Abstract
Introduction
The increase in access to Emergency Departments (ED) worldwide causes inefficiencies, but also signals its importance. The Coronavirus (Covid-19) outbreak allows to study the reactions of patients to the news about the spreading of the infection, which may have generated the fear that ED was no longer safe.
Methods
We study access to ED of a large teaching hospital in Brescia - one of the most hit provinces in Italy by Covid-19 - during the pandemic (from the announcement of the first cases to the explosion of the pandemic, to months after end of the acute phase) to study how patients reacted to the news that ED could no longer be a safe place. We analyse triage code, mode of arrival to ED, and accesses related to chest and abdominal pain, to evaluate who was discouraged most.
Results
Accesses have drastically reduced immediately after the news of the first contagion. During the lockdown accesses and admissions to hospital ward have decreased; this may mean that some patients may have suffered reduced health or increased mortality risks because of this decision. At the end of June accesses to ED and admissions to hospital ward are still lower than usual.
Discussion
Fear of contagion and appeals not to use ED directly by Covid-19 patients may have discouraged access also for pressing health need.
Keywords: Covid-19 pandemic, ED accesses, Fear, Patients behaviour, Hospital reaction
1. Introduction
In the last decades, health care needs have moved from acute to chronic conditions, calling for a reorganisation in the delivery of health care services. In spite of this shift, the number of patients admitted to Emergency Departments (ED) has risen worldwide, both in systems characterised by public and private health care finance. [[1], [2], [3]]. The change in demand composition [4,5] supply shortages, availability of primary or community care services [[6], [7], [8], [9]], strategic behaviour [[10], [11], [12]], overestimation of health needs [13] may be responsible for this increase, which is also the signal of the importance and the confidence that patients attach to ED services. The Coronavirus disease (Covid-19) outbreak has created a major disruption in health care delivery, both for patients that were infected and for those that were not treated because of the pandemic [14]. In this article we study the effects that other factors - such as the fear that the ED may not be safe and the campaign to reduce direct accesses to the ED – have had on ED accesses.
Narrative literature shows that during the Covid-19 pandemic the number of access to ED has dramatically reduced in Italy; most of the headlines seem to suggest that in prevalence inappropriate accesses have been discouraged because of fear. In actual fact, since there is no evidence showing that only the latter have decreased, it is important to study who has kept at large from ED because of fear to be infected, and as a response to the pressing invitations by health care regulators (the Ministry of Health, the Italian Civil Protection, the Regional Health Authorities) to avoid straight access to ED for Covid-19 symptoms. These messages, together with the broadcasting of alarming news by all media, might have discouraged patients with non-Covid-19 symptoms to access because of the fear of infection and congestion of the ED. In this article, we analyse patients admitted to the ED of Spedali Civili University Hospital, Brescia, and a large teaching hospital in one of the most hit provinces in Italy by the Covid-19 pandemic. We exploit the time elapsed between the announcement of the first case and the explosion of the pandemic in Brescia to study the reactions of patients to the news about the spreading of the contagion in Lombardy, which may have generated in the patients the fear that ED was no longer the safe place they were used to think it was.
We show that ED accesses have drastically reduced, even during the first week after the first contagion, when the virus was circulating undetected [15] and there was no evidence that that visiting an ED might have increased the probability of being infected. During the lockdown, accesses have dramatically reduced and at the end of June, in spite of the significant reduction in the number of new infections, ED access are not yet back to normal. While the reduction for less urgent patients (green and white codes) may have increased appropriateness of care, the decrease in access for more urgent conditions (yellow and white codes) might have meant that some patients might have suffered a reduce health or an increased mortality risk because of this decision [16].
2. Material and methods
This study uses patients’ registry data for the Emergency Department (ED) of Spedali Civili University Hospital in Brescia, Italy. The Hospital is serving an area of nearly 1,200,000 people in the east of Lombardy with 1570 beds, and was the hospital which admitted the largest number of Covid-19 patients in Italy. In the last 3 years, the number of accesses to ED ranged between 78.000 and 80.300 per year.
After the first epidemic of Covid-19 in Wuhan (China), Lombardy, (a region in the north of Italy), and in particular the provinces of Bergamo, Brescia, Lodi and Cremona had become the most affected area in Europe [17]. The pandemic event officially started on February 20th, when the so-called “patient one” was found positive at the hospital of Codogno. In Brescia, the first admissions of Covid19 positive patients through ED date on February 23rd, but in the first week few cases reached ED. The stream of patients started at the beginning of March; since then, more than 3.000 patients suspected for Covid-19 accessed to ED.
From the onset of the pandemic, newspapers, news channels, and online websites regularly update their pages with official information on the spread of the virus (collected by the Ministry of Health in collaboration with Italian National Institute of Health - Istituto Superiore Sanità ISS). The Civil Protection Department broadcasted at 18.00 daily through a press conference until April the 30th. Since the inception of the pandemic, Regional Health Authorities and the Ministry of Health have opened toll-free telephone lines for information on Covid-19. These lines had the explicit goal to avoid congestion for the emergency numbers, an event that actually took place in the peak days of the health crisis. We analyse accesses to the ED of Spedali Civili in Brescia during four periods:
-
•
Before the Covid-19 outbreak, from February 1st to February 22nd 2020, before the first Covid-19 positive case in Codogno and the lockdown of ten municipalities of the nearby province of Lodi.
-
•
The so-called “Fear week”, from February 23rd to March 1st. The lockdown of some municipalities in Lombardy has begun, the daily press conference begins with the updating of the pandemic data, appeals were made not to access ED directly, but to use the emergency numbers. During that period, virtually, no Covid-19 patients were admitted to the ED in Brescia.
-
•
Epidemic of Covid-19 associated disease, from March 2nd to May 3rd. On Monday, March 2nd 31 Covid-19 positive patients were admitted at the ED; on March 8th the lockdown of all the Lombardy region begun. Since March 1st a tent was set up for a pre-triage in order to keep ER free from non-tested Covid-19 patients
-
•
Phase 2: from May 4th to June 30th. The lockdown constraints are relaxed; during “Phase 2″ the prescription of social distancing and (in Lombardy) the use of face masks was maintained while in Phase 3 (since June 15th) several restrictions were lifted, but the protocols to access the ED did not change.
We compare accesses between the different periods in 2020 and to the same periods of the previous year, 2019.
Similarly to many EDs in Europe, on arrival patients are assigned a priority tag based on a five colour code that measures the criticality of patients’ condition: black (dead on arrival); red (urgent patients that must be attended to immediately); yellow (less urgent patients), green for whom some waiting is possible, while white codes represent an inappropriate use of the ED (patients have a fixed co-payment, whereas for the other codes access is free. See [18]). For each ED access from February to June 2019 and 2020, the department information system has made available anonymous data on basic demographic characteristics of the patients; their main symptoms, means of arrival and priority code; their waiting time, defined as the minutes elapsed between the arrival and the time they have been taken in charge; if they have been tested for Covid-19 and finally if they have been admitted to hospital or not. The information system of the laboratories has provided daily data on the number of ED patients tested positive for Covid-19 from February 28th to May 14th 2020. The retrospective nature of this study allows to use complete anonymized patients data; this implies that ethical committee approval was unnecessary, in accordance with local policy.
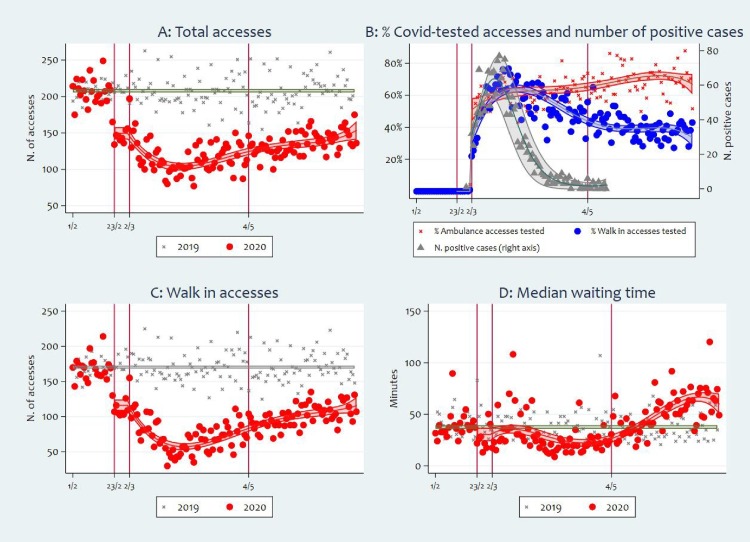
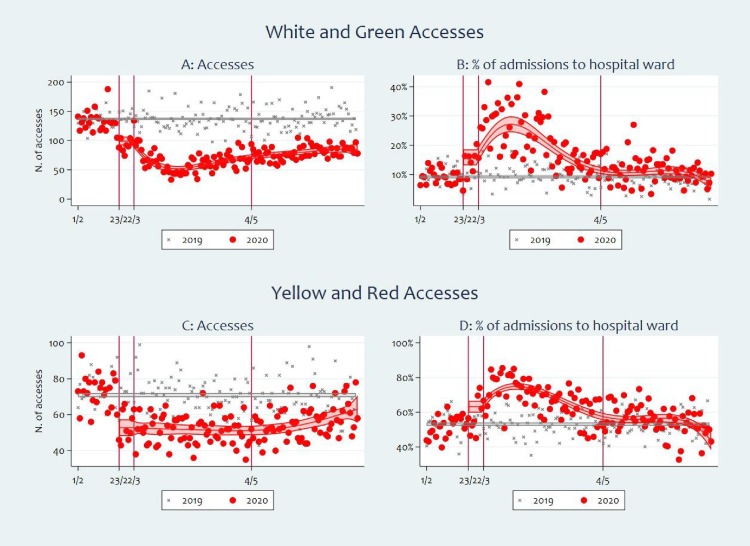
In Fig. 1, Fig. 2 we show the daily statistics separately for years 2019 and 2020 and the predicted values by the regression models, with the corresponding 90 % confidence interval. For the daily number of accesses (Figs. 1A, C, 2 A and C) and the median waiting time (Fig. 1D), we regress the outcome variable on a constant, a dummy variable - which takes value one since the beginning of the “fear week”, and a 4th degree polynomial in the number of days since the start of pandemic March 2nd 2020. For the percentage of admissions to hospital ward (Fig. 2B and D) and the percentage of accesses tested for Covid-19 (Fig. 1B), a logit transformation is applied to the outcome variables. For the number of patients positive to the Covid-19 test (Fig. 1B), a negative binomial regression model is used. For the percentage of tested patients and the number of positive cases (Fig. 1B), only days form March 2nd 2020 are used.
Fig. 1.
Daily total (A) and walk-in accesses (C); daily percentage of Covid-19 tested accesses by access type and number of Covid-19 positive (B); daily median waiting time. Vertical lines identify the pre-Covid-19 period (before February 23rd), the “fear week” (February 23rd - March 1st), the epidemic period (March 2nd – May 3rd) and Phase 2 (from May 4th).
Fig. 2.
Daily accesses and share of admissions to hospital ward total by triage code. Vertical lines identify the pre-Covid-19 period (before February 23rd), the “fear week” (February 23rd - March 1st), the epidemic period (March 2nd – May 3rd) and Phase 2 (from May 4th).
3. Results
Table 1 shows that in the “fear week” the average daily number of ED accesses decreased by about 67 cases (−31.8 %) with respect to the same period in 2019, with a very sharp decrease that followed immediately the news about “patient one” in Codogno as shown in Fig. 1A. The reduction in the number of daily accesses was very rapid at the beginning of the pandemic (in the first weeks in March), when the department was clogged with Covid-positive cases. The accesses started increasing at the beginning of April, when the daily updates on the contagion showed that the peak was reached. The news about the start of Phase 2 (announced on April 26th) and the beginning of Phase 3 (15th June) do not seem to have produced a big impact on the number of ED daily accesses, which at the end of June still experienced an average reduction by about 50 case with respect to 2019. Overall, since the beginning of Phase 2, the average daily accesses are lower than in the “fear week” (136 vs 144.5, see Table 1), although the number of Covid-19 positive cases in ED is about the same as during the “fear week” (Fig. 1B).
Table 1.
Average daily number of accesses and admissions to hospital, and average daily percentage of admissions to hospital, by period, year and priority codes. Delta is the difference between 2020 and 2019 means, Std.Err. is the standard error of the difference, and pvalue is computed for the null hypothesis of equality between 2020 and 2019 means vs the bilateral alternative.
|
Daily accesses | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total |
Yellow & Red priority codes |
White & Green priority codes |
|||||||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | Pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 209.18 | 205.73 | −3.45 | 4.80 | 0.473 | 74.36 | 72.73 | −1.64 | 2.73 | 0.55 | 134.82 | 133.00 | −1.82 | 4.55 | 0.69 |
| Fear week | 211.86 | 144.50 | −67.36 | 3.95 | <0.001 | 70.29 | 52.88 | −17.41 | 4.13 | <0.001 | 141.57 | 91.63 | −49.95 | 4.27 | <0.001 |
| Pandemic | 208.25 | 115.08 | −93.17 | 3.79 | <0.001 | 70.89 | 51.56 | −19.33 | 1.58 | <0.001 | 137.37 | 63.52 | −73.84 | 3.28 | <0.001 |
| Phase 2 | 207.29 | 135.97 | −71.33 | 3.59 | <0.001 | 69.05 | 55.84 | −13.21 | 1.87 | <0.001 | 138.24 | 80.12 | −58.12 | 2.81 | <0.001 |
|
admitted to hospital |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total |
Yellow & Red priority codes |
White & Green priority codes |
|||||||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | Pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 54.32 | 50.27 | −4.05 | 2.54 | 0.112 | 39.50 | 37.95 | −1.55 | 2.20 | 0.482 | 14.82 | 12.32 | −2.50 | 1.11 | 0.024 |
| Fear week | 49.14 | 42.88 | −6.27 | 3.85 | 0.104 | 38.00 | 30.38 | −7.63 | 2.75 | 0.006 | 11.14 | 12.50 | 1.36 | 2.31 | 0.557 |
| Pandemic | 51.54 | 48.65 | −2.89 | 1.82 | 0.114 | 37.78 | 35.24 | −2.54 | 1.31 | 0.054 | 13.76 | 13.41 | −0.35 | 1.00 | 0.728 |
| Phase 2 | 49.24 | 39.66 | −9.59 | 1.49 | <0.001 | 36.55 | 30.60 | −5.95 | 1.24 | <0.001 | 12.69 | 9.05 | −3.64 | 0.73 | <0.001 |
|
admitted to hospital (%) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total |
Yellow & Red priority codes |
White & Green priority codes |
|||||||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | Pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 25.96 | 24.43 | −1.53 | 1.07 | 0.154 | 53.10 | 51.99 | −1.12 | 2.02 | 0.581 | 11.01 | 9.29 | −1.72 | 0.78 | 0.028 |
| Fear week | 23.19 | 29.53 | 6.34 | 2.05 | 0.002 | 54.16 | 57.59 | 3.43 | 3.75 | 0.36 | 7.86 | 13.44 | 5.58 | 1.97 | 0.005 |
| Pandemic | 24.82 | 42.78 | 17.96 | 1.31 | <0.001 | 53.42 | 67.93 | 14.51 | 1.51 | <0.001 | 10.06 | 21.53 | 11.47 | 1.21 | <0.001 |
| Phase 2 | 23.75 | 29.33 | 5.58 | 0.82 | <0.001 | 52.93 | 55.10 | 2.17 | 1.42 | 0.126 | 9.18 | 11.38 | 2.20 | 0.71 | 0.002 |
The reduction in the number of accesses was driven by walk-in accesses (Fig. 1C), that is, individuals that reached ED without having their access arranged by the emergency services (mostly ambulance). ED was able to respond rather efficiently to the crisis: the median waiting time between triage and treatment did not increase during the first weeks in March and stayed lower than usual during the pandemic (Fig. 1D), despite the fact that patients started to be massively tested for Covid (Fig. 1B) and that it was required to wait for the results of the nasopharyngeal swab before treatment [19]. The longer procedures combined with the number of accesses slowly approaching pre-Covid figures caused the rise in the waiting times in Phase 2 that became longer than in 2019.
From Fig. 1B we can also see that the massive campaign that Regional health authorities launched to reduce the number of unfiltered accesses to ED of patients with Covid-19 symptoms was not fully effective. The campaign would in fact have been effective if patients directly accessing the ED (walk-in accesses) did not have Covid-19 symptoms. Since patients with Covid-19 symptoms were tested, we compare the share of Covid-19 tested patients for ambulance and walk-in accesses to see if they are qualitatively different in this respect. In the first weeks, about 60 % of walk-in and ambulance accesses were tested, it is only in April that the percentage of walk-in accesses tested started declining toward about 40 %. We read this result as evidence that a significant proportion of patients seems to have ignored the appeals not to drive to ED. A more accurate test would be represented by the number of unfiltered accesses (walk-in access) that were found positive; however the nature of our data does allow to match patients data (which records the prescription of a swab) with clinical outcomes (which record the result of the swab).
Table 1 shows that the reduction in the number of accesses to ED was not accompanied by a proportional reduction in the number of patients admitted to hospital wards through ED. In fact, as a whole, the percentage of patients admitted to ED that required hospital treatment went up to 29.5 % on average in the fear week and to 42.8 % during the pandemic phase, levels that are significantly higher than the corresponding statistics in 2019. This increase reduced the gap in admissions to hospital wards through ED to 6.3 units in the fear week (−12.8 % with respect to 2019) and to 2.9 during the pandemic (−5.6 %). The beginning of Phase 2 did not mean going back to pre-Covid levels: the percentage of ED accesses admitted to hospital wards was still 29.3 % that, despite the rise in the total number of accesses to ED, brings on average to 9.6 fewer daily hospital wards admissions (difference that is statistically different from zero).
Table 1 presents also the average daily accesses for yellow and red codes (centre) and white and green codes (right). In the “fear week”, the reduction is more important for white and green codes (−49.9 units, −35.3 % with respect to the same period in 2019) than for red and yellow codes (−17.4, −24.8 %). Both reductions are significantly different from zero (p value <0.001). These differences increased during the pandemic phase (−73.8 and −19.3) and reduced slightly in Phase 2 (−58.1 and −13.2). As a consequence, the mix of priority codes changed over time. This is not the only characteristics of the pool of patients that changed in the period considered: the case mix (Table A1 in the Appendix), gender and age (Table A2 in the Appendix) also evolved throughout the different phases and with respect to 2019. The change in the mix of causes during the fear week and Phase 2 is rather limited (and mainly due to the higher prevalence of fever cases), changes in gender and age composition can be explained by the higher vulnerability of older and male patients to Covid-19 (see e.g. [20,21]).
Fig. 2 compares the dynamics of accesses and the ratio of admission to the hospital wards by priority codes. The number of green and white codes experienced a sharp reduction until the end of March, when they started increasing again, without reaching the before-crisis numbers (Fig. 2A). These are the accesses with a higher risk of being inappropriate. The increase in the ratio of patients requiring hospitalization (Fig. 2B) was enough to make no significant difference in the number of patients admitted to hospital wards before Phase 2; whereas in Phase 2 the number of admissions is still 3.6 daily units lower than those in the same period in 2019 (and statistically significantly different from zero, see Table 1).
For yellow and red codes, the picture is rather different. We can observe a sharp decrease in the number of accesses during the “fear week” and since then there is no evidence of recovering (Fig. 2C). The hospitalisation rate increased in the first weeks of the Covid-19 pandemic and was slightly higher than normal, but in Phase 2, due to the reduction in the number of accesses, the number of admissions was about 6 patients lower compared with the same week in 2019 (and statistically significantly different from zero, see Table 1).
To limit the bias of possible composition effects on our conclusions, we focus on two more homogeneous group of patients, i.e. access to ED for chest and abdominal pain. For these patients a delay may have severe consequences and long-last effects: The gender mix did not change with respect to normal period, and the average age increased during the pandemic only for patients with abdominal pain (see Table A2).
As shown in Table 2 , in the “fear week”, we estimate that, on average, 3.3 patients with chest pain and 5.3 with abdominal pain did not visit ED daily (about −32 % in both cases). For abdominal pain, the percentage of hospital admissions significantly increased in the same period, and it has partially compensated the decrease in the number of accesses, leaving the number of admissions at the pre-crisis level. This seems to suggest that only few patients with abdominal pain requiring secondary care kept at large from ED during the fear week. In the following weeks, the number of accesses to ED for chest and abdominal pain was further reduced and the admission rate peaked above 40 %. In both cases, it is interesting to note that in Phase 2 the number of accesses is still significantly lower than normal, as well as hospital admissions (by about one daily units for chest and two for abdominal pain).
Table 2.
Average daily number of accesses and admissions to hospital, and average daily percentage of admissions to hospital, for chest and abdominal pain symptoms, by period and year. Delta is the difference between 2020 and 2019 means, Std.Err. is the standard error of the difference, and pvalue is computed for the null hypothesis of equality between 2020 and 2019 means vs the bilateral alternative.
|
Daily accesses | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chest Pain |
Abdominal pain |
|||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 10.41 | 10.77 | 0.36 | 1.02 | 0.721 | 16.23 | 13.23 | −3.00 | 1.04 | 0.004 |
| Fear week | 10.14 | 6.88 | −3.27 | 1.08 | 0.003 | 16.29 | 11.00 | −5.29 | 1.40 | <0.001 |
| Pandemic | 11.38 | 4.46 | −6.92 | 0.60 | <0.001 | 14.90 | 4.44 | −10.46 | 0.69 | <0.001 |
| Phase 2 | 9.10 | 6.53 | −2.57 | 0.58 | <0.001 | 15.36 | 9.88 | −5.48 | 0.82 | <0.001 |
|
of which admitted to hospital |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chest Pain |
Abominala pain |
|||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 3.32 | 3.05 | −0.27 | 0.57 | 0.636 | 6.50 | 4.95 | −1.55 | 0.68 | 0.025 |
| Fear week | 2.86 | 2.25 | −0.61 | 0.71 | 0.391 | 5.14 | 5.25 | 0.11 | 1.03 | 0.917 |
| Pandemic | 3.84 | 1.84 | −2.00 | 0.33 | <0.001 | 6.17 | 2.27 | −3.90 | 0.42 | <0.001 |
| Phase 2 | 3.12 | 2.21 | −0.91 | 0.31 | <0.001 | 6.17 | 3.98 | −2.19 | 0.45 | <0.001 |
|
of which admitted to hospital (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Chest Pain |
Abdominal pain |
|||||||||
| 2019 | 2020 | Delta | Std.Err. | pvalue | 2019 | 2020 | Delta | Std.Err. | pvalue | |
| Before | 32.08 | 26.26 | −5.82 | 4.48 | 0.195 | 39.41 | 37.83 | −1.58 | 3.50 | 0.652 |
| Fear week | 27.69 | 27.65 | −0.04 | 6.70 | 0.995 | 30.30 | 48.67 | 18.38 | 5.67 | 0.001 |
| Pandemic | 34.44 | 42.57 | 8.13 | 4.37 | 0.064 | 41.31 | 51.74 | 10.43 | 4.06 | 0.011 |
| Phase 2 | 33.61 | 34.90 | 1.29 | 3.49 | 0.711 | 40.59 | 41.37 | 0.78 | 3.01 | 0.795 |
4. Discussion
In Italy, the Covid-19 pandemic caused a crisis, never experienced before, resulting in a revolution that invested the entire national health care system. It was necessary a sudden reorganization of the hospital care and in particular of the Emergency Departments to meet patients need [22]. The ED seems to have coped rather well with the crisis: in spite of the additional routines that were implemented because of the pandemic, median waiting times were not higher than normal. The Department has also changed access to treatment by setting up a tent outside the hospital where patients with Covid-19 symptoms were triaged and received first care. This organisation should have reassured patients on the ED safety. The evidence from our analysis is instead rather different. Our results show a dramatic decrease in access to ED immediately after the announcement of the lockdown in nearby territories, in a week where there was no evidence of contagion in Brescia, a reduction that increased during the most acute phase of the pandemic, and which has not been recovered at its end. The reduction is mostly driven by self-referral, i.e. those patients that decide to go straight to ED without contacting any other primary or emergency care service. Usually, they are also less urgent codes (white or green), and their reduction is probably determined by the combined effect of fear of being infected and the massive campaign to keep Covid-19 patients away from ED. For green and white codes, this might have meant an increase in the appropriateness of ED care since the probability of these accesses being inappropriate is high [11]. However, also red and yellow codes have decreased and, something perhaps more worrying for its long-term consequences, they have not resumed to normal at the end of the pandemic. A more formal analysis, along the lines proposed by [23] is necessary and should be carried out as soon as detailed data on hospital admissions is available.
The “fear” effect, and the effect of the pandemic afterward, has changed the mix of patients, increasing the fraction of male and the average age. For the weeks of the pandemic, this is in line with the results of the first studies on the Covid outbreak [17,24]. The mix was still different from pre-Covid situation also in Phase 2, at the end of the acute phase. An increase in age may also be interpreted as a signal of increased appropriateness for ED admissions (patients that access ED to avoid GP gatekeeping are usually younger [11]).
The general conclusion that can be drawn from this analysis is that the news about Covid-19 cases and the campaign to avoid accessing ED directly may have backfired: it has not stopped patients with Covid-19 symptoms to drive to hospital, but it might have delayed access for some patients, which may have undermined their health. This is especially true for patients with acute cardiovascular conditions as some new evidence seems to suggest [16,[25], [26], [27]]. This result is consistent with the literature showing that the delay in health care may lead to severe consequences [27,28].
After the lockdown, in Phase 2, the number of accesses was still lower than usual, the rate of hospital admissions decreased. The overall effect was that 9.5 daily admissions to hospital through the ED were still missing, a result in line with what observed for paediatric accesses [29]. This decrease cannot be due to objectively justifiable safety concerns (the number of Covid-19 was negligible): the new protocols adopted to keep the ED a safe place might have created a long-lasting change in the demand for ED accesses, something that will have to be carefully monitored in the future.
5. Conclusions
The Covid-19 pandemic has changed the focus of the discussion around ED accesses from overcrowding and demand management [[30], [31], [32]] to the analysis of the causes for the observed drop since the pandemic and its effects on patients health.
In this article, we have analysed access to the ED of Spedali Civili of Brescia, a large teaching hospital in one of the most hit provinces in Italy by the Covid-19 pandemic. The delay between the announcement of the first case and the explosion of the pandemic allows to study the reactions of patients to such bad news and to observe their behaviour during the lockdown and during the weeks leading to “business as usual”. The news about the diffusion of the contagion, coupled with the appeals to use alternative emergency services to access ED by Covid-19 patients may have generated fear that have discouraged access. However, discouragement may not have always worked in the right direction. A large number of patients with Covid-19 symptoms have accessed ED directly anyway, either because they have not followed the advice or because they have tried to no avail. In fact, the emergency lines were understaffed and the ambulance services were not sufficient to meet all the requests [33]. Our analysis confirms that the overall governance system does not have proved to be enough resilient [34,35]. From a policy perspective, this calls for a change in hospital organization for a timely distribution of supplies.
At the same time, some non-Covid-19 patients have instead given up visiting ED. The new safety protocols reduce the objective risk of contagion and should have restored patients’ perception of the ED as a safe place. Nevertheless, at the end of June, accesses were still below average across all priority codes. The initial fear generated by the pandemic or the increased waiting times may still refrain some individuals to access ED. Our data analysis suggests that a non-negligible fraction of the discouraged patients is likely to need complex treatments that require admission to hospital ward. It is therefore important to implement policies to reassure further the population on the safety of the ED and to shorten the waiting times to safeguard as much as possible patients with serious conditions not correlated with the COVID disease.
CRediT authorship contribution statement
Emirena Garrafa: Conceptualization, Methodology, Writing - review & editing. Rosella Levaggi: Conceptualization, Methodology, Writing - review & editing. Raffaele Miniaci: Conceptualization, Methodology, Investigation, Writing - review & editing. Ciro Paolillo: Conceptualization, Methodology, Data curation, Writing - review & editing.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgments
The authors would like to thank the reviewers and the Editor for their helpful comments. The usual disclaimer applies.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.healthpol.2020.10.006.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Vedovetto A., Soriani N., Merlo E., Gregori D. The burden of inappropriate emergency department pediatric visits: why Italy needs an urgent reform. Health Services Research. 2014;49:1290–1305. doi: 10.1111/1475-6773.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality . US Department of Health & Human Services; 2018. Preventable emergency department visits. [Google Scholar]
- 3.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. The American Journal of Managed Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 4.Schuur J.D., Venkatesh A.K. The growing role of emergency departments in hospital admissions. The New England Journal of Medicine. 2012;367:391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 5.Morganti K.G., Bauhoff S., Blanchard J.C., Abir M., Iyer N., Smith A., et al. The evolving role of emergency departments in the United States. Rand Health Quarterly. 2013;3:3. [PMC free article] [PubMed] [Google Scholar]
- 6.Coster J.E., Turner J.K., Bradbury D., Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Academic Emergency Medicin. 2017;24:1137–1149. doi: 10.1111/acem.13220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fishman J., McLafferty S., Galanter W. Does spatial access to primary care affect emergency department utilization for nonemergent conditions? Health Services Research. 2018;53:489–508. doi: 10.1111/1475-6773.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krämer J., Schreyögg J. Substituting emergency services: primary care vs. hospital care. Health Policy (New York) 2019 doi: 10.1016/j.healthpol.2019.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Wong C.Y., Hall J. Does patients’ experience of general practice affect the use of emergency departments? Evidence from Australia. Health Policy (New York) 2018 doi: 10.1016/j.healthpol.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 10.MacKichan F., Brangan E., Wye L., Checkland K., Lasserson D., Huntley A., et al. Why do patients seek primary medical care in emergency departments? An ethnographic exploration of access to general practice. BMJ Open. 2017:7. doi: 10.1136/bmjopen-2016-013816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levaggi R., Montefiori M., Persico L. Speeding up the clinical pathways by accessing emergency departments. The European Journal of Health Economics. 2020;21:37–44. doi: 10.1007/s10198-019-01107-5. [DOI] [PubMed] [Google Scholar]
- 12.Leporatti L., Ameri M., Trinchero C., Orcamo P., Montefiori M. Targeting frequent users of emergency departments: prominent risk factors and policy implications. Health Policy (New York) 2016;120:462–470. doi: 10.1016/j.healthpol.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Botelho A., Dias I.C., Fernandes T., Pinto L.M.C., Teixeira J., Valente M., et al. Overestimation of health urgency as a cause for emergency services inappropriate use: insights from an exploratory economics experiment in Portugal. Health & Social Care in the Community. 2019 doi: 10.1111/hsc.12720. 0. [DOI] [PubMed] [Google Scholar]
- 14.Propper C., Stoye G., Zaranko B. The wider impacts of the coronavirus pandemic on the NHS. Fiscal Studies. 2020 doi: 10.1111/1475-5890.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cereda D., Tirani M., Rovida F., Demicheli V., Ajelli M., Poletti P., et al. 2020. The early phase of the COVID-19 outbreak in Lombardy, Italy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masroor S. Collateral damage of COVID-19 pandemic: delayed medical care. Journal of Cardiac Surgery. 2020;35:1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odone A., Delmonte D., Scognamiglio T., Signorelli C. COVID-19 deaths in Lombardy, Italy: data in context. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levaggi R., Montefiori M. Definition of a prospective payment system to reimburse emergency departments. BMC Health Services Research. 2013:13. doi: 10.1186/1472-6963-13-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Casagranda I., Coen D., Paolillo C., Cavazza M., Carvellin G., Bellone A., et al. Changing emergency department and hospital organization in response to a changing epidemic. Emergency Care Journal. 2020:16. doi: 10.4081/ecj.2020.8969. [DOI] [Google Scholar]
- 20.Azmat G., Petrongolo B. Gender and the labor market: what have we learned from field and lab experiments? Labour Economics. 2014;30:32–40. doi: 10.1016/j.labeco.2014.06.005. [DOI] [Google Scholar]
- 21.Jin J.M., Bai P., He W., Wu F., Liu X.F., Han D.M., et al. Gender differences in patients with COVID-19: focus on severity and mortality. Frontiers in Public Health. 2020;8 doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Comelli I., Scioscioli F., Cervellin G. Impact of the covid-19 epidemic on census, organization and activity of a large urban emergency department. Acta Biomedica. 2020;91:45–49. doi: 10.23750/abm.v91i2.9565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pikoulis E., Solomos Z., Riza E., Puthoopparambil S.J., Pikoulis A., Karamagioli E., et al. Gathering evidence on the decreased emergency room visits during the coronavirus disease 19 pandemic. Public Health. 2020;185:42–43. doi: 10.1016/j.puhe.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giamello J.D., Abram S., Bernardi S., Lauria G. The emergency department in the COVID-19 era. Who are we missing? European Journal of Emergency Medicine. 2020 doi: 10.1097/MEJ.0000000000000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacMillan C. 2020. Hospitals report fewer heart attacks and strokes amid COVID-19.https://www.yalemedicine.org/stories/hospitals-covid-fears/ [Accessed May 25, 2020] [Google Scholar]
- 26.Bakker J. 2020. Lives at risk due to 50% drop in heart attack A&E attendances.https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-outbreak [Accessed May 25, 2020] [Google Scholar]
- 27.Baldi E., Sechi G.M., Mare C., Canevari F., Brancaglione A., Primi R., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. The New England Journal of Medicine. 2020 doi: 10.1056/nejmc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Richards M., Anderson M., Carter P., Ebert B.L., Mossialos E. The impact of the COVID-19 pandemic on cancer care. Nature Cancer. 2020;1:565–567. doi: 10.1038/s43018-020-0074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. The Lancet Child & Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sivey P. Should I stay or should I go? Hospital emergency department waiting times and demand. Health Economics. 2017;27:e30–42. doi: 10.1002/hec.3610. [DOI] [PubMed] [Google Scholar]
- 31.Montefiori M., di Bella E., Leporatti L., Petralia P. Robustness and effectiveness of the triage system in the pediatric context. Applied Health Economics Health Policy. 2017;15:795–803. doi: 10.1007/s40258-017-0340-z. [DOI] [PubMed] [Google Scholar]
- 32.Cremonesi P., di Bella E., Montefiori M., Persico L. The robustness and effectiveness of the triage system at times of overcrowding and the extra costs due to inappropriate use of emergency departments. Applied Health Economics Health Policy. 2015;13:507–514. doi: 10.1007/s40258-015-0166-5. [DOI] [PubMed] [Google Scholar]
- 33.Zoli A., Pagliosa A., Sechi G.M., Bergonzi L. 2020. Covid-19 triage filter in Lombardy Region, Italy. Bruxelles, Belgium. [Google Scholar]
- 34.Costa-Font J., Levaggi R., Turati G. Resilient managed competition during pandemics: lessons from the Italian experience during COVID-19. Health Economics, Policy and Law. 2020 doi: 10.1017/S1744133120000353. e-pub ahea:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Armocida B., Formenti B., Ussai S., Palestra F., Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020;5:e253. doi: 10.1016/S2468-2667(20)30074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.