physical stimulation or trauma such as facial massage10.
The typical clinical characteristics of NF are painless and rapidly growing lesions that result in a suspicion of malignancy. The lesions are mostly wellcircumscribed and solitary small masses, which have an average diameter of less than 3 cm2. The case of maxillary sinus NF reported in Saudi Arabia had symptoms that rapidly progressed within two months. The boy was unable to open his eye due to the mass effect8. In our case, the symptoms had been present for almost four years, and had not worsened during that time. The average duration of NF is 41 days (range: 11-100 days)1. Nearly all reported cases of NF were solitary and featured lesions less than 3 cm in diameter. Only two patients had multiple lesions, while less than 9% of 134 cases complained of pain11. Due to the nonspecific clinical presentation of NF, an accurate histopathologic diagnosis is crucial, since a misdiagnosis may lead to aggressive and unnecessary treatment.
NF lesions share certain common features. They are composed of spindle-shaped fibroblasts with myxoid tissue and a vascular component featuring a minimal number of mononuclear cells and occasional multinucleated giant cells. The nuclei are hyperchromatic, vary in size, and frequently exhibit normal mitotic activity11. The cells are arranged in a storiform (cartwheel) growth pattern12.
The immunohistological profile of NF is consistent3. Immunohistochemistry relies on the principle of antibodies specifically binding to certain antigens within biological tissues in order to detect those antigens in the cells of a tissue section. Myofibroblasts are reactive to vimentin, SMA, and CD68 (a histiocytic marker). Desmin and hcaldesmon are used to differentiate between the leiomyoma and leiomyosarcoma types, whereas CD34 is used to distinguish NF from dermatofibrosarcoma. In relation to the diagnosis and prognosis, the Ki-67 index is useful in determination of soft tissue sarcoma10. Moreover, S100 is specific for melanoma.
Prior cases of periorbital NF and maxillary sinus NF revealed well-defined and circumscribed tumours8,13. To date, no study has documented either bony erosion or invasive growth. However, there was erosion into the fovea ethmoidalis and lamina papyracea in our case.
Surgical excision represents the standard treatment for NF, although there are other treatment modalities available, including steroid injection, laser therapy, adjuvant chemotherapy, and postoperative radiotherapy. We proceeded with an endoscopic biopsy, leaving a remnant behind in certain places due to the likelihood of intraoperative complications. A case of NF within the zygoma was noted to have undergone spontaneous regression following an incisional biopsy14. For cases of facial NF, non-surgical treatments are preferred; for example, intralesional triamcinolone injection and laser therapy, due to the risk of insufficient excision stemming from the desire to reduce scarring over the face, which may act as a precipitating factor for a new NF lesion due to myofibroblast proliferation10. There have been cases of facial NF with spontaneous regression11.
In relation to NF, the rate of recurrence following a surgery is incredibly low (0.4-1%)3. Indeed, in four out of five postoperative patients, no recurrence was documented1. Our patient clinically experienced no recurrence after almost one year of follow-up. A repeat paranasal sinus CT scan was planned postoperatively after one year to review the size of mass.
Conclusion
NF is a rare disease in the paranasal sinus, although it can be included in the differential diagnosis of a nasal mass. Appropriate examination and investigation are very important in order to make a correct diagnosis and prevent the patient from an unnecessary treatment. Aside from surgical excision, other treatment options do exist for NF, including laser therapy, steroid injection, and observation.
References
- 1.Pandian TK, Zeidan MM, Ibrahim KA, Moir CR, Ishitani MB, Zarroug AE. Nodular fasciitis in the pediatric population: a single center experience. J Pediatr Surg. 2013;48:1486–9. doi: 10.1016/j.jpedsurg.2012.12.041. [DOI] [PubMed] [Google Scholar]
- 2.Konwaler BE, Keasbey L, Kaplan L. Subcutaneous pseudosarcomatous fibromatosis (fasciitis). Am J Clin Pathol. 1955;25:241–52. doi: 10.1093/ajcp/25.3.241. [DOI] [PubMed] [Google Scholar]
- 3.Mullin D, Lindsay FW, Keefe MA. Nodular fasciitis of the nasal cavity: a case report. Ear Nose Throat J. 2007;86:74851. [PubMed] [Google Scholar]
- 4.Haddad AJ, Avon SL, Clokie CM, Sandor GK. Nodular fasciitis in the oral cavity. J Can Dent Assoc. 2001;67:664–7. [Google Scholar]
- 5.Carr MM, Fraser RB, Clarke KD. Nodular fasciitis in the parotid region of a child. Head Neck. 1998;20:645–8. doi: 10.1002/(sici)1097-0347(199810)20:7<645::aid-hed12>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 6.Zuber TJ, Finley JL. Nodular fasciitis. South Med J. 1994;87:842–4. doi: 10.1097/00007611-199408000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Chaithanyaa N, Somannavar P, Annajal NA. Nodular fasciitis over the anterior wall of the maxillary sinus: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e10–e5. doi: 10.1016/j.oooo.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Alsaied AS, Lotfy MA. Maxillary sinus nodular fasciitis. Saudi Med J. 2014;35:88–92. [PubMed] [Google Scholar]
- 9.Vyas T, Bullock MJ, Hart RD, Trites JR, Taylor SM. Nodular fasciitis of the zygoma: A case report. Can J Plast Surg. 2008;16:241–3. doi: 10.1177/229255030801600405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oh BH, Kim J, Zheng Z, Roh MR, Chung KY. Treatment of Nodular Fasciitis Occurring on the Face. Ann Dermatol. 2015;27:694–701. doi: 10.5021/ad.2015.27.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49:1668–78. doi: 10.1002/1097-0142(19820415)49:8<1668::aid-cncr2820490823>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 12.Thompson LD. Nodular fasciitis. Ear Nose Throat J. 2002;81:830. [PubMed] [Google Scholar]
- 13.Ruoppi P, Vornanen M, Nuutinen J. A rapidly progressing periorbital mass in an infant: fasciitis nodularis. Acta Otolaryngol. 2004;124:324–7. doi: 10.1080/00016480310015678. [DOI] [PubMed] [Google Scholar]
- 14.Yanagisawa A, Okada H. Nodular fasciitis with degeneration and regression. J Craniofac Surg. 2008;19:1167–70. doi: 10.1097/SCS.0b013e318176ac1a. [DOI] [PubMed] [Google Scholar]


