Abstract
Background
Optimal personal protective equipment (PPE) preparedness is key to minimize healthcare workers (HCW) infection with COVID-19. This two-phase survey evaluated PPE preparedness (adherence to Ministry of Health India (MoH) PPE-recommendations; HCW-training; PPE-inventory; PPE-breach management) in Indian intensive care units (ICU).
Materials and methods
The phase 1 survey was distributed electronically to intensivists from 481 Indian hospitals between March 25, 2020, and April 06, 2020, as part of a multinational survey. Phase 2 was repeated in 320 Indian hospitals between April 20, 2020, and April 30, 2020.
Results
Response rate was 25% from 22 states. PPE practice varied between states and between private, government, and medical colleges. Between phase 1 and phase 2, all aspects of PPE training improved: donning/doffing 43% vs 66%, respectively; p value <0.01); safe waste disposal practices (38% vs 52%; p value = 0.09); intubation training (18% vs 31%; p value = 0.05); and transport (18% vs 31%; p value = 0.05). Perception of confidence for adequate PPE-training improved from 39 to 53% (p value = 0.26). In all, 47 to 60% ICUs adhered to MoH recommendations. Wearing N95-masks at all times increased from 47 to 60% (p value = 0.89). Very few ICUs provided quantitative/qualitative N95 masks fit testing (12% vs 29%; p value <0.01). Low-cost practices like “buddy-system” for donning-doffing (27% vs 44%; p value = 0.02) and showering after PPE breach (10% vs 8%; p value = 0.63) were underutilized. There was reluctance to PPE reuse. In all, 71% were unaware/diffident about PPE inventory.
Conclusion
Despite interstate variability, most ICUs conformed to MoH recommendations. This survey conducted during initial pandemic phase demonstrated improved PPE preparedness uniformly across India with scope for further improvement. We suggest implementation of quality improvement measures to improve pandemic preparedness and minimize HCW infection rates, focused on regular PPE training, buddy system, and PPE-breach management.
How to cite this article
Haji JY, Subramaniam A, Kumar P, Ramanathan K, Rajamani A. State of Personal Protective Equipment Practice in Indian Intensive Care Units amidst COVID-19 Pandemic: A Nationwide Survey. Indian J Crit Care Med 2020;24(9):809–816.
Keywords: COVID-19, Donning-doffing, Healthcare workers, HCW infections, Personal protective equipment preparedness, Personal protective equipment training, SARS-CoV-2
Introduction
The coronavirus disease-2019 (COVID-19) pandemic in India has witnessed a surge in healthcare worker (HCW) infections even as the pandemic may be yet to peak.1 Since the severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) virus is highly transmissible through droplet and airborne routes, intensive care unit (ICU) HCWs are at particularly high risk due to their exposure to aerosol-generating procedures (AGPs).2,3 To prevent HCW infections, a robust culture of pandemic preparedness, defined by adherence to guidelines, HCW-training, procuring PPE stocks, and responding appropriately to PPE breach is essential. A comprehensive position statement issued by the Indian Society of Critical Care Medicine outlines the dos and don'ts while handling COVID-19 patients.4 In a recent survey of intensivists from ICUs in six Asia-Pacific countries conducted by our group, the level of pandemic preparedness in Indian ICUs was compared to the other countries.5 Since India is a unique country comprising of heterogeneous health systems, we conducted this follow-up survey in Indian ICUs to help evaluate this issue better and propose solutions to improve PPE preparedness that may potentially minimize HCW infections.
Materials and Methods
The survey methodology is provided in detail in our original survey.5 Following ethical approval, the survey weblink was distributed by e-mail, text message, and WhatsApp to qualified intensivists working in hospitals having a 24/7 Emergency/Casualty Department and an ICU capable of mechanically ventilating patients for >24 hours. In phase 1, it was sent to intensivists across six Asia-Pacific countries, including India between March 25, 2020, and April 06, 2020. The phase 2 survey was distributed to HCWs only in Indian hospitals between April 20, 2020, and April 30, 2020. Two reminders were sent 3 days apart. Only one HCW per hospital could respond. Participation was voluntary, with no incentives offered. For this manuscript, only the responses from Indian HCWs were analyzed. Survey responses were exported from the online survey platform and analyzed using SPSS Statistics Version 26 (IBM), using the Ministry of Health India (MoH) PPE guidelines as the reference standard.6 The data analysis was primarily descriptive and reported as percentages of valid responses. The responses from Indian HCWs between phases 1 and 2 were compared using Fisher's exact test with a 2-tailed α-level of 5% considered significant (p value < 0.05).
Results
A total of 204 responses were received, with 125/481 in phase 1 (26%) and 79/320 (25%)—overall, 25% response rate. Responses were obtained from 22 of 26 Indian states (Table 1). The survey respondents were intensivists (61%), anesthetists (28%), ICU nurses (8%), and emergency department doctors and nurses (3%). Most respondents were from private hospitals (76%), the other quarter comprised of respondents from Government Hospitals (17%) and Private Medical Colleges (7%) (Suppplementary Table 1). All results below are presented as a comparison of the proportion of responses obtained in phase 1 vs phase 2 (expressed in percentages).
Table 1.
Distribution of survey responders across states and union territories
| State/territory | Overall, n (%) | Phase 1, n (%) | Phase 2, n (%) |
|---|---|---|---|
| Karnataka | 42 (20.6) | 27 (21.6) | 15 (19) |
| Maharashtra | 27 (13.2) | 16 (12.8) | 11 (13.9) |
| Tamil Nadu | 20 (9.8) | 11 (8.8) | 9 (11.4) |
| Delhi | 22 (10.8) | 11 (8.8) | 11 (13.9) |
| Gujarat | 18 (8.8) | 10 (8.0) | 8 (10.1) |
| Uttar Pradesh | 11 (5.4) | 8 (6.4) | 3 (3.8) |
| Kerala | 10 (4.9) | 6 (4.8) | 4 (5.1) |
| Haryana | 8 (3.9) | 6 (4.8) | 2 (2.5) |
| Odisha | 8 (3.9) | 3 (2.4) | 5 (5.1) |
| West Bengal | 8 (3.9) | 7 (5.6) | 1 (1.3) |
| Andhra Pradesh | 5 (2.45) | 3 (2.4) | 2 (2.5) |
| Madhya Pradesh | 4 (2.0) | 2 (1.6) | 2 (2.5) |
| Rajasthan | 4 (2.0) | 2 (1.6) | 2 (2.5) |
| Telangana | 4 (2.0) | 3 (2.4) | 1 (1.3) |
| Chhattisgarh | 2 (1.0) | 2 (1.6) | 0 |
| Punjab | 2 (1.0) | 1 (0.8) | 1 (1.3) |
| Andaman Nicobar Islands | 1 (0.5) | 1 (0.8) | 0 |
| Assam | 1 (0.5) | 0 | 1 (1.3) |
| Bihar | 2 (1.0) | 0 | 1 (1.3) |
| Himachal Pradesh | 1 (0.5) | 1 (0.8) | 0 |
| Jharkhand | 2 (1.0) | 2 (1.6) | 0 |
| Puducherry | 1 (0.5) | 1 (0.8) | 0 |
| Tripura | 1 (0.5) | 0 | 1 (1.3) |
| Grand total | 204 | 125 | 79 |
Training of HCWs in Minimizing the Risk of Acquiring SARS-CoV-2 Infection from Suspected COVID-19 Patients
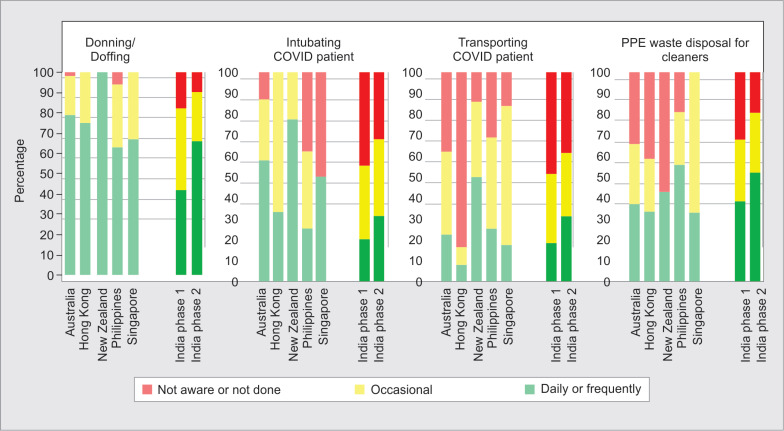
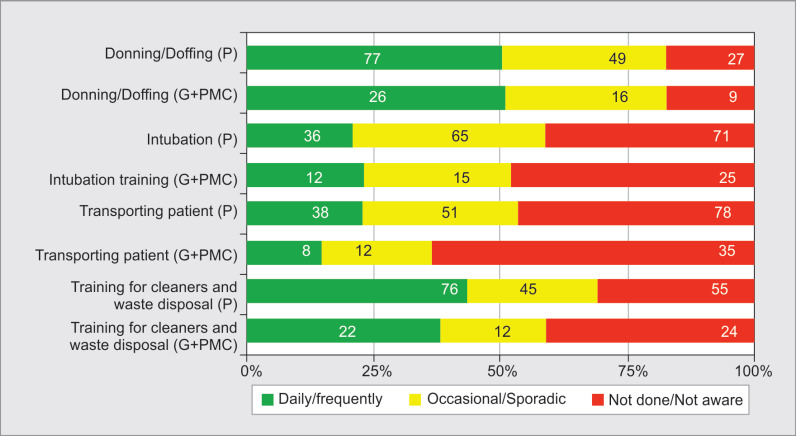
Four aspects of training were evaluated—training in PPE donning and doffing, safe waste disposal, endotracheal intubation, and intrahospital transport. A significant increase was seen in phase 2 in the number of respondents reporting regular training in all these aspects (Table 2): donning and doffing PPE (43% in phase 1 vs 66% in phase 2, p value <0.01); safe waste disposal practices (38% vs 52%; p value =0.09); intubation training for COVID-19 patients (18% vs 31%; p value =0.05); and transport (18% vs 31%; p value = 0.05). Overall, the training pattern was uniform across hospitals in the private, government, and medical colleges (Suppplementary Fig. 1). In comparison to the original Asia-Pacific countries surveyed,5 the PPE training in India improved significantly in phase 2 (Fig. 1).
Table 2.
The responses from Indian HCWs between phases 1 and 2 compared using Fisher's Exact Test with a 2-tailed alpha-level of 5% considered significant (p < 0.05)
| Phase 1, n (%) | Phase 2, n (%) | p value | |
|---|---|---|---|
| HCW PPE training | |||
| Donning and doffing | 54 (43) | 52 (66) | <0.001 |
| Intubation practices | 23 (18) | 24 (31) | 0.05 |
| Intrahospital patient transport | 23 (18) | 24 (31) | 0.05 |
| Safe waste PPE disposal | 48 (38) | 41 (52) | 0.09 |
| PPE practices | |||
| N95 masks at all times | 59 (47) | 47 (60) | 0.89 |
| N95 only for AGPs | 46 (37) | 22 (28) | 0.23 |
| Regular fit-testing | 15 (12) | 23 (29) | <0.01 |
| Eye protection | 84 (67) | 55 (70) | 0.76 |
| Coverall* | 69 (55) | 62 (78) | <0.01 |
| Double gloving | 66 (53) | 53 (67) | 0.08 |
| Observer/buddy system | 34 (27) | 35 (44) | 0.02 |
| PPE inventory | 21 (17) | 24 (31) | 0.03 |
| PPE breach | |||
| Unsure what PPE breach means | 64 (51) | 1 (1.3) | <0.01 |
| Advice of post-breach care | 15 (12) | 11 (14) | 0.84 |
| Advice of showering post-exposure | 13 (10) | 6 (8) | 0.63 |
| Perception of safety and confidence | |||
| Adequacy of PPE training | 49 (39) | 42 (53) | 0.06 |
| Concerns that PPE practice is suboptimal | 66 (53) | 34 (43) | 0.21 |
Coverall means full body suit
HCW, healthcare worker; PPE, personal protective equipment; AGP, aerosol-generating procedure
Fig. 1.
Training patterns in India in phase 1 and phase 2 survey compared to other Asia-Pacific countries (Australia, New Zealand, Hong Kong, Singapore and Philippines)5 which were surveyed in phase 1. Four main domains (1) donning/doffing (2) Intubation (3) Transporting (4) Training for cleaners and waste disposal
PPE Practices
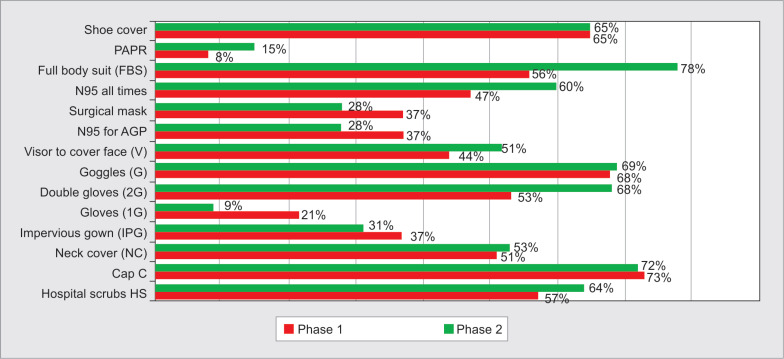
The proportion of respondents who reported a practice that conformed to the MoH guidelines (which recommend donning N95 masks at all times irrespective of AGPs) was 47% in phase 1 vs 60% in phase 2 (p value = 0.89). Other respondents reported using N95 masks for AGPs only (37% in phase 1 vs 28% in phase 2; p value = 0.23). Very few ICUs reported provision of quantitative/qualitative fit testing for N95 masks (12% vs 29%; p value < 0.01). The corresponding numbers for eye-protective goggles, face shields, or both were 67% vs 70% (p value = 0.76); coverall (full body suits)/gowns 55% vs 78%; p value < 0.01); and head cover and shoe cover 65% in both phases. Double gloving was reported by 53% vs 67%; p value = 0.08 (Fig. 2).
Fig. 2.
Personal protective equipment usage pattern compared between two phases of the survey
PPE Reuse
This question was only explored in phase 2, with only 20% of respondents reporting that they would consider reusing face shields and/or N95 masks after appropriate sterilization. In all, 26% of respondents were unaware of any policy on reusing PPE (Suppplementary Table 2).
Other Aspects of PPE Practices
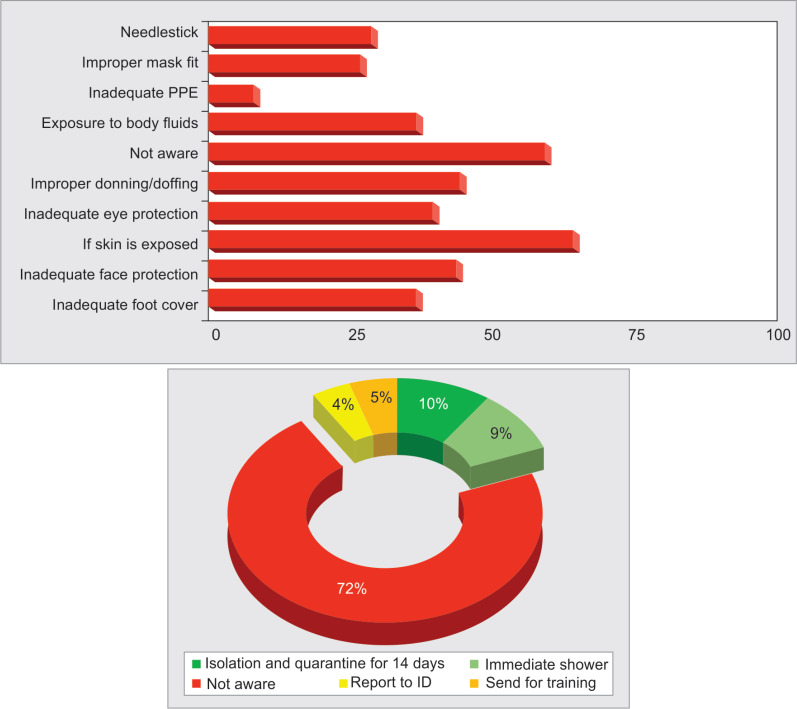
There were a significant number of respondents who reported being unaware of what constitutes a PPE breach and/or the policies for a breach in their hospitals in phase 1 (49%). In phase 2, we changed the answer format to give the respondents options for PPE breach (Fig. 3). The proportion of hospitals that employed an observer/buddy system regularly to scrutinize the donning and doffing process increased from 27% to 44% (p value = 0.02) (Table 2). However, in both phases, very few respondents reported having clear advice regarding showering after patient exposure (10.4% vs 8%, p value = 0.63) (s Table 1) or PPE-breach (12% vs 14%, p value = 0.84) (Fig. 3).
Fig. 3.
PPE breach and reporting of PPE breach
PPE Inventory
When specifically explored about respondents’ confidence if their hospital's PPE stock inventory would last for three patients for a week, most respondents (71%) reported that they were either unaware of their PPE stock or that their current stock would not last more than a week. Only 17% of respondents in phase 1 and 31% in phase 2 reported having enough stock to manage >3 COVID-19 patients for at least 1 week (p value = 0.03).
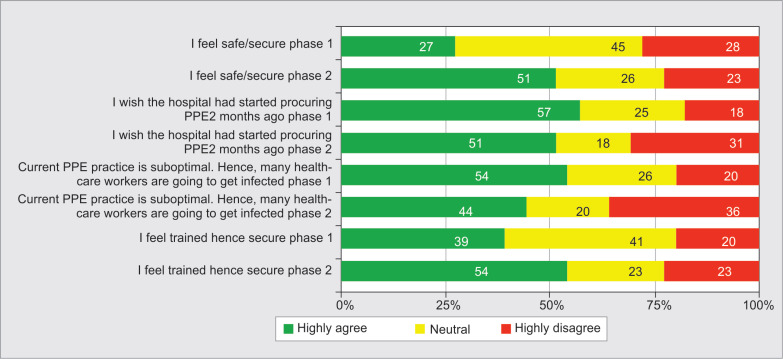
Perception of Confidence
The proportion of respondents who felt adequately trained in PPE practices increased from 39% in phase 1 to 53% in phase 2 (p value = 0.26). Correspondingly, the proportion of respondents who reported feeling that they or their colleagues may get infected with SARS-CoV-2 due to suboptimal PPE practices decreased from 53 to 43% (p value = 0.06) (Fig. 4).
Fig. 4.
Perception of safety and confidence in training and PPE stock between two phases of the survey
Discussion
This study was initiated at a time when many ICUs in India were gearing up to prepare for the emerging pandemic. It highlighted a mix of positive findings and areas of improvement for PPE preparedness, across both private and government sectors. Encouragingly, the PPE usage practices reported by most clinicians conformed to the MoH guidelines in both phases, suggesting a high level of awareness of the principles behind these guidelines. While the level of training in phase 1 was suboptimal in most institutions, a statistically significant improvement was observed in the 2 weeks separating phases 1 and 2, again suggesting that the hospital administrators were becoming cognizant of the importance of training and preparedness (Fig. 2). However, despite this improvement, the responses from a large proportion of respondents in phase 2 suggested that their hospitals’ preparedness remained suboptimal. Therefore, it is conceivable that HCW infection rates may further worsen, as the pandemic continues to surge across the country. Nevertheless, ever since the survey was conducted, with furthermore worldwide surge coupled with rise in cases in India, there has been increased emphasis on improved resource allocation of PPE with better material.
The fact that 40% of respondents did not report employing basic PPE practices, such as double gloves, eye protection, hospital scrubs, and shoe covers, is worrisome. Several studies have proven less scope of breach and soiling during PPE-doffing when double gloves are used.7 As the SARS-CoV-2 virus is widely distributed on floors and other surfaces,7 these low-cost measures may aid in minimizing the rates of fomite spread.
It was encouraging to observe the HCW mind-set of the improved frequency of PPE-training across the two time periods. However, despite the COVID-19 caseload exponentially rising across all major cities, it is concerning that less than a third of Indian HCWs were getting only occasional or sporadic PPE-training in donning and doffing even in late-April given that PPE training is considered as one of the effective mechanisms for pandemic preparedness.8 This was evenly spread across both government and private hospitals.
In line with this trend, many respondents were unaware of PPE-breach identification and reporting protocols.9 For instance, only a fifth reported undergoing fit testing, but very few respondents considered improper N95 mask fit as a PPE breach. The HCW was not comfortable in reusing N95 masks. The recent international guidelines recommend against extended wear, as it increases the risk of self-inoculation and cross-contamination.10 Moreover, mask fit and filtration capabilities degrade with extended use.10
Similarly, very few ICUs employed low-cost practices, such as showering after a potential breach, or the observer/buddy system, which is recommended by the MoH.10 It is not unreasonable to surmise that implementing such basic low-cost practices may be effective in reducing HCW infection rates substantially. Arguably, the best way to achieve this is optimal PPE training. Unfortunately, this was also suboptimal in several ICUs, with one-third to two-third of ICUs still reporting inadequate training processes even in phase 2. Simulation studies have shown a high incidence of HCW contamination during the doffing process.11 Regular dedicated simulation training has been shown to be effective in minimizing contamination and also improves HCW confidence.11
This survey demonstrated a high level of HCW anxiety regarding the safety of themselves and/or their colleagues. This was in line with recent publications that showed that >90% of HCWs had some element of anxiety.12,13 This may have been exacerbated by the scale of this unprecedented pandemic, especially with rising numbers of HCW infections.14 The lack of preparedness extended to PPE-stock management, with a large proportion of respondents being either unaware or not having enough stock for even 3 COVID-19 patients, despite India being the second largest producer of PPE in the world.15 Respondents felt that their hospital should have started procuring PPE in advance.
The strength of the study includes the following: First, this was the first survey performed on Indian HCWs to evaluate PPE practices in their local institutions. Second, the study methodology followed a robust process to design, test, and distribute the questionnaire to a range of government and private institutions across India. Third, to keep it relevant to India, we followed the MoH India PPE guidelines as the reference standard. Fourth, various aspects of PPE preparedness were explored. Fifth, responses were obtained from almost every state/Union Territory. Finally, the survey effectively captured the impact created by the surging pandemic. During phase 1 of the survey, India had only 2,000 confirmed cases, confined to very few states. However, during phase 2, this had increased exponentially to ∼35,000 cases across India.
The limitations of the study included a low response rate of 25%. However, in the context of an ongoing pandemic, we believe that this response rate is reasonable. Training in major AGPs, such as cardiopulmonary resuscitation, prone ventilation, and other airway procedures, such as extubation, tracheostomy, and bronchoscopy, were not explored, mainly to keep the response time feasible. Inherent to any survey, responses to questions on perceived safety and PPE stocks may be prejudiced by personal beliefs or speculations. However, the aim of this survey was to highlight the uncertainty amongHCWs and methods to improve conditions and address this anxiety. Finally, although the link between PPE preparedness and HCW infections is plausible, no study has established a causal effect. This will require a scientific evaluation of the magnitude of HCW infections with SARS-CoV-2, including any associations with the PPE-preparedness in their local hospitals. It may be timely to undertake such an evaluation, as the pandemic has surged exponentially in India since the completion of phase 2 of this survey.
We suggest that the following proposals summarized in Table 3 to be urgently implemented at various levels to provide an immediate improvement in PPE preparedness. At the level of the ministry, we suggest that the MoH promote consistent mandatory training practices across the country. Also, the MoH should consider adopting other international practices such as PPE-inventory to best facilitate resource allocation.16 Reassurance from policy makers in stock, PPE quality and reporting, and post-exposure policies would all help improve HCW productivity in stressful situations.17 We strongly recommend an immediate commencement of PPE training in every hospital and/or ICU. The infection prevention guidelines should be regularly updated as the pandemic progresses with time. Other key strategies include implementation of low-cost measures, such as buddy systems and cultivate a safety-culture environment that improves the HCW well-being during such pandemics.17 Infection prevention goes beyond PPE-use and requires systematic measures to improve preparedness and safety culture to ensure the safety and well-being of HCWs during such pandemics.17 While PPE provides immediate physical and psychological safety to the HCWs, incorporation of engineering and administrative solutions will aid in bringing in an enduring culture of safety in health systems, thereby improving HCW morale and well-being.18,19
Table 3.
Recommendations for better PPE practice
| PPE6 | As per MoH—full body suit/gown/PAPR |
| Hospital scrubs at all times | |
| Impervious plastic apron at all times | |
| N95 at all times | |
| Double gloves at all times | |
| Cap, shoe cover at all times | |
| Strengthened logistics and medical supplies to ensure adequate PPE | |
| Training8 | Mandatory training of PPE use—when, what, how, how long, limitations, care, maintenance, disposal. |
| Retraining | |
| If inadequacy in employees PPE knowledge detected. | |
| If there is change in employment | |
| If there is change in PPE | |
| Onsite training by infection control with didactic lecture, practical sessions in donning doffing and disposal. | |
| Simulations in performing AGPs while in PPE (intubation, transport, waste disposal) | |
| Online resources such as training videos created by the MoH | |
| PPE Breach9 | Prevention |
| Mandatory fit testing | |
| Buddy system | |
| Showering after patient exposure | |
| Audits of compliance check | |
| Retraining | |
| Minimal patient contact by remote monitoring and tele medicine | |
| Robust mechanisms to minimize aerosol-generation and exposure during aerosol-generation procedures | |
| In case breach | |
| Reporting to infection control | |
| Surveillance for symptoms | |
| Quarantine | |
| Re-induction | |
| Emergency surveillance system to monitor all exposed HCWs, contributing to prompt detection, effective triage, and isolation of infected HCW |
MoH, ministry of health, India; PPE, personal protective equipment; PAPR, powered air-purifying respirator; AGP, aerosol-generating procedure; HCWs, healthcare workers
Conclusion
The survey, conducted in the early phase of COVID-19 pandemic in India, found that most ICUs in India largely conformed to the MoH guidelines. Many hospitals implemented appropriate measures to improve their PPE preparedness with time. However, there is still scope for improvement across several domains, some of which may be coordinated at the governmental level, and others at local levels. We suggest that quality improvement measures be urgently initiated to improve pandemic preparedness and minimize HCW infection rates. The focus should be on regular training on proper donning/doffing, fit testing, transporting of COVID-19 patients, and safe cleaning/disposal practices to ensure safe PPE use. Low-cost approaches such as buddy-system and postexposure/patient contact shower practices should also be adopted. HCWs should be educated in recognizing and reporting breach of PPE and given retraining if any lapse in PPE practice or change in PPE.
Supplmentary Fig. 1.
Training in (1) donning/doffing; (2) Intubation; (3) Transporting; (4) Training for cleaners and waste disposal and comparison between private (P) and government run institutions. (G = government hospitals/medical colleges + PMC = private medical colleges)
Supplementary Table 1.
Distribution of respondents across private and government sector and their designation
| Private | 76% |
| Government | 17% |
| Private medical college | 7% |
| Designation of responders | |
| Intensivist | 61% |
| Anesthetist | 28% |
| Nurse | 8% |
| Emergency room doctor/nurse | 3% |
Supplementary Table 2.
Safety measures for decreasing exposure and health risk to HCWs on COVID duty
| Family visitation/communication strategies for COVID patients | |
|---|---|
| No family visit allowed | 54% |
| Video conferencing | 17% |
| Brief visits in full PPE | 6% |
| Not decided/no changes | 23% |
| Showering/shampooing after caring for a COVID patient | |
| Only if PPE was breached | 12% |
| Immediately after every single patient-contact episode | 8% |
| Only at the end of your shift/after reaching home | 55% |
| No advice/guideline given | 20% |
| Limited bathrooms available | 5% |
| “Buddy-system” mandatory every time to check donning and doffing | |
| Mandatory every time to check donning and doffing | 33% |
| To check donning and doffing, but not always | 15% |
| Not mandatory (ad hoc) | 44% |
| Never | 8% |
| PPE re-use | |
| Never reuse | 72% |
| Reuse simple surgical mask | 20% |
| Reuse N95 | 18% |
| Wash and reuse face shields | 23% |
| Reuse masks and face shields after ETO/plasma sterilization | 23% |
| Specialized “COVID intubation team” | |
| Yes—anesthetists | 53% |
| Yes—senior intensivist | 14% |
| No specified airway team | 33% |
ACKNOWLEDGMENTS
Dr Jumana Haji would like to acknowledge Dr Swati Rajagopal Consultant-Infectious Diseases and Travel Medicine at Aster CMI hospital and Dr Rajeshwari K. G. consultant Microbiology at Aster CMI hospital for their kind evaluation of the article. Dr Arvind Rajamani would like to acknowledge Dr Kiran Shekar Adult Intensive Care Services, the Prince Charles Hospital Brisbane, Queensland, Australia; Dr Jinghang Luo Basic Physician Trainee Western Health, VIC; Shailesh Bihari ICU consultant, Flinders university and Flinders Medical center, Bedford Park SA 5042; Dr Wai Tat Wong FCICM Clinical Professional Consultant The Chinese University of Hong Kong; Ms Navya Gullapalli Medical Student Final Year Medical Student Monash University, Clayton VIC; Dr Markus Renner Markus Senior staff specialist Dunedin Hospital, SDHB; Dr Claudia Maria Clinical Fellow Makati Medical Center, Philippines For their work on the Asia Pacific PPE survey paper along with India.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.S D. 10 per cent cases linked to hospital infections in Mumbai, point to lack of stringent protocols. Times of India 2020 April 10th 2020.
- 2.Morawska L, Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta Y, Chaudhry D, Abraham OC, Chacko J, Divatia J, Jagiasi B, et al. Critical care for COVID-19 affected patients: osition statement of the Indian Society of Critical Care Medicine. Indian J Crit Care Med. 2020;24(4):222–241. doi: 10.5005/jp-journals-10071-23395. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajamani A, Subramaniam A, Shekar K, Haji J, Luo J, Bihari S, et al. Variations in personal protective equipment preparedness in intensive care units during the COVID-19 pandemic: a survey of Asia-pacific countries. medRxiv. 2020;2020 [Google Scholar]
- 6.Services MoHaFWDGoH. Novel Coronavirus Disease 2019 (COVID-19): Guidelines on rational use of Personal Protective Equipment. Services DoH, ed.; India: 2020. [Google Scholar]
- 7.Casanova LM, Rutala WA, Weber DJ, Sobsey MD. Effect of single-vs double-gloving on virus transfer to health care workers’ skin and clothing during removal of personal protective equipment. Am J Infect Control. 2012;40(4):369–374. doi: 10.1016/j.ajic.2011.04.324. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Administration OSaH. PPE for Emergency Response and Recovery Workers. Labor USDo, ed.; United States: 2020. [Google Scholar]
- 9.WHO. Risk assessment and management of exposure of health dare workers in the context of COVID-19. World Health Organisation.; 2020. WHO: WHO; [Google Scholar]
- 10.Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46(7):1303–1325. doi: 10.1007/s00134-020-06092-5. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fogel I, David O, Balik CH, Eisenkraft A, Poles L, Shental O, et al. The association between self-perceived proficiency of personal protective equipment and objective performance: an observational study during a bioterrorism simulation drill. Am J Infect Control. 2017;45(11):1238–1242. doi: 10.1016/j.ajic.2017.05.018. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murthy PR, Venkatesha Gupta GK, Ajith Kumar AK. Is anxiety a rising concern during COVID-19 pandemic among healthcare workers? Indian J Crit Care Med. 2020;24(5):369–370. doi: 10.5005/jp-journals-10071-23434. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety and perceived mental healthcare need in indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaishya RVA. Protect our healthcare workers: rapid response: “the plight of health care workers in india during COVID-19 pandemic. BMJ. 2020. p. 369.
- 15.Yaday N. India's PPE Industry: How COVID-19 Demonstrated Untapped Local Production Capacity. India Briefing; 2020.
- 16.Australia and New Zealand Critial Health Resource Information System. 2020. https://chris.health.gov.au/#!/portal/home.) https://chris.health.gov.au/#!/portal/home.) (Accessed July 2nd, 2020, at.
- 17.Subramaniam A, Reddy M, Zubarev A, Kadam U, Lim ZJ, Anstey C, et al. Development and validation of a tool to appraise guidelines on SARS-CoV-2 infection prevention strategies in healthcare workers. medRxiv 2020. 2020. DOI: [DOI] [PMC free article] [PubMed]
- 18.A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators [published correction appears in JAMA 1996 Apr 24;275(16):1232]. JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 19.Barratt R, Shaban RZ, Gilbert GL. Characteristics of personal protective equipment training programs in Australia and New Zealand hospitals: a survey. Infect Dis Health. 2020. DOI: [DOI] [PMC free article] [PubMed]