Abstract
Introduction
Self-medication is an important part of daily self-care, without the supervision of health professionals. It is commonly practiced by pregnant women all over the world and may result in maternal and fetal risks. Hence, this study assessed self-medication practices and associated factors among pregnant women attending Kemisie General Hospital.
Methods
A facility-based cross-sectional study was conducted using a structured questionnaire on pregnant women who were attending antenatal care at Kemisie General Hospital. A simple random sampling technique was employed to select the study participants. Descriptive and inferential statistics were computed using the Statistical Package for Social Sciences version 20.
Results
Among 223 pregnant women, 60 (26.9%; 95% CI: 20.9%, 32.9%) and 111 (48.9%; 95% CI: 43%, 58%) practiced self-medication on conventional and herbal medicine, respectively. The predictors of self-medication of conventional medicine among pregnant women were prior experience to the drug (P-value: 0.00, AOR=126.04, 95% CI: 32.55–488.04) and no pervious history of abortion (P-value: 0.00, AOR=0.01,95% CI:0.002–0.04), while college educational level (P-value: 0.00, AOR=13.45,95%, CI: 3.58–50.5), history prior herbal medicine use (P-value: 0.00, AOR=9, 95% CI: 3.32–24.39), Ruta chalepensis (P-value:0.001,AOR=193.7,95% CI:8.64–4342.1) and Ocimum lamiifolium type of herb use (P-value: 0.004, AOR=12.72, 95% CI: 2.27–71.38), and 5–10km health facility distance (P-value:0.022, AOR=0.1, 95% CI: 0.01–0.73) were predictors for self-medication practice of herbal medicines among pregnant women.
Conclusion
Nearly one-third and two-third of pregnant women practiced self-medication on conventional and herbal medicine, respectively. Prior experience to the drug and no previous history of abortion associated with self-medication of conventional medicine, while college educational level, history prior herbal medicine use, Ruta chalepensis and, Ocimum lamiifolium type of herb use, and 5–10km distance were predictors for self-medication practice of herbal medicines. Improving health service coverage and awareness creation on rational medication use is recommended to prevent fetal and maternal risks.
Keywords: self-medication, conventional medicine, herbal medicine, pregnant women
Introduction
According to World Health Organization, self-medication is the treatment of self-diagnosed disorders or symptoms by use of medicines or intermittent or continued use of medicines prescribed by physicians for chronic or recurring diseases.1 It is one of the basic components of self-care and includes taking of drugs, herbs or home remedies2 by one’s own initiative, or by the advice of another person, without consulting a doctor.3
Self-medication is a common practice all over the world. The World Health Organization reported that about 70–80% of the world’s population relies on the use of non-conventional medicines in their primary healthcare.2 In developing countries, self-medication is widely practiced due to poor medical services and a lack of professional control of pharmaceutical products. This forced people to self-medicate various forms of substances and herbs that are often used for different medical complaints.4 In addition, in most of the economically deprived countries, including Ethiopia, many drugs are dispensed over the counter, and nearly 60%–80% of health-related problems are treated through self-medication as a lower-cost alternative.5,6
Pregnant women’s are one of the vulnerable population groups who practice self-medication frequently and repeatedly for the prevention of abortion, treatment of pregnancy-related problems such as dysmenorrhea, menopausal symptoms, menstrual disorders, mood disorders, osteoporosis, pregnancy, and prevention of anemia.7
Self-medication is commonly practiced by pregnant women due to better accessibility, affordability, and availability of herbal medicines.4 Assuming natural treatment has no problem with the fetus and the mother, and better efficacy compared to modern medicine forced pregnant women to practice self-medication.7,8 Moreover, the severity of illness, emergency use and prior experience of illness pushed pregnant women to self-medicate.4,9–12
Self-medication is an essential part of daily self-care and is affected by various factors such as income, local culture, age, gender, education level, knowledge, access to medicines, time, perception of risk of self-medication, previous medication use, gestational age, and occupation.6–8,13,14
Use of self-medication by pregnant women with medicine and/or herb can disturb the development of the embryo or fetus and may cause serious structural and functional adverse effects, including low birth weight, premature birth, feeding problems, respiratory problems, malformations, developmental fetal toxicity, and other potential harm to the fetus4,11,15–17 and mother.4,14,18 In addition, the increased practice of self-medication will exacerbates the danger of drug interaction and adverse event and results in irrational use of drugs.5 Thus, it is appropriate to evaluate and know the drugs that are consumed during pregnancy.17 This study was conducted to determine the pattern of self-medication and contributing factors among pregnant women attending the antenatal care (ANC) clinic of Kemisie General Hospital.
Methods
Study Area and Period
The study was conducted at Kemisie General Hospital, Kemisie town, North East Ethiopia, from April 20 to June 15, 2019. Kemisie is located 326 km from Addis Ababa. The hospital provides specialized health services to the town and the surrounding population. There are different wards and clinics within Kemisie General Hospital, from which the ANC clinic is one of the services provided.
Study Design
A facility-based cross-sectional study was employed to assess self-medication among pregnant women who were attending ANC at Kemisie General Hospital.
Population
All pregnant women who attended ANC during the study period at Kemisie General Hospital were the source population, while all pregnant women who attended ANC at Kemisie General Hospital during the study period and who fulfilled the inclusion criteria were the study population. All pregnant women who were unable to hear or communicate with and with mental disabilities and mothers who refused to give information about the use of traditional medicine or modern medicine during pregnancy were excluded from the study.
Sample Size Determination and Sampling Technique
The sample size was estimated by using a single population proportion formula using 26.6% prevalence,15 95% confidence level, and 5% tolerable sampling error. Since the source population was less than 10,000 (725), the sample size was adjusted with a total of 223 participants. A simple random sampling technique was employed to select the study participants.
Study Variables
The dependent variables were the prevalence of self-medication practice of conventional and herbal medicine use and independent variables were socio-demographic characteristics of pregnant women, obstetrics characteristics, and previous history of self-medication of conventional and herbal medicine use.
Data Collection Procedure and Quality Assurance
The data were pretested in five percent of the sample size at the Dessie referral hospital. After collecting the pilot data, the responses of the respondents were entered in a spreadsheet and the data were cleaned using principal component analysis. The reliability of the questionnaire was also checked using Cronbach’s alpha test and a value of 77% was obtained. The data were collected using a structured interviewer-administered questionnaire by two nurses who had no working relation to the hospital after recruiting and training with the supervision of the principal investigators. Data were checked for completeness, accuracy, and consistency immediately after collection and appropriately arranged and kept in a secured place for compilation and analysis.
Data Processing and Analysis
Data were entered and analyzed using the Statistical Package for Social Sciences version 20. After bivariate logistic regression analyses, variables with a p-value less than 0.25 was entered in the multivariate logistic regression and those with a p-value less than 0.05 were taken as statistically significant.
Definition of Terms
Self-medication: It is taking drugs, herbs or home remedies on one’s own initiative or on the advice of another person, without consulting a doctor.3
Conventional medicines: Is a medicine what you get from medical doctors, nurses, physical therapists, psychologists, and similar health-care professionals.
Herbal medicine: Is the use of medicinal plants for the prevention and treatment of diseases.19
Results
Of 223 pregnant women, 71 (31.8%) were in the aged group of 25–29 years and 142 (63.7%) were married. Moreover, 86 (38.6%) pregnant women were at the college level, and 131 (58.7%) pregnant women were within 5 kilo meters (km) (Table 1).
Table 1.
Socio-Demographic Characteristics of Pregnant Women Attending ANC at Kemisie General Hospital, 2019 (N=223)
| Characteristics | Frequency | Percent (%) |
|---|---|---|
| Age (year) | ||
| 15–19 | 58 | 26 |
| 20–24 | 24 | 10.8 |
| 25–29 | 71 | 31.8 |
| 30–34 | 37 | 16.6 |
| 35–39 | 24 | 10.8 |
| 40–49 | 9 | 4.0 |
| Marital status | ||
| Single | 4 | 1.8 |
| Married | 142 | 63.7 |
| Divorced | 48 | 21.5 |
| Widowed | 29 | 13 |
| Educational level | ||
| Illiterate | 44 | 19.7 |
| Primary school | 38 | 17.0 |
| Secondary school | 18 | 8.1 |
| College/diploma | 86 | 38.6 |
| University/degree | 37 | 16.6 |
| Residence | ||
| Urban | 156 | 70 |
| Rural | 67 | 30 |
| Distance from health facility | ||
| <5km | 131 | 58.7 |
| 5–10km | 43 | 19.3 |
| >10km | 49 | 22 |
| Average monthly income | ||
| 1000–1400 | 41 | 18.4 |
| 1500–1900 | 5 | 2.2 |
| 2000–2400 | 51 | 22.9 |
| 2500–2900 | 91 | 40.8 |
| 3000–3400 | 35 | 15.7 |
Nearly half (52%) of pregnant women were in the second trimester. Two hundred fourteen (96%) pregnant women had less than five gravid and had less than three children. Twenty-nine (13%) of them had a history of previous abortion (Table 2).
Table 2.
Obstetric Characteristics of Pregnant Women Attending ANC at Kemisie General Hospital, 2019 (N=223)
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Gestational age | First trimester | 59 | 26.5 |
| Second trimester | 116 | 52.0 | |
| Third trimester | 48 | 21.5 | |
| Number of gravid | 1–5 | 214 | 96.0 |
| >5 | 9 | 4.0 | |
| Number of child | 1–3 | 214 | 96.0 |
| 4–5 | 9 | 4.0 | |
| Previous abortion | Yes | 29 | 13.0 |
| No | 194 | 87.0 |
Self-Medication Practice of Conventional Medicine
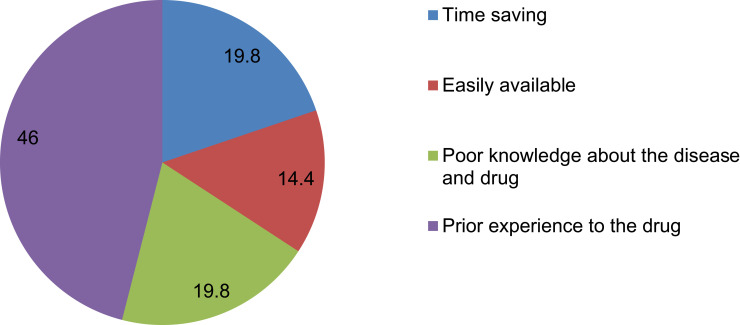
Sixty (26.9%; 95% CI: 20.9%, 32.9%) pregnant women practiced self-medication on conventional medicine during their current pregnancy. The most common reason for practicing self-medication was having prior experience with the drug 51 (46%), followed by poor knowledge about the disease, treatment and time saving 22 (19.8%) (Figure 1).
Figure 1.
Conventional drugs self-medication reasons among pregnant women at Kemisie General Hospital, 2019 (N=60).
The stated reasons for self-medication were using drugs to treat headaches 18 (30%) followed by common cold (28%), while the most widely used drug for self-medication was paracetamol (31.7%). The most common source of information for self-medication was pharmacist/druggist 26 (43%), and 30 (50%) got drugs from community drug retail outlets. Twelve (20%) pregnant women knew the dose of the drug, while 17 (28.3%) of them had no information about the drug they used for self-medication during pregnancy (Table 3).
Table 3.
Characteristics of Conventional Drugs Self-Medication Among Pregnant Women at Kemisie General Hospital, 2019 (N=60)
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Indication | Headache | 18 | 30 |
| Nausea/Vomiting | 9 | 15 | |
| Urinary tract infection | 4 | 7 | |
| Common cold | 17 | 28 | |
| Cough | 12 | 20 | |
| Common drugs used for self-medication | Paracetamol | 19 | 31.7 |
| Aspirin | 4 | 6.7 | |
| Amoxicillin* | 12 | 20 | |
| Cough syrup | 17 | 28.3 | |
| Hyoscine | 8 | 13.3 | |
| Sources of information | Yourself | 14 | 23 |
| Husband | 4 | 7 | |
| Neighbor | 8 | 13 | |
| Internet | 8 | 13 | |
| Pharmacist/Druggist | 26 | 43 | |
| Attainment of drugs used for self-medication | Neighbor | 7 | 11.7 |
| Friend | 4 | 6.7 | |
| Shop | 18 | 30 | |
| Community drug retail outlets | 30 | 50 | |
| Other** | 1 | 1.7 | |
| Knowledge about the drugs used for self-medication | Dose | 12 | 20 |
| Side effect | 13 | 21.7 | |
| Administration | 18 | 30 | |
| No information | 17 | 28.3 | |
Notes: Amoxicillin*, prescription medicine; Other**, working area, family.
Age, marital status, educational level, distance from health facility, average monthly income, obstetric characteristics and characteristics of conventional drugs had p-value less than 0.25, and were not fitted to multivariate logistics regression analysis. Multivariate logistic regression analysis showed that previous abortion and previous history of self-medication were significantly associated with current self-medication. Women with a previous history of self-medication were 126.04 folds to practice self-medication than those with no previous history of self-medication (AOR: 126.04, 95% CI (32.55–488.03)) and women’s with previous history of abortion were 129.68 times to practice self-medication than those women’s with no previous history of abortion (Table 4).
Table 4.
Factors Associated with Conventional Drugs Self-Medication Among Pregnant Women at Kemisie General Hospital, 2019 (N=60)
| Variables | Self-Medication | (COR,95% CI) | (AOR,95% CI) | |
|---|---|---|---|---|
| Yes(N) | No(N) | |||
| Place of residence | ||||
| Urban | 52(86.7) | 104(63.8) | 3.69(1.64–8.29) | 1.4(0.26–7.41) |
| Rural | 8(13.3) | 59(36.2) | 1.00 | 1.00 |
| Number of gravid | ||||
| 1–5 | 55(91.7) | 159(97.5) | 0.28(0.07–1.07) | 0.27(0.02–3.32) |
| >5 | 5(8.3) | 4(2.5) | 1.00 | 1.00 |
| Previous history of abortion* | ||||
| Yes | 25(41.7) | 4(2.5) | 28.39(9.29–86.76) | 129.68(28.70–585.86) |
| No | 35(58.3) | 159(97.5) | 1.00 | 1.00 |
| Prior self-medication* | ||||
| Yes | 43(71.7) | 8(4.9) | 49.00(19.81–121.23) | 126.04(32.55–488.04) |
| No | 17(28.3) | 155(95.1) | 1.00 | 1.00 |
Note: *P value <0.05.
Self-Medication Practice of Herbal Medicine
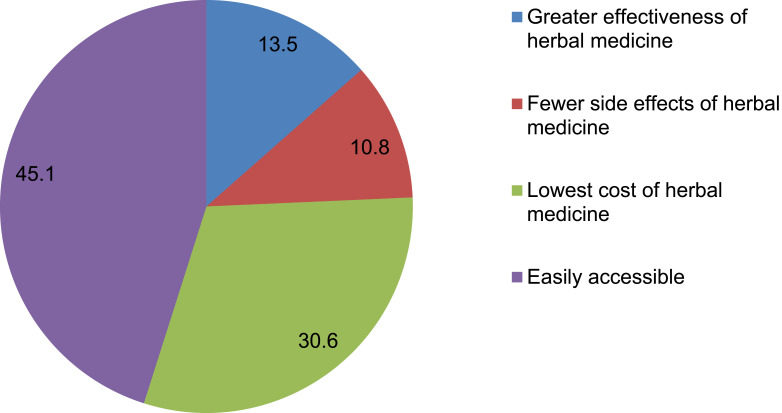
One hundred eleven (49.8%; 95% CI: 43%, 58%) of pregnant women practiced self-medication on herbal medicine during their current pregnancy. The stated reason for herbal medicine self-medication was easy accessibility 50 (45.1%) followed by lower cost 34 (30.6%) (Figure 2).
Figure 2.
Reasons for herbal medicine use among pregnant women at Kemisie General Hospital, 2019 (N=111).
Seventy (63%) pregnant women used the herbs to treat the common cold and the most widely used herb was Damakesie (Ocimum lamiifolium) (49.5%) and Tenadam (Ruta chalepensis) (43%). Fifty-eight (52.3%) pregnant women got information from their family and friends and forty-three (38.7%) pregnant women attained herbal medicines through self-preparation (Table 5).
Table 5.
Characteristics of Herbal Medicine Self-Medication Among Pregnant Women at Kemisie General Hospital, 2019 (N=111)
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Type of herbs used | Ginger (Zingiberofficinale) | 4 | 3.6 |
| Tenadam (Ruta chalepensis) | 48 | 43 | |
| Damakesie (Ocimum lamiifolium) | 55 | 49.5 | |
| Tosign(Ethiopian Thymus) | 4 | 3.6 | |
| Indication of using herbal medicine | Headache | 37 | 33 |
| UTI | 4 | 3.6 | |
| Common cold | 70 | 63 | |
| Source of information about herbal medicine | Traditional healer | 49 | 44 |
| Health profession | 4 | 3.6 | |
| Family & friends | 58 | 52.3 | |
| Sources of the herbal medicine | Self-preparation | 43 | 38.7 |
| Herbalist | 16 | 14.4 | |
| Traditional birth attendant | 15 | 13.5 | |
| Market place | 4 | 3.6 | |
| Neighbors | 33 | 29.7 |
In the univariate logistic regression analysis, age, marital status, residence, distance from health facility, average monthly income, obstetric characteristics and characteristics of herbal medicines were not fitted to multiple logistics regression analysis (p-value <0.25). Multivariate logistic regression analysis revealed that pregnant women who were at college educational level were 13.45 times (AOR: 13.45, 95% CI (3.58–50.50)) to use herbal medicine as compared to pregnant women at the university level. Pregnant women with history prior herbal medicine use were 9 (AOR: 9, 95% CI (3.32–24.39)) times more likely to use herbal medicine as compared to pregnant women with no history to prior herbal medicine use. The odds of pregnant women who lived <5km and 5–10km were 62% (AOR: 0.38, 95% CI (0.07–1.99)) and 90% (AOR: 0.1, 95% CI (0.01–0.73)) less likely to had self-medication than pregnant women who lived greater than 10km (Table 6).
Table 6.
Factors Associated with Herbal Medicine Self-Medication Among Pregnant Women at Kemisie General Hospital, 2019 (N=111)
| Variables | Herbal Medicine Use | (COR,95% CI) | (AOR,95% CI) | |
|---|---|---|---|---|
| Yes N (%) | No N (%) | |||
| Educational level | ||||
| Illiterate | 36(32.4) | 8(7.1) | 23.25(7.27–74.34) | 2.614(0.35–19.75) |
| Primary school | 4(3.6) | 34(30.4) | 0.61(0.15–2.36) | 0.06(0.0–1.65) |
| College* | 61(55) | 25(22.3) | 12.61(4.68–33.94) | 13.45(3.58–50.50) |
| University | 6(5.4) | 31(27.7) | 1.00 | 1.00 |
| Distance from health facility | ||||
| <5km* | 63(56.8) | 68(60.7) | 0.11(0.39–0.28) | 0.38(0.07–1.99) |
| 5–10km* | 4(3.6) | 39(34.8) | 0.01(0.00–0.04) | 0.10(0.01–0.73) |
| >10km | 44(39.6) | 5(4.5) | 1.00 | 1.00 |
| Type of herbs used | ||||
| Ruta chalepensis* | 48(43.2) | 35(31.3) | 4.8(1.45–15.83) | 193.71(8.64–4342.13) |
| Ocimum lamiifolium * | 55(49.6) | 47(42) | 4.1(1.26–13.29) | 12.717(2.26–71.38) |
| Ethiopian Thymus | 4(3.6) | 14(12.5) | 1.00 | 1.00 |
| Prior herbal medicine use | ||||
| Yes* | 91(82) | 19(17) | 22.27(11.16–44.46) | 9.00(3.32–24.39) |
| No | 20(18) | 93(83) | 1.00 | 1.00 |
Note: *p<0.05.
Discussion
The prevalence of self-medication of conventional medicine was 60 (26.9%; 95% CI: 20.9%-32.9%). This was in line with the study done at the public hospital of Harar town (28.8%)2 and Ondo state (35.2%),20 but higher than studies done in Egypt (16.6%)21 and Addis Ababa (18.2%)15 and lower than Nigeria (62.9%)18 and Yemen (54.1%).22 A systematic review and meta-analysis also reported a high prevalence of self-medication.23,24 This was due to poor awareness of pregnant women regarding medicines,17,25 selling of prescription medications without prescription and loose regulatory system.26
The prevalence of herbal medicine use was 111 (49.8%; 95% CI: 43%-58%). This result was consistent with the study done at the University of Gondar referral and teaching hospital (48.6%).8 The result was higher than that in Nigeria (38.6%),27 Nigeria (6.6%),18 Northern Uganda (20.4%),28 Addis Ababa (10.9%),15 Harar town (40.6%)2 and Hossana (13.1%),29 but lower than that done in Bangladesh (70%).30 This was due to women’s can easily access herbal medicines and self-prepare remedies at home.
The most common reasons for practicing self-medication of conventional medicine were having prior experience with the drug and time saving. This was comparable to the studies done in Egypt21 and Harar town.2 Easily accessibility and lower cost of herbal medicine were the common reasons for herbal medicine use. Similar results were reported by Addis Ababa,15 Bangladesh,30 Gonder,8 and Hossana.29
In this study, 30% and 28% of pregnant women used drugs to treat headaches and common cold, respectively. The most widely used drug for self-medication was paracetamol (31.7%) and cough syrup (28.3%). This was comparable to the study done at Addis Ababa15 and Harar town.2 This was attributed to the availability of medications and perceiving the disease conditions as mild illness and assuming the disease did not require health-care visit. Damakesie (Ocimum lamiifolium) and Tenadam (Ruta chalepensis) were used as a self-medication among pregnant women in this study. Similar findings were also reported at Harar2 and Hossana.29 The availability of the stated herbs in every households were responsible for patterns of resort.4
In the present study, the most common source of information for self-medication of conventional medicine was pharmacist/druggist and themselves. Similar source of information was reported in Harar town.2 Pharmacists are one of the most accessible health-care professionals in the community to offer ongoing education on medicines management, monitoring and advice to the population.31 The most common source to obtain conventional medicine was community drug retail outlet. This was similar to the studies done at Bahirdar,32 Hossana,29 Uganda28 and Harar town.2 Private health facilities were often concerned on client attraction to promote and improve their market value, and continuity of care.33
Concerning the source of information for herbal medicine use, pregnant women families and friends were the common sources. It was similar to the study done at Gonder,8 Harar town2 and Hossana town.29 Pregnant women got herbal medicine commonly from neighbors and self-preparation. The result was similar with the studies done at Hossana,29 Bahirdar,32 and Addis Ababa,15 but differs from the study done at Uganda.28 This might be attributed to the high influence of peers and close relatives due to low cost, easily accessibility and prior experience of traditional medicines.4
The prior experience of self-medication on conventional medicine showed a significant association with self-medication practice of conventional medicine among pregnant women. Those pregnant women who had prior experience of self-medication were 126 times more likely (P-value: 0.00, AOR = 126.04, CI: 32.55–488.04) to practice self-medication compared to those pregnant women with no prior experience. The finding was in line with studies done at Hossana,29 Harar2 and.34 Prior herbal medicine use was also significantly (P-value: 0.00, AOR=9, 95% CI: 3.32–24.39) associated with the herbal medicine use among pregnant women and similar findings were reported in Bangladesh,30 Bahirdar,32 and Gonder8 (9, 15). (11) This might be due to the fact that pregnant women attitude and practice to their earlier exposure to various conventional medicines might boost self-medication.
The previous history of abortion and self-medication are directly related. Pregnant women’s with previous history of abortion were 129.69 times to practice self-medication than those women’s with no previous history of abortion (P-value: 0.00, AOR = 129.68, CI: 28.70–585.86). For termination of fetus and inducing abortion, pregnant women might practice self-medication of drugs, herbs or home remedies by their own initiative, or on the advice of another person, without consulting and visiting health facilities.2,29
The results of this study showed that the odds of those pregnant women whose distance from the health facility was 5–10km were 90% less likely to practice self-medication compared to those pregnant women who came from greater than 10km. Distance from the health facility was also a predictor for self-medication done in Bangladesh,30 Bahirdar,32 and Gonder.8 An increase in the residence of pregnant women from the health facility will cause demand for the herbal medicine to rise, and hence, pregnant women more likely to use herbs as self-medication to reduce direct and indirect medical cost of health services. Thus, affordability by patient determines the choice of therapy.35
Even though there was no statistically significant association between income level and knowledge of pregnant women to self-medication, a significant number of pregnant women practiced self-medication of herbal and conventional medicine. But in developed countries including Ethiopia, these variables were supposed to be the determinant for self-medication since lower level of knowledge and income of pregnant women increased the practice of self-medication.2,15
Understanding the prevalence of self-medication and associated factors will help health-care providers in educating and counseling pregnant women about the consequence of self-medication and herbal medicine use. The findings are also crucial to a ministry of health to design and implement strategies to control conventional and herbal medicines marketing, distribution, and use. This will enhance rational drug use and promote drug therapy. Furthermore, the cross-sectional type of study design did not allow for the causal–effect relationship to be inferred or concluded from the results of the study. Recall bias and social desirability bias among pregnant women might affect the study findings as they were requested to respond based on their life experience.
Conclusion
Nearly one-third and two-third of pregnant women practiced self-medication on conventional and herbal medicine, respectively. The predictors of self-medication of conventional medicine among pregnant women were prior experience to the drug and no pervious history of abortion, while college educational level, history prior herbal medicine use, Ruta chalepensis type of herb use, Ocimum lamiifolium type of herb use and 5–10km health facility distance were predictors for self-medication practice of herbal medicines among pregnant women. It is recommended that healthcare providers should address pregnant women about the effects and unsafe use of conventional and herbal medicines. Improving health service coverage and awareness creation on rational medication use was recommended to prevent fetal and maternal risks.
Acknowledgment
The authors would like to acknowledge the Wollo University College of Medicine and Health Sciences Department of Pharmacy.
Funding Statement
There is no funding to report.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; KM, kilometer.
Data Sharing Statement
The datasets are available from the corresponding author upon reasonable request.
Ethical Consideration
Before commencing data collection, ethical approval was obtained from Ethics Review Committee of the Department of Pharmacy, College of Medicine and Health Sciences, Wollo University (WU Phar/076/11). Then, the study was conducted in the selected facilities after granting permission from each facility administrator and Kemisie town health office. Verbal informed consent was approved by the Ethics Review Committee of the Department of Pharmacy, Wollo University and this study was conducted in accordance with the Declaration of Helsinki. Moreover, participant under the age of 18 years was approved by the Ethics Review Committee of the Department of Pharmacy, Wollo University to provide informed consent on their own behalf. Verbal informed consent was obtained from study participants after providing information regarding the purpose of the study, why and how they are selected to be involved in the study, and what will be expected of them. Confidentiality of patient-specific data was maintained throughout the study.
Authors’ Contribution
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no potential competing interest.
References
- 1.Organization WH. Guidelines for the regulatory assessment of medicinal products for use in self-medication. World Health Organization; 2000. [Google Scholar]
- 2.Jambo A, Mengistu G, Sisay M, Amare F, Edessa D. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar town, Ethiopia. Front Pharmacol. 2018;9:1063. doi: 10.3389/fphar.2018.01063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernandez-Juyol M, Job-Quesada J. Dentistry and self-medication: a current challenge. Medicina oral: organo oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal. 2002;7(5):344. [PubMed] [Google Scholar]
- 4.Abasiubong F, Bassey EA, Udobang JA, Akinbami OS, Udoh SB, Idung AU. Self-Medication: potential risks and hazards among pregnant women in Uyo, Nigeria. Pan Afr Med J. 2012;13(1). [PMC free article] [PubMed] [Google Scholar]
- 5.Befekadu A, Dhekama NH, Mohammed MA. Self-medication and contributing factors among pregnant women attending antenatal care in Ethiopia: the case of Jimma University specialized hospital. Med Sci. 2014;3(1):969–981. doi: 10.5455/medscience.2013.02.8098 [DOI] [Google Scholar]
- 6.Ayalew MB. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adherence. 2017;11:401. doi: 10.2147/PPA.S131496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Afshary P, Mohammadi S, Najar S, Pajohideh Z, Tabesh H. Prevalence and causes of self-medication in pregnant women referring to health centers in southern of Iran. Int J Pharm Sci Res. 2015;6(2):612. [Google Scholar]
- 8.Mekuria AB, Erku DA, Gebresillassie BM, Birru EM, Tizazu B, Ahmedin A. Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at University of Gondar referral and teaching hospital, Ethiopia: a cross-sectional study. BMC Complement Altern Med. 2017;17(1):86. doi: 10.1186/s12906-017-1608-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marwa KJ, Njalika A, Ruganuza D, Katabalo D, Kamugisha E. Self-medication among pregnant women attending antenatal clinic at Makongoro health centre in Mwanza, Tanzania: a challenge to health systems. BMC Pregnancy Childbirth. 2018;18(1):16. doi: 10.1186/s12884-017-1642-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte Hospital, Western Ethiopia. Jundishapur J Nat Pharm Prod. 2014;9(4). doi: 10.17795/jjnpp-17368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emmanuel A, Achema G, Afoi BB, Maroof R. Self medication practice among pregnant women attending antenatal clinic in selected hospitals In Jos, Nigeria. 2014.
- 12.Yusuff KB, Omarusehe LD. Determinants of self medication practices among pregnant women in Ibadan, Nigeria. Int J Clin Pharm. 2011;33(5):868. doi: 10.1007/s11096-011-9556-4 [DOI] [PubMed] [Google Scholar]
- 13.Ebrahimi H, Atashsokhan G, Amanpour F, Hamidzadeh A. Self-medication and its risk factors among women before and during pregnancy. Pan Afr Med J. 2017;27(1). doi: 10.11604/pamj.2017.27.183.10030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gebremedhin GL, Gomathi P. Assessment of drug use and effect in pregnant women attending antenatal care in hospitals of Mekelle, Tigray, Ethiopia. J Drug Deliv Ther. 2014;4(6):75–82. doi: 10.22270/jddt.v4i6.999 [DOI] [Google Scholar]
- 15.Beza SW. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health. 2018;46(1):10. doi: 10.1186/s41182-018-0091-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohammed MA, Ahmed JH, Bushra AW, Aljadhey HS. Medications use among pregnant women in Ethiopia: a cross sectional study. J Appl Pharm Sci. 2013;3(4):116. [Google Scholar]
- 17.Banzal N, Saxena K, Dalal M. Research publications. J Basic Clin Pharmacol. 2017;6(4):924–927. doi: 10.18203/2319-2003.ijbcp20171105 [DOI] [Google Scholar]
- 18.Joseph B, Ezie I, Aya B, Dapar M. Self-medication among pregnant women attending ante-natal clinics in Jos-North, Nigeria. 2017.
- 19.Firenzuoli F, Gori L. Herbal medicine today: clinical and research issues. Evid Based Complement Alternat Med. 2007;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ojo IC, Okafor NA, Adeola OE, Adamolekun MM, Adewoyin RF Factors influencing self-medication practice among pregnant women attending antenatal clinic in primary health facilities in Akure South Local Government, Ondo State.
- 21.Khalaf S, Aly S, Ahmed A. Prevalence and attitude regarding non prescribed medications among pregnant women attending maternal and child health care centers in Assiut City.
- 22.Alkadasia MN, Putaiahb ET. Study of self-medication among pregnant women and associations with socio-demographic data in Al-qaedah district, Ibb, Yemen. J Med Res Health Sci. 2019;2(3):576–586. [Google Scholar]
- 23.Mohseni M, Azami-Aghdash S, Sheyklo SG, et al. Prevalence and reasons of self-medication in pregnant women: a systematic review and meta-analysis. Int J Community Based Nurs Midwifery. 2018;6(4):272. [PMC free article] [PubMed] [Google Scholar]
- 24.Adane F, Seyoum G, Alamneh YM, Abie W, Desta M, Sisay B. Herbal medicine use and predictors among pregnant women attending antenatal care in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):1. doi: 10.1186/s12884-020-2856-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baghianimoghadam MH, Mojahed S, Baghianimoghadam M, Yousefi N, Zolghadr R. Attitude and practice of pregnant women regarding self-medication in Yazd, Iran. Arch Iran Med. 2013;16(10). [PubMed] [Google Scholar]
- 26.Wado TE, Gunasekaran T, Dhanaraju MD. Pharmacist–patient communication barriers in dispensing practice: a descriptive study in Adama Hospital Medical College, Adama City, Oromia regional state, Ethiopia. J Pharm Health Serv Res. 2015;6(4):219–224. doi: 10.1111/jphs.12113 [DOI] [Google Scholar]
- 27.Duru CB, Uwakwe KA, Chinomnso NC, et al. Socio-demographic determinants of herbal medicine use in pregnancy among Nigerian women attending clinics in a tertiary Hospital in Imo State, south-east, Nigeria. Am J Med Stud. 2016;4(1):1–10. [Google Scholar]
- 28.Nyeko R, Tumwesigye NM, Halage AA. Prevalence and factors associated with use of herbal medicines during pregnancy among women attending postnatal clinics in Gulu district, Northern Uganda. BMC Pregnancy Childbirth. 2016;16(1):296. doi: 10.1186/s12884-016-1095-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laelago T, Yohannes T, Lemango F. Prevalence of herbal medicine use and associated factors among pregnant women attending antenatal care at public health facilities in Hossana Town, Southern Ethiopia: facility based cross sectional study. Arch Public Health. 2016;74(1):7. doi: 10.1186/s13690-016-0118-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmed M, Hwang JH, Hasan MA, Han D. Herbal medicine use by pregnant women in Bangladesh: a cross-sectional study. BMC Complement Altern Med. 2018;18(1):333. doi: 10.1186/s12906-018-2399-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicholls J, MacKenzie C, Braund R. Preventing drug-related adverse events following hospital discharge: the role of the pharmacist. Integr Pharm Res Pract. 2017;6:61. doi: 10.2147/IPRP.S104639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abeje G, Admasie C, Wasie B. Factors associated with self medication practice among pregnant mothers attending antenatal care at governmental health centers in Bahir Dar city administration, Northwest Ethiopia, a cross sectional study. Pan Afr Med J. 2015;20. doi: 10.11604/pamj.2015.20.276.4243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nigussie WD. Patient counselling at dispensing of medicines in health care facility outpatient pharmacies of Bahir Dar city, Northwest Ethiopia. Sci J Public Health. 2014;2(2):126–134. [Google Scholar]
- 34.Mbarambara PM, Songa PB, Wansubi LM, Mututa PM, Minga BBK, Bisangamo CK. Self-medication practice among pregnant women attending antenatal care at health centers in Bukavu, Eastern DR Congo. Int J Innov Appl Stud. 2016;16(1):38. [Google Scholar]
- 35.Abdulganiyu G, Fola T. What is the cost of illness of type II diabetes mellitus in a developing economy. Int J Pharm Pharm Sci. 2014;6(Suppl 2):927–931. [Google Scholar]