Highlights
-
•
Full-length SARS-CoV-2 prefusion spike with Matrix-M™ (NVX-CoV2373) vaccine.
-
•
Induced hACE2 receptor blocking and neutralizing antibodies in macaques.
-
•
Vaccine protected against SARS-CoV-2 replication in the nose and lungs.
-
•
Absence of pulmonary pathology in NVX-CoV2373 vaccinated macaques.
Keywords: SARS-CoV-2, COVID-19, Spike glycoprotein, NVX-CoV2373 nanoparticles, Matrix-M adjuvant, Nonhuman primate
Abstract
There is an urgent need for a safe and protective vaccine to control the global spread of SARS-CoV-2 and prevent COVID-19. Here, we report the immunogenicity and protective efficacy of a SARS-CoV-2 subunit vaccine (NVX-CoV2373) produced from the full-length SARS-CoV-2 spike (S) glycoprotein stabilized in the prefusion conformation. Cynomolgus macaques (Macaca fascicularis) immunized with NVX-CoV2373 and the saponin-based Matrix-M™ adjuvant induced anti-S antibody that was neutralizing and blocked binding to the human angiotensin-converting enzyme 2 (hACE2) receptor. Following intranasal and intratracheal challenge with SARS-CoV-2, immunized macaques were protected against upper and lower infection and pulmonary disease. These results support ongoing phase 1/2 clinical studies of the safety and immunogenicity of NVX-CoV2327 vaccine (NCT04368988).
1. Introduction
There is an urgent need for a safe and effective severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine to prevent coronavirus disease 2019 (COVID-19). We have developed a recombinant nanoparticle vaccine constructed from the full–length, wild-type SARS–CoV-2 spike glycoprotein (GenBank gene sequence MN908947, nucleotides 21563–25384) optimized for the baculovirus-Spodoptera frugiperda (Sf9) insect cell expression system [1]. In mice and nonhuman primates (NHP), NVX-CoV2373 with a Matrix-M saponin-based adjuvant induced high titer anti-spike IgG that blocks binding to the hACE2 receptor, neutralize wild type virus, and protects mice against SARS-CoV-2 challenge with no evidence of vaccine-associated enhanced respiratory disease. NVX-CoV2373 vaccine also induces multifunctional CD4+ T-cell responses of IFN-γ, IL-2, and TNF-α biased towards a Th1 phenotype, and generates antigen-specific germinal center B cells in the spleen [1]. Safety and immunogenicity NVX-CoV2327 vaccine is currently under evaluation in humans (NCT04368988) and primary safety and immunogenicity outcomes described [2]. We evaluate in the current study NVX-CoV2373 vaccine immunogenicity, induction of receptor blocking, and neutralizing antibodies compared to levels in human COVID-19 convalescent sera. And in a nonhuman primate challenge model, protection against upper and lower virus replication and pulmonary disease.
2. Materials and methods
2.1. Cell lines, virus, antibody reagents, and receptors
Vero E6 cells (ATCC, CRL-1586) were maintained in Minimal Eagles Medium (MEM) supplemented with 10% fetal bovine serum, 1% glutamine and 1% penicillin and streptomycin. The SARS-CoV-2 (WA-1, 2020) isolated was obtained from the Center for Disease Control and stock virus prepared in Vero E6 cells. Histidine-tagged hACE2 receptor was purchased from Sino Biologics (Beijing, CN). Rabbit anti-SARS-CoV spike protein was purchased form Biodefense and Emerging Infections Research Resources Repository (BEI Resources, Manassas, VA).
2.2. Recombinant SARS-CoV-2 spike protein
NVX-CoV2327 was codon optimized synthetically produced from the full-length S glycoprotein gene sequence (GenBank MN908947 nucleotides 21563–25384) for expression in Spodoptera frugiperda (Sf9) cells (GenScript Piscataway, NJ, USA) as described [1]. Briefly, the S1/S2 furin cleavage site 682-RRAR-685 was modified 682-QQAQ-685 and two proline substitutions introduced at positions K986P and V987P (2P) to stabilize the full-length SARS-CoV-2 S [3].
2.3. Animal ethics
The in-life portion of the study was conducted at BIOQUAL, Inc (Rockville, MD). Female and male, > 3 years old at study initiation, cynomolgus macaques (Macaca fascicularis) were obtained from Primgen, Inc (Hines, IL) and maintained at BIOQUAL, Inc for the entire in-life portion of the study. BIOQUAL, Inc. is accredited by AAALACC International. Animals were maintained and treated according to the Institutional Biosafety Committee guidelines and the study was pre-approved by the Institutional Animal Care and Use Committee (IACUC). The study was conducted in accordance with the National Institutes of Health Guide for Care and Use of Laboratory Animals (NIH publication 8023, Revised 1978).
2.4. Cynomolgus macaque immunization
Antigen and adjuvant dose levels were selected based upon our prior experience in baboons and humans immunized with NVX-CoV2373 (5 μg or 50 μg) with and without Matrix-M (50 μg). In both studies, functional hACE2 receptor blocking antibodies, virus neutralizing titers, and antigen-specific CD8 and CD4 T cells were increased in animals receiving the adjuvanted vaccine compared to immunization with the antigen alone [1], [2]. In this study, cynomolgus macaques > 3 years old (n = 4/group) at study initiation received 5 or 25 μg NVX-CoV2327 with 50 μg Matrix-M (Novavax AB, Uppsala, Sweden) administered in 500 μL in the thigh muscle in two doses spaced 21 days apart. A separate group was immunized with a fractional dose (2.5 μg) NVX-CoV2373 with 25 μg Matrix-M in two doses spaced 21 days apart and a placebo group received formulation buffer. Serum was collected before immunization on day 0, day 21 just prior to the second immunization, and day 33.
2.4.1. Anti-spike (S) IgG ELISA
Anti-SARS-CoV-2 spike (S) protein IgG ELISA titers were measured as described [1]. Briefly, 96-well microtiter plates (ThermoFischer Scientific, Rochester, NY, USA) were coated with 1.0 µg/mL of SARS-CoV-2 rS protein. Plates were washed with phosphate buffer and tween (PBS-T) and nonspecific binding was blocked with TBS Startblock blocking buffer (ThermoFisher, Scientific). Serum samples were serially diluted 3-fold down starting with a 1:100 dilution (ie, 10-2 to 10-8) and added to the coated plates at room temperature for 2 h. Following incubation, plates were washed with PBS-T and HRP-conjugated mouse anti-monkey IgG (Southern Biotech, Birmingham, AL, USA) was added for 1 h. Plates were washed with PBS-T and 3,3′,5,5′-tetramethylbenzidine (TMB) peroxidase substrate (Sigma, St Louis, MO, USA) was added. Reactions were stopped with TMB stop solution (ScyTek Laboratories, Inc. Logan, UT). Plates were read at OD 450 nm with a SpectraMax Plus plate reader (Molecular Devices, Sunnyvale, CA, USA). Anti-S IgG EC50 titers were calculated by 4-parameter fitting using SoftMax Pro 6.5.1 GxP software. Individual animal anti-S IgG EC50 titers, group geometric mean titers (GMT) were plotted using GraphPad Prism 7.05 software.
2.5. Inhibition of hACE2 receptor binding and neutralization
Antibodies that block binding of hACE2 receptor to the S-protein and neutralize in a cytopathic effect assay (CPE) in Vero E6 cells were measured as described previously as the serum titer that blocks 100% CPE [1]. Serum antibody titer at 50% binding inhibition (IC50) of hACE2 to SARS-CoV-2 S protein was determined in the SoftMax Pro program. Individual animal hACE2 receptor inhibiting titers, mean titers, and SEM were plotted using GraphPad Prism 7.05 software. Neutralizing antibody titers were determined as the dilution of serum that inhibited 100% of CPE (CPE100) at 3 days post infection of Vero E6 cells in a 96 well plate format.
2.6. SARS-CoV-2 challenge procedure
The virus challenge study was done at BIOQUAL, Inc. within a BSL-3 containment facility. SARS-CoV-2 generated from isolate 2019-nCoV/USA-WA1/2020 was received from BEI Resources (NR-52281; lot # 70033175) and expanded in Vero E6 cells for challenge stock generation. Animals were sedated and challenged with a targeted total dose of 1.1 × 104 pfu SARS-CoV-2 by intranasal (IN) and intratracheal (IT) in a volume of 0.25 mL each route. BAL and nasal swabs were collected 2- and 4-days post challenge. Necropsy was performed 7 days following challenge and lung tissues collected for histopathology.
2.7. RNA subgenomic RT-PCR
The subgenomic viral mRNA (sgRNA) was measured in macaque bronchoalveolar lavage (BAL) and nasal swabs collected 2- and 4-days post challenge using RT-PCR as described [4]. To generate a standard curve, the SARS-CoV-2 E gene sgRNA was cloned into a pcDNA3.1 expression plasmid. The insert was transcribed using an AmpliCap-Max T7 High Yield Message Maker Kit (Cellscript, Madison, WI) to obtain RNA for standards. Prior to RT-PCR, samples collected from challenged animals or standards were reverse-transcribed using Superscript III VILO (Invitrogen) according to the manufacturer’s instructions. A Taqman custom gene expression assay (ThermoFisher Scientific, Rockville, MD) was designed using the sequences targeting the E gene sgRNA. Reactions were carried out on a Quant Studio 6 and 7 Flex Real-Time PCR System (Applied Biosystems, Foster City, CA) according to the manufacturer’s specifications. Standard curves were used to calculate sgRNA in copies per mL. The quantitative assay was sensitive to 50 copies per mL.
2.8. Histopathology
Animals were euthanized 7-days following SARS-CoV-2 challenge (Day 42) and lung tissues collected. Tissue were prepared for histologic examination by Experimental Pathology Laboratories, Inc. (EPL, Sterling, VA). The lungs were fixed with 10% formalin, paraffin embedded, and sections stained with hematoxylin and eosin (H&E) for histological examination. Slides were examined for total inflammation, periarteriolar, and peribronchiolar inflammation and epithelial cell denuding.
2.9. Human COVID-19 convalescent serum
Convalescent serum samples (n = 32) were provided by Dr. Pedro A Piedra (Baylor College of Medicine, Houston, TX, USA). Samples were collected from COVID-19 individuals 18–79 years of age 4–6 weeks after testing positive for SARS CoV-2. Symptoms ranged from asymptomatic, mild to moderate symptoms, to severe symptoms requiring hospitalization. Sera were analyzed for anti-SARS-CoV-2 S IgG, hACE2 receptor inhibition, and virus neutralizing antibody titers.
3. Results
3.1. Immunogenicity of NVX-CoV2373 in nonhuman primates compared to COVID-19 convalescent human sera
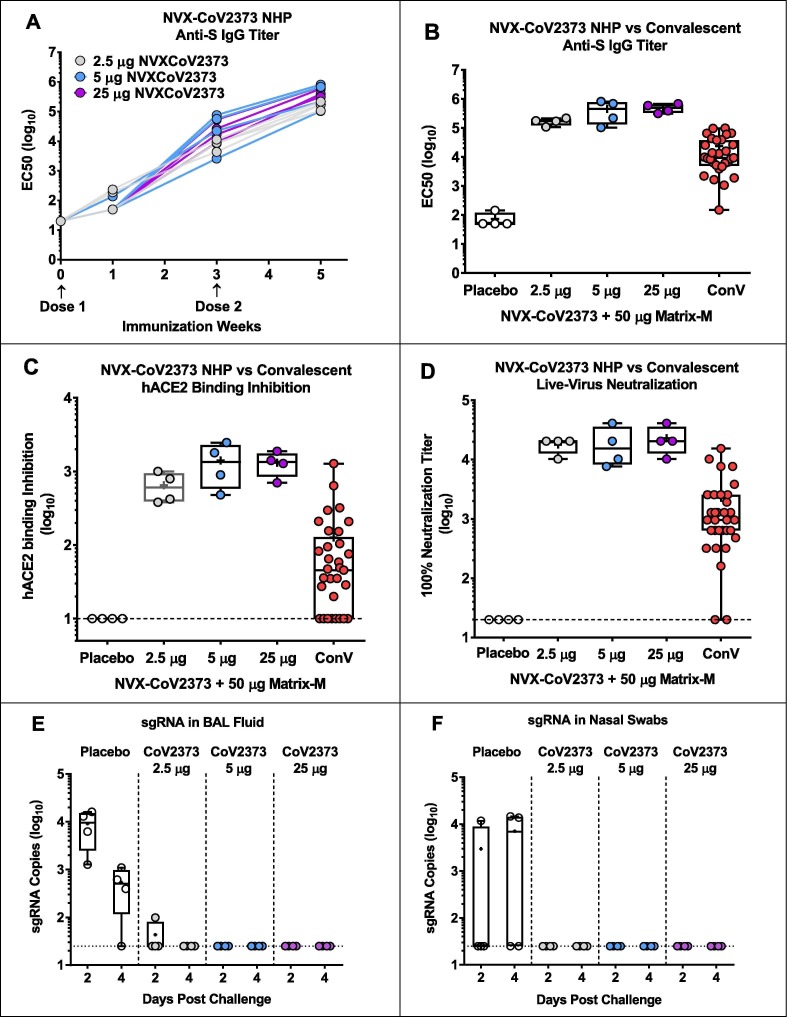
Macaques immunized with the prime/boost regimen of 2.5, 5, and 25 μg NVX-CoV2373 with 25 μg in the low and 50 μg Matrix-M adjuvant in the two higher doses induced anti-S IgG (EC50) antibodies at Day 21 after a single dose (GMT = 7,810, 22,386 and 21,472, respectively). Two weeks following a booster immunization, anti-S IgG EC50 titers increased to GMT EC50 = 163,036, 335,017 and 469,739, respectively (Fig. 1 A). In contrast, SARS-CoV-2 anti-S antibody in convalescent human sera was 6.9- to 14.2-fold less with at GMT EC50 of 23,614 (Fig. 1 B). And, hACE2 receptor inhibition titers of 649, 1,410, and 1,320 in 2.5, 5, and 25 µg NVX-CoV2373 dose groups respectively were 5.2 – 11.2-fold higher than in convalescent sera (Fig. 1 C). Finally, SARS-CoV-2 GMT neutralization antibody titers of 17,920–23,040 CPE100 in immunized macaques, were 7.9 – 10.1-fold higher than in convalescent sera (Fig. 1 D).
Fig. 1.
Immunogenicity of NVX-CoV2373 vaccine in cynomolgus macaques. (A) Groups of cynomolgus macaques (n = 4 per arm) were immunized weeks 0 and 3 with 2.5 μg NVX-CoV2373 with 25 μg Matrix-M1 or 5 μg or 25 μg NVX-CoV2373 with 50 μg Matrix-M1. Anti-spike EC50 IgG titers were measured weeks 0, 1, 3, and 5. Lines indicate anti-spike IgG titers for individual macaques in each group. (B) Anti-spike EC50 IgG serum titers week 5 in NVX-CoV2373 immunized NHP compared to anti-S EC50 IgG titers in convalescent human sera. (C) ACE2 inhibition IC50 serum titers week 5 NVX-CoV2373 immunized macaques compared to ACE2 inhibition titers in convalescent human sera, (D) Neutralization CPE100 titers against wild type SARS-CoV-2 virus week 5 NVX-CoV2373 immunized macaques compared to neutralization CPE100 titers in convalescent human sera, (E) Subgenomic RNA (sgRNA) copies in BAL fluid days 2 and 4 post challenge SARS-CoV-2 virus in placebo and NVX-CoV2373 immunized macaques. (F) sgRNA copies in nasal swab samples days 2 and 4 post challenge with SARS-CoV-2 virus in placebo and NVX-CoV2373 immunized macaques. Dashed horizontal line indicates the limit of detection (LOD). ConV: Human convalescent serum. BAL: bronchoalveolar lavage.
3.2. Viral load in nasal swabs and BAL
To evaluate the potential efficacy of NVX-CoV2373 vaccine, macaques were challenged with SARS-CoV-2 virus in upper and lower airways. Macaques in the placebo group had 9,131 sgRNA copies/mL in the BAL at 2 days post challenge and remained elevated at day 4 except for one animal. In contrast, immunized animals had no detectable sgRNA in BAL fluid other than one animal in the low dose group at day 2 which cleared replicating virus RNA by day 4 (Fig. 1 E). Half of the controls had ~ 4 log10 of virus sgRNA copies in nasal swabs and in contrast, no detectable sgRNA was in the nose of NVX-CoV2373 vaccinated animals (Fig. 1 F).
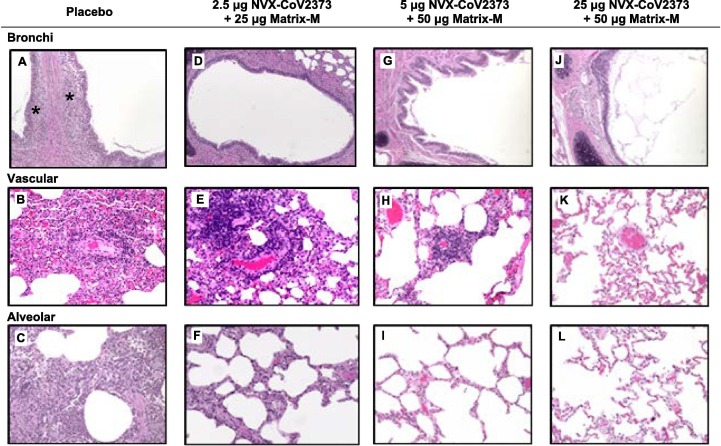
3.3. Lung pathology
Lung tissues were collected from all animals at 7 days post challenge and sections examined for pathologic changes within the upper and lower airways. Consistent with previous reports of SARS-CoV-2 infection in rhesus macaques [5], [6], [7], [8], [9], [10], [11] placebo control animals had moderate to severe inflammation that involved the mucosa of the bronchi, perivascular mononuclear infiltrate with mixed infiltrates of macrophages and neutrophils within the alveoli. In contrast, there was little, or no inflammation observed in the lungs of macaques immunized with NVX-CoV2373 vaccine 7 days post challenge (Fig. 2 ). These findings were consistent the absence of sgRNA in BAL fluids and nasal swabs of vaccinated animals by day 4 post challenge (Fig. 1 E and 1F).
Fig. 2.
Representative histopathology of lungs from NVX-CoV2373 vaccinated cynomolgus macaques challenged with SARS-CoV-2 (WA1 strain). (A, B, C) Microscopic findings in placebo treated animals includes eosinophils expanding the mucosa of bronchi (asterisks), perivascular mononuclear infiltrates, and mixed inflammation (macrophages and neutrophils) within alveoli. Three out of four animals exhibited a combination of the majority of findings. (D, E, F) Microscopic findings in the group immunized with 2.5 μg NVX-CoV2373/Matrix-M includes minimal to mild mononuclear perivascular infiltrates, and no changes in the bronchi. Rare foreign material was observed in the one male with mixed inflammation. (G, H, I) Histological findings in the group immunized with 5 μg NVX-CoV2373/Matrix-M includes minimal to mild perivascular mononuclear or mixed cell infiltrates (1/1 males and 2/3 females), mild to moderate mixed cell inflammation (1/3 females), and minimal to mild alveolar macrophages (1/1 males and 3/3 females). The female with mixed inflammation additionally observed acellular bacteria and foreign material. (J, K, L) There were no remarkable pathologic changes observed in the bronchi, vascular, or alveoli of animals vaccinated with 25 μg NVX-CoV2373/Matrix-M.
4. Discussion
Macaques have recently been shown to be permissive to infection with SARS-CoV-2 and to develop upper and lower respiratory track pathology that is similar to human infection. Using a dose range of SARS-CoV-2 (1.1 × 104 pfu to 1.1 × 106 pfu), Shan, C et al. [5] and Chandrashekar A et al. [6] show pathological changes in lungs of naïve animals develop multifocal regions of inflammation and evidence of viral pneumonia, which included expansion of alveolar septae and interstitial edema with mixed mononuclear and polymorphonuclear cell infiltrate. In addition, terminal broncholar epithelium showed evidence of necrosis and occasional bronchiolar epithelial syncytial cells. Replicating virus was also observed in oropharyngeal swabs 1 day post infection (dpi) and in BAL fluids 5–7 dpi. Based upon similarities with human infection and pathology, this model has been used to evaluate the immunogenicity of COVID-19 vaccine candidates including nucleic acid based pDNA [9] and mRNA-1273 [10], virus vector ChAdOx1nCoV-19 [8], inactivated virus PiCoVacc [7], and recombinant subunit [12] vaccines. Vaccinated macaques generally have reduced virus load in the BAL fluids and lower respiratory tract tissue and nasal swabs following challenge with SARS-CoV-2 compared to non-vaccinated animals. In animals receiving one or two doses of the ChAdOx1nCoV-19 vaccine, however, there was no difference in nasal virus shedding between vaccinated and non-vaccinated control animals [8], suggesting the model may be able to distinguish differences in vaccine efficacy.
Here, we report the immunogenicity and the protective efficacy of a prefusion, stabilized, full-length SARS-CoV-2 S vaccine (NVX-CoV2373) in the cynomolgus macaque model [11]. Prime and booster immunization with NVX-CoV2373 vaccine with Matrix M adjuvant induced high levels of anti-S IgG and antibodies that blocked SARS-CoV-2 spike protein binding to the hACE2 receptor and neutralized the virus. Importantly, vaccinated nonhuman primates had little or no detectable replicating virus (sgRNA) in either upper or lower respiratory tracks. These results demonstrate a potential of NVX-CoV2373 vaccine to protect the lower respiratory track against pulmonary disease and upper respiratory track against virus replication thus helping to establish herd immunity and to halt the COVID-19 pandemic and its devastating global impact.
Author contributions
MGX, GS, GG, JHT, ADP, MJM, MBF and LE contributed to conceptualization of experiments, generation of data and analysis, and interpretation of the results. NP, JHT, BZ, and SM performed experiments. MGX, NP and KL coordinated projects. GS, GG, MBF, PAP, MGX, NP and LE contributed to drafting and making critical revisions with the help of others.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding for certain studies was provided by the Coalition for Epidemic Preparedness Innovations (CEPI), PO Box 123, Torshov, 0412 Oslo, Norway. The authors thank Drs. Hanna Andersen (BioQual, Inc.) for support in conducting the primate challenge study and Shannon Wallace (Experimental Pathology Laboratories) for providing histopathological services and support.
References
- 1.Jing-Hui Tian, Nita Patel, Robert Haupt, Haixia Zhou, Stuart Weston, Holly Hammond, et al. SARS-CoV-2 spike glycoprotein vaccine candidate NVX-CoV2373 elicits immunogenicity in baboons and protection in mice. bioRxiv 2020; doi: https://doi.org/10.1101/2020.06.29.178509. [DOI] [PMC free article] [PubMed]
- 2.Keech C., Albert G., Cho I., Robertson A., Reed P., Neal S., Plested J.S., Zhu M., Cloney-Clark S., Zhou H., Smith G., Patel N., Frieman M.B., Haupt R.E., Logue J., McGrath M., Weston S., Piedra P.A., Desai C., Callahan K., Lewis M., Price-Abbott P., Formica N., Shinde V., Fries L., Lickliter J.D., Griffin P., Wilkinson B., Glenn G.M. Phase 1–2 Trial of a SARS-CoV-2 Recombinant Spike Protein Nanoparticle Vaccine. N Engl J Med. 2020 doi: 10.1056/NEJMoa2026920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.-L., Abiona O., Graham B.S., McLellan J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science:abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wölfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Müller M.A., Niemeyer D., Jones T.C., Vollmar P., Rothe C., Hoelscher M., Bleicker T., Brünink S., Schneider J., Ehmann R., Zwirglmaier K., Drosten C., Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 5.Shan C., Yao Y.-F., Yang X.-L., Zhou Y.-W., Gao G.e., Peng Y., Yang L., Hu X., Xiong J., Jiang R.-D., Zhang H.-J., Gao X.-X., Peng C., Min J., Chen Y., Si H.-R., Wu J., Zhou P., Wang Y.-Y., Wei H.-P., Pang W., Hu Z.-F., Lv L.-B., Zheng Y.-T., Shi Z.-L., Yuan Z.-M. Infection with novel coronavirus (SARS-CoV-2) causes pneumonia in Rhesus macaques. Cell Res. 2020;30(8):670–677. doi: 10.1038/s41422-020-0364-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chandrashekar A., Liu J., Martinot A.J., McMahan K., Mercado N.B., Peter L., Tostanoski L.H., Yu J., Maliga Z., Nekorchuk M., Busman-Sahay K., Terry M., Wrijil L.M., Ducat S., Martinez D.R., Atyeo C., Fischinger S., Burke J.S., Slein M.D., Pessaint L., Van Ry A., Greenhouse J., Taylor T., Blade K., Cook A., Finneyfrock B., Brown R., Teow E., Velasco J., Zahn R., Wegmann F., Abbink P., Bondzie E.A., Dagotto G., Gebre M.S., He X., Jacob-Dolan C., Kordana N., Li Z., Lifton M.A., Mahrokhian S.H., Maxfield L.F., Nityanandam R., Nkolola J.P., Schmidt A.G., Miller A.D., Baric R.S., Alter G., Sorger P.K., Estes J.D., Andersen H., Lewis M.G., Barouch D.H. SARS-CoV-2 infection protects against rechallenge in rhesus macaques. Science. 2020;369(6505):812–817. doi: 10.1126/science:abc4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao Q., Bao L., Mao H., Wang L., Xu K., Yang M., Li Y., Zhu L., Wang N., Lv Z., Gao H., Ge X., Kan B., Hu Y., Liu J., Cai F., Jiang D., Yin Y., Qin C., Li J., Gong X., Lou X., Shi W., Wu D., Zhang H., Zhu L., Deng W., Li Y., Lu J., Li C., Wang X., Yin W., Zhang Y., Qin C. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369(6499):77–81. doi: 10.1126/science:abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neeltje van Doremalen, Teresa Lambe, Alexandra Spencer, Sandra Belij-Rammerstorfer, Jyothi N. Purushotham, Julia R. Port, et al. ChAdOx1 nCoV-19 vaccination prevents SARS-CoV-2 pneumonia in rhesus macaques. bioRXiv. 2020; https://doi:10.1101/2020.05.13.093195. [DOI] [PMC free article] [PubMed]
- 9.Yu J., Tostanoski L.H., Peter L., Mercado N.B., McMahan K., Mahrokhian S.H., Nkolola J.P., Liu J., Li Z., Chandrashekar A., Martinez D.R., Loos C., Atyeo C., Fischinger S., Burke J.S., Slein M.D., Chen Y., Zuiani A., Lelis F.J.N., Travers M., Habibi S., Pessaint L., Van Ry A., Blade K., Brown R., Cook A., Finneyfrock B., Dodson A., Teow E., Velasco J., Zahn R., Wegmann F., Bondzie E.A., Dagotto G., Gebre M.S., He X., Jacob-Dolan C., Kirilova M., Kordana N., Lin Z., Maxfield L.F., Nampanya F., Nityanandam R., Ventura J.D., Wan H., Cai Y., Chen B., Schmidt A.G., Wesemann D.R., Baric R.S., Alter G., Andersen H., Lewis M.G., Barouch D.H. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science. 2020;369(6505):806–811. doi: 10.1126/science:abc6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corbett K.S., Flynn B., Foulds K.E., Francica J.R., Boyoglu-Barnum S., Werner A.P., Flach B., O’Connell S., Bock K.W., Minai M., Nagata B.M., Andersen H., Martinez D.R., Noe A.T., Douek N., Donaldson M.M., Nji N.N., Alvarado G.S., Edwards D.K., Flebbe D.R., Lamb E., Doria-Rose N.A., Lin B.C., Louder M.K., O’Dell S., Schmidt S.D., Phung E., Chang L.A., Yap C., Todd J.-P., Pessaint L., Van Ry A., Browne S., Greenhouse J., Putman-Taylor T., Strasbaugh A., Campbell T.-A., Cook A., Dodson A., Steingrebe K., Shi W., Zhang Y.i., Abiona O.M., Wang L., Pegu A., Yang E.S., Leung K., Zhou T., Teng I.-T., Widge A., Gordon I., Novik L., Gillespie R.A., Loomis R.J., Moliva J.I., Stewart-Jones G., Himansu S., Kong W.-P., Nason M.C., Morabito K.M., Ruckwardt T.J., Ledgerwood J.E., Gaudinski M.R., Kwong P.D., Mascola J.R., Carfi A., Lewis M.G., Baric R.S., McDermott A., Moore I.N., Sullivan N.J., Roederer M., Seder R.A., Graham B.S. Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. N Engl J Med. 2020;383(16):1544–1555. doi: 10.1056/NEJMoa2024671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rockx B., Kuiken T., Herfst S., Bestebroer T., Lamers M.M., Oude Munnink B.B., de Meulder D., van Amerongen G., van den Brand J., Okba N.M.A., Schipper D., van Run P., Leijten L., Sikkema R., Verschoor E., Verstrepen B., Bogers W., Langermans J., Drosten C., Fentener van Vlissingen M., Fouchier R., de Swart R., Koopmans M., Haagmans B.L. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science. 2020;368(6494):1012–1015. doi: 10.1126/science:abb7314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang J., Wang W., Chen Z., Lu S., Yang F., Bi Z., Bao L., Mo F., Li X., Huang Y., Hong W., Yang Y., Zhao Y., Ye F., Lin S., Deng W., Chen H., Lei H., Zhang Z., Luo M., Gao H., Zheng Y., Gong Y., Jiang X., Xu Y., Lv Q.I., Li D., Wang M., Li F., Wang S., Wang G., Yu P., Qu Y., Yang L.I., Deng H., Tong A., Li J., Wang Z., Yang J., Shen G., Zhao Z., Li Y., Luo J., Liu H., Yu W., Yang M., Xu J., Wang J., Li H., Wang H., Kuang D., Lin P., Hu Z., Guo W., Cheng W., He Y., Song X., Chen C., Xue Z., Yao S., Chen L.u., Ma X., Chen S., Gou M., Huang W., Wang Y., Fan C., Tian Z., Shi M., Wang F.-S., Dai L., Wu M., Li G., Wang G., Peng Y., Qian Z., Huang C., Lau J.-N., Yang Z., Wei Y., Cen X., Peng X., Qin C., Zhang K., Lu G., Wei X. A vaccine targeting the RBD of the S protein of SARS-CoV-2 induces protective immunity. Nature. 2020;586(7830):572–577. doi: 10.1038/s41586-020-2599-8. [DOI] [PubMed] [Google Scholar]