Abstract
COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been shown to cause multisystemic damage. We undertook a systematic literature review and comprehensive analysis of a total of 55 articles on arterial and venous thromboembolism in COVID-19 and articles on previous pandemics with respect to thromboembolism and compared the similarities and differences between them. The presence of thrombosis in multiple organ systems points to thromboembolism being an integral component in the pathogenesis of this disease. Thromboembolism is likely to be the main player in the morbidity and mortality of COVID -19 in which the pulmonary system is most severely affected. We also hypothesize that D-dimer values could be used as an early marker for prognostication of disease as it has been seen to be raised even in the pre-symptomatic stage. This further strengthens the notion that thromboembolism prevention is necessary. We also examined literature on the neurovascular and cardiovascular systems, as the manifestation of thromboembolic phenomenon in these two systems varied, suggesting different pathophysiology of damage. Further research into the role of thromboembolism in COVID-19 is important to advance the understanding of the virus, its effects and to tailor treatment accordingly to prevent further casualties from this pandemic.
Key Words: COVID-19, Thromboembolism, Neurovascular disease, Cardiovascular disease, Immunothrombosis, D-dimer
Introduction
From its beginnings in late 2019 as a severe pneumonia of an unknown etiology in Wuhan China1 to being declared a pandemic by the WHO on 11 March 2020, COVID-19 has caused life altering changes across geographical borders. The disease, caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2), has to date been responsible for more than 800,000 deaths globally, economic upheaval and significant lifestyle changes. When compared to the case fatality rates of previous influenza pandemics, COVID-19 has a rate of 4%2 which is higher than the 1918 Spanish flu and 2009 H1N1 flu pandemic which had fatality rates of 2-3%3 and 0.01%4 respectively. Current evidence lists pneumonia, sepsis, respiratory failure, and acute respiratory distress syndrome (ARDS) as the leading causes of morbidity and death amongst hospitalized patients with COVID-19.5, 6 – 7 However, more recently immune mediated thrombosis has been a consistent finding in a significant number of patients with COVID-19 and understanding its pathophysiological mechanisms and impact on morbidity and mortality in COVID-19 may open new avenues in disease prognostication and management.8
Broadly, the pathogenesis of COVID-19 is through 2 mechanisms; direct invasion into tissue via angiotensin converting enzyme-2 (ACE2) receptors and immune mediated injury.9 , 10 ACE2 is a membrane-associated aminopeptidase expressed in vascular endothelium, renal and cardiovascular tissue, and epithelium of the small intestine and testes.11 A region of the extracellular portion of the ACE2 receptor interacts with high affinity to one of the 4 structural proteins of SARS-CoV-2, the spike protein. This facilitates penetration into the host cell where the virus then replicates, matures and is subsequently released.12 Upon release of the virus, an immune response is triggered leading to a cytokine storm and immunothrombosis.13 The triggering of the immune system in this manner is not unique to SARS-CoV-2 and has been seen in many other viral infections such as severe influenza caused by highly virulent subtypes, namely H1N1 and H5N1, that are characterized by an over induction of the proinflammatory cytokines TNF-, IL-1, IL-6, IL-8, and monocyte chemotactic protein-1 (MCP-1).14, 15 – 16 However what stands out about COVID-19 is the prominence of its thrombotic complications as a result of immunothrombosis with a cumulative incidence as high as 31% in critically ill COVID-19 patients,17 , 18 as compared to 5.9% (7 out of 119 patients) in the 2009 H1N1 pandemic as published in a Canadian study.19 As immunothrombosis has been the proposed cause of these thrombotic complications, this article will focus on immunothrombosis in this ongoing pandemic.
Systematic literature review
We first formulated the research question: “How significant is thromboembolism in the morbidity and mortality of COVID-19?” and focused on answering it. We also focused on thromboembolism with regards to the neurovascular and cardiovascular systems.
We proceeded to select and filter relevant articles from PubMed and Web of Science databases using the keywords “COVID”, ‘SARSCoV2’, ‘Coronavirus’, ‘Arterial thromboembolism’, ‘Venous thromboembolism’, ‘H1N1’ and ‘Spanish Flu’. More than 300 papers were published between 2000–2020 with these keywords and these papers were collected and screened based on their relevance to our research question resulting in 55 articles being deemed suitable for our review.
We thoroughly reviewed these 55 articles looking at arterial and venous thromboembolism in COVID-19 and previous pandemics comparing the similarities and differences between them with a more selective look at the neurovascular and cardiovascular systems.
Immunothombosis
Immunothrombosis occurs following the cytokine storm brought on by triggers such as infection. It is a process from which thrombi form as a result of interaction between the innate immune effector systems (such as monocyte/macrophages and neutrophils and the complement system), platelets and coagulation factors.13 Disseminated intravascular coagulation (DIC) is considered an advanced stage of immuno-thrombosis, where the immune system is no longer able to restrict intrinsic associated molecular patterns and immuno-thrombosis becomes overwhelming. In this stage, thrombosis is detrimental because it can cause multiple organ failure.20 The diagnosis of DIC is established by the identification of laboratory abnormalities. Prothrombin time (PT), activated partial thromboplastin time (aPTT), platelet count, fibrinogen concentration, fibrin degradation product (FDP) and D-dimer measurements have been the classical assays used in the recognition, diagnosis and monitoring of DIC and forms part of the International Society of Thrombosis and Hemostasis (ISTH) scoring system for DIC.21 Among these laboratory investigations, elevation in fibrin marker (D-dimers and FDP) confers the highest points in the diagnostic algorithm for DIC proposed by ISTH. D-dimer, which is degraded cross-linked fibrin, has been found to be elevated in patients with COVID-19 especially at higher levels of disease severity, however data regarding FDP levels in these patients have not been explored.22
When compared to DIC of other etiologies such as malignancies or sepsis, low platelet count and prolonged PT are rarely seen in COVID related coagulopathy. Martin-Rojas et al demonstrated a very low percentage (5.3%) of patients with COVID-19 that met the ISTH criteria for DIC. This has resulted in the coining of a new term, pulmonary intravascular coagulopathy, which suggests pulmonary specific inflammation, vasculopathy and thrombosis which differs from classical DIC. Further studies are required to establish the exact type of coagulopathy in COVID-19 as more evidence seems to indicate that it is a distinct entity.23
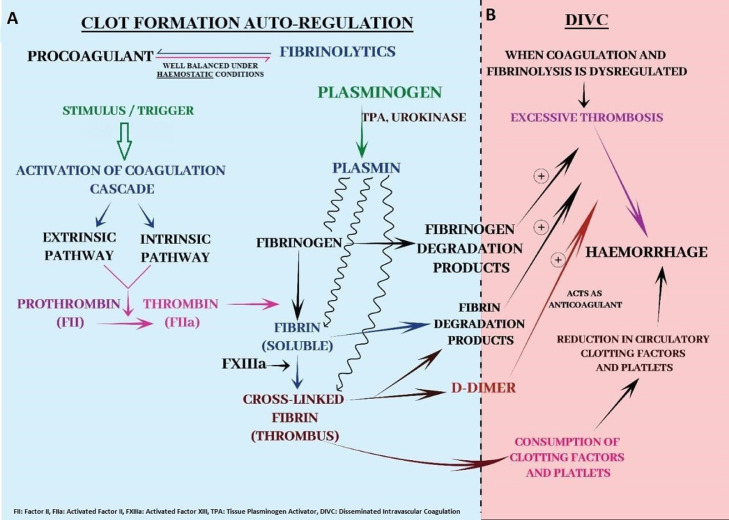
The brief pathophysiology of D-dimer formation and immuno-thrombosis with haemorrhage seen in DIC is depicted in Fig. 1 .
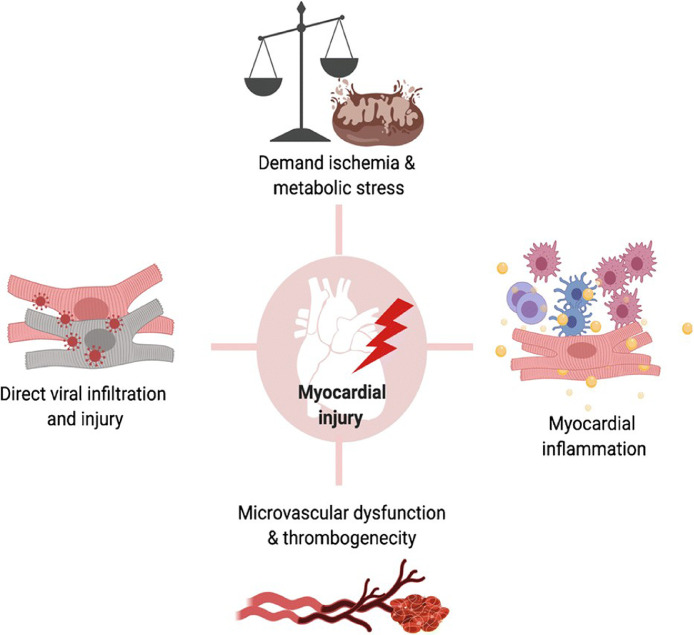
Fig. 2.
This figure illustrates the different mechanisms postulated for myocardial injury in COVID-19.56
Fig. 1.
The blue background (A) illustrates an outline of the coagulation cascade with its end result of thrombus formation and counter-regulatory fibrinolysis via plasmin activation which strikes a haemostatic balance between clotting and bleeding. Note that the thrombus/cross-linked fibrin breakdown results in fibrin degradation products and D-dimer, which is seen early in COVID-19. The pink background (B) illustrates the dysregulation of thrombosis and fibrinolysis which results in excessive thrombosis followed by haemorrhage known as disseminated intravascular coagulation.
Elevated D-dimer levels have been found to be a poor prognostic factor and have been associated with a reduced chance of survival among patients with COVID-19. Two recent studies by Ning T et al 22 and Guan et al 6 from China had found markedly elevated D-dimer levels amongst their COVID-19 mortalities with median D-dimer values of those that succumbed to the disease being at least 3 times higher than those who did not. In another a retrospective study from China in April 2020, Litao Zhang et al showed that a D-Dimer level on admission greater than 2.0 μg/mL could predict in-hospital mortality in COVID-19 patients, which is lower than previously recommended D-Dimer values of 3 to 4 times the upper limit of normal for COVID patients. This study also found that 12 of the 13 patients in the non-survivors group had D-dimer levels > than 2.0 μg/mL, but interestingly more than 50% (7 out of 12) of them had no severe symptoms on admission.24
While previous studies on SARS infection have shown alterations in platelet counts and isolated prolonged activated partial thromboplastin time, D-dimer levels were not significantly elevated.25 In another study in Hong Kong, there was no significant association between D-dimer levels and ICU admission or deaths in 138 patients with SARS, although raised D-dimer was detected in nearly half of the patients.26 These findings, when examined in comparison to COVID-19 cases suggest that the value of D-Dimer as a prognostic tool may be unique to the SARS-CoV2 virus and not all coronavirus infections.
Thus, D-dimer level could potentially be an early and helpful marker to improve the management of COVID-19 and point clinicians to the possibility of silent thrombosis occurring in the pre-symptomatic stage which might dictate the natural history, progression and severity of the disease in a manner that has not been seen in previous coronavirus infections.
Venous thromboembolism in COVID-19
Venous thromboembolism (VTE) refers to the formation of a thrombus within the venous system and consists of 2 clinical entities; pulmonary embolism (PE) and deep vein thrombosis (DVT).
A retrospective review of 100 COVID-19 patients who underwent contrast enhanced CT scans of the chest, 23% of patients had radiological evidence of pulmonary embolism.27 In another study looking at thrombotic complications of critically ill COVID-19 patients, the cumulative incidence of thrombotic complications was as high as 31%, even though all patients were on standard thromboprophylaxis, with 25 out of 31 of these thrombotic events being pulmonary embolisms.17 A larger Dutch study of 184 critically ill COVID-19 patients demonstrated that 65 patients (35%) developed pulmonary embolism. In the same study, 41 patients succumbed to their illness in ICU and most of the patients who died had not been referred for imaging tests to diagnose thrombotic complications which indicates that the rate of pulmonary embolism might be higher.18
Extensive histopathological studies of the pulmonary system of COVID-19 patients have given us a better understanding of the pathophysiology of COVID-19 pneumonia in comparison to other coronavirus infections. The main cause of mortality in COVID-19, which is ARDS, shows typical diffuse alveolar damage (DAD) with lymphocytic infiltrates, protein exudates and hyaline membrane formation as seen in SARS28, MERS29 as well as COVID-19 infections. However, there was a significant increase in microthrombi in the alveolar capillaries of COVID-19 patients.30, 31 – 32 In the post mortem of 21 COVID-19 patients, pulmonary histopathological findings revealed characteristic DADs however, 5 out of 11 patients who had immunohistochemistry for fibrin performed, revealed microthrombi in the alveolar capillaries and 4 of the total 21 patients had peripheral and prominent central pulmonary embolism.32 In another post mortem study of 5 COVID-19 patients, typical ARDS features with DAD were not seen even though histopathological evidence of microthrombi was present in all patients.33
The most striking difference between the pulmonary findings of COVID-19 and other coronavirus infections seems to be the prevalence of thrombosis in the imaging tests and histopathological examination be it in the form of microthrombi or large vessel pulmonary embolism, which demonstrates a more extensive prothrombotic process. This could prompt the notion that microthrombosis in the lungs, as part of the primary immunothrombosis mechanism, might precede a cytokine storm and worsen direct damage by the virus to lung tissues rather than microthrombi being the late response to direct damage and hypercytokinemia as previously thought.
The other component of VTE is deep vein thrombosis (DVT), which on its own carries lower mortality compared to pulmonary embolism but significant morbidity and is not to be overlooked. Cui et al studied a cohort of 81 patients with COVID-19 pneumonia, all of whom received adequate thromboprophylaxis, and found that 25% of patients developed lower extremity DVT. A total of 8 patients with lower limb DVT died but it was not elaborated upon how many were due to a pulmonary embolism secondary to DVT.34 A cross-sectional study of 2 hospitals in Wuhan, China revealed an extremely high rate of DVT where 41 out of 48 patients (85.4%) admitted into the intensive care unit for COVID-19 developed lower extremity DVT and all but one patient was on low molecular weight heparin prophylaxis.35 The incidence of DVT in COVID-19 patients compared to the critically ill patients without COVID-19, is significantly different with 2 studies in Thailand and Tehran showing an incidence on 3.6%36 and 3.5%37 respectively. The incidence of DVT in severe ARDS patients with possible H1N1 viral pneumonia were 9/71(12.6%) for lower extremities and 10/71(14.1%) for upper extremities.38 This demonstrates an increased rate on DVT in COVID patients compared to other critically ill patients and also reinforces the need to reassess the prophylactic anticoagulation dosage or the use of both chemoprophylaxis and mechanical prophylaxis concurrently.
Neurovascular disease (NVD)
COVID-19 has not spared the central and peripheral nervous system with case reports of cerebrovascular disease39, acute necrotizing haemorrhagic encephalopathy40, transverse myelitis41 and Guillain Barre syndrome.42 Not surprisingly, patients with COVID-19 who have NVD resulting from thrombosis have shown significantly elevated D-dimer and CRP levels which indicates a hypercoagulable state and an increased inflammatory response. This was shown in a retrospective study of 221 patients with COVID-19, of which 13 (5.9%) patients developed a new onset of NVD which included ischaemic strokes, intracranial haemorrhage and cerebral venous thrombosis. Among the 13 patients, 11 of them developed ischaemic strokes with 5 large vessel occlusions, 3 small to medium vessel occlusions and 3 cardioembolic strokes. Of these 13 NVD patients, 5 patients died resulting in a high mortality rate of 38.5%. Other significant risk factors, excluding raised D-dimer and CRP, that were associated with a high mortality rate for these patients with NVD, were comorbidities, age and increased severity of COVID-19 infection.39 Beyrouti et al reported on 6 COVID-19 patients with ischaemic stroke. All patients had large vessel occlusions (LVO) and 5 out of 6 patients had very high D-dimer levels of >7000 μg/L (median level reported in COVID-19 is 900 μg/L). The D-dimer for the 6th patient was 1080 μg/L after intravenous thrombolysis which was still above the median level. Interestingly, 2 patients developed LVO despite being on therapeutic anticoagulation and one patient developed stroke during the pre-symptomatic phase.43 These findings lend further weight to the presumption that thrombosis is the main perpetrator of morbidity at any stage of the COVID-19 infection, including the pre-symptomatic stage, and can be devastating as patients were reported to have developed LVO ischaemic stroke despite therapeutic anticoagulation.
Cardiovascular disease
When it comes to cardiac injury, there seems to be a discord from the other organs affected in this disease, where the culprit seems to possibly be from a non-thrombotic origin. SARS- CoV-2 infects host cells through ACE2 receptors which are highly expressed in the cardiac tissue causing acute myocardial injury and chronic damage to the cardiovascular system.44 This is also the same pathogenicity seen in MERSCoV infections.45 The most common cardiac abnormality is in its biomarkers, with an elevation of high sensitivity Troponin I (hsTI) which is directly proportional to disease severity and death.46 , 47 Kang Y et al describes 3 likely mechanisms of myocardial injury: acute coronary syndrome due to plaque rupture or thrombosis (type I myocardial infarction (MI) or supply-demand mismatch (type II MI), myocardial injury due to DIC, and non-ischaemic injury (myocarditis, stress-induced cardiomyopathy, or cytokine release syndrome).47
One of the first reviews on myocardial injury manifesting with increased hsTI in COVID-19 patients was a cohort of 41 COVID-19 pneumonia patients of which 13 patients ended up in intensive care. Among the 13 patients, 4 (31%) of them had elevated hsTI above the 99th percentile. Of the 13 patients in ICU, there was a high mortality rate of 5 deaths (38%) and an odds ratio of severe disease or death with troponin elevation of 12.0 [1.2–121.8].48 Two other larger studies from China also observed significantly elevated hsTI among patients with severe disease and non-survivors with odds ratio of 80.1 [10.3–620.4]49 and 15.1 [6.7–34.1].50 Patients with elevated hsTI also had significantly elevated D-dimer, high-sensitivity C-reactive protein, procalcitonin, globulin and other biomarkers of cardiac injury (N-terminal pro–brain natriuretic peptide, myoglobin, creatine kinase–myocardial band test) having p<0.001 compared to the normal hsTI arm which indicates a diffuse inflammatory process.50 Serial hsTI was able to prognosticate the disease progression as non-survivors had a higher level of hsTI elevation which showed a steady rise until death while troponin levels for survivors remained unchanged.46
Based on available studies to date, we are able to confidently correlate a high hsTI with severe disease and death; although the question remains as to how many of these are purely due to thrombosis (Type I MI) and not a supply demand mismatch (Type II MI). A study from Lombardy reviewed a cohort of 28 patients with STEMI where 24 patients (85.7%) had STEMI as the first clinical manifestation of COVID-19 (no COVID-19 testing was done at the time of coronary angiography) and the remaining 4 patients suffered from STEMI during hospitalization for COVID-19. Twenty-two patients (78.6%) presented with typical chest pain with or without dyspnoea, 6 patients (21.4%) had dyspnoea without chest pain. Out of the 28 patients, 17 (60.7%) had evidence of obstruction requiring revascularization and 11 patients (39.3%) did not have obstructive coronary artery disease.51 Bangalore S et al published a case series of COVID-19 patients with STEMI from 6 hospitals in New York. They identified 18 patients with COVID-19 who had ST-segment elevation indicating potential acute myocardial infarction and 9 patients underwent coronary angiogram. Six out of nine patients (67%) had obstructive disease.52 These two studies demonstrate that despite patients having STEMI, either as a possible first presentation of COVID-19 or developing STEMI after the diagnosis of COVID-19, a significant number of patients did not have evidence of coronary obstruction which leads us to believe that coronary thrombosis might not be the main etiology of cardiac damage in this devastating disease.
Till date, the mechanism by which COVID-19 inflicts myocardial damage is not fully understood although it appears to be due to myocardial injury rather than thrombosis. Oudit et al showed that 35% of the patients with SARS infection had the SARS-CoV genome detected in the heart. This indicates that there's direct damage of cardiomyocytes by the virus.53 Because SARS-COV and SARS-CoV-2 are highly homologous in genome, they may share the same mechanism of myocardial injury and opposed to a thrombotic damage from coronary occlusion.50
Treatment
Thus far, the mainstay of therapy for COVID-19 has been immunomodulation by early detection of cytokine storms and initiation of immunomodulatory therapy, the details of which are beyond the scope of this article. However as discussed, the prominence of thrombotic complications necessitates that attention also be focused on thrombolysis and anticoagulation. There has been, and will always be, a risk versus benefit consideration into anticoagulation therapy for treatment of thromboembolic disease, and an even bigger debate for prevention of thromboembolism. These considerations have been carried forward into the management of thromboembolic disease in COVID-19.
The CHEST guideline and expert panel report recommend the use of low molecular weight heparin (LMWH) or fondaparinux in acutely ill and critically ill patients as thromboprophylaxis with standard dose preventive anticoagulation in the absence of contraindications. Unfractionated heparin (UFH) is not the preferred option as it would increase staff exposure due to its bidaily administration compared to the once daily dosage of LMWH. It is also not recommended to extend preventive therapy upon discharge.
As for the treatment of pulmonary embolism or DVT, LMWH or intravenous UFH is recommended with preference towards LMWH to limit staff exposure and avoid the potential for heparin pseudo-resistance. Upon discharge, direct oral anticoagulants (DOAC) or vitamin K antagonists (VKA) are both acceptable long term treatment options with a minimum of 3 months therapy. Antiplatelet therapy is not recommended as thromboprophylaxis in COVID-19.54
Thrombolytic therapy in COVID-19 for PE is only recommended in patients with objectively confirmed acute PE with hemodynamic instability and/or cardiopulmonary deterioration.
In the management of NVD, particularly acute ischaemic stroke, there are no specific clinical guidelines established in the handling of COVID-19 positive patients who are eligible for thrombolysis. Management of hemodynamic status must always balance the risk and benefits of such treatment in COVID positive cases. A single case report in a Filipino patient with COVID-19 who was administered intravenous thrombolysis for an acute ischaemic stroke with a National Institutes of Health Stroke Scale (NIHSS) score of 4 showed fluctuations in motor power over the course of admission but her neurological deficit did not show any major improvement and neither did she develop bleeding complications. There is no established guidelines for secondary prevention with antiplatelet therapy in COVID-19 patients with ischaemic stroke however the Consensus for Prevention and Management of COVID-19 for Neurologists recommends preventive anticoagulation for ischaemic stroke patients with a high D-dimer level due to the high possibility of cardioembolic etiology of stroke.55
In regard to COVID-19 and myocardial injury, there is no specific targeted therapy to prevent or reduce the risk of myocardial injury and supportive care is the mainstay of treatment at this moment. As patients with underlying cardiovascular disease are at a higher risk of morbidity and mortality from COVID-19, early stratification of patients is vital for close monitoring and anticipation of complications in this group of individuals.48 , 50 There has been a debate on whether angiotensin converting enzyme inhibitors(ACE-i) or angiotensin receptor blockers(ARB) are beneficial or detrimental for patients with COVID-19 as ACE2 expression is increased with ACE-i and ARB which is a target for COVID-19 but there is no significance in outcomes and larger clinical trials are required.50
Conclusion
The role of thrombosis in the disease process of COVID-19, as highlighted in this article, appears to be the main player in directly contributing to the morbidity and mortality of infected patients. Elevated D-dimer levels in the pre-symptomatic stage of COVID-19 infections further emphasizes the likelihood of ongoing silent thrombosis, thus consideration of early treatment of elevated D-Dimer levels even in the absence of clinical symptoms needs to be explored.
While manifestation of VTE and arterial thrombosis in the neurovascular system is recognized, interestingly, the cardiovascular system seems to be damaged from direct invasion of the virus into the myocardium rather than by direct occlusion of the main coronary vessels by thrombi. This suggests the existence of varied mechanisms of injury in different organs and thus further understanding of these differences in pathophysiology could be essential for the development of future targeted therapy to a specific organ.
In patients with severe disease, extensive research is still required to ascertain optimal chemo/mechanical thromboprophylaxis regimens. Consideration of extended thromboprophylaxis after discharge to reduce morbidity and mortality while striking a balance between prevention of thrombosis and development of haemorrhagic complications must also be undertaken.
As we endeavor to understand more about this disease and its devastating complications, better treatment options will continue to emerge and in due course reduce the morbidity and mortality of this pandemic that has profoundly affected us in one way or another.
Footnotes
Declaration of interest
Presaad Pillai -none
Joyce Pauline Joseph, - None
Nurul Huda Mohamad Fadzillah, - None
Masliza Mahmod, - None
Financial disclosures
Presaad Pillai, - Reports no disclosures
Joyce Pauline Joseph, - Reports no disclosures
Nurul Huda Mohamad Fadzillah, - Reports no disclosures
Masliza Mahmod, - Reports no disclosures
References
- 1.Morens DM, Daszak P, Taubenberger JK. Escaping pandora's box - another novel coronavirus. N Engl J Med. 2020;382(14):1293–1295. doi: 10.1056/NEJMp2002106. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization; Geneva: 2020. WHO coronavirus disease (COVID-19) dashboard.https://covid19.who.int/ Available online: (last cited: 5/9/2020) [Google Scholar]
- 3.Mills C.E., Robins J.M., Lipsitch M. Transmissibility of 1918 pandemic influenza. Nature. 2004;432(7019):904–906. doi: 10.1038/nature03063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong Jessica Y., Kelly Heath, Ip Dennis K.M., Wu Joseph T., Leung Gabriel M., Cowling Benjamin J. Case fatality risk of influenza A(H1N1pdm09): a systematic review. Epidemiology (Cambridge, Mass.). November 2013;24(6) doi: 10.1097/EDE.0b013e3182a67448. 10.1097/EDE.0b013e3182a67448. ISSN 1044-3983. PMC 3809029. PMID 24045719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [published correction appears in Lancet. 2020 Jan 30;:] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [published online ahead of print, 2020 Feb 24] 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta. 2020;507:167–173. doi: 10.1016/j.cca.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292. doi: 10.1016/j.cell.2020.02.058. .e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donoghue M, Hsieh F, Baronas E. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. Circ Res. 2000;87(5):E1–E9. doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 12.Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215 doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta. 2020;507:167–173. doi: 10.1016/j.cca.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Subramaniam S, Scharrer I. Procoagulant activity during viral infections. Front Biosci (Landmark Ed) 2018;23:1060–1081. doi: 10.2741/4633. Published 2018 Jan 1. [DOI] [PubMed] [Google Scholar]
- 15.D'Elia RV, Harrison K, Oyston PC, Lukaszewski RA, Clark GC. Targeting the "cytokine storm" for therapeutic benefit. Clin Vaccine Immunol. 2013;20(3):319–327. doi: 10.1128/CVI.00636-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramos I, Fernandez-Sesma A. Modulating the innate immune response to influenza a virus: potential therapeutic use of anti-inflammatory drugs. Front Immunol. 2015;6:361. doi: 10.3389/fimmu.2015.00361. Published 2015 Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klok FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klok FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bunce Paul E., High Sasha M., Nadjafi Maral. Pandemic H1N1 Influenza infection and vascular thrombosis. Clinical Infectious Diseases. 15 January 2011;52(2):e14–e17. doi: 10.1093/cid/ciq125. VolumeIssue. [DOI] [PubMed] [Google Scholar]
- 20.Ito T. PAMPs and DAMPs as triggers for DIC. J Intensive Care. 2014;2:65. doi: 10.1186/s40560-014-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Venugopal A. Disseminated intravascular coagulation. Indian J Anaesth. 2014;58(5):603–608. doi: 10.4103/0019-5049.144666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martín‐Rojas RM, Pérez‐Rus G, Delgado‐Pinos VE. et al COVID‐19 coagulopathy: an in‐depth analysis of the coagulation system. Eu J Haematol. 10.1111/ejh.13501 [DOI] [PMC free article] [PubMed]
- 24.Zhang L, Yan X, Fan Q. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J Thromb Haemost. 2020;18(6):1324–1329. doi: 10.1111/jth.14859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee N, Hui D, Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 27.Grillet F, Behr J, Calame P, Aubry S, Delabrousse E. Acute pulmonary embolism associated with COVID-19 pneumonia detected with pulmonary CT angiography. Radiology. 2020;296(3):E186–E188. doi: 10.1148/radiol.2020201544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ding Y, Wang H, Shen H. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J Pathol. 2003;200(3):282–289. doi: 10.1002/path.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ng DL, Al Hosani F, Keating MK. Clinicopathologic, immunohistochemical, and ultrastructural findings of a fatal case of middle east respiratory syndrome coronavirus infection in the United Arab Emirates, April 2014. Am J Pathol. 2016;186(3):652–658. doi: 10.1016/j.ajpath.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang H, Zhou P, Wei Y. Histopathologic changes and SARS-CoV-2 immunostaining in the lung of a patient with COVID-19. Ann Intern Med. 2020;172(9):629–632. doi: 10.7326/M20-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Menter T, Haslbauer JD, Nienhold R. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020 doi: 10.1111/his.14134. [published online ahead of print, 2020 May 4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magro C, Mulvey JJ, Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ren B, Yan F, Deng Z. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation. 2020;142(2):181–183. doi: 10.1161/CIRCULATIONAHA.120.047407. [DOI] [PubMed] [Google Scholar]
- 36.Prichayudh S, Tumkosit M, Sriussadaporn S. Incidence and associated factors of deep vein thrombosis in Thai surgical ICU patients without chemoprophylaxis: one year study. J Med Assoc Thai. 2015;98(5):472–478. [PubMed] [Google Scholar]
- 37.Miri M, Goharani R, Sistanizad M. Deep vein thrombosis among intensive care unit patients; an epidemiologic study. Emerg (Tehran) 2017;5(1):e13. [PMC free article] [PubMed] [Google Scholar]
- 38.Obi AT, Tignanelli CJ, Jacobs BN. Empirical systemic anticoagulation is associated with decreased venous thromboembolism in critically ill influenza A H1N1 acute respiratory distress syndrome patients. J Vasc Surg Venous Lymphat Disord. 2019;7(3):317–324. doi: 10.1016/j.jvsv.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 39.Li Y, Li M, Wang M. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020 doi: 10.1136/svn-2020-000431. [published online ahead of print, 2020 Jul 2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296(2):E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao K., Huang J., Dai D., Feng Y., Liu L., Nie S. Acute myelitis after SARS-CoV-2 infection: a case report. MedRxiv. 2020 doi: 10.1101/2020.03.16.20035105. [DOI] [Google Scholar]
- 42.Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beyrouti R, Adams ME, Benjamin L. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91(8):889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann Saudi Med. 2016;36(1):78–80. doi: 10.5144/0256-4947.2016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kang Y, Chen T, Mui D. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020;106(15):1132–1141. doi: 10.1136/heartjnl-2020-317056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mestres G, Puigmacià R, Blanco C, Yugueros X, Esturrica M, Riambau V. Risk of peripheral arterial thrombosis in COVID-19. J Vasc Surg. 2020;72(2):756–757. doi: 10.1016/j.jvs.2020.04.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo T, Fan Y, Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):1–8. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stefanini GG, Montorfano M, Trabattoni D. ST-Elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141(25):2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bangalore S, Sharma A, Slotwiner A. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382(25):2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oudit GY, Kassiri Z, Jiang C. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moores LK, Tritschler T, Brosnahan S. Prevention, diagnosis, and treatment of vte in patients with coronavirus disease 2019: chest guideline and expert panel report. Chest. 2020 doi: 10.1016/j.chest.2020.05.559. S0012-3692(20)31625-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jin H, Hong C, Chen S. Consensus for prevention and management of coronavirus disease 2019 (COVID-19) for neurologists. Stroke Vasc Neurol. 2020;5(2):146–151. doi: 10.1136/svn-2020-000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheng P., Zhu H., Witteles R.M. Cardiovascular Risks in Patients with COVID-19: Potential Mechanisms and Areas of Uncertainty. Curr Cardiol Rep. 2020;22:34. doi: 10.1007/s11886-020-01293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]