Abstract
Background
Although total knee replacement (TKR) is an effective intervention for end-stage arthritis of the knee, a significant number of patients remain dissatisfied following this procedure. Our aim was to identify and assess the factors affecting patient satisfaction following a TKR.
Materials and methods
In accordance with the PRISMA guidelines, two reviewers searched the online databases for literature describing factors affecting patient satisfaction following a TKR. The research question and eligibility criteria were established a priori. Any clinical outcome study that described factors relating to overall satisfaction after primary TKR was included. Quality assessment for the included studies was performed by two accredited orthopaedic surgeons experienced in clinical research.
Results
The systematic review identified 181 relevant articles in total. A history of mental health problems was the most frequently reported factor affecting patient satisfaction (13 reportings). When the results of the quality assessment were taken into consideration, a negative history of mental health problems, use of a mobile-bearing insert, patellar resurfacing, severe pre-operative radiological degenerative change, negative history of low back pain, no/less post-operative pain, good post-operative physical function and pre-operative expectations being met were considered to be important factors leading to better patient satisfaction following a TKR.
Conclusion
Surgeons performing a TKR should take these factors into consideration prior to deciding whether a patient is suitable for a TKR. Secondarily, a detailed explanation of these factors should form part of the process of informed consent to achieve better patient satisfaction following TKR. There is a great need for a unified approach to assessing satisfaction following a TKR and also the time at which satisfaction is assessed.
Electronic supplementary material
The online version of this article (10.1007/s00264-020-04607-9) contains supplementary material, which is available to authorized users.
Keywords: Total knee replacement, Total knee arthroplasty, Satisfaction, Dissatisfaction, Systematic review
Introduction
Total knee replacement (TKR) is one of the most effective surgical interventions for relief of pain and functional recovery in patients with advanced osteoarthritis (OA) of the knee. Management of OA costs the UK economy equivalent to 1% of its gross national product per year [1]. In the USA, the annual number of TKRs has been projected to rise by over 670% to 3.48 million cases by 2030 [2]. Outcomes of TKR are traditionally assessed by survival analysis with revision as the end point, and technical outcomes of this intervention are excellent. According to the UK National Joint Registry (NJR) annual report, the survival rate has been reported to be over 99.5% after one year and 95.6% at ten years [3].
A revision TKR is most commonly performed for loosening, fracture or infection. However, survival analysis tends to underestimate poor function, pain or dissatisfaction because these problems do not necessarily lead to a revision and are not recorded in the registry. Another issue is that reporting of the outcome of a TKR has predominantly been based on surgeon-derived outcome measures, which include range of movement (ROM), joint stability and post-operative alignment [4–6]. However, a report identified a poor correlation between surgeon-derived and patient-reported outcomes, with surgeons overestimating outcomes in comparison with the patients’ [7]. This correlates well with the fact that a significant number of patients experience continual pain and functional disability and therefore remain dissatisfied following the procedure [8–10].
In the largest ever reported series on satisfaction following a TKR, which included a survey of 27,372 patients, 17% of the unrevised patients were either dissatisfied or uncertain regarding their outcome [11]. Baker et al. [12] also reviewed the data from the NJR in the UK and reported that 71% of the patients experienced improvement of knee symptoms, but only 22% of them rated the results as excellent. Therefore, although the surgeon-reported outcomes may be good and the patient has no indication for a revision, they may still be dissatisfied following their index TKR. This may be due to a multitude of reasons, but to the best of our knowledge, there has been no systematic review which has specifically focused on the factors that affect patient satisfaction following a TKR. The aim of this systematic review, therefore, was to identify and assess the factors affecting patient satisfaction following a TKR.
Methods
The protocol of this systematic review was developed and has been registered in the International Prospective Register of Systematic Reviews (PROSPERO 2017 CRD42017084659). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used for designing this study [13].
Search strategy
Two accredited orthopaedic surgeons experienced in clinical research searched the online database Medline, Embase, BNI, AMED, Cochrane and Google Scholar for literature relating to satisfaction following a TKR. The PICO (participants, interventions, comparators, outcomes) tool was adopted and modified to formulate the research question and establish the inclusion and exclusion criteria. Selected articles were then exported to Mendeley reference manager software to organise screen and select articles.
Study screening and selection
Clinical outcome studies that described the factors relating to the overall or general satisfaction/dissatisfaction following a primary TKR irrespective of any pathology were included. The inclusion and exclusion criteria are described in Table 1. Any discrepancies at the title and abstract revision stage were resolved by automatic inclusion to ensure thoroughness. Any discrepancies at the full-text stage were resolved by consensus between the two reviewers. If a consensus could not be reached, a third, more senior reviewer was consulted to resolve the discrepancy.
Table 1.
Inclusion and exclusion criteria applied to articles identified in the literature
| Inclusion criteria | |
| 1. All levels of evidence | |
| 2. Written in the English language | |
| 3. Studies on humans | |
| 4. Studies reporting factors affecting overall satisfaction and/or dissatisfaction following a primary total knee replacement | |
| 5. Operative procedure consisted solely of total knee replacement | |
| 6. Total knee replacement irrespective of any pathology | |
| Exclusion criteria | |
| 1. Studies whose results included other procedures | |
| 2. Studies reporting satisfaction/dissatisfaction for only a small part of the procedure (e.g. ‘satisfaction in either pain control, skin closure, range of motion, nursing quality, anaesthesia, nerve block or physiotherapy’ was excluded) | |
| 3. Studies not reporting patient’s satisfaction (e.g. ‘studies on family’s or carer’s satisfaction’ were excluded) | |
| 4. Studies describing trial protocols without any results | |
| 5. Studies with follow-up period of 3 months or less | |
| 6. Revision total knee replacement | |
| 7. Unicompartmental knee replacement | |
| 8. Patellofemoral knee replacement | |
| 9. Cadaveric or radiological studies | |
| 10. Reviews, systematic reviews |
Data extraction and analysis
The two reviewers independently extracted relevant study data from the final pool of included articles and recorded this data on a spreadsheet designed a priori in Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA). The quality of studies including bias was then analysed and assessed using the Joanna Briggs Institute Critical Appraisal Checklist (JBICAC) for cohort studies, case–control studies, cross-sectional studies and case series [14]. For RCTs, a modified version of critical appraisal checklist by van Tulder et al. was used [15].
Statistical methods
Statistical analysis in this study focused on descriptive statistics. After assessing the quality of each study, the score was converted into a percentage from the full score (%), which was then considered to be the ‘strength’ of that particular study. Microsoft Excel 2013 was used for our analysis in reporting the factors affecting patient satisfaction following a TKR, based on the strength of studies as per the type of evidence. The potential factors were then categorised into seven groups designed from the findings of the studies included. The strength of each factor was presented, regardless of whether it was a FACTOR (‘it is a factor for patient satisfaction’) or a Not-FACTOR (‘it is a factor which does NOT relate to patient satisfaction’—in other words, ‘researcher X found Factor Z was irrelevant to patient satisfaction’).
Details are described in Electronic Supplementary Material 1 and Table 2.
Table 2.
Search strategy for Medline
| No. | Searches | Medline results |
|---|---|---|
| 1 | satisf$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 366,508 |
| 2 | tkr.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 1908 |
| 3 | tka.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 8888 |
| 4 | “total knee arthroplasty”.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 15,890 |
| 5 | “total knee replacement”.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 5129 |
| 6 | 2 or 3 or 4 or 5 | 21,446 |
| 7 | dissatisf$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 17,906 |
| 8 | 1 or 7 | 374,612 |
| 9 | 6 and 8 | 2187 |
Results
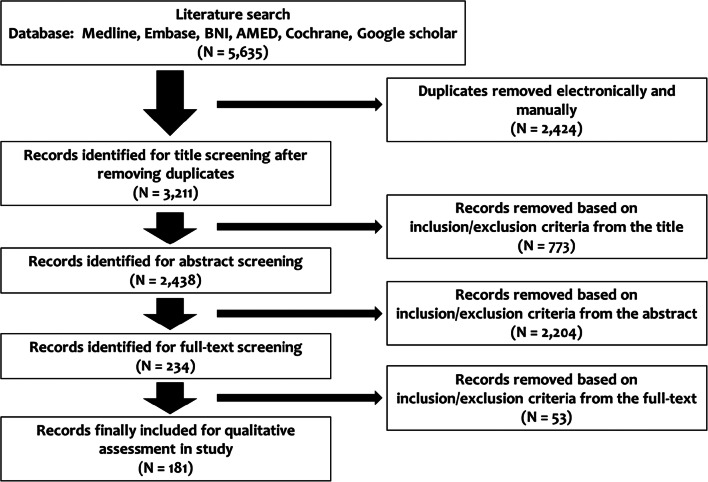
A total of 5635 articles were found following the initial search of the electronic databases and citation tracking, followed by removing 2424 duplicate articles. After review by title and abstract, 2977 articles were excluded and 234 potential articles remained for a full-text review. After application of the inclusion and exclusion criteria, a further 53 articles were discarded, leaving 181 relevant articles for the final inclusion, analysis and assessment. The study finally included 40 RCTs (22.1%), 93 cohort studies (51.4%), nine case–control studies (5.0%), 37 cross-sectional studies (20.4%) and 2 case series (1.1%) (Electronic Supplementary Material 2). Flowchart for the review is shown in Fig. 1 and the details of all the 181 studies are shown in Table 3. A total of 22 authors were found to have written several papers. To ensure that duplicate numbers were not included in our analysis, we contacted all these authors and reminder emails were sent as well to ensure a reply. Only five authors replied back with no overlap in their studies, three authors said that there was an overlap and 14 did not reply back. Those who did not reply back were treated as if it was an overlap and, thus, not considered. Due to the lack of homogeneity between studies, a meta-analysis was deemed unsuitable for this study.
Fig. 1.
PRISMA flowchart for results of the literature database search
Table 3.
Details of 181 included studies (alphabetical order of the first author’s name)
| First author | Serial no. | Factors affecting or relating to satisfaction | Measuring method for satisfaction | Year | Country | Type of study | Assessment timing | Number of TKRs | Men | Women | Age | BMI | Primary diagnosis | Surgical approach | Patellar resurface | Prosthesis | Use of cement | Anaesthesia |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adam | 1 | No difference between age 75 years or older and younger than 75 years | British Orthopaedic Association grading system | 1994 | UK | Cohort | Minimum 2 years | 125 | 18 | 67 |
78 G1 64 G2 |
NA | OA | NA | NA | NA | NA | NA |
| Albayrak | 2 | Patient satisfaction was higher in patients with low pain intensity | 4 grades (very satisfied, satisfied, dissatisfied, very dissatisfied) | 2016 | Turkey | Cross-sectional | 22.8 months | 274 | NA | NA | 66.8 | 32.3 | OA | MPP | NA | NA | Yes | Spinal or combined (spinal + epidural) |
| Ali | 3 |
(1) Very satisfied group had less pain, less anxiety or depression (2) Mean range of motion was 11 degrees greater in very satisfied group than the dissatisfied group |
4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2014 | Sweden | Cross-sectional | 10.5 years | 118 | 32 | 82 | 78.5 | 31.0 | OA | NA | NA | NA | NA | NA |
| Ali | 4 | No difference between patellar resurface group and non-resurface group | 4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2016 | Sweden | Randomised controlled trial | 6 years | 74 | 29 | 45 | 68.5 | 30.0 | OA | MPP | Yes and no | Triathlon (CR) | Yes | 62 spinal, 12 general |
| Ali | 5 |
(1) Patients with pre-operative anxiety or depression had more than 6 times higher risk to be dissatisfied compared with patients with no anxiety or depression (P < 0.001) (2) Patients with deep prosthetic infection had 3 times higher risk to be dissatisfied with the operation outcome (P < 0.03) (3) Dissatisfied patients had 1-day longer hospital stay compared with the satisfied patients (P < 0.001) |
4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2016 | Sweden | Cohort | 4 years | 186 | 66 | 120 | 72.5 | 30.0 | OA | MPP | NA | Triathlon (CR), PFC (CR) | NA | 87% spinal, 13% general |
| Altay | 6 | No difference between midvastus approach and MPP | 6 grades | 2011 | Turkey | Cohort | 41.3 months | 104 | 14 | 38 | 67.8 | 31.2 | NA | MPP, midvastus | NA | Maxim (fixed bearing) (PS) | NA | Spinal |
| Anderson | 7 |
(1) Poor mental health score, decreased physical function and increased bodily pain score negatively related to satisfaction (2) Age, gender, diagnosis, weight and pre-operative medical comorbidities did not relate to satisfaction |
5 grades (very satisfied, somewhat satisfied, neutral, somewhat dissatisfied, very dissatisfied) | 1996 | USA | Cohort | 2.85 years | 119 | 33 | 86 | 79.6 | NA | OA, RA | NA | NA | NA | NA | NA |
| Aunan | 8 | No difference between patellar resurfacing and non-resurfacing | VAS (0–100) | 2016 | Norway | Randomised controlled trial | 3 years | 129 | 48 | 67 | 70.0 | 29.5 | OA | MPP | Yes and no | NexGen (fixed bearing) (CR) | Yes | NA |
| Baker | 9 |
(1) Pain, women gender, OA, age younger than 65 and ASA 1 negatively related to satisfaction (2) Grade of the surgeon (consultant or not), site of the incision, use of a tourniquet and removal of the fat pad did not relate to satisfaction |
3 grades (yes (satisfied), not sure, no) | 2007 | UK | Cross-sectional | Minimum 1 year | 8231 | 3557 | 4671 | 70.8 | NA | OA, other | NA | NA | NA | NA | NA |
| Baker | 10 | Patients with BMI > 35 were less satisfied than the control group (18.5 < BMI < 24) | 4 grades (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) | 2013 | UK | Cohort | 3 years | 1367 | 585 | 782 | 68.8 | 29.5 | OA | NA | NA | PFC, triathlon | Yes | NA |
| Baker | 11 | The perception of symptom improvement (operative success) positively related to satisfaction | 5 grades (excellent, very good, good, fair, poor) | 2013 | UK | Cohort | 199 days | 22278 | NA | NA | NA | NA | OA | NA | NA | NA | NA | NA |
| Barlow | 12 | No difference between (1) stemmed prosthesis and non-stemmed prosthesis; (2) short (< 80 mm) stem and long (> 80 mm) stem; (3) one stem and two stems | Satisfied or not | 2016 | USA | Cohort | 2 years | 13825 | 4977 | 8848 | 67.5 | 30.4 | OA, inflammatory disease, AVN, post-trauma OA, fracture, other | NA | NA | NA | NA | NA |
| Barrack | 13 | No difference between patients with patellar resurfacing and those without it | Satisfied or not | 2001 | USA | Randomised controlled Trial | 70.5 months | 93 | NA | NA | NA | NA | OA | NA | Yes and no | MG II (CR) | Yes | NA |
| Barrack | 14 |
(1) Patients with incomes of less than USD 25,000, and women were less satisfied (2) Race, education, employment status and implant type (CR or PS, rotating platform, high flexion, gender specific) had no effect on satisfaction |
Satisfied or not | 2013 | USA | Cohort | 2.6 years | 661 | 256 | 405 | 54.0 | NA | OA | NA | NA | Unknown (52% CR, 27% PS, 9% rotating-platform, 6% high-flexion, 5% sex-specific) | NA | NA |
| Bican | 15 | Patients with fibromyalgia were less satisfied | 4 grades (very satisfied, satisfied, dissatisfied, very dissatisfied) | 2011 | USA | Case–control | 3.4 years | 180 | 2 | 57 | 61.0 | 34.0 | Fibromyalgia, OA | MPP | Yes | NA | Yes | Combined (spinal + epidural) or general |
| Bierke | 16 | Mean dissatisfaction scores were significantly higher in patients with somatisation dysfunction | 5 grades (very satisfied, satisfied, mediocre satisfied, unsatisfied, very unsatisfied) | 2016 | Germany | Cohort | 12 months | 100 | 37 | 63 | 60.6 | 29.9 | OA | MPP | No | Genesis II (CR) | Yes | General |
| Bierke | 17 | Patients with anxiety and particularly patients with pain catastrophizing tended to be dissatisfied | 5 grades (very satisfied, satisfied, mediocrely satisfied, unsatisfied, very unsatisfied) | 2017 | Germany | Cohort | 9 months | 138 | 87 | 51 | 69.0 | 29.9 | OA | MPP | NA | Genesis II | NA | General |
| Biyani | 18 | No difference between CS and PS | 5 grades (very satisfied, satisfied, neutral, dissatisfied, very dissatisfied) | 2017 | USA | Cohort | 1 year | 82 | 0 | 82 | 66.5 (Median) | 29.4 (Median) | NA | MPP | Yes | Triathlon (CS, PS) | NA | NA |
| Blyth | 19 | Using iNav Electromagnetic navigation system had no effect on satisfaction | 6 grades | 2015 | UK | Randomised controlled trial | 1 year | 198 | 116 | 82 | 65.5 | NA | OA | NA | NA | NexGen LPS-flex (PS) | Yes | NA |
| Boese | 20 | No difference between PFC Sigma rotating platform high flex and PFC Sigma rotating plat form | 5 grades | 2011 | USA | Case–control | 16.7 months | 153 | 63 | 90 | 64.0 | NA | OA | MPP | NA | PFC Sigma RP (rotating platform) (CR), PFC Sigma RP-F (rotating platform) (PS) | Yes | NA |
| Bonnin | 21 | Of the patients who reported they were as active as they expected to be before TKR, 98.2% were satisfied, while of the patients who reported they were insufficiently active, 52.3% were not satisfied (P < 0.0001) | 5 grades (very satisfied, satisfied, moderately satisfied, somewhat dissatisfied, dissatisfied) | 2010 | France | Cross-sectional | 44 months | 347 | 120 | 227 | 75.0 | 27.9 | OA, RA, AVN | NA | Yes and no | Noetos (PS), NexGen (PS)—282 mobile bearing, 65 fixed bearing |
Cemented tibia 338 Cemented femur 337 |
NA |
| Bourne | 22 | Patients with expectations not met, pre-operative pain at rest, and a post-operative complication requiring hospital readmission were less satisfied | 5 grades (very dissatisfied, dissatisfied, neutral, satisfied, very satisfied) | 2010 | Canada | Cross-sectional | 1 year | 1703 | 644 | 1059 | 69.3 | 32.0 | OA, RA, post-trauma OA, other | NA | Yes and no | Unknown (53% CR, 47% PS) | NA | NA |
| Bugada | 23 | Higher BMI and anxiety/depression levels were associated with dissatisfaction | VAS (0–10) | 2017 | Italy | Cohort | 6 months | 563 | 185 | 421 | 72 | NA | NA | NA | NA | NA | NA | General |
| Bullens | 24 | RA patients were more satisfied than OA patients | VAS (0–100) | 2001 | Netherlands | Cross-sectional | 4.9 years | 126 | NA | NA | 67.4 | NA | OA, RA, juvenile rheumatoid arthritis, haemophilic arthropathy | NA | Yes and no | PFC (95% CR, 5% PS) | Yes | NA |
| Burnett | 25 | No difference between patients with patellar resurfacing and those without it | Original questionnaire (41 points) | 2009 | USA | Randomised controlled trial | Minimum 10 years | 78 | NA | NA | 78.0 | NA | NA | NA | Yes and no | MG II (CR) | Yes | NA |
| Burnett | 26 | No difference between patients with patellar resurfacing and those without it | Original questionnaire | 2004 | USA | Randomised controlled trial | 7.3 years | 90 | 39 | 51 | 70.0 | 31.9 | OA | MPP | Yes and no | AMK (CR) | Hybrid (cemented tibia) | NA |
| Burnett | 27 | No difference between patients with patellar resurfacing and those without it | Original questionnaire (41 questions) | 2007 | USA | Randomised controlled trial | 110 months | 56 | 19 | 9 | 78.0 | NA | OA | NA | Yes and no | MG II (fixed bearing) (CR) | Yes | General |
| Chang | 28 | Patients with regular physical activity after TKR were more satisfied | VAS (0–10) | 2014 | South Korea | Cohort | 24 months | 369 | 30 | 339 | 68.8 | 27.4 | OA | NA | NA | NA | NA | NA |
| Chang | 29 | Post-operative severe pain relates to dissatisfaction | 4 grades (enthusiastic, satisfied, noncommittal, disappointed) | 2010 | South Korea | Cross-sectional | 1 year | 383 | 10 | 230 | 68.8 | 26.2 | OA | MPP | Yes | E-motion (mobile), Genesis II (fixed) | Yes | NA |
| Chinnappa | 30 | Radiologic leg length discrepancy (LLD) did not relate to patient satisfaction, but perception of LLD related to satisfaction | 5 grades | 2017 | Australia | Cohort | 6 months | 91 | 34 | 57 | 70.2 | 29.4 | OA, post-traumatic arthritis, AVN, RA | MPP | NA | PS implant made by Smith and Nephew | Yes | NA |
| Choi | 31 | No difference between standard PS rotating platform mobile bearing TKR and high flexion PS rotating platform mobile bearing TKR | 5 grades | 2010 | South Korea | Randomised controlled trial | 28 months | 170 | 9 | 119 | 70.5 | 26.6 | OA | MPP | Yes | PFC Sigma RP (rotating platform) (PS), PFC Sigma RP-F (rotating platform) (PS) | Yes | NA |
| Choi | 32 |
(1) Mobile bearing group is better than medial-pivot fixed bearing group in satisfaction (2) Patients with flexion contracture are less satisfied |
New KSS (40 points) | 2016 | South Korea | Cohort | Minimum 5 years | 101 | 12 | 89 | 67.1 | 27.5 | OA | MPP | Yes | 52 ACS (mobile bearing), 49 Advance (fixed bearing) | Yes | General |
| Clement | 33 | Patients with poor mental health were less satisfied | 4 grades (very satisfied, satisfied, neutral, unsatisfied) | 2013 | UK | Cohort | 1 year | 962 | 418 | 544 | 70.5 | NA | OA | NA | Yes and no | Kinemax, PFC sigma, Triathlon | NA | NA |
| Clement | 34 | Patients with back pain were less satisfied | 4 grades (very satisfied, satisfied, neutral, dissatisfied) | 2013 | UK | Cohort | 1 year | 2392 | 1017 | 1375 | 70.4 | NA | OA | NA | NA | Kinemax, Triathlon, PFC Sigma | NA | NA |
| Clement | 35 | Diabetes melitus had no effect on satisfaction | 4 grades (very satisfied, satisfied, uncertain, unsatisfied) | 2013 | UK | Cohort | 1 year | 2392 | 1014 | 1375 | 70.3 | NA | OA | NA | NA | Kinemax, Triathlon, PFC Sigma | NA | NA |
| Clement | 36 | Patients with a subclinical improvement in their general physical well-being were less likely to be satisfied | 4 grades (very satisfied, satisfied, neutral, unsatisfied) | 2013 | UK | Cohort | 12 months | 2330 | 996 | 1334 | 70.2 | NA | OA | NA | NA | Kinemax, Triathlon, PFC Sigma | Yes | NA |
| Clement | 37 | Post-operative OKS positively related to satisfaction | 4 grades (very satisfied, satisfied, neutral, unsatisfied) | 2013 | UK | Cohort | 1 year | 2392 | 1017 | 1357 | 70.4 | NA | OA | NA | NA | Kinemax, PFC sigma, Triathlon | NA | NA |
| Clement | 38 | Pre-operative OKS and improvement in OKS positively related to satisfaction | 4 grades (very satisfied, satisfied, unsure, unsatisfied) | 2013 | UK | Cross-sectional | 1 year | 966 | 421 | 545 | 70.6 | NA | OA | NA | NA | Kinemax, PFC sigma, Triathlon | NA | NA |
| Clement | 39 | Using ASM navigation did not relate to satisfaction | 4 grades (very satisfied, satisfied, uncertain, unsatisfied) | 2017 | UK | Cohort | 1 year | 295 | 121 | 174 | 68.4 | 31.0 | OA | MPP | NA | NA | Yes | NA |
| Clement | 40 | Age and gender did not relate to satisfaction. The risk of dissatisfaction was significantly increased if a patient’s expectation was not achieved | 4 grades (very satisfied, satisfied, neutral, unsatisfied) | 2014 | UK | Cohort | 1 year | 322 | 128 | 194 | 70.5 | NA | OA | NA | NA | Kinemax, Triathlon, PFC Sigma | Yes | NA |
| Clement | 41 | No difference in gap balanced technique and measured resection technique in computer-navigated TKR | 5 grades (very satisfied, satisfied, neutral, unsatisfied, very unsatisfied) | 2017 | UK | Cohort | 5.4 years | 144 | 65 | 79 | 69.0 | 31.2 | NA | MPP | NA | Columbus | Yes | NA |
| Collados-Maestre | 42 |
(1) Patients with pre-operative low back pain were less satisfied (2) Patients with severe low back pain were less satisfied than patients with moderate low back pain |
VAS (0–10) | 2016 | Spain | Cohort | 3.2 years | 48 | 19 | 29 | 73.7 | 30.4 | OA | MPP | Yes | Trekking (CR) | Hybrid (cemented tibia) | Spinal |
| Collados-Maestre | 43 | Single radius prosthesis group was better than multi radius prosthesis group | 5 grades (very satisfied, satisfied, neutral, dissatisfied, very dissatisfied) | 2016 | Spain | Randomised controlled trial | 5.7 years | 237 | 72 | 165 | 71.0 | 31.0 | OA | MPP | Yes | Trekking (fixed bearing) (CR, single-radius), Multigen (fixed bearing) (CR, multi-radius) | Hybrid (cemented tibia) | Spinal |
| Conditt | 44 | No difference between PS and CR | Total Knee Function Questionnaire | 2004 | USA | Cohort | 1 year | 49 | 21 | 28 | 70.5 | NA | NA | NA | NA | AMK (21 PS, 28 CR) | NA | NA |
| Devers | 45 | Post-operative passive knee flexion did not relate to satisfaction | 5 grades | 2011 | USA | Cross-sectional | 4 years | 122 | 29 | 93 | 69.0 | 30.8 | OA, RA, post-trauma OA | NA | NA | PFC Sigma (PS) | NA | NA |
| Dixon | 46 | Patients with Triathlon were more satisfied than those with Kinemax Plus | 4 grades | 2014 | UK | Cohort | 12 months | 453 | 150 | 303 | 69.0 | NA | OA, RA | NA | Yes and no | Triathlon (fixed bearing) (92% CR, 8% PS), Kinemax plus (53% fixed bearing) | Yes | NA |
| Dhurve | 47 |
(1) Age and BMI did not relate to satisfaction (2) Poor improvement of range of motion (ROM), pain catastrophizing and depression, severe swelling and unwilling to do post-operative rehabilitation programs related to dissatisfaction |
5 grades (very satisfied, satisfied, neutral, dissatisfied or very dissatisfied) | 2016 | Australia | Cross-sectional | Minimum 1 year | 301 | 142 | 159 | 73.9 | 30 | NA | NA | NA | NA | NA | NA |
| Dickstein | 48 | Severe pain and inability to use the stairs related to dissatisfaction | Satisfied or not | 1997 | Israel | Cross-sectional | 12 months | 79 | 26 | 53 | 70 | NA | OA | NA | NA | NA | Yes | NA |
| Duivenvoorden | 49 | Patients with pre-operative depressive or anxiety symptoms were less satisfied | 5 grades | 2013 | Netherlands | Cohort | 12 months | 128 | 56 | 72 | 66.2 | NA | OA | NA | NA | NA | NA | NA |
| Filardo | 50 | Control Preference Scale related to satisfaction | NRS (0–10) | 2016 | Italy | Cohort | 12 months | 176 | 56 | 120 | 66 | 28.0 | OA | MPP | NA | NA | NA | NA |
| Franklin | 51 | Patients who used narcotics before TKA were more likely to be dissatisfied | Unclear | 2010 | USA | Cohort | 12 months | 6346 | 2065 | 4224 | 67.4 | 31.9 | OA | NA | NA | NA | NA | NA |
| Fricka | 52 | No difference between cemented TKR and cementless TKR | Satisfied or not | 2015 | USA | Randomised controlled trial | 2 years | 99 | 37 | 62 | 59.3 | 32.0 | NA | Subvastus | Yes | NexGen CR-flex (fixed bearing) (CR) |
50 Yes 49 No |
NA |
| Furu | 53 | Patients with greater knee extensor strength were more satisfied | New KSS (40 points) | 2016 | Japan | Cohort | 1 year | 30 | 4 | 24 | 73.6 | 25.5 | OA, RA | MPP | Yes | Bi-surface, NexGen LPS-flex (fixed bearing) (PS) | Yes | NA |
| Giurea | 54 | Patients with specific personality traits (life satisfaction, performance orientation and emotional stability) were more satisfied | Satisfied or not | 2016 | Austria | Cohort | Minimum 2 years | 70 | 32 | 48 | 66.0 | NA | OA | MPP | Yes | E.motion UC (rotating platform) (CR) | Yes | NA |
| Gong | 55 | Significantly different satisfaction rate amongst the four personality: choleric type, 74.2%; sanguine type, 92.3%; melancholic type, 81.2%; phlegmatic type, 87.3% | VAS (0–100) | 2014 | China | Cross-sectional | 6 months | 387 | 109 | 278 | 59.6 | 27.8 | OA | NA | NA | Gemini MK II | NA | Epidural or nerve block |
| Goodman | 56 | No difference between RA patients and OA patients | 5 grades | 2016 | USA | Cohort | 2 years | 4456 | 1852 | 2604 | 67.1 | 30.7 | OA, RA | NA | NA | NA | NA | NA |
| Goudie | 57 | Patients with post-operative flexion contracture of 5 degrees or greater were less satisfied | 4 grades (very satisfied, satisfied, unsure, dissatisfied) | 2011 | UK | Cohort | 2 years | 811 | 317 | 489 | 69.0 | 30.5 | OA | NA | NA | Unknown (779 CR, 32 PS) | NA | NA |
| Gustke | 58 | By using Orthosensor, 96.7% in the medial-lateral balanced group and 82.0% in the unbalanced group were satisfied | 5 grades | 2014 | USA | Cohort | 1 year | 137 | 47 | 90 | 71.0 | 30.5 | OA | MPP, subvastus, midvastus | Yes | NA | Yes | NA |
| Ha | 59 | Patients with greater improve in ROM following TKR were more satisfied | 4 grades (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) | 2016 | South Korea | Cohort | 3.2 years | 630 | 58 | 572 | 66.2 | 26.7 | OA, RA, AVN | NA | No | 206 NexGen LPS-flex (PS), 163 Genesis II, 160 Triathlon, 101 Vanguard | NA | NA |
| Hamilton | 60 | Patients using Triathlon prosthesis were more satisfied than those using Kinemax prosthesis | 4 grades (very satisfied; satisfied; unsure, dissatisfied) | 2015 | UK | Randomised controlled trial | 3 years | 212 | 81 | 131 | 69.0 | NA | OA | NA | No | Triathlon (fixed bearing) (CR), Kinemax (fixed bearing) (CR) | Yes | NA |
| Harvie | 61 | Computer-navigated TKA did not relate to satisfaction | 5 grades | 2010 | Australia | Randomised controlled trial | 5 years | 46 | 18 | 28 | 70.1 | NA | OA and RA | NA | No | NA | NA | NA |
| Hawker | 62 | Less education and greater BMI negatively related to satisfaction | 5 grades | 1998 | Canada, USA | Cross-sectional | Minimum 2 years | 1193 | 344 | 849 | 72.6 | NA | OA, RA, post-trauma OA, other | NA | NA | NA | NA | NA |
| Heesterbeek | 63 | No difference between fixed and mobile bearing | NRS (0–10) | 2016 | Netherlands | Cross-sectional | 10 years | 189 | 52 | 106 | 67.1 | 28.6 | OA | NA | Yes and no | NA | NA | NA |
| Hernandez-Vaquero | 64 | Minimally invasive surgery had no effect on satisfaction | VAS (0–10) | 2010 | Spain | Randomised controlled study | 6 months | 62 | 11 | 51 | 70.6 | 31.5 | OA | Mini-midvastus, MPP | Yes | Triathlon (CR) | Yes | NA |
| Hinarejos | 65 | No difference between single radius prosthesis and multi-radius prosthesis | VAS (0–10) | 2016 | Spain | Cohort | 5 years | 474 | 126 | 348 | 72.2 | 31.3 | OA | MPP | Yes | Triathlon (PS, single-radius), Genutech (PS, multi-radius) | Yes | NA |
| Hirschmann | 66 | Lateral subvastus approach related to better satisfaction | VAS (0–10) | 2010 | Switzerland | Cohort | 2 years | 143 | 55 | 88 | 69 | 30 | OA | Lateral parapatellar approach, subvastus approach, or MPP | Yes and No | NA | Yes or hybrid | NA |
| Hui | 67 | No difference between oxidised zirconium and cobalt–chromium femoral components | British Orthopaedic Association grading system | 2011 | Australia | Randomised controlled trial | 5 years | 80 | 15 | 25 | NA | NA | OA | MPP | Yes | Genesis II | Yes | Spinal and/or epidural |
| Huijbregts | 68 |
(1) Coronal alignment of the femoral component was 0.5 degrees more accurate (P < 0.05) in patients who were satisfied (2) Dissatisfaction was associated with OKS |
5 grades (very satisfied, satisfied, neutral/not sure, dissatisfied, very dissatisfied) | 2016 | Australia | Cohort | 1 year | 230 | 105 | 106 | 69.0 | 30.2 | OA, RA, AVN, unknown | MPP, lateral parapatellar | Yes and no (including patellectomy) | Genesis II, Legion, ACS (139 CR, 91 PS) | NA | NA |
| Hwang | 69 | Patellar resurfacing did not relate to satisfaction | Satisfied or not | 2011 | South Korea | Case–control | 7 years | 275 | 6 | 264 | 68 | 26.5 | OA | MPP | Yes and no | LCS (mobile bearing) | Yes | NA |
| Jacobs | 70 | Patients with intact ACL (at the time of CR TKR) were less satisfied | 3 grades (satisfied, I'm not sure, dissatisfied) | 2016 | USA | Cohort | 5.1 years | 562 | 183 | 379 | 65.0 | 34.0 | NA | NA | NA | Vanguard Mono-lock (CR) | NA | NA |
| Jacobs | 71 |
(1) African American patients were 3.0 times more likely to be dissatisfied than Caucasians (2) Patients with mild degenerative changes were 2.1 times more likely to be dissatisfied than patients with severe degenerative changes |
3 grades (yes (satisfied), I'm not sure, no) | 2014 | USA | Cross-sectional | 3.5 years | 989 | 326 | 663 | 65.0 | 34.3 | OA | MPP | Yes | Unknown (CR) | NA | NA |
| Jacobs | 72 |
(1) No difference in age, gender and BMI between satisfied patients and dissatisfied patients (2) Satisfied patients showed greater improvement in ROM, Knee Society pain score and Knee Society function score than dissatisfied patients |
4 grades (yes (satisfied), I'm not sure, no) | 2014 | USA | Cross-sectional | 2.8 years | 768 | 247 | 521 | 65.0 | 34.3 | OA | NA | Yes | Vanguard complete femoral component with Monolock tibial component (CR) | NA | NA |
| Jacobs | 73 | Patients with movement-elicited pain or pain at rest were less satisfied | 3 grades (yes (satisfied), I'm not sure, no) | 2015 | USA | Cohort | 3.8 years | 316 | 91 | 184 | 65.1 | 33.9 | OA | NA | NA | Unknown (CR) | NA | NA |
| Jacobs | 74 | Patients with intra-operative greater forces (> 10 lbf) in the medial compartment than in the lateral compartment in extension were more satisfied | Satisfied or not | 2016 | USA | Cohort | 6 months | 50 | 21 | 29 | 66.1 | 34.5 | OA | MPP | NA | Vanguard (CR), Persona (CR) | NA | NA |
| Jain | 75 | Patient satisfaction was higher in the Vega and Genesis II groups than the E.motion group | British Orthopaedic Association grading system | 2017 | UK, South Korea, India | Cohort | 2 years | 627 | 30 | 597 | 69.6 | 27.3 | OA | MPP | Yes | Vega-PS, E.motion-PS, Genesis II | Yes | NA |
| Kaneko | 76 | The varus ligament balance with 30, 60 degrees of flexion negatively correlated with satisfaction | New KSS (40 points) | 2016 | Japan | Case series | 2 years | 39 | 8 | 31 | 78 | 24.4 | OA | NA | NA | Bi-cruciate stabilised substituting (BCS) prosthesis | Yes | NA |
| Kawahara | 77 |
(1) Patients with internal rotation of the femoral component greater than 3 degrees relative to the surgical epicondylar axis were less satisfied (2) Internal or external malrotation of tibial component had no effect on satisfaction |
New KSS (40 points) | 2014 | Japan | Cross-sectional | 3.9 years | 92 | NA | NA | 75.7 | 25.6 | OA | NA | Yes | NexGen LPS-flex (fixed bearing) (PS) | NA | NA |
| Kawakami | 78 | No significant difference between CR and PS | New KSS (40 points) | 2015 | Japan | Randomised controlled trial | 98 months | 48 | 8 | 40 | 74.2 | NA | OA | MPP | NA | NexGen CR-flex (CR), NexGen LPS-flex (PS) | Na | NA |
| Keurentjes | 79 | Patients with severe radiographic OA (K/L grades 3, 4) were more satisfied than patients with mild radiographic OA (K/L grades 0, 1 and 2) | NRS (0–10) | 2013 | Netherlands | Cohort | 2.82 years | 278 | 86 | 192 | 69.2 | NA | OA | NA | NA | NA | NA | NA |
| Keurentjes | 80 | Completed level of schooling had no effect on satisfaction | NRS (0–10) | 2013 | Netherlands | Cohort | 3.16 years | 262 | 88 | 174 | 67.7 | NA | OA | NA | NA | NA | NA | NA |
| Khamis | 81 | No difference between Scorpio NRG CR and PFC Sigma CR | Satisfied or not | 2013 | Bahrain | Cohort | 1 year | 299 | 145 | 154 | 65.9 | NA | OA | MPP | NA | Scorpio NRG (CR), PFC Sigma (CR) | NA | NA |
| Kim | 82 | Patients with medial pivot fixed bearing prosthesis were less satisfied than those with PFC Sigma mobile bearing prosthesis | VAS (0–10) | 2008 | South Korea | Randomised controlled study | 2.6 years | 184 | 7 | 85 | 69.5 | 27.8 | OA | MPP | Yes | Advance (fixed bearing) (CR), PFC Sigma (mobile bearing) (CR) | Yes | NA |
| Kim | 83 | Patients with rotating platform (E.motion RP) were more satisfied than those with floating platform (E.motion FP) | 4 grades (enthusiastic, satisfied, not committed, disappointed) | 2009 | South Korea | Cohort | 24 months | 186 | 9 | 177 | 68.5 | 26.3 | NA | MPP | Yes | 93 E.motion FP (CR), 93 E.motion RP (PS) | Yes | NA |
| Kim | 84 | No difference between gender-specific LPS-flex and conventional LPS-flex | VAS (0–10) | 2010 | South Korea | Randomised controlled study | 2.13 years | 170 | 0 | 85 | 69.7 | 27.1 | OA | MPP | Yes | LPS-flex (gender specific, conventional) (PS) | Yes | NA |
| Kim | 85 | No difference between patients with patellar resurfacing and those without it using high-flexion prosthesis | 5 grades (fully satisfied, satisfied, barely satisfied, dissatisfied, very dissatisfied) | 2014 | South Korea | Cohort | Minimum 7 years | 92 | 8 | 84 | 66.2 | 27.0 | OA | MPP | Yes and No | NexGen LPS-flex (fixed bearing) (PS) | Yes | NA |
| Kim | 86 | Poor pre-operative WOMAC pain score and post-operative decrease in range of motion negatively related to dissatisfaction | 4 grades (enthusiastic, satisfied, noncommittal, disappointed) | 2009 | South Korea | Cross-sectional | Minimum 12 months | 438 | 9 | 261 | 68.4 | 26.4 | OA | MPP | Yes | Genesis II (fixed bearing), E.motion (mobile bearing) | Yes | NA |
| Kim | 87 | No difference between NexGen CR-flex and NexGen CR | VAS (0–10) | 2009 | South Korea | Randomised controlled study | 3.13 years | 108 | 5 | 49 | 69.7 | 26.7 | OA | MPP | Yes | NexGen (CR), NexGen CR-flex (CR) | Yes | NA |
| Kim | 88 | No difference between standard NexGen CR-flex and gender-specific NexGen CR-flex | VAS (0–10) | 2010 | South Korea | Randomised controlled study | 3.25 years | 276 | 0 | 138 | 71.2 | 27.3 | OA | NA | Yes | NexGen CR-flex (gender specific, conventional) (CR) | Yes | NA |
| Kim | 89 | Dissatisfied patients tended to perceive high flexion activities to be more important than satisfied patients | 4 grades (enthusiastic, satisfied, not committed, disappointed) | 2010 | South Korea | Cross-sectional | Minimum 12 months | 261 | 0 | 261 | 68.4 | 26.7 | OA | MPP | Yes | 216 Genesis II (fixed bearing), 208 E.motion (mobile bearing) | Yes | NA |
| Kim | 90 | No significant influence by post-operative leg length discrepancy | 5 grades (fully satisfied, satisfied, barely satisfied, dissatisfied, very dissatisfied) | 2015 | South Korea | Cohort | 30 months | 148 | 15 | 133 | 69.5 | 26.6 | OA | Midvastus | No | Columbus (PS) | Yes | NA |
| Kim | 91 | PFC CR mobile-bearing Sigma were better than Medial-Pivot knee prosthesis about satisfaction | 4 grades | 2017 | South Korea | Randomised controlled study | 12.1 years | 364 | 52 | 130 | 65.6 | 29.8 | OA | MPP | Yes | Medial-Pivot (PS), PFC Sigma CR | Yes | NA |
| Kim | 92 | Cement use did not relate to satisfaction | VAS (0–10) | 2013 | South Korea | Randomised controlled study | 16.6 years | 160 | 17 | 63 | 54.3 | 27.8 | OA | MPP | Yes | NexGen CR | Yes | NA |
| Kim | 93 | Using a highly cross-linked polyethylene did not relate to satisfaction in PS TKR | VAS (0–10) | 2014 | South Korea | Case–control | 5.9 years | 308 | 20 | 288 | 60.3 | 29.1 | OA | MPP | Yes | Yes | Yes | NA |
| Klit | 94 | There were no statistically significant differences in the outcome of pre-operatively depressed and non-depressed patients concerning satisfaction | 5 grades (very satisfied, satisfied, neutral, dissatisfied and very dissatisfied) | 2013 | Denmark | Cohort | 12 months | 115 | 54 | 61 | 54 | NA | OA | MPP | NA | CR, fixed (AGC, PFC, Triathlon), CR, rotating bearing (PFC-Sigma Vanguard ROCC, NexGen), PS, fixed (LPS-flex) | NA | NA |
| Kornilov | 95 | The patients who reported ‘very good’ overall satisfaction tended to be younger | 5 grades | 2017 | Russia, Norway | Cohort | 1 year | 79 | 4 | 65 | 63 | NA | OA | MPP | NA | NA | Yes | Spinal |
| Kosse | 96 | Satisfaction did not improve by using patient-specific instrumentation | VAS (0–10) | 2017 | Netherlands | Randomised controlled trial | 12 months | 42 | 20 | 22 | 63.1 | 27.95 | OA | MPP | Yes | Genesis II (PS, fixed) | Yes | |
| Kotela | 97 | No difference between patient-specific CT-based instrumentation (signature) and conventional | VAS (0–100) | 2015 | Poland | Randomised controlled trial | 12 months | 95 | 29 | 66 | 66.3 | 29.8 | OA | MPP | No | Vanguard (CR) | No | NA |
| Krushell | 98 | 85% of patients with BMI > 40 were satisfied and 95% of patients with BMI < 30 were satisfied | Satisfied or not | 2007 | USA | Case–control | 90 months | 78 | NA | NA | 68.1 | 35.0 | OA | MPP, midvastus | Yes | Osteonics series 3000, Osteonics series 7000, Scorpio | Yes | NA |
| Khuangsirikul | 99 | Computer-assisted TKA did not relate to satisfaction | Original questionnaire | 2016 | Thailand | Cohort | 10 years | 144 | 14 | 130 | 76.9 | NA | OA | NA | NA | NA | NA | NA |
| Kuriyama | 100 | Post-operative noise had no relation to satisfaction | New KSS (40 points) | 2016 | Japan | Cross-sectional | 12 months | 35 | NA | NA | NA | NA | OA, RA. AVN | NA | NA | Bi-surface (fixed bearing) (PS) | NA | NA |
| Kuroda | 101 | No item in pre-operative new Knee Society Scores (objective knee indicators, symptoms, satisfaction, expectations, functional activities) had impact on satisfaction | New KSS (40 points) | 2016 | Japan | Cohort | 1 year | 79 | 12 | 63 | 74.8 | NA | OA, AVN, RA | NA | NA | PFC Sigma, e-motion | NA | NA |
| Kwon | 102 | Generalised joint laxity did not relate to satisfaction | VAS (0–10) | 2016 | South Korea | Case–control | 3 years | 338 | 0 | 338 | 68 | 25.9 | OA | MPP | Yes | PFC | Yes | NA |
| Kwon | 103 | Intra-operative periarticular injection with corticosteroid did not improve satisfaction | VAS (0–10) | 2013 | South Korea | Randomised controlled trial | 6 months | 76 | 0 | 76 | 69.3 | 25.9 | OA | MPP | No | PFC sigma PS | Yes | NA |
| Lehnen | 104 | Computer-assisted TKR was better than conventional TKR regarding satisfaction | 5 grades (extremely satisfied, very satisfied, moderately satisfied, slightly satisfied, not at all satisfied) | 2011 | Switzerland | Cohort | 12 months | 165 | 59 | 106 | 70.0 | NA | NA | MPP | NA | LCS (mobile bearing) | Yes | NA |
| Li | 105 | Continuous irrigation of 4000 ml cold saline with 0.5% epinephrine group was better than normal temperature solution group | VAS (0–10) | 2016 | China | Cohort | 60 h | 389 | 53 | 336 | 61.0 | 28.7 | OA | NA | NA | Gemini Link (CR) | Yes | Epidural or nerve block |
| Lim | 106 | No difference between patients with and without history of previous knee surgery (anterior cruciate ligament reconstruction or high tibial osteotomy) | 6 grades (excellent, very good, good, fair, poor; terrible) | 2016 | Singapore | Cross-sectional | 2 years | 303 | 220 | 83 | 65.0 | 27.2 | OA | MPP | NA | NA | NA | NA |
| Lingard | 107 | No difference amongst TKRs undertaken in the USA, UK and Australia | 4 grades (very satisfied to very dissatisfied) | 2006 | USA, UK, Australia | Cohort | 12 months | 598 | 254 | 344 | 69.3 | 29.3 | OA | NA | Yes and no | Kinemax | Yes | NA |
| Liow | 108 | No difference between iASSIST computer-assisted stereotaxic navigation group and conventional group | 6 grades | 2016 | Singapore | Case–control | 6 months | 192 | 53 | 139 | 65.5 | 27.9 | OA | MPP | NA | NA | NA | NA |
| Liow | 109 | No difference between robotic-assisted TKR and conventional TKR | 6 grades | 2016 | Singapore | Randomised controlled trial | 2 years | 60 | NA | NA | 67.9 | NA | OA | MPP | Yes | NexGen LPS-flex (PS) | NA | NA |
| Lizaur-Utrilla | 110 | Patients with mobile bearing insert were more satisfied than those with fixed bearing insert | VAS (0–10) | 2012 | Spain | Randomised controlled trial | 2 years | 119 | 25 | 94 | 74.2 | 32.0 | OA | MPP | Yes | Trekking mobile bearing (CR), Multigen Plus fixed bearing (CR) | Hybrid (cemented tibia) | Epidural |
| Lizaur-Utrilla | 111 | Dissatisfaction rate was higher in patients waiting longer than 6 months | 5 grades (very satisfied, satisfied, neutral, dissatisfied, very dissatisfied) | 2016 | Spain | Cohort | 1 year | 192 | 65 | 127 | 69.7 | 30.7 | OA | MPP | Yes | Trekking | Hybrid (cemented tibia) | Spinal |
| Lizaur-Utrilla | 112 | Satisfaction was higher in the octogenarian group than the septuagenarian | VAS (0–10) | 2016 | Spain | Cohort | 3.2 years | 292 | 212 | 80 |
83.1 G1 75.2 G2 |
30.2 | OA | NA | Yes | Yes | Hybrid | Epidural |
| Losina | 113 | Patients having a lack of hospital choice were less satisfied | 4 grades (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) | 2005 | USA | Cross-sectional | 2 years | 932 | 308 | 624 | 74.0 | NA | OA, other | NA | NA | NA | NA | NA |
| Lygre | 114 |
(1) Patella resurfacing did not relate to satisfaction (B) Patients with NexGen were more satisfied than those with AGC |
VAS (0–100) | 2010 | Norway | Case–control | 7.1 years | 972 | 281 | 691 | 76.0 | NA | OA | NA | Yes and No | AGC (CR), Genesis I (CR), NexGen (CR), LCS (CR) | NA | NA |
| Machhindra | 115 | No difference between Ultra Congruent prosthesis and PS prosthesis | 4 grades (enthusiastic, satisfied, noncommittal, disappointed) | 2015 | South Korea | Cohort | 2 years | 281 | 10 | 219 | 80.0 | 27.4 | OA | MPP | Yes | E.motion ultra-congruent (mobile bearing) (UC), E.motion (mobile bearing) (PS) | Yes | NA |
| Maddali | 116 | No difference between outcomes of one-stage and two-stage TKR for bilateral knee arthritis | 4 grades (very satisfied, satisfied, unsure, dissatisfied) | 2015 | China | Cohort | 2.4 years | 278 | 46 | 93 | 68.9 | 24.0 | OA, RA | MPP | No | Gemini MK II (mobile bearing) (PS) | Yes | General |
| Mannion | 117 | Patients with problems in other joints and poor improvement in symptoms and function were less satisfied | 4 grades (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) | 2009 | Switzerland | Cross-sectional | 2 years | 112 | 34 | 78 | 67.0 | NA | OA | NA | NA | NA | NA | NA |
| Matsuda | 118 | Old age and varus post-operative alignment negatively related to satisfaction | New KSS (40 points) | 2013 | Japan | Cross-sectional | 5 years | 375 | 64 | 311 | 71.0 | 26.0 | OA, RA, other | NA | Yes | Unknown (82% PS, 18% CR) | NA | NA |
| Matsumoto | 119 | Patient satisfaction exhibited positive correlations with joint component gap difference | New KSS (40 points) | 2017 | Japan | Cohort | 1 year | 35 | 6 | 29 | 75.5 | NA | OA | MPP | NA | E-motion floating platform mobile-bearing CR | NA | NA |
| Mayman | 120 | More patients were extremely satisfied with patellar resurfacing | 4 grades (extremely satisfied, satisfied, unsure, or disappointed) | 2003 | Canada | Randomised controlled trial | 2 years | 100 | 42 | 58 | 72 | NA | OA | NA | Yes and no | NA | Yes | NA |
| McLawhorn | 121 | Patients with reported allergies were less satisfied | 3 grades (somewhat to very satisfied, neither satisfied or dissatisfied, somewhat to very dissatisfied) | 2015 | USA | Cohort | 2 years | 257 | 119 | 138 | 67.5 | 30.1 | NA | NA | NA | Unknown (PS) | Yes | NA |
| Meftah | 122 | No significant difference between rotating platform and fixed bearing | VAS (0–10) | 2016 | USA | Cohort | 12.3 years | 55 | 16 | 24 | 54.3 | 31.8 | OA, RA, post-trauma OA | MPP | Yes | PFC Sigma (20 rotating platform, 34 fixed bearing) (PS) | Yes | NA |
| Meijerink | 123 | Patients with PFC prosthesis were more satisfied than those with CKS prosthesis | VAS (0–100) | 2011 | Netherlands | Randomised controlled trial | 5.6 years | 77 | 27 | 50 | 67.0 | 29.0 | OA, RA | MPP | No | PFC (fixed bearing) (CR), CKS (fixed bearing) (CR) | Yes | NA |
| Meijerink | 124 | There was no relation between surgeon’s pre-operative assessment of the difficulty or surgeon’s immediate post-operative satisfaction and patient’s satisfaction | VAS (0–100) | 2009 | Netherlands | Cohort | 1 year | 53 | 15 | 36 | 67.0 | NA | OA, RA | NA | NA | PFC, CKS | NA | NA |
| Merle-Vincent | 125 | Absence of complications, BMI less than 27, high radiological joint narrowing score, age greater or equal to 70 years and absence of depression positively related to satisfaction | 5 grades (0, 25, 50, 75, 100% of satisfaction) | 2011 | France | Cohort | 2 years | 264 | 78 | 186 | 75.0 | 28.4 | OA | NA | NA | NA | NA | NA |
| Miner | 126 |
(1) WOMAC pain score and WOMAC function score were positively related to satisfaction (2) Knee flexion angle, age, gender and BMI did not relate to satisfaction |
4 grades | 2003 | UK | Cohort | 12 months | 684 | 283 | 401 | 69.8 | 29.5 | OA | NA | NA | Kinemax | NA | NA |
| Mistry | 127 | Presence of altered sensation did not affect satisfaction | British Orthopaedic Association grading system & VAS (0–10) | 2005 | New Zealand | Cohort | 1 year | 29 | 8 | 21 | 72.7 | NA | NA | NA | NA | NA | NA | NA |
| Mont | 128 | Patient’s pre-operative activity level did not relate to satisfaction | VAS (0–10) | 2007 | USA | Cohort | 7 years | 144 | 44 | 70 | 70.0 | 29.0 | OA, RA, AVN | NA | NA | Duracon (CR) | NA | NA |
| Murphy | 129 | No difference between patients with femoral component implanted in 4 degrees flexion in the sagittal plane and those with femoral component implanted in a neutral position | NRS (0–10) | 2014 | Australia | Randomised controlled trial | 1 year | 40 | 15 | 25 | 70.3 | 30.5 | OA | MPP | No | Profix (CR) | NA | NA |
| Nakahara | 130 | Post-operative ability of climbing up or down a flight of stairs, getting into or out of a car, moving laterally (stepping to the side) and walking and standing effected on satisfaction | New KSS (questions 3, 4, 5 only) | 2015 | Japan | Cross-sectional | 5 years | 520 | 62 | 325 | 72.0 | NA | OA, RA, AVN | NA | NA | Unknown (82% PS, 18% CR) | NA | NA |
| Nakano | 131 | Use of CT-free navigation had no effect on satisfaction | New KSS (40 points) | 2013 | Japan | Cohort | 118 months | 27 | 3 | 24 | 71.5 | NA | OA | MPP | NA | PFC Sigma (PS) | NA | NA |
| Nam | 132 | Patients with metallic allergy were less satisfied | New KSS (40 points) | 2016 | USA | Cohort | Minimum 2 years | 589 | 226 | 363 | 62.3 | 32.9 | NA | NA | NA | NA | NA | NA |
| Nam | 133 |
(1) Female patients, patients from low-income households (< USD 25,000 annually) were less satisfied (2) Education level, employment status and using custom cutting guides, gender-specific prosthesis, high-flex prosthesis, rotating platform bearing or kinematic alignment technique had no effect on satisfaction |
Satisfied or not | 2014 | USA | Cross-sectional | 2.6 years | 661 | NA | NA | 54.3 | NA | OA | NA | NA | Vanguard | Yes | NA |
| Nam | 134 | Using custom cutting guides (signature) had no effect on satisfaction | Satisfied or not | 2016 | USA | Cohort | 3 years | 448 | 154 | 294 | 61.9 | NA | OA | Midvastus | Yes | Vanguard (fixed bearing) (CR) | Yes | NA |
| Narayan | 135 | Deep knee flexion did not relate to patient satisfaction after TKR (even in a population where squatting and sitting cross-legged are part of the normal lifestyle) | 5 grades (extremely satisfied, satisfied, neutral, unsatisfied, extremely unsatisfied) | 2009 | India | Cohort | 25.12 months | 36 | 10 | 17 | 58.7 | NA | OA | NA | NA | PFC, Genesis II (23 CR, 13 PS) | NA | NA |
| Nishio | 136 | Regarding intra-operative kinematic patterns, medial pivot group were more satisfied than non-medial pivot group | New KSS (40 points) | 2014 | Japan | Cross-sectional | 42 months | 40 | 8 | 32 | 73.0 | 25.6 | OA | Subvastus | Yes | PFC Sigma RP-F (mobile bearing) (PS) | NA | NA |
| Noble | 137 | Age less than 60, absence of residual symptoms, fulfilment of expectations and absence of functional impairment positively related to satisfaction | Total Knee Function Questionnaire | 2006 | USA | Cross-sectional | Minimum 1 year | 253 | 105 | 148 | 68.1 | NA | OA, RA, post-trauma OA | NA | NA | NA | NA | NA |
| Nunez | 138 | Post-operative WOMAC score related to satisfaction | 5 grades | 2009 | Spain | Cohort | 7 years | 112 | 26 | 86 | 67.3 | 30.7 | OA | NA | NA | NA | NA | NA |
| Nunley | 139 | In CR TKR, rotating platform, gender-specific design and high flex design had no effect on satisfaction (compared with conventional CR prosthesis) | Satisfied or not | 2015 | USA | Cohort | 2.6 years | 527 | 196 | 331 | 55.6 | NA | OA, post-trauma OA, AVN | NA | NA | Vanguard (CR), unknown (rotating platform (CR, PS), gender-specific (CR), high-flex (CR)) | NA | NA |
| Park | 140 | In simultaneous bilateral TKR, there was no difference between cemented and cementless TKR | VAS (0–10) | 2011 | South Korea | Randomised controlled trial | 13.6 years | 100 | 11 | 39 | 58.4 | 26.6 | OA, inflammatory disease | MPP | Yes | NexGen (CR) | Yes and no | NA |
| Parsley | 141 | No difference between PS and ultra-congruent prosthesis | Total Knee Function Questionnaire | 2006 | USA | Cohort | Minimum 2 years | 209 | 61 | 148 | 67.9 | 29.9 | NA | Midvastus | NA | Sulzer Apollo (PS), Sulzer NK-II Ultra-congruent | Yes | NA |
| Perez-Prieto | 142 | Pre-operative depression had no effect on satisfaction | Satisfied or not | 2014 | Spain | Cohort | 1 year | 716 | 550 | 166 | 72.5 | 31.4 | NA | NA | NA | NA | NA | NA |
| Pulavarti | 143 | Patients with patella denervation were more satisfied | 4 grades (excellent, good, fair, poor) | 2014 | UK | Randomised controlled trial | 26.4 months | 126 | 58 | 68 | 69.9 | 29.2 | OA | MPP | No | Unknown (CR) | NA | NA |
| Ranawat | 144 | No difference between fixed bearing and rotating platform | VAS (0–10) | 2004 | Italy | Cohort | 46 months | 52 | 9 | 17 | 74.0 | NA | OA, RA | NA | Yes | PFC Sigma (mobile bearing and fixed bearing) (PS) | Yes | NA |
| Ranawat | 145 | No difference between Attune PS and PFC Sigma PS | VAS (0–10) | 2016 | USA | Cohort | 2 years | 200 | 62 | 138 | 70.6 | 29.3 | OA | MPP | Yes | 100 Attune (61 fixed bearing, 39 rotating platform) (PS), 100 PFC Sigma (83 fixed bearing, 17 rotating platform) (PS) | Yes | NA |
| Razmjou | 146 | Patients with neuropathic pain were less satisfied | 6 grades (very satisfied, somewhat satisfied, a little bit satisfied, a little bit dissatisfied, somewhat dissatisfied, very dissatisfied) | 2015 | Netherlands | Cross-sectional | 5 years | 63 | 16 | 47 | 67.0 | NA | OA | NA | NA | NA | NA | NA |
| Roberts | 147 |
(1) Male patients and patients with OA were less satisfied (2) Age had no effect on satisfaction |
Satisfied or not | 2007 | UK | Cross-sectional | 15 years | 912 | NA | NA | 69.5 | NA | OA, RA, other | NA | Yes and No | Freeman-Samuelson, Insall Burstein II, Kinematic, Kinemax, Omnifit, PFC | NA | NA |
| Roberts | 148 | Patients with patellar resurfacing were more satisfied than those without it | 5 grades | 2015 | USA | Randomised controlled trial | 10 years | 327 | 170 | 157 | 70.6 | 29.2 | OA | MPP | Yes and No | PFC Sigma (fixed bearing) (CR) | NA | Spinal |
| Robertsson | 149 |
(1) Women gender, not chronic pain, old age and non-patellar resurfacing negatively related to satisfaction (2) Satisfaction rate was RA > OA > post-trauma arthritis > AVN |
4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2000 | Sweden | Cross-sectional | 6 years | 27372 | NA | NA | 71.0 | NA | OA RA, ON, other | NA | Yes and no | NA | NA | NA |
| Schlegel | 150 | Patients with surface-cemented tibial component were more satisfied than patients with fully cemented tibial component | 5 grades | 2015 | Germany | Cohort | 11.4 years | 67 | 4 | 63 | 66.0 | NA | RA, OA | MPP | Yes | PFC (fixed bearing) (CR) | Yes (25 surface only, 42 fully cemented) | NA |
| Schnurr | 151 | Patients with mild to moderate OA were less satisfied | 5 grades (completely satisfied, partially satisfied, neutral, partially unsatisfied, completely unsatisfied) | 2013 | Germany | Cohort | 2.8 years | 996 | 338 | 658 | 68.0 | NA | OA | MPP | NA | PFC Sigma, NexGen high-flex | NA | NA |
| Schuster | 152 | Post-operative anterior–posterior stability had no effect on satisfaction | VAS (0–10) | 2011 | Switzerland | Cohort | 47.2 months | 127 | 32 | 80 | 70.7 | 29.3 | NA | NA | NA | balanSys (fixed bearing) (CR) | NA | NA |
| Scott | 153 | Poor OKS, poor pre-operative SF-12 mental component score, depression, back pain and pain in other joints negatively related to satisfaction | 4 grades (very satisfied, satisfied, unsure, dissatisfied) | 2010 | UK | Cohort | 12 months | 1141 | 515 | 698 | 70.1 | NA | OA | NA | No | PFC Sigma (CR), Kinemax (CR), Triathlon (CR) | NA | NA |
| Scott | 154 | In staged bilateral TKR, satisfaction on the first side was not always translated into that of the other side | 4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2014 | UK | Cohort | 12 months | 70 | 30 | 40 | 71.7 | NA | OA, inflammatory disease | NA | NA | NA | NA | NA |
| Scott | 155 | No difference between TKR for primary OA and post-trauma (tibial plateau fracture) OA | 4 grades (very satisfied, satisfied, uncertain, dissatisfied) | 2015 | UK | Cohort | Minimum 5 years | 124 | 32 | 92 | 66.0 | NA | OA, post-trauma OA (tibial plateau fracture) | MPP | NA | Unknown (CR) | Yes | NA |
| Scott | 156 | Poor pre-operative OKS, poor improvement in OKS and post-operative stiffness (in patients under 55 years) independently predicted dissatisfaction | 4 grades (very satisfied, satisfied, unsure, dissatisfied) | 2016 | UK | Cohort | 12 months | 177 | 78 | 99 | 50.0 | 34.0 | OA, post-trauma OA, inflammatory disease | NA | No | 109 Triathlon (CR), 63 PFC Sigma (CR), 4 Kinemax (CR), 1 hinged implant | NA | NA |
| Senioris | 157 | Patellar congruence had no effect in mobile-bearing TKR | 4 grades (excellent, good, fair, poor) | 2016 | France | Cohort | 14 months | 30 | 8 | 22 | 68.8 | 31.2 | OA | Midvastus | No | HLS KneeTec (mobile bearing) (PS) | No | General |
| Seo | 158 | Octogenarians had same level of satisfaction as young patients | NRS (0–10) | 2015 | South Korea | Cohort | 1 year | 757 | 68 | 689 |
81.9 G1 67.7 G2 |
28.8 | OA | MPP | Yes | NA | Yes | NA |
| Sharkey | 159 | Combination of post-operative noise and numbness negatively related to satisfaction | 5 grades (completely satisfied, partially satisfied, neutral, partially unsatisfied, completely unsatisfied) | 2011 | USA | Cross-sectional | 15 months | 49 | 24 | 25 | 68.0 | 31.6 | OA | NA | NA | NA | NA | NA |
| Shukla | 160 | No difference between MPP and midvastus approach | New KSS (40 points) | 2016 | India | Cohort | 1 year | 52 | 22 | 30 | 61.4 | NA | NA | MPP, midvastus | NA | Genesis II (PS) | NA | NA |
| Singisetti | 161 | No difference between navigation (articular surface mounted (ASM) navigation technique) and conventional technique | 4 grades (very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied) | 2015 | UK | Cohort | 2 years | 355 | 151 | 204 | 67.3 | 30.0 | NA | NA | NA | Triathlon | NA | NA |
| Stickles | 162 | BMI did not relate to satisfaction | 5 grades (very satisfied, somewhat satisfied, neutral, somewhat dissatisfied, very dissatisfied) | 2001 | USA | Cross-sectional | 1 year | 1011 | 374 | 637 | 69.9 | 31.2 | OA | NA | NA | NA | NA | NA |
| Sun | 163 | Patelloplasty is better than traditional patellar management | Original questionnaire | 2012 | China | Cohort | 55 months | 152 | 72 | 80 | 64.7 | NA | OA | MPP | No | PFC Sigma | Yes | NA |
| Thambiah | 164 | Post-operative WOMAC function scores, post-operative WOMAC final scores, improvements in the physical health component of the SF-36 score, and expectations being met were the factors which effect satisfaction | 5 grades (extremely satisfied, satisfied, neutral, dissatisfied, extremely dissatisfied) | 2015 | Singapore | Cohort | 1 year | 110 | 32 | 78 | 64.0 | 26.7 | OA | NA | NA | NA | NA | NA |
| Thomsen | 165 | No difference between standard CR prosthesis and high flexion PS prosthesis | VAS (0–10) | 2013 | Denmark | Randomised controlled trial | 1 year | 66 | 14 | 19 | 67.2 | 29.4 | OA, RA | MPP | Yes | AGC (CR), NexGen LPS-flex (PS) | Yes | Combined (spinal + epidural) |
| Thomsen | 166 | No difference between gender-specific TKR and LPS-flex | VAS (0–10) | 2011 | Denmark | Randomised controlled trial | 1 year | 48 | 0 | 24 | 66 | 29.3 | OA | MPP | NA | Gender Solutions high-flex prosthesis in one knee and a NexGen LPS-flex prosthesis in the other knee | Yes | Spinal |
| Tsukiyama | 167 |
(1) Medial joint laxity made patients less satisfied (2) Lateral joint laxity did not affect satisfaction |
New KSS (40 points) | 2017 | Japan | Cross-sectional | 57 months | 50 | 10 | 31 | 73 | NA | OA | NA | NA | NA | NA | NA |
| van der Ven | 168 | No difference between high-flex prosthesis and conventional prosthesis | VAS (0–10) | 2017 | Netherlands | Randomised controlled trial | 1 year | 48 | 25 | 23 | 65 | 31.5 | OA, RA | NA | NA | NA | NA | NA |
| van de Groes | 169 | Patients with femoral component medial malpositioned more than 5 mm were more satisfied | NRS (0–10) | 2014 | Netherlands | Cross-sectional | 105.6 months | 40 | NA | NA | 75.7 | 31.0 | OA, RA | NA | No | LCS, PFC | NA | NA |
| van Houten | 170 | Patients with post-operative anterior knee pain were less satisfied | VAS (0–10) | 2016 | Netherlands | Cohort | 10 years | 60 | 15 | 45 | 63.7 | NA | OA | NA | No | balanSys (43 fixed bearing, 17 AP-glide bearing) (CR) | NA | NA |
| Vissers | 171 | Pre-operative functional capacity and level of daily activity had no effect on satisfaction | 5 grades (very satisfied, moderately satisfied, neutral, moderately dissatisfied, very dissatisfied) | 2010 | Netherlands | Cross-sectional | 6 months | 44 | 20 | 24 | 63.5 | 30.8 | OA | NA | NA | Genesis II | NA | NA |
| Von Keudell | 172 | Amongst 3 age groups (54 or younger, 55 to 64, 65 or older), 65 or older group tended to be more satisfied than others | NRS (0–10) | 2014 | USA | Cohort | 6.4 years | 245 | 80 | 165 | 62.6 | NA | OA | NA | NA | PFC Sigma | NA | NA |
| Wang | 173 | No difference between post-operative continuous femoral nerve block and patient-controlled epidural analgesia | 4 grades (excellent, good, general, poor) | 2015 | China | Randomised controlled trial | 12 months | 162 | NA | NA | NA | NA | NA | NA | NA | NA | NA | General |
| Waters | 174 | Patients with patellar resurfacing were more satisfied than those without it | 4 grades | 2003 | UK | Randomised controlled trial | 5.3 years | 474 | 157 | 233 | 69.1 | NA | OA, RA, inflammatory disease | MPP | Yes and no | PFC | NA | General |
| White | 175 | Amongst custom prosthesis (iTotal, cemented, CR), PFC Sigma (cemented, PS, fixed bearing) and PFC Sigma (non-cemented, CR, rotating platform), patients with custom prostheses were worst in satisfaction | VAS (0–10) | 2016 | USA | Cohort | 2 years | 74 | 31 | 43 | 52.2 | NA | OA | MPP | NA | iTotal (CR), PFC Sigma (rotating platform) (CR), PFC Sigma (fixed bearing) (PS) | NA | NA |
| Williams | 176 |
(1) Knee Society pain score, OKS, SF-12 (physical/mental), and knee flexion angle positively related to satisfaction (2) Age, BMI, length of stay, gender, diagnosis had no effect on satisfaction |
4 grades (very happy, happy, OK (not perfect), never happy) | 2013 | UK | Cross-sectional | 12 months | 486 | 172 | 314 | 70.9 | 31.1 | OA, RA | NA | NA | LCS (mobile bearing), ROCC (mobile bearing) | NA | NA |
| Wylde | 177 | No difference between fixed bearing and mobile bearing | 4 grades | 2008 | UK | Randomised controlled trial | 2 years | 250 | 110 | 132 | 68.0 | NA | OA, RA | NA | Yes and no | Kinemax plus (fixed bearing, mobile bearing) | NA | NA |
| Yagishita | 178 | Patients with high flexion PS prosthesis were more satisfied than those with high flexion CR prosthesis in simultaneous bilateral TKR | VAS (0–100) | 2012 | Japan | Randomised controlled trial | 5 years | 58 | 4 | 25 | 74.3 | 26.3 | OA | NA | NA | NexGen CR-flex, NexGen LPS-flex | NA | NA |
| Yeung | 179 | There was no relation between BMI and satisfaction | VAS (0–10) | 2011 | Australia | Case–control | 9.2 years | 535 | 230 | 305 | 71.0 | 28.0 | OA | NA | NA | NA | No | NA |
| Zha | 180 | No difference between patients with lateral retinacular release and those without it | 4 grades (very satisfied, satisfied, unsure, dissatisfied) | 2014 | China | Randomised controlled trial | 18 months | 139 | 46 | 93 | 68.2 | 24.0 | OA | MPP | No | Gemini MK II (mobile bearing) | Yes | General |
| Zha | 181 | Chondromalacia patellae did not influence satisfaction | 4 grades (very satisfied, satisfied, unsure or dissatisfied) | 2017 | China | Case series | 36 months | 290 | 123 | 167 | 67.7 | 25.0 | OA | MPP | No | LCS mobile bearing | Yes | NA |
Age are shown in years (mean). Body mass index are shown in kg/m2 (mean). Full information of the studies are listed in Electronic Supplementary Material 1
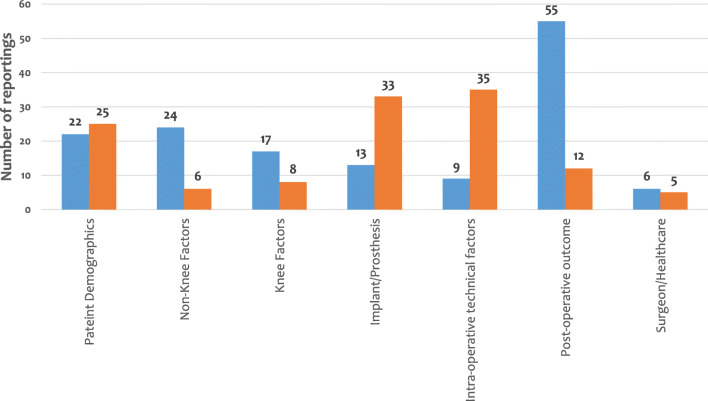
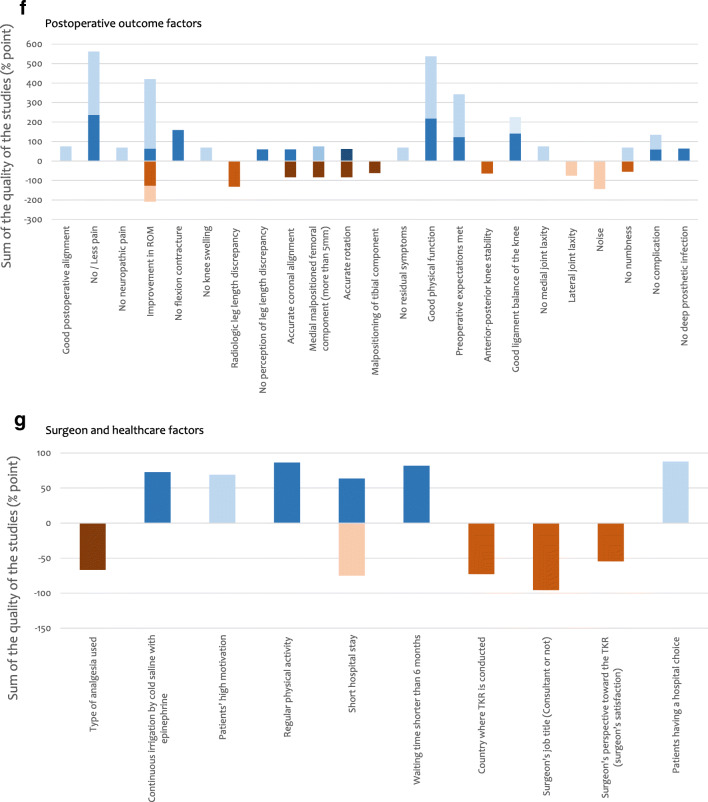
From all these studies, we found 98 factors, which could potentially affect patient satisfaction and these were then categorised into seven groups as follows:
Patient demographics
Non-knee factors
Knee factors
Factors relating to implants/prostheses
Intra-operative technical factors
Post-operative outcome factors
Surgeon and healthcare factors
All the 98 factors as well as scales/scores which were reported to relate to patient satisfaction are summarised in Table 4. Details of the results in each group are described in Electronic Supplementary Material 3. The number of reportings for each group is presented in Fig. 2, and the methods used to measure satisfaction are shown in Table 5.
Table 4.
Potential factors for patient satisfaction following primary total knee replacement (TKR) with their groups
| Factors | Sub-factors for satisfaction | Serial number of reporting studies |
|---|---|---|
| 1. Patient demographics (47) | ||
| Age (17) | Young | 95, 118, 137, 149 (4) |
| Old | 9, 112, 125, 172 (4) | |
| Not-FACTOR | 1, 7, 40, 47, 72, 126, 147, 158, 176 (9) | |
| Gender (10) | Male | 9, 14, 133, 149 (4) |
| Female | 147 (1) | |
| Not-FACTOR | 7, 40, 72, 126, 176 (5) | |
| Body mass index (BMI), weight (12) | Normal BMI | 10, 23, 62, 98, 125 (5) |
| Not-FACTOR | 7, 47, 72, 126, 162, 176, 179 (7) | |
| Ethnicity (2) | Caucasian > African American | 71 (1) |
| Not-FACTOR | 14 (1) | |
| Income (2) | Annual income > 25,000 USD | 14, 133 (2) |
| Social background (education, employment, insurance) (4) | High education | 62 (1) |
| Not-FACTOR | 14, 80, 133 (3) | |
| 2. Non-knee factors (30) | ||
| Back pain (3) | No low back pain | 34, 42, 153 (3) |
| Allergy (2) | No allergy | 121, 132 (2) |
| Fibromyalgia (1) | No fibromyalgia | 15 (1) |
| Problems in other joints (2) | No problem in other joints | 117, 153 (2) |
| General condition (1) | ASA 2 or worse | 9 (1) |
| Comorbidity (1) | No medical comorbidity | 7 (1) |
| Use of narcotics (1) | No use of narcotics | 51 (1) |
| Diabetes mellitus (1) | Not-FACTOR | 35 (1) |
| Generalised joint laxity (1) | Not-FACTOR | 102 (1) |
| Mental health anxiety, depression and personality traits (15) | No mental problem | 3, 5, 7, 16, 17, 23, 33, 47,49, 54, 55, 125, 153 (13) |
| Not-FACTOR | 94, 142 (2) | |
| Pre-operative activity level (2) | Not-FACTOR | 128, 171 (2) |
| 3. Knee factors (25) | ||
| Pre-operative stiff knee (1) | No stiff knee | 156 (1) |
| Pre-operative knee pain (4) | No pain at rest | 22, 73 (2) |
| Chronic pain | 149 (1) | |
| No movement-elicited pain | 73 (1) | |
| History of past knee surgery (ACL reconstruction, HTO) (1) | Not-FACTOR | 106 (1) |
| Satisfaction on the first side (in bilateral TKR) (1) | Not-FACTOR | 154 (1) |
| Diagnosis (7) | RA > OA | 24 (1) |
| Not OA | 147 (1) | |
| RA > OA > post-trauma > AVN | 149 (1) | |
| Not-FACTOR | 7, 56, 155, 176 (4) | |
| Degree of degeneration (4) | Severe pre-operative radiographic degenerative change | 71, 79, 125, 151 (4) |
| Chondromalacia patellae (1) | Not-FACTOR | 181 (1) |
| Patellar congruence (1) | Not-FACTOR | 157 (1) |
| Intact ACL in CR-TKR (1) | No intact ACL | 70 (1) |
| Knee extensor strength (1) | Great knee extensor strength | 53 (1) |
| Intra-operative joint force (1) | Greater intra-operative force in the medial compartment | 74 (1) |
| Intra-operative kinematic pattern of the knee (1) | Medial pivot kinematic pattern | 136 (1) |
| Patient’s perspective (1) | High flexion activities | 89 (1) |
| 4. Factors related to implants/prostheses (46) | ||
| Specific prosthesis (7) | Triathlon > Kinemax | 60 (1) |
| Triathlon > Kinemax Plus | 46 (1) | |
| PFC > CKS | 123 (1) | |
| Vega, Genesis II > E.motion | 75 (1) | |
| NexGen > AGC | 114 (1) | |
| Not-FACTOR | 81, 145 (2) | |
| Cruciate-retaining/posterior-stabilised/ultra-congruent design (8) | PS > CR | 178 (1) |
| Not-FACTOR | 14, 18, 44, 78, 115, 141, 165 (7) | |
| Design of the bearing (insert) (12) | Mobile-bearing insert | 32, 82, 91, 110 (4) |
| Rotating mobile > floating mobile | 83 (1) | |
| Not-FACTOR | 14, 63, 122, 133, 139, 144, 177 (7) | |
| Single radius prosthesis/multi-radius prosthesis (2) | Single radius > multi-radius | 43 (1) |
| Not-FACTOR | 65 (1) | |
| Use/type/number of stem (1) | Not-FACTOR | 12 (1) |
| Highly cross-linked polyethylene (1) | Not-FACTOR | 93 (1) |
| Material of femoral components (1) | Not-FACTOR | 67 (1) |
| Gender-specific design (6) | Not-FACTOR | 14, 84, 88, 133, 139, 166 (6) |
| High-flexion design (7) | Not-FACTOR | 14, 20, 31, 87, 133, 139, 168 (7) |
| Customised prosthesis (1) | Non-customised (= off-the-shelf) prosthesis | 175 (1) |
| 5. Intra-operative technical factors (44) | ||
| Approach, incision (4) | Lateral subvastus approach | 66 (1) |
| Not-FACTOR | 6, 9, 160 (3) | |
| Cement technique (4) | Surface-cemented > fully cemented (for tibial component) | 150 (1) |
| Not-FACTOR | 52, 92, 140 (3) | |
| Kinematic alignment technique (1) | Not-FACTOR | 133 (1) |
| Gap balancing/measured resection technique (1) | Not-FACTOR | 41 (1) |
| Navigation/patient-specific instrument/custom cutting guide/robotic surgery (13) | Using a navigation system | 104 (1) |
| Not-FACTOR | 19, 39, 61, 96, 97, 99, 108, 109, 131, 133, 134, 161 (12) | |
| Patellar resurfacing (13) | Patellar resurfacing | 120, 148, 149, 174 (4) |
| Not-FACTOR | 4, 8, 13, 25, 26, 27, 69, 85, 114 (9) | |
| Lateral retinacular release (1) | Not-FACTOR | 180 (1) |
| Minimally invasive surgery (MIS) (1) | Not-FACTOR | 64 (1) |
| Periarticular injection with corticosteroid (1) | Not-FACTOR | 103 (1) |
| Patellar treatment (in cases without patellar resurfacing) (2) | Patellar denervation | 143 (1) |
| Patelloplasty | 163 (1) | |
| Use of a tourniquet (1) | Not-FACTOR | 9 (1) |
| Removal of fat pad (1) | Not-FACTOR | 9 (1) |
| One-stage/two-stage bilateral TKR (1) | Not-FACTOR | 116 (1) |
| 6. Post-operative outcome factors (55) | ||
| Knee alignment (1) | Good post-operative alignment | 118 (1) |
| Pain (8) | No/less pain | 2, 3, 7, 9, 29, 48, 170 (7) |
| No neuropathic pain | 146 (1) | |
| Range of motion (9) | Improvement in ROM | 3, 47, 59, 72, 86, 176 (6) |
| Not-FACTOR | 45, 126, 135 (3) | |
| Flexion contracture (2) | No flexion contracture | 32, 57 (2) |
| Knee swelling (1) | No knee swelling | 47 (1) |
| Radiologic leg length discrepancy (2) | Not-FACTOR | 30, 90 (2) |
| Perception of leg length discrepancy (1) | No perception of leg length discrepancy | 30 (1) |
| Malpositioning of femoral component (4) | Accurate coronal alignment | 68 (1) |
| Medial malpositioned femoral component (more than 5 mm) | 169 (1) | |
| Accurate rotation | 77 (1) | |
| Not-FACTOR | 129 (1) | |
| Malpositioning of tibial component (1) | Not-FACTOR | 77 (1) |
| Residual symptom (1) | No residual symptoms | 137 (1) |
| Physical function (7) | Good physical function | 7, 11, 36, 48, 117, 130, 137 (7) |
| Degree of expectation met (5) | Pre-operative expectations met | 21, 22, 40, 137, 164 (5) |
| Anterior–posterior knee stability (1) | Not-FACTOR | 152 (1) |
| Ligament balance (3) | Good ligament balance of the knee | 58, 76, 119 (3) |
| Medial joint laxity (1) | No medial joint laxity | 167 (1) |
| Lateral joint laxity (1) | Not-FACTOR | 167 (1) |
| Noise (2) | Not-FACTOR | 100, 159 (2) |
| Altered sensation (2) | No numbness | 159 (1) |
| Not-FACTOR | 127 (1) | |
| Complication (3) | No complication | 22, 125 (2) |
| No deep prosthetic infection | 5 (1) | |
| 7. Surgeon and healthcare factors (11) | ||
| Type of analgesia used (1) | Not-FACTOR | 173 (1) |
| Post-operative irrigation (1) | Continuous irrigation by cold saline with epinephrine | 105 (1) |
| Post-operative rehabilitation (2) | Patients’ high motivation | 47 (1) |
| Regular physical activity | 28 (1) | |
| Length of hospital stay (2) | Short hospital stay | 5 (1) |
| Not-FACTOR | 176 (1) | |
| Waiting time before TKR (1) | Shorter than 6 months | 111 (1) |
| Country where TKR is conducted (1) | Not-FACTOR | 107 (1) |
| Surgeon’s job title (consultant or not) (1) | Not-FACTOR | 9 (1) |
| Surgeon’s perspective towards the TKR (surgeon’s satisfaction) (1) | Not-FACTOR | 124 (1) |
| Hospital choice (1) | Patients having a hospital choice | 113 (1) |
| (Relating scores/scales) (17) | ||
| Relation (+) | WOMAC score | 86, 126, 138, 164 (4) |
| Oxford Knee Score | 37, 38, 68, 153, 156, 176 (6) | |
| Knee Society Score | 72, 176 (2) | |
| SF-12 score | 153, 176 (2) | |
| SF-36 score | 164 (1) | |
| Control Preference Scale | 50 (1) | |
| Relation (−) | New Knee Society Score | 101 (1) |
Reporting studies are described using serial numbers in Table 3. The number of each category is shown in parentheses
Not-FACTOR ‘it is a factor which does NOT relate to patient satisfaction’
Fig. 2.
Number of reportings in seven groups of factors for patient satisfaction following total knee replacement. Blue bar means FACTOR (‘it is a factor for patients’ satisfaction’) and orange bar means Not-FACTOR (‘it is a factor which does NOT relate to patients’ satisfaction’)
Table 5.
Measuring methods for patients’ satisfaction
| 2 Grades (satisfied or not) (15) | |
| 12, 13, 14, 48, 52, 54, 69, 74, 81, 98, 133, 134, 139, 142, 147 | |
| 3 Grades (5) | |
| 9, 70, 71, 73, 121 | |
| 4 Grades (45) | |
| 2, 3, 4, 5, 10, 15, 29, 33, 34, 35, 36, 37, 38, 39, 40, 46, 57, 59, 60, 72, 83, 86, 89, 91, 107, 113, 115, 116, 117, 120, 126, 143, 149, 153, 154, 155, 156, 157, 161, 173, 174, 176, 177, 180, 181 | |
| 5 Grades (36) | |
| 7, 11, 16, 17, 18, 20, 21, 22, 30, 31, 41, 43, 45, 47, 49, 56, 58, 61, 62, 68, 85, 90, 94, 95, 104, 111, 125, 135, 138, 148, 150, 151, 159, 162, 164, 171 | |
| 6 Grades (6) | |
| 6, 19, 106, 108, 109, 146 | |
| Numerical Rating Scale (NRS) (0–10) (8) | |
| 50, 63, 79, 80, 129, 158, 169, 172 | |
| Visual Analogue Scale (VAS) (0–10) (28) | |
| 23, 28, 42, 64, 65, 66, 84, 87, 88, 96, 102, 103, 105, 110, 112, 122, 127, 128, 140, 144, 145, 152, 165, 166, 168, 170, 175, 179 | |
| VAS (0–100) (11) | |
| 8, 24, 55, 82, 92, 93, 97, 114, 123, 124, 178 | |
| New Knee Society Score (15) | |
| 32, 53, 76, 77, 78, 100, 101, 118, 119, 130, 131, 132, 136, 160, 167 | |
| British Orthopaedic Association grading system (4) | |
| 1, 67, 75, 127 | |
| Total Knee Function Questionnaire (3) | |
| 44, 137, 141 | |
| Authors’ original questionnaire (5) | |
| 25, 26, 27, 99, 163 | |
| Unclear (1) | |
| 51 |
Studies are described using serial numbers in Table 3. The number of studies in each group is shown in parentheses
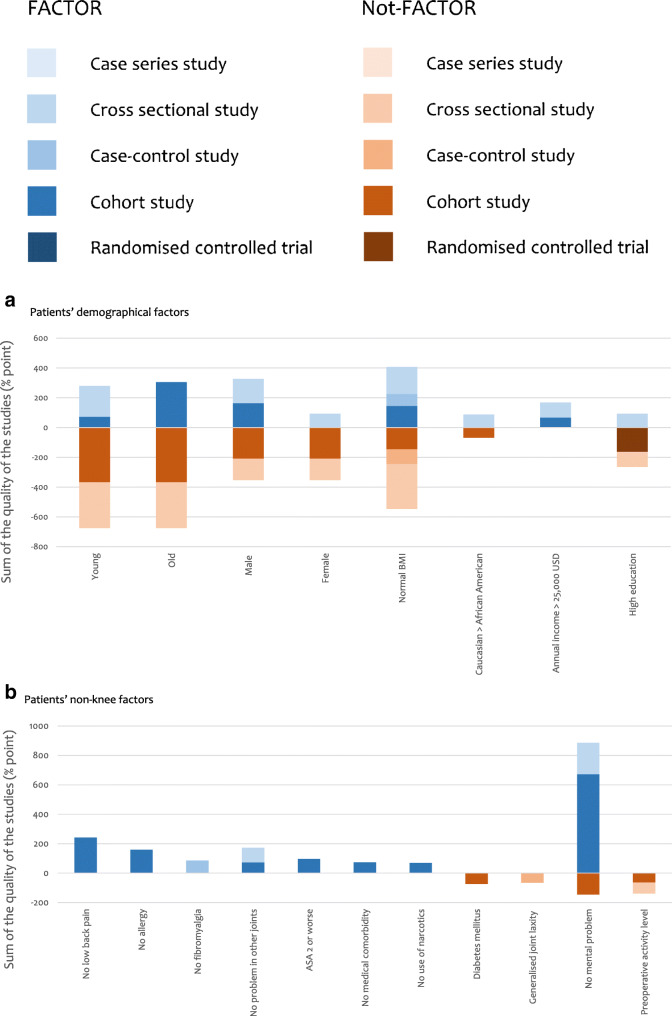
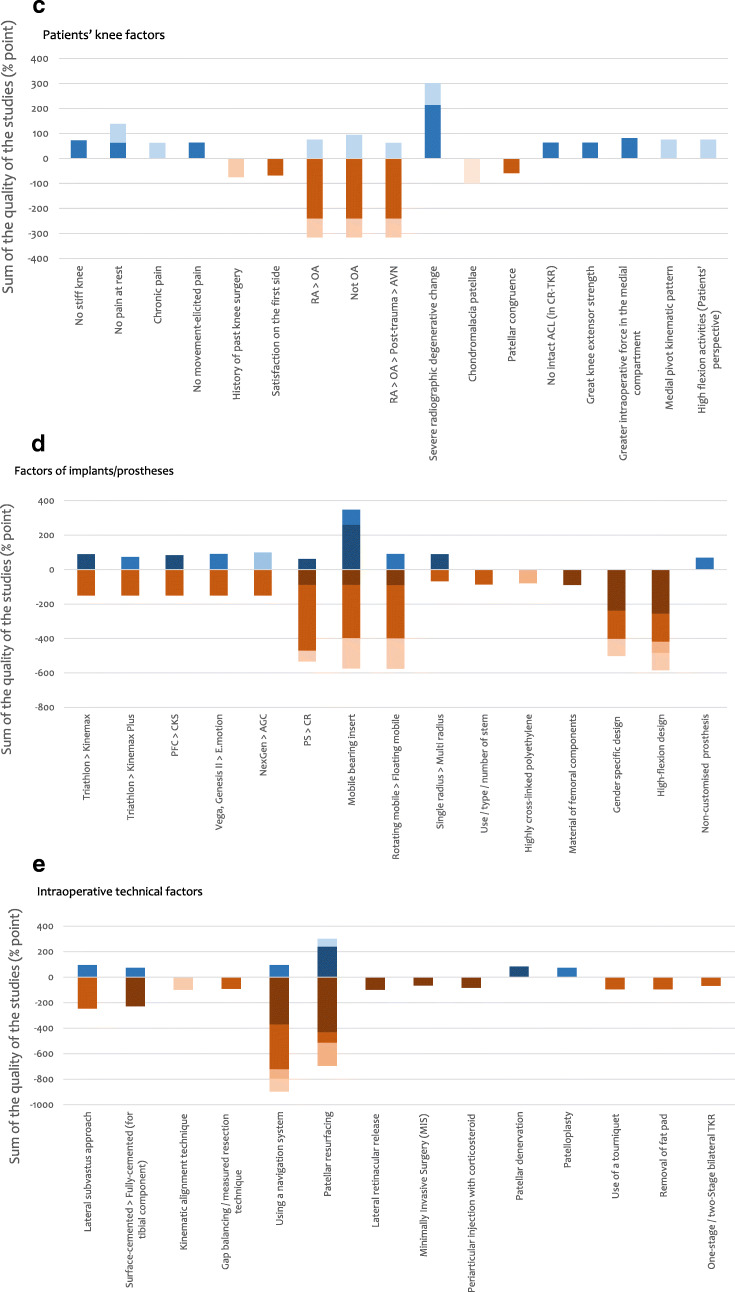
The quality of all the 181 studies was assessed and the results are shown in Tables 6, 7, 8, 9 and 10. The strength of each factor was described using the sum of percentage in each type of study (RCT, cohort study, case–control study, cross-sectional study and case series) (Fig. 3). RCTs were considered to be the strongest (deep colour in Fig. 3) and this was followed by cohort study, case–control study and cross-sectional study, respectively. Case series was considered to be the weakest (light colour in Fig. 3).
Table 6.
Results of quality assessment of 181 studies—cohort studies: 93 studies. The Joanna Briggs Institute Critical Appraisal Checklist is used
|
Scoring: Yes = 2 / Unclear = 1 / No = 0 / NA = not applicable Q1: Were the two groups similar and recruited from the same population? Q2: Were the exposures measured similarly to assign people to both exposed and unexposed groups? Q3: Was the exposure measured in a valid and reliable way? Q4: Were confounding factors identified? Q5: Were strategies to deal with confounding factors stated? Q6: Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)? Q7: Were the outcomes measured in a valid and reliable way? Q8: Was the follow-up time reported and sufficient to be long enough for outcomes to occur? Q9: Was follow-up complete, and if not, were the reasons to lose to follow-up described and explored? Q10: Were strategies to address incomplete follow-up utilised? Q11: Was appropriate statistical analysis used? | |||||||||||||
| Study (serial no.) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Total ( /22) | % |
| 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 19 | 86.4 |
| 5 | 1 | 1 | 2 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 14 | 63.6 |
| 6 | 2 | 2 | 1 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 18 | 81.8 |
| 7 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 16 | 72.7 |
| 10 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 21 | 95.5 |
| 11 | 0 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 14 | 63.6 |
| 12 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 19 | 86.4 |
| 14 | 0 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 15 | 68.2 |
| 16 | 0 | 0 | 2 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | 12 | 54.5 |
| 17 | 0 | 0 | 2 | 0 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 13 | 59.1 |
| 18 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | 1 | 16 | 72.7 |
| 23 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 19 | 86.4 |
| 28 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 19 | 86.4 |
| 30 | 0 | 1 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 13 | 59.1 |
| 32 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 19 | 86.4 |
| 33 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 0 | 2 | 16 | 72.7 |
| 34 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 20 | 90.9 |
| 35 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 0 | 2 | 16 | 72.7 |
| 36 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 1 | 1 | 2 | 18 | 81.8 |
| 37 | 0 | 2 | 2 | 0 | 0 | 1 | 2 | 2 | 2 | 0 | 2 | 13 | 59.1 |
| 39 | 2 | 2 | 2 | 0 | 0 | 1 | 2 | 2 | 2 | 0 | 2 | 15 | 68.2 |
| 40 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 14 | 63.6 |
| 41 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 20 | 90.9 |
| 42 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 17 | 77.3 |
| 44 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 19 | 86.4 |
| 46 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 49 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 16 | 72.7 |
| 50 | 0 | 2 | 2 | 0 | 0 | 1 | 2 | 2 | 1 | 1 | 2 | 13 | 59.1 |
| 51 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 53 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 14 | 63.6 |
| 54 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 56 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 20 | 90.9 |
| 57 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 58 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 59 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 14 | 63.6 |
| 65 | 2 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 15 | 68.2 |
| 66 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 21 | 95.5 |
| 68 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 70 | 0 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 14 | 63.6 |
| 73 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 14 | 63.6 |
| 74 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 18 | 81.8 |
| 75 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 20 | 90.9 |
| 79 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 21 | 95.5 |
| 80 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 21 | 95.5 |
| 81 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 1 | 0 | 0 | 1 | 12 | 54.5 |
| 83 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 20 | 90.9 |
| 85 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 18 | 81.8 |
| 90 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 94 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 95 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 99 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 101 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 104 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 21 | 95.5 |
| 105 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 107 | 0 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 111 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 18 | 81.8 |
| 112 | 1 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 15 | 68.2 |
| 115 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 19 | 86.4 |
| 116 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 119 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 121 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 17 | 77.3 |
| 122 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 124 | 0 | 1 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 12 | 54.5 |
| 125 | 0 | 2 | 1 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 13 | 59.1 |
| 126 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 16 | 72.7 |
| 127 | 1 | 2 | 2 | 0 | 0 | 2 | 2 | 1 | 1 | 0 | 1 | 12 | 54.5 |
| 128 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 1 | 14 | 63.6 |
| 131 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 1 | 15 | 68.2 |
| 132 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 18 | 81.8 |
| 134 | 1 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 1 | 14 | 63.6 |
| 135 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 1 | 12 | 54.5 |
| 138 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 18 | 81.8 |
| 139 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 21 | 95.5 |
| 141 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 142 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 144 | 2 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 17 | 77.3 |
| 145 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 21 | 95.5 |
| 150 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 151 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 152 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 14 | 63.6 |
| 153 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 154 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 15 | 68.2 |
| 155 | 1 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 17 | 77.3 |
| 156 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 157 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 158 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 160 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 161 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 17 | 77.3 |
| 163 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 16 | 72.7 |
| 164 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 13 | 59.1 |
| 170 | 0 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 0 | 2 | 15 | 68.2 |
| 172 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 18 | 81.8 |
| 175 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 1 | 15 | 68.2 |
Studies are described using serial numbers in Table 3
Table 7.
Results of quality assessment of 181 studies—case–control studies: 9 studies. The Joanna Briggs Institute Critical Appraisal Checklist is used
|
Scoring: Yes = 2 / Unclear = 1 / No = 0 / NA = not applicableQ1: Were the groups comparable other than the presence of disease in cases or the absence of disease in controls? Q2: Were cases and controls matched appropriately? Q3: Were the same criteria used for identification of cases and controls? Q4: Was exposure measured in a standard, valid and reliable way? Q5: Was exposure measured in the same way for cases and controls? Q6: Were confounding factors identified? Q7: Were strategies to deal with confounding factors stated? Q8: Were outcomes assessed in a standard, valid and reliable way for cases and controls? Q9: Was the exposure period of interest long enough to be meaningful? Q10: Was appropriate statistical analysis used? | ||||||||||||
| Study (serial no.) | Q1 | 1. Q2 | 2. Q3 | 3. Q4 | 4. Q5 | 5. Q6 | 6. Q7 | 7. Q8 | 8. Q9 | 9. Q10 | Total ( /20) | % |
| 15 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 17 | 85.0 |
| 20 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 2 | 13 | 65.0 |
| 69 | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 16 | 80.0 |
| 93 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 16 | 80.0 |
| 98 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 16 | 80.0 |
| 102 | 1 | 1 | 1 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 13 | 65.0 |
| 108 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 15 | 75.0 |
| 114 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 | 100.0 |
| 179 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 | 100.0 |
Studies are described using Serial numbers in Table 3
Table 8.
Results of quality assessment of 181 studies—cross-sectional studies: 37 studies. The Joanna Briggs Institute Critical Appraisal Checklist is used
|
Scoring: Yes = 2 / Unclear = 1 / No = 0 / NA = not applicable Q1: Were the criteria for inclusion in the sample clearly defined? Q2: Were the study subjects and the setting described in detail? Q3: Was the exposure measured in a valid and reliable way? Q4: Were objective, standard criteria used for measurement of the condition? Q5: Were confounding factors identified? Q6: Were strategies to deal with confounding factors stated? Q7: Were the outcomes measured in a valid and reliable way? Q8: Was appropriate statistical analysis used? | ||||||||||
| Study (serial no.) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Total ( /16) | % |
| 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 14 | 87.5 |
| 3 | 2 | 2 | 1 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 9 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 14 | 87.5 |
| 21 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 22 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 24 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 29 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 15 | 93.8 |
| 38 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 16 | 100.0 |
| 45 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 13 | 81.3 |
| 47 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 48 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 55 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 62 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 15 | 93.8 |
| 63 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 12 | 75.0 |
| 71 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 14 | 87.5 |
| 72 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 77 | 1 | 1 | 2 | 2 | 0 | 0 | 2 | 2 | 10 | 62.5 |
| 86 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 89 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 100 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 106 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 113 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 14 | 87.5 |
| 117 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 16 | 100.0 |
| 118 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 130 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 133 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 16 | 100.0 |
| 136 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 137 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 146 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 147 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 15 | 93.8 |
| 149 | 0 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 10 | 62.5 |
| 159 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 11 | 68.8 |
| 162 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 14 | 87.5 |
| 167 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 169 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 171 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
| 176 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 | 75.0 |
Studies are described using serial numbers in Table 3
Table 9.
Results of quality assessment of 181 studies—case series studies: 2 studies. The Joanna Briggs Institute Critical Appraisal Checklist is used
|
Scoring: Yes = 2 / Unclear = 1 / No = 0 / NA = not applicable Q1: Were there clear criteria for inclusion in the case series? Q2: Was the condition measured in a standard, reliable way for all participants included in the case series? Q3: Were valid methods used for identification of the condition for all participants included in the case series? Q4: Did the case series have consecutive inclusion of participants? Q5: Did the case series have complete inclusion of participants? Q6: Was there clear reporting of the demographics of the participants in the study? Q7: Was there clear reporting of clinical information of the participants? Q8: Were the outcomes or follow-up results of cases clearly reported? Q9: Was there clear reporting of the presenting site(s)/clinic(s) demographic information? Q10: Was statistical analysis appropriate? | ||||||||||||
| Study (serial no.) | Q1 | 1. Q2 | 1. Q3 | 1. Q4 | 1. Q5 | 1. Q6 | 1. Q7 | 1. Q8 | 1. Q9 | 10. Q10 | Total ( /20) | % |
| 76 | 1. 2 | 2. 2 | 2. 1 | 2. 1 | 1. 2 | 1. 2 | 1. 2 | 1. 1 | 2. 2 | 11. 2 | 17 | 85.0 |
| 181 | 2. 2 | 3. 2 | 3. 2 | 3. 2 | 2. 2 | 2. 2 | 2. 2 | 2. 2 | 3. 2 | 12. 2 | 20 | 100.0 |
Studies are described using serial numbers in Table 3
Table 10.
Results of quality assessment of 181 studies—randomised controlled trials: 40 studies. A modified version of critical appraisal checklist by van Tulder et al [15] is used
|
Scoring: Yes = 2 / Unclear = 1 / No = 0 / NA = not applicable Q1: Acceptable method of randomisation Q2: Concealed treatment allocation Q3: Similar group values at baseline Q4: Blinded assessor Q5: No or similar co-interventions Q6: Acceptable compliance (≥ 75%) Q7: Acceptable drop-out rate (≤ 30%) Q8: Similar timing of the outcome assessment in all groups Q9: Intention to treat analysis | |||||||||||
| Study (serial no.) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total ( /18) | % |
| 4 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 8 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 18 | 100.0 |
| 13 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 19 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 25 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 14 | 77.8 |
| 26 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 0 | 14 | 77.8 |
| 27 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 0 | 13 | 72.2 |
| 31 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 17 | 94.4 |
| 43 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 52 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | 66.7 |
| 60 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 61 | 1 | 1 | 2 | 2 | 2 | 1 | 0 | 2 | 0 | 11 | 61.1 |
| 64 | 1 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | 66.7 |
| 67 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 78 | 1 | 1 | 1 | 0 | 2 | 2 | 2 | 2 | 0 | 11 | 61.1 |
| 82 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 84 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 14 | 77.8 |
| 87 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 14 | 77.8 |
| 88 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 14 | 77.8 |
| 91 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 92 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 14 | 77.8 |
| 96 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 15 | 83.3 |
| 97 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 13 | 72.2 |
| 103 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 109 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | 66.7 |
| 110 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 120 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 14 | 77.8 |
| 123 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 129 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 140 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 143 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 148 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 165 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 166 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 168 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 15 | 83.3 |
| 173 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 0 | 12 | 66.7 |
| 174 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 0 | 13 | 72.2 |
| 177 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 16 | 88.9 |
| 178 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 2 | 0 | 11 | 61.1 |
| 180 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 18 | 100.0 |
Studies are described using serial numbers in Table 3
Fig. 3.
Sum of percentage from full score (%) based on the quality assessment in each type of study for each factor. Blue bar means FACTOR (‘it is a factor for patients’ satisfaction’) and orange bar means Not-FACTOR (‘it is a factor which does NOT relate to patients’ satisfaction’). a Patients’ demographical factors. b Patients’ non-knee factors. c Patients’ knee factors. d Factors of implants/prostheses. e Intra-operative technical factors. f Post-operative outcome factors. g Surgeon and healthcare factors
When the results of the quality assessment were taken into consideration, a negative history of mental health problems, use of a mobile-bearing insert, patellar resurfacing, severe pre-operative radiological degenerative change, negative history of low back pain, no/less post-operative pain, good post-operative physical function and pre-operative expectations being met were considered to be important factors. Significant factors affecting patient satisfaction are summarised in Tables 11, 12 and 13.
Table 11.
List of frequently reported factors as FACTOR (‘it is a factor for patient satisfaction’)
| Factors (number of reportings) | |
|---|---|
| 1st place | No mental health problems (13 reportings) |
| 2nd place | No/less post-operative pain (7 reportings) |
| 2nd place | Good post-operative physical function (7 reportings) |
| 4th place | Improvement in ROM (6 reportings) |
| 5th place | Normal BMI (5 reportings) |
| 5th place | Pre-operative expectations met (5 reportings) |
BMI body mass index, ROM range of motion
Table 12.
List of factors which have the highest sum of percentage score (a percentage from full score) of FACTOR (‘it is a factor for patient satisfaction’) only based on the quality assessment for various combination of the types of the studies
| RCT | RCT + Cohort |
RCT + Cohort + Case–control |
RCT + Cohort + Case–control + Cross-sectional |
RCT + Cohort + Case–control + Cross-sectional + Case series |
|
|---|---|---|---|---|---|
| 1st place | Use of mobile bearing insert (261.1%) | No mental health problems (672.6%) | No mental health problems (672.6%) | No mental health problems (885.2%) | No mental health problems (885.2%) |
| 2nd place | Patellar resurfacing (238.9 %) | Use of mobile-bearing insert (347.5%) | Use of mobile bearing insert (347.5%) | No/less post-operative pain (561.5%) | No/less post-operative pain (561.5%) |
RCT randomised controlled trial
Table 13.
List of factors which have the highest sum of percentage score (a percentage from full score) of FACTOR (‘it is a factor for patient satisfaction’) and Not-FACTOR (‘it is a factor which does NOT relate to patient satisfaction’) based on the quality assessment for all type of the studies
| Factors (% score) | |
|---|---|
| 1st place | No mental health problems (739.8%) |
| 2nd place | No/less post-operative pain (561.5%) |
| 3rd place | Good physical function (536.9%) |
| 4th place | Pre-operative expectations met (341.5%) |
| 5th place | Severe pre-operative radiographic degenerative change (301.2%) |
| 6th place | No low back pain (240.9%) |
Percentage score of Not-FACTOR was calculated as negative value
Discussion
The dissatisfaction rate following a TKR remains around 20% and is a constant source of frustration for the patient and the surgeon [11, 12]. Our study has systematically reviewed all the articles looking at satisfaction following a TKR to determine the factors, which could be responsible for this issue. Several factors were deemed to be important in affecting patient satisfaction based on the number of studies in which they were reported as well as the results of the quality assessment of the study (Tables 11, 12 and 13).
Negative history of mental health problems
A negative history of mental health problems was the most frequently reported factor affecting patient satisfaction (Table 11) and also scored the highest sum of percentage of FACTOR based on the quality assessment for RCT + cohort study (± case–control study ± cross-sectional study ± case series study) (Table 12). In addition, it was ranked first in terms of the highest sum of percentage of FACTOR and Not-FACTOR based on the quality assessment for all types of the studies (Table 13). Depressive symptoms and anxiety were reported to be predictive of long-term pain and functional impairment as measured by the Knee Society Score in 83 patients at 5 years [16]. In addition, it was reported that pre-operative anxiety/depression is an independent risk for severe post-operative pain and may explain as to why there is a subset of patients with unexplained pain after surgery [17]. Moreover, Macleod et al. report that patients with mental disability suffered a greater level of comorbidity and were socially deprived, which is also related to poorer physical health which then has an impact on satisfaction [18]. Finally, another study reported that patients with poor mental health, which can impair coping mechanisms for pain, might present with less severe disease, and this could also influence their satisfaction [19].
Use of a mobile-bearing insert
The use of a mobile-bearing insert had the highest sum of percentage of FACTOR based on the quality assessment for RCTs. Also, it had the second highest sum of percentage of FACTOR based on the quality assessment for RCT + cohort study (± case–control study) (Table 12). The rationale behind the design of a mobile-bearing insert is to solve the kinematic conflict between low-stress articulation and free axial femoral–tibial rotation by allowing rotation of a highly conforming polyethylene insert [20]. Theoretically, the design of the mobile-bearing insert could lead to better ROM especially during flexion [21]. A greater loss of flexion was reported after 12 months in patients with a TKR with a fixed-bearing prosthesis in comparison with a mobile-bearing prosthesis [22]. It is quite intuitive to comprehend that a good post-operative ROM relates to patient satisfaction, and our results support this (improvement in ROM was the 4th most frequently reported factor for patient satisfaction). Kim et al. suspect the low constraint of mobile-bearing insert may restore normal kinematics of the knee and it contributes to favourable clinical outcomes compared with a fixed-bearing insert [23]. Price et al. in a prospective multicentre trial of 39 simultaneous bilateral procedures also found that patients with a mobile-bearing insert had significantly better clinical results than patients with a fixed-bearing insert [21].
Patellar resurfacing
Patellar resurfacing has the second highest sum of percentage of FACTOR based on the quality assessment for RCTs (Table 12). Four studies showed patients with patella resurfacing were more satisfied than those without it [11, 24–26]. Amongst them, one study focused on only knees with no exposed bone on the undersurface of the patella to determine the potential advantages of leaving the patella non-resurfaced [25]. Dissatisfaction in patella non-resurfaced patients may be due to the higher rate of post-operative anterior knee pain, and patients whose patella was not resurfaced at the index TKR tended to have a higher revision rate as well [25–28]. However, it should be noted that this issue may be strongly related to the design of the implant. There have also been abundant literature that showed that the patellofemoral design in TKR is critical and can vary the forces on the patellofemoral joint as well as patellofemoral tracking [29–31]. Two of the 4 studies relate to a specific prosthesis (PFC) which is notoriously patella unfriendly [25, 26], so this relationship may therefore not necessarily hold true for the newer implants with patella-friendly designs.
Severe pre-operative radiological degenerative change
Severe pre-operative radiological degenerative change has the fifth highest sum of percentage of FACTOR and Not-FACTOR based on the quality assessment for all types of studies (Table 13). Although the classic indication for replacing a patient’s knee is end-stage arthritis (Kellgren–Lawrence grade IV [32]), there are a number of patients who have a TKR much before grade IV radiological changes have set in and it is dependent on the symptoms of the patient. The individual indication is complex and involves multiple factors [33]. Patients with mild pre-operative OA were reported to have a worse prognosis in improvement in physical functioning [34, 35], and therefore, it is difficult to meet their expectations post-operatively [35]. These effects are more noticeable in patients undergoing a TKR as compared with those who have had a THR [34]. The knee is a complex joint and the biomechanics of this joint are much more difficult to replicate with a prosthetic knee as compared with a prosthetic hip which may partly explain a smaller increase in physical functioning and a poor rate of satisfaction in patients with mild OA having a TKR [36].
No low back pain
No low back pain has the sixth highest sum of percentage of FACTOR and Not-FACTOR based on the quality assessment for all types of the studies (Table 13). The prevalence of chronic low back pain in the UK has been reported to range from 6 to 11% [29], and this is increased to 55% in patients with OA of the knee [30]. Furthermore, low back pain has been demonstrated to be three to four times more likely to be present in patients with a history of depression [37]. Also, patients with chronic low back pain have a higher rate of musculoskeletal and neuropathic pain conditions, depression, anxiety and sleep disorders [31]. In addition, patients with low back pain reported to have more symptoms from their osteoarthritic knee which may suggest a lower threshold for pain in this cohort leading to dissatisfaction [30].
Normal BMI
Normal BMI was the fifth most frequently reported factor for patient satisfaction (Table 11). BMI greater than 30 kg/m2 was reported to be associated with a higher rate of revision and poorer functional outcomes as well which again contributes to dissatisfaction [38]. In addition, morbidly obese patients are likely to suffer from wound problems, ligament injuries and infections peri-operatively which lead to dissatisfaction [22]. Another study showed that despite lower pre- and post-operative WOMAC and SF-36 scores, obese patients experienced similar improvements compared with non-obese patients, although levels of satisfaction in the obese group were lower than those in the non-obese group [39]. The authors stated that one explanation for this might be that satisfaction was more closely associated with the absolute post-operative functional level rather than the magnitude of any improvement, as the rate of satisfaction mirrored absolute values of post-operative WOMAC and SF-36 scores.
Other factors
Other than factors discussed in the previous section, no/less post-operative pain, good post-operative physical function, improvement in ROM and pre-operative expectations being met were considered to be important for patient satisfaction based on the number of reportings and the results of quality assessment (Tables 11, 12 and 13). TKR is a painful procedure and it does take at least six to 12 months to get the maximum benefit from this procedure [40], and therefore, setting realistic expectations with the patient in the pre-operative clinic is essential to avoid dissatisfaction.
Limitations and strengths of the study
Our study has several limitations. Firstly, the method of measuring satisfaction is different in each study, and therefore, a uniform way of assessing satisfaction is essential for the orthopaedic community. Secondly, the timing of assessment of satisfaction after the index TKR varied amongst studies and this again requires standardisation. Thirdly, in many of the studies included in this review, the authors have only focused on one factor and the mutual or overall effect of multiple factors was not assessed. Fourthly, no statistical tests of intra-class correlation coefficients, inter-rater reliability and heterogeneity amongst the studies were performed in this systematic review. Finally, there are several studies in which patients are duplicated amongst studies and our review was limited to publications in English, so there is a possibility of publication bias.
However, despite all these limitations, the main strength of this study lies in its broad and comprehensive initial literature search as well as complete and in-depth quality assessment for each study and the factors. We have determined all the factors which could potentially affect patient satisfaction following a TKR which have been reported in the literature thus far.
Conclusion
No history of mental health problems, use of a mobile bearing insert, patellar resurfacing, severe pre-operative radiological degenerative change, no low back pain, normal BMI, no/less post-operative pain, good physical function post-operatively, improvement in ROM and pre-operative expectations being met were considered to be significant factors leading to better patient satisfaction following a TKR.
Surgeons performing a TKR should take these factors into consideration prior to deciding whether a patient is suitable for a TKR. Secondarily, a detailed explanation of these factors should form part of the process of informed consent to achieve better patient satisfaction following TKR.
There is great need for a unified approach to assessing satisfaction following a TKR and also the time at which satisfaction is assessed.
Moreover, further studies and ideally larger RCTs focusing on each of these factors are required to determine the exact correlation of these factors with satisfaction.
Electronic supplementary material
(DOCX 15.6 kb)
(DOCX 41.7 kb)
(DOCX 17.8 kb)
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Naoki Nakano, Email: gnaokix1981@gmail.com.
Haitham Shoman, Email: haitham.sh89@gmail.com.
Fernando Olavarria, Email: olavarria.f@gmail.com.
Tomoyuki Matsumoto, Email: matsun@m4.dion.ne.jp.
Ryosuke Kuroda, Email: kurodar@med.kobe-u.ac.jp.
Vikas Khanduja, Email: vk279@cam.ac.uk.
References
- 1.NICE report: Osteoarthritis: the care and management of osteoarthritis. https://www.nice.org.uk/guidance/cg177/resources/osteoarthritis-care-and-management-pdf-35109757272517. (date last accessed 16 Dec 2018)
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/00004623-200704000-00012. [DOI] [PubMed] [Google Scholar]
- 3.NJR Annual reports 2016. http://www.njrcentre.org.uk/njrcentre/Reports,PublicationsandMinutes/Annualreports/tabid/86/Default.aspx (date last accessed 16 Dec 2018)
- 4.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 5.Hakim J, Volpin G, Amashah M, Alkeesh F, Khamaisy S, Cohen M, Ownallah J (2019) Long-term outcome of total knee arthroplasty in patients with morbid obesity. Int Orthop [DOI] [PubMed]
- 6.Cho KJ, Seon JK, Jang WY, Park CG, Song EK. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop. 2019;43(6):1345–1354. doi: 10.1007/s00264-018-4231-1. [DOI] [PubMed] [Google Scholar]
- 7.Bullens PHJ, Van Loon CJM, De Waal Malefijt MC, Laan RFJM, Veth RPH. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplast. 2001;16(6):740–747. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 8.Hawker GA. Who, when, and why total joint replacement surgery? The patientʼs perspective. Curr Opin Intern Med. 2006;5(6):639–643. doi: 10.1097/01.bor.0000240367.62583.51. [DOI] [PubMed] [Google Scholar]
- 9.Peersman G, Verhaegen J, Favier B (2019) The forgotten joint score in total and unicompartmental knee arthroplasty: a prospective cohort study. Int Orthop [DOI] [PubMed]
- 10.Sugita T, Miyatake N, Aizawa T, Sasaki A, Kamimura M, Takahashi A (2018) Quality of life after staged bilateral total knee arthroplasty: a minimum five-year follow-up study of seventy-eight patients. Int Orthop [DOI] [PubMed]
- 11.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71(3):262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 12.Baker PN, Rushton S, Jameson SS, Reed M, Gregg P, Deehan DJ. Patient satisfaction with total knee replacement cannot be predicted from pre-operative variables alone: a cohort study from the National Joint Registry for England and Wales. Bone Joint J. 2013;95B(10):1359–1365. doi: 10.1302/0301-620X.95B10.32281. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.JBI JBI-CAT. Critical appraisal tools. http://joannabriggs.org/research/critical-appraisal-tools.html (date last accessed 16 Dec 2018)
- 15.van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 16.Brander V, Gondek S, Martin E, Stulberg SD. Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res. 2007;464:21–26. doi: 10.1097/BLO.0b013e318126c032. [DOI] [PubMed] [Google Scholar]
- 17.Bonnin MP, Basiglini L, Archbold HA. What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1411–1417. doi: 10.1007/s00167-011-1549-2. [DOI] [PubMed] [Google Scholar]
- 18.Macleod U, Mitchell E, Black M, Spence G. Comorbidity and socioeconomic deprivation: an observational study of the prevalence of comorbidity in general practice. Eur J Gen Pract. 2004;10(1):24–26. doi: 10.3109/13814780409094223. [DOI] [PubMed] [Google Scholar]
- 19.Verra ML, Angst F, Staal JB, et al. Differences in pain, function and coping in Multidimensional Pain Inventory subgroups of chronic back pain: a one-group pretest-posttest study. BMC Musculoskelet Disord. 2011;12:145. doi: 10.1186/1471-2474-12-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carothers JT, Kim RH, Dennis DA, et al. Mobile-bearing total knee arthroplasty: a meta-analysis. J Arthroplast. 2011;26(4):537–542. doi: 10.1016/j.arth.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 21.Price AJ, Rees JL, Beard D, et al. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis: a multicentre single-blind randomised controlled trial. J Bone Joint Surg (Br) 2003;85-B:62–67. doi: 10.1302/0301-620X.85B1.13233. [DOI] [PubMed] [Google Scholar]
- 22.Shakespeare D, Kinzel V, Ledger M. Achieving ligament stability and correct rotational alignment of the femur in knee arthroplasty: a study using the Medial Pivot knee. Knee. 2005;12:419–423. doi: 10.1016/j.knee.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res. 2009;467(2):493–503. doi: 10.1007/s11999-008-0221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayman D, Bourne RB, Rorabeck CH, Vaz M, Kramer J. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplast. 2003;18:541–545. doi: 10.1016/S0883-5403(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 25.Roberts DW, Hayes TD, Tate CT, Lesko JP. Selective patellar resurfacing in total knee arthroplasty: a prospective, randomized, double-blind study. J Arthroplast. 2015;30(2):216–222. doi: 10.1016/j.arth.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85–A(2):212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. The John Insall Award : patella resurfacing versus nonresurfacing in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:12–25. doi: 10.1097/01.blo.0000148594.05443.a3. [DOI] [PubMed] [Google Scholar]
- 28.Burnett RSJ, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty: a concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91(11):2562–2567. doi: 10.2106/JBJS.H.00109. [DOI] [PubMed] [Google Scholar]
- 29.Tanzer M, McLean CA, Laxer E, et al. Effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in total knee arthroplasty. Can J Surg. 2001;44:127–133. [PMC free article] [PubMed] [Google Scholar]
- 30.Benjamin JB, Szivek JA, Hammond AS, et al. Contact areas and pressures between native patellas and prosthetic femoral components. J Arthroplast. 1998;13:693–698. doi: 10.1016/S0883-5403(98)80015-6. [DOI] [PubMed] [Google Scholar]
- 31.Andriacchi TP, Yoder D, Conley A, et al. Patellofemoral design influences function following total knee arthroplasty. J Arthroplast. 1997;12:243–249. doi: 10.1016/S0883-5403(97)90019-X. [DOI] [PubMed] [Google Scholar]
- 32.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riddle DL, Jiranek WA, Neff RS, Whitaker D, Hull JR. Extent of tibiofemoral osteoarthritis before knee arthroplasty: multicenter data from the osteoarthritis initiative. Clin Orthop Relat Res. 2012;470(10):2836–2842. doi: 10.1007/s11999-012-2328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keurentjes JC, Fiocco M, So-Osman C, et al. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PLoS One. 2013;8(4):e59500. doi: 10.1371/journal.pone.0059500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meding JB, Ritter MA, Faris PM, Keating EM, Harris W. Does the preoperative radiographic degree of osteoarthritis correlate to results in primary total knee arthroplasty? J Arthroplast. 2001;16(1):13–16. doi: 10.1054/arth.2001.16501. [DOI] [PubMed] [Google Scholar]
- 36.Wolterbeek N, Garling EH, Mertens BJ, Nelissen RG, Valstar ER. Kinematics and early migration in single-radius mobile- and fixed-bearing total knee prostheses. Clin Biomech (Bristol, Avon) 2012;27(4):398–402. doi: 10.1016/j.clinbiomech.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 37.Clement ND, MacDonald D, Simpson AHRW, Burnett R. Total knee replacement in patients with concomitant back pain results in a worse functional outcome and a lower rate of satisfaction. Bone Joint J. 2013;95-B(12):1632–1639. doi: 10.1302/0301-620X.95B12.31684. [DOI] [PubMed] [Google Scholar]
- 38.Singh JA, O'Byrne M, Harmsen S, Lewallen D. Predictors of moderate-severe functional limitation after primary total knee arthroplasty (TKA): 4701 TKAs at 2-years and 2935 TKAs at 5-years. Osteoarthr Cartil. 2010;18(4):515–521. doi: 10.1016/j.joca.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baker P, Muthumayandi K, Gerrand C, Kleim B, Bettinson K, Deehan D. Influence of body mass index (BMI) on functional improvements at 3 years following total knee replacement: a retrospective cohort study. PLoS One. 2013;8(3):e59079. doi: 10.1371/journal.pone.0059079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dailiana ZH, Papakostidou I, Varitimidis S, et al. Patient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord. 2015;16:366. doi: 10.1186/s12891-015-0814-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15.6 kb)
(DOCX 41.7 kb)
(DOCX 17.8 kb)