Abstract
In this paper, we report three cases of pediatric patients with COVID-19 infection who presented with different symptoms and also anosmia and/or ageusia. The common feature of these 3 patients is that the smell and / or taste disorder developed without nasal symptoms such as nasal congestion, nasal obstruction or rhinorrhea. Although 40% of anosmies contains viral etiologies, COVID- 19 differs from other viral anosmies by the lack of nasal congestion and runny nose. Coronaviruses could invade the brain via the cribriform plate close to the olfactory bulb and the olfactory epithelium. We may expect some structural changes in the olfactory bulb so we evaluated our patient with cranial imaging.
The world was faced with a novel form of coronavirus, named coronavirus disease 2019 (COVID-19), by the World Health Organization (WHO) in December 2019. According to the Coronavirus Study Group (CSG) of the International Committee, the virus became known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Sayin et al., 2020) [1]. In the early phases of the pandemic, fever, dyspnea, coughing, and travel to endemic counties were used as the main screening parameters. However, during the course of the outbreak, different symptomatology including chemosensory involvement, as evaluated by smell and taste dysfunctions, was reported (Qiu et al., 2020) [2]. Published reports of adult patients with COVID-19 infection also different from pediatric population. Olfactory disorders have been well studied in the adult population, but little is known about these disorders in the pediatric population. Children usually showed milder respiratory symptoms or were asymptomatic, while loss of taste or sensation of smell were less reported (Mak et al., 2020 Aug) [3].
In this paper, we report three cases of pediatric patients with COVID-19 infection who presented with different symptoms and also anosmia and/or ageusia. The common feature of these 3 patients is that the smell and/or taste disorder developed without nasal symptoms such as nasal congestion, nasal obstruction or rhinorrhea. While it was possible to learn the smell disorder with anamnesis in children, it was difficult to define the taste disorder. Most subjects were not asked about taste and smell impairment especially at pediatric patient groups. The high average age of our patients suggested that they answered our questions clearly. The fact that we questioned symptoms with anamnesis and that we could not perform objective tests during the pandemic period were the points that limited us. Chemosensory disorders resolved spontaneously within 5 days. All patients were checked with rapid antigen test due to the frequent influenza infection in order to exclude influenza, which is a common infection causing odor disorders in April [4]. Radiological evaluation were assessed at early phase of COVID-19 infection because to date no published pediatric anosmia screening tools in COVID-19 have been validated (Hall et al., 2020) [5]. We used cranial neuroimaging technique. Three-dimensional (3D) constructive interference in steady state (CISS) is a gradient-echo magnetic resonans imaging (MRI) sequence, FLAIR and coronal contrast fat-suppressed T1W sequences were used for the olfactory region with a 1.5 T MRI device (Siemens/Japan). TR/TE, 80 0 0/133 ms; TSE factor 80; bandwidth, 120 Hz/pixel; section thickness, 2 mm; matrix 240 × 240; FOV, 230 × 230 × 20; voxel size, 0.95 × 0.95 × 2 mm; ETL = 220 with variable flip angle; acquisition time = 4 min 36 sec. Sections were taken parallel to the olfactory plate. MRI of the cases were evaluated by an experienced pediatric neuroradiologist (FP). The olfactory bulb size increase, pathological signal increase, contrast enhancement and olfactory cleft were evaluated with MRI in terms of pathological signal increase.
1. Case 1
A 13-year-old girl (HE) admitted our pediatric emergency department at April 16, 2020. She had headache. She presented hospital on the 2nd day after her headache onset, her breath problem was later added symptom. In the family history, we learned that her grandmother died due to COVID-19 pneumonia and her mother received COVID-19 pneumonia treatment for 6 days in the hospital. She was previously healthy, she was not taking any medications. Throat and nasopharyngeal saliva was taken for testing of COVID-19. Thorax tomography, laboratory tests revealed viral pneumonia and SARS-CoV-2 was detected by reverse-transcription-polymerase chain reaction (RT-PCR). The patient's Influenza A and Influenza B rapid antigen test was negative. The most common viral agents that can cause smell impairment were thus excluded.
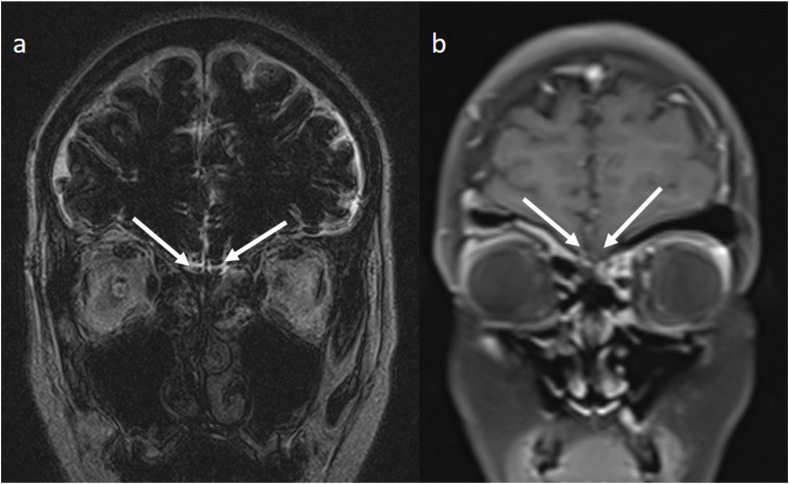
She realized an acute loss of the olfactory function without nasal obstruction. There was no dysgeusia because the patient reported no changes in salty, sweet, sour, and bitter. Cranial magnetic imaging was performed to include the olfactory nerve pathway and olfactor bulb (OB). Because chemosensory involvement added to the patient's headache complaints 2 days later. Despite the sudden onset of a complete loss of olfactory function, we found normal OB volume without abnormal signal intensity in the OB and tract and no sign of nasal congestion (Fig. 1 a, b). Chemosensory involvement that started on April 16, 2020 and ended on April 21, 2020, the patient stated that her sense of smell improved again. Apart from COVID-19 viral pneumonia, the patient's anosmia resolved in 4 days without any additional treatment for chemosensory involvement.
Fig. 1a/b.
No signal change or contrast material uptake was observed in the olfactory bulb in coronal CISS (a) and contrast-enhanced coronal T1A sections (b) performed in a 13-year-old girl.
2. Case 2
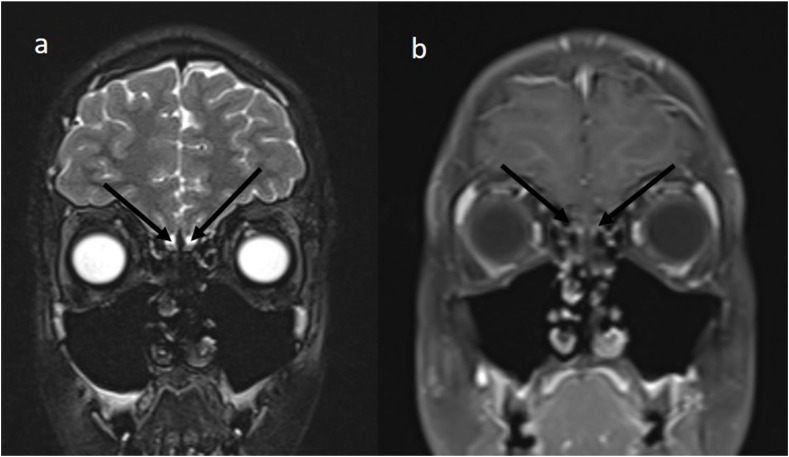
A 13-year-old male patient (MD), who complained of fever once 3 days ago, applied to our clinic. Anosmia disorder started 2 days after the patient's fever complaint. Our clinic was hospitalized due to the positive result of the swab taken from the child in the external center where they applied because his father was COVID positive swap result. He reported no respiratory symptoms upon admission, while further questioning revealed anosmia and ageusia. He had no nasal obstruction or rhinorrea. He had subfebrile fever with stable vital signs in room air. Systemic examination was unremarkable. The patient was evaluated for influenza A/B infections and was found negative. The patient underwent a computed tomographic scan of thorax for viral COVID-19 pneumonia because of fever and smell disorder. He had bilateral patchy ground-glass opacities. Olfactor bulb and olfactor nerve were evaluated by MRI due to the patient's odor and taste disorder (Fig. 2 a, b) There were no anomalies of the olfactory bulbs and tracts. Also this patient anosmia resolved in 3 days.
Fig. 2a/b.
No pathology was found in the olfactory bulb in the coronal CISS (a) and contrast-enhanced coronal T1A sections (b) of a 13-year-old male patient.
3. Case 3
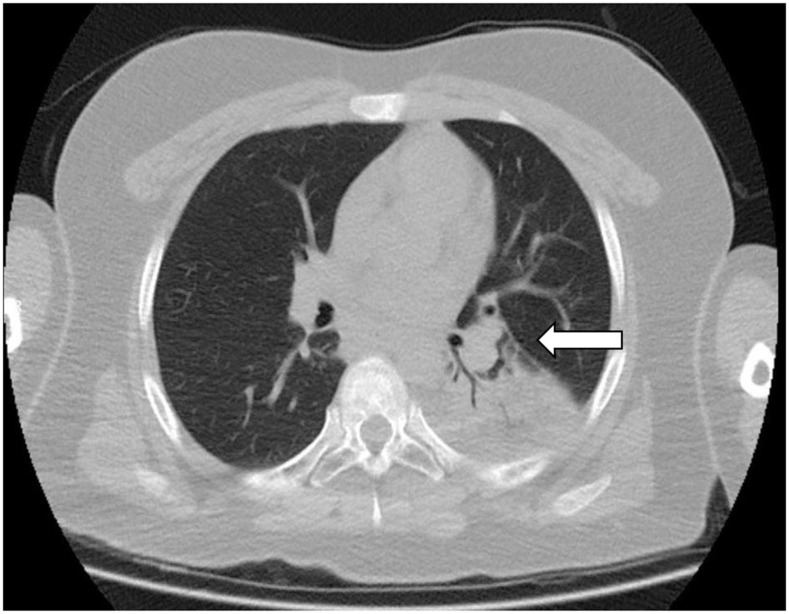
Fever, cough, weakness, headache and chest pain complaints started on April 12, 2020 of a 13 year old male patient (MEY). As the patient's complaints continued to increase, the patient was evaluated as moderate to severe COVID-19 pneumonia (respiratory distress requiring oxygen support) intensified in the lung basal due to bilateral consolidation areas and ground-glass appearance (Fig. 3 ) and hospitalization was made in pediatric intensive care service. Swab samples were taken for the diagnosis of COVID-19. The patient had resistant fever and desaturation in the room air (SPO2 = % 88). Then the patient referred to the intensive care unit. After 5 days in the intensive care unit, he was taken to the pediatrics service for follow-up, the complaints of the patient, whose smell and taste disorder were noticed, continued the decrease in the service. Cranial MRI was performed after the patient's clinical condition improved but the smell and taste disorder continued, but an exact pathology was not detected. This patient was also negative for influenza infections.
Fig. 3.
In a 13-year-old male patient, a consolidation area consistent with pneumonia was observed in the posterior segment of the left upper lobe of the left lung with air bronchograms.
4. Discussion
Although 40% of anosmies contains viral etiologies, COVID- 19 differs from other viral anosmies by the lack of nasal congestion and runny nose [6]. Coronaviruses could invade the brain via the cribriform plate close to the olfactory bulb and the olfactory epithelium. We may expect some structural changes in the olfactory bulb that were not observed in these cases. However it is important to assess the volume of the olfactory bulb so we also detected MRI results with this scope. Moreover, Yao et al. have reported that the volume of the olfactory bulb is decreased in patients with postinfectious olfactory loss and is inversely related to the duration [7]. For these reason we didn't want to lose time. We evaluated MRI at the early phase of chemosensory impairment days.
There are MRI studies of the olfactory region to evaluate the sudden sense of smell and taste that occur in adults with COVID-19 infection [[8], [9], [10], [11]]. MRI is used, and some studies have attempted to evaluate inflammation by administering contrast material. In this study, we evaluated our cases using three-dimensional (3D) constructive interference in steady state (CISS) is a gradient-echo MRI sequence, 3D FLAIR and coronal contrast fat-suppressed T1A sequences. In studies conducted with adults, cases with increased size in the olfactory bulb, pathological signal increase and contrast material uptake and increased signal in the olfactory cleft have been reported in patients with sudden loss of smell and taste [[8], [9], [10], [11]]. These imaging findings were found to be temporary in repeated MRI examinations in some studies [8]. These pathological images detected by MRI are thought to be the result of virus-related inflammation in COVID-19 infection [11]. However, in some of the studies, no finding was found in the olfactory region with MRI in adult patients [9]. In the literature, loss of sense of smell and taste in childhood is a rare finding, and there is no imaging study performed on the olfactory region. In our study, no pathological imaging finding in the olfactory region was detected in the MRI examination of 3 children with loss of smell and taste.
Published studies indicated that smell impairment in SAR-CoV-2 recovered early. At present, no treatment for SARS-CoV-2-related smell impairment exists [12]. The present cases has some limitations. This report's knowledge was limited to published data to date. Literature about this subject is updating very fast. However, nasal procedures, detailed examinations, and close contact with subjects were avoided during the pandemic, which resulted in a limited number of information about our cases. The reviewed articles were mostly observational and questionnaire-based. Measurement of olfactory bulb is a rare evaluation that made in pediatric subjects. Absence of previous cranial MRI imaging made it impossible to compare current findings in same pediatric subjects. Larger studies with objective testing methods and longer follow up periods will deepen our knowledge about SARS-CoV-2-related taste/smell impairment in pediatric population.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Sayin I., Yazıcı Z.M., Oz F. Otolaryngology-head and neck surgery perspective of COVID-19. Turkiye Klinikleri J. Med. Sci. 2020;40(2):120–124. doi: 10.5336/medsci.2020-75313. [DOI] [Google Scholar]
- 2.Qiu C., Cui C., Hautefort C., Haehner A., Zhao J., Yao Q. Olfactory and gustatory dysfunction as an early identifier of COVID-19 in adults and children. An International Multicenter Study Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820934376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mak P.Q., Chung K.S., Wong J.S.C., Shek C.C., Kwan M.K.W. Anosmia and ageusia: not an uncommon presentation of COVID-19 infection in children and adolescents pediatr. Inf. Disp. J. 2020 Aug;39(8):e199–e200. doi: 10.1097/INF.0000000000002718. [DOI] [PubMed] [Google Scholar]
- 4.https://grip.gov.tr/depo/influenza-raporu/2019/Haftalk_nfluenzaGrip_Srveyans_Raporu_2020_2._hafta.pdfHaftalk_nfluenzaGrip_Srveyans_Raporu_2020_2._hafta.pdf
- 5.Hall A., Frauenfelder C., Butler C., Coyle P., Hopkins C. Paediatric olfactory dysfunction: a chance to detect COVID-19? Arch. Dis. Child. 2020 doi: 10.1136/archdischild-2020-319971. [DOI] [PubMed] [Google Scholar]
- 6.Galougahi M.K., Ghorbani J., Bakhshayeshkaram M., Naeini A.S., Haseli S. Olfactory bulb magnetic resonance imaging in SARS-CoV-2-induced anosmia: the first report. Acad. Radiol. 2020 Jun;27(6):892–893. doi: 10.1016/j.acra.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao L., Yi X., Pinto J.M., Yuan X., Guo Y., Liu Y. Olfactory cortex and olfactory bulb volume alterations in patients with post-infectious olfactory loss. Brain Imaging Behav. 2018;12:1355e62. doi: 10.1007/s11682-017-9807-7. [DOI] [PubMed] [Google Scholar]
- 8.Laurendon T., Radulesco T., Mugnier J. Bilateral transient olfactory bulb edema during COVID-19-related anosmia. Neurology. 2020 Aug 4;95(5):224–225. doi: 10.1212/WNL.0000000000009850. [DOI] [PubMed] [Google Scholar]
- 9.Aragoa M.F.V.V., Leal M.C., Cartaxo Filho O.Q., Fonseca T.M., Valenca M.M. Anosmia in COVID-19 associated with injury to the olfactory bulbs evident on MRI. AJNR. 2020 Jun 25 doi: 10.3174/ajnr.A6675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li C., Syue L., Tsai Y. Anosmia and olfactory tract neuropathy in a case of COVID-19. J. Microbiol. Immunol. Infect. 2020 Jun 20;S1684–1182(20) doi: 10.1016/j.jmii.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chetrit A., Lechien J.R., Ammar A. Magnetic resonance imaging of COVID-19 anosmic patients reveals abnormalities of the olfactory bulb: preliminary prospective study. J. Infect. 2020;S0163–4453(20):30509–30510. doi: 10.1016/j.jinf.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sayin I., Yazici Z.M. Taste and smell impairment in SARS-CoV-2 recovers early andSpontaneously: experimental data strongly linked to clinical data. ACS Chem. Neurosci. 2020 Jul 15;11(14):2031–2033. doi: 10.1021/acschemneuro.0c00296. [DOI] [PubMed] [Google Scholar]