Abstract
The Trieste Habitat Micro-area Programme (HMP), an innovative social-health service policy, has offered a natural experiment to empirically evaluate the social mechanisms through which social capital may have an impact on health inequalities. To date, literature clarifying this causal chain is scanty. This empirical study tested the following hypotheses: H1) innovative social-health practices can activate social mechanisms intentionally and systematically so as to generate social capital; H2) such social mechanisms increase specific properties of social capital, in particular those influencing more vulnerable individuals’ relationships; H3) investing in these properties can enhance capabilities and, consequently, control over the health of more vulnerable individuals.
The study was carried out during 2016–2018 and used both qualitative and quantitative methods. The qualitative part investigated the field experience of the HMP through interviews, focus groups and workshops with HMP professionals. The quantitative part assessed the effect HMP might have on these properties and the capacity to face health risks of more vulnerable individuals. Three samples, each of 200 individuals, residing in the target and in control areas were interviewed using a semi-structured questionnaire. One control sample was matched to the 200 treated subjects using a Propensity Score Matching.
The results of the study suggest that the HMP intervention stimulated the development of empowerment, collaboration and interdependence among vulnerable people. This produced an increase in their social capital under several aspects, including enhanced trust, network extension and participation, cooperation and reciprocal help with neighbours, as well as improving their judgement on quality, timing and efficacy of the help received from institutions, relatives or friends. These findings show that socially shared relationships can create innovative local models of a universalistic generative welfare system, which would be both inclusive and able to enhance individual capabilities. These models could be disseminated and carried over to other contexts.
Keywords: Health inequalities, Capabilities, Social capital, Generative welfare, Social determinant, Urban health promotion, Social mechanisms
Highlights
-
•
A qualitative and quantitative study on a local experience of generative welfare.
-
•
The role social mechanisms play in generating specific properties of social capital.
-
•
These properties enhance vulnerable individuals' capabilities and may contribute to reduce health inequalities.
-
•
These social mechanisms can be activated by public health services, to strengthen the generative welfare model.
1. Theoretical framework and research questions
Health in European cities is unevenly distributed, despite the apparent level of well-being and social protection that characterizes Europe (Marmot, 2010; WHO, 2012). This unequal distribution has been attributed to the populations' varied social make-up in different areas and to the environmental and socioeconomic contextual characteristics of these areas (Van Lenthe et al., 2005). Numerous publications have reported on how the social factors like education, social class, income and wealth, influence health over an individual's life span (Roberts, 2015). Conversely, studying the effects exposure to contextual factors may have on health is a more complex issue and literature is scanty.
This is much due to the difficulty in defining and measuring such an exposure (Galster, 2012). This is particularly true when it comes to exposure to social contextual circumstances, e.g., social capital and its interaction with individual social disadvantage.
Individuals we define as vulnerable have fewer resources and less individual capacity to control the health consequences of adverse life experiences, and are often forced to live in the most disadvantaged and segregated areas, which offer fewer opportunities. If these more vulnerable individuals are to develop capabilities enabling them to perform well under adverse circumstances, then their possibilities of action and the alternatives available within an everyday environment must be expanded (Di Monaco 2014; Sen, 1986). These characteristics, both personal and contextual, make people more or less vulnerable depending on their capabilities.
Previous research has identified social capital as a key feature of the social context (Moore 2014), which would represent an additional resource able to counterbalance the potential negative health effects of adverse social circumstances, beyond individual resources and capabilities (Coleman, 1990). However, individuals in deprived areas have fewer possibilities to count on social relationships. On average, they have less social capital, as defined by Bourdieu (1986) as “the aggregate of actual or potential resources linked to possession of a durable network”. According to this theory, social capital, which would be generated by the overall social position of the people belonging to a certain community (Bird 2010), would allow them to access numerous types of resources through social relationships, i.e., helping one another out, sharing information, keeping an eye on one another's property and personal safety, developing activities and initiatives within the neighbourhood, etc. (Carpiano, 2008). Moreover, deprived areas usually have less social cohesion and trust: ‘Trust, norms which regulate living together and the network of civic associations are all elements which improve the efficacy of social organisations, promoting common initiatives’ (Putnam, 1993).
Social capital has an intrinsically double nature of social construction and is made up of individual relationships, which, in part, concerns the properties of these relationships and the meaning assigned to them (Kawachi, Subramanian, & Kim, 2008). It also includes the individual use people make of social capital to mobilise these relationships to reach their objectives (Coleman, 1990; Kawachi et al., 2013; Moore 2017).
The quality of this social infrastructure is continually influenced by numerous factors, i.e., the socio-economic status of the individuals involved, which create and maintain these relationships stable, and the activation of various social mechanisms stemming from the interaction with specific institutional contexts (Barbera 2004; Waverijn 2016). These mechanisms include trust, social exchange and reciprocity, cooperation and learning.
Consequently, these social interactions both constitute a representation of the presence of specific properties of the social capital in use and create conditions where they can be amplified and reinforced, as they modify the institutional context and the social norms the individuals interact with. We are specifically referring to social capital and not to ‘social support’, which can be given to subjects in difficulty by means of specific social relationships (Gale 2018). Social support refers to mono-directional top/down relationships where vulnerable people are merely passive users and totally dependent. Conversely, bi- and multi-directional social relationships generate behavioural effects, amplifying intentional behaviour and generating ‘empowerment’, i.e., new competencies and a greater degree of autonomous freedom of choice (Di Monaco 2014). Recent research has empirically assessed the direct influence social capital has on individual and collective behaviour generated through the spread of social norms, which occurs along with personal interaction. In particular, we are referring to the interaction experienced within a defined space and characterized by strong binding, family, friendship and a sensation of “togetherness” (neighbourhood) appears to be particularly effective (Centola 2018; Pentland, 2015).
Therefore, when a deprived area is considered, its social capital can be defined as a structural element of social relationships, which characterizes the groups and sub-groups of people who live there (Villalonga-Olivesa 2018). Each individual's social capital is not simply a fixed characteristic but can be created or amplified (Edwards 2010; Jones 2014; Wilmot 2017) with the contribution of the vulnerable individuals themselves. This can be achieved by specific social mechanisms, intentionally reproduced by individual, collective and institutional players.
Social-health services are players who have the specific mission of promoting health, especially in deprived areas. Therefore, the capabilities of individuals, above all vulnerable subjects, should be nurtured, making feasible and preferable individual and collective health-oriented behaviours.
This may be feasible only if the traditional ponderous bureaucratic mentality, which still defines the organization of many health services, is by-passed (Laverack, 2016). These services should redesign their organization to manage social processes and should construct alliances and integration processes amongst the various local services in a systematic manner, so as to create value for the individual.
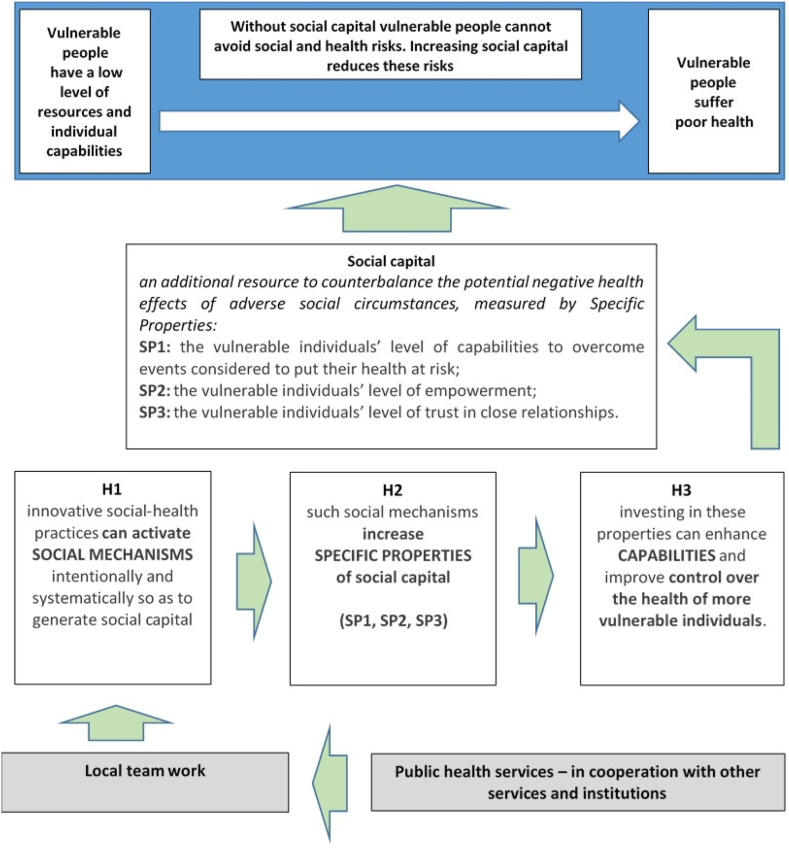
The Trieste HMP was implemented in 2010 (in the current mode) and has provided a natural experiment (Craig 2012) for a controlled cross-sectional study on how this social chain works testing and assessing the following hypotheses:
H1)
➢ innovative social-health practices can activate social mechanisms intentionally and systematically so as to generate social capital;
H2)
➢ such social mechanisms increase specific properties of social capital, in particular those influencing relationships of the more vulnerable individuals,
H3)
➢ investing in these properties can enhance capabilities and improve control over the health of more vulnerable individuals.
As there are no adequate definitions for all circumstances, our working definition of social capital was tailored to our research purposes (Van der Gaag and Webber 2008). Three specific properties of social capital were considered essential for the protection of vulnerable individuals’ health in critical social circumstances:
SP1: the vulnerable individuals’ level of capabilities to overcome events considered to put their health at risk;
SP2: the vulnerable individuals’ level of empowerment;
SP3: the vulnerable individuals’ level of trust in close relationships (Fig. 1).
Fig. 1.
HMP intervention theory and assessment strategy.
2. Research strategies and methods
2.1. The HMP intervention in Trieste
This innovative local generative welfare HMP programme has provided public health services in 15 of the most deprived neighbourhoods in Trieste, Italy. They have been named Micro-areas and have from 500 to 2000 inhabitants each, for a total of 18,000. These services are jointly managed by the three main local authorities (healthcare, social care, social housing) in the city of Trieste (the old harbour dating back to the Habsburg Empire in North-East Italy). Trieste is the largest city in the Friuli-Venezia Giulia region, with 203,000 inhabitants. It has an ageing urban population, with 259 people over 65 per 100 under 14 years, 17% of single-parent households, compared to the Italian average of 13.5%, a high life expectancy, a high average income (GDP per capita per year of 30,000 euros, compared to an Italian average of 27,700 euros), and a significant presence of foreigners (10.2% of the resident population), mainly from Eastern Europe.
An ambulatory/office/recreational space (AOR open space) was set-up in each of these 15 micro-areas, usually in a public housing apartment, used as the operative site for the local HMP professionals for social and/or healthcare activities. The HMP professional is responsible for mapping and engaging with vulnerable individuals and assessing the resources available in the area, based on epidemiological, social data and other local information in the services and community. HMP professionals are also dedicated to providing proactive care for vulnerable subjects, linking those in need to actions provided by services, volunteers and other resources available within the community. The AORs have been designed as an open space, where people can go to “meet”, i.e. they not only go for health consultations, but also to meet one other and take part in social and everyday activities; for company, to help one another, cook together, play social games, share books and expenses. The same premises may also be used as a theatre, for dancing courses, gymnastics, computer courses, reading, etc. Some of the people who go to the AORs take on the role of experts/educators, dedicating their time and skills to the others.
2.2. Research strategy: a mix of qualitative and quantitative methods focused to causal links to gain a deeper insight
Our research strategy literally turns the approach taken in many previous studies on social capital upside down. Indeed, many of these previous studies have been criticised as they empirically measured the correlation between social capital and health indicators, deducing the existence of causality links from the statistical associations observed (Van der Gaag and Webber 2008). Conversely, whilst respecting the work of others, our intention is that of assessing the presence of these causal links in two converging ways (Astier 2005).
Firstly, the mechanisms activated by the HMP service and their impact on individual capabilities were investigated (Di Monaco 2014; Sen, 1986). Under the hypothesis that by implementing its innovative practices, HMP could trigger the growth of social mechanisms designed to create new relationships (H1), the effect of the HMP intervention on the number of relationships and the specific properties of the social capital, created in favour of a better inclusion of vulnerable individuals, was then investigated (H2). The effect the HMP had on vulnerable individuals’ capabilities to control events considered risky for their own health was also assessed (H3). This research strategy aimed at assessing whether social capital is a capacitating social infrastructure i.e., if it enables individuals to reach their objectives more easily, depending on individual resources and competencies. Furthermore, it was hypothesized that a social infrastructure can be created and/or amplified by establishing relationships through specific social mechanisms, i.e., activities generating appropriate conditions for the proactive interdependence of various individuals.
We then focused on the functioning of each social mechanism and its ability to create a stable social infrastructure. On the basis of literature data, it was assumed that social mechanisms can be determined by three characteristics, that is: considering any vulnerable individual X, the following mechanisms could elicit or amplify health-oriented behaviour: 1) strategic interdependence: when X's choices or gratifications are connected to those of other players; 2) process interdependence: when other players sequentially influence the choices of the individual X; 3) spatial-relational interdependence: when space proximity increases the number of relationships and affects the speed and direction of X's choices (Barbera 2004; Hedström 1998). These criteria have been used in empirical research to identify and recognise social mechanisms. Therefore, on the basis of these assumptions, our research was organised in two phases.
2.3. The qualitative research phase
The first phase tested the aforementioned three hypotheses (H1, H2, H3) applying qualitative methods. The presence of causal links was assessed investigating the sequence of events involved in the process, examining if they were able to generate proactive interdependence. The HPM professionals' intentional behaviour was aimed at triggering interdependence (social mechanisms), which, in turn, aimed at activating new relationships between the individuals involved (new specific properties of social capital). The new relationships would then supposedly modify behaviours potentially capable of putting their health at risk, changing individual capabilities, i.e., the choices made by vulnerable individuals and their effective possibility to make them within the social context they live in. Practically, net of differences in individual (physical and cognitive) competencies and available economic resources, vulnerable individuals would have the concrete possibility and orientation to avoid risky behaviour.
For example, someone living alone with functional limitations in walking or going out, is at risk of poor nutrition. However, if the inhabitants of that area are in the habit of doing the shopping for anybody who cannot go out and both the helper and the person helped accept their roles willingly, this health risk would be avoided by the mobilisation and reciprocity of the network. Thus, the HMP professional would work much the same as a relay does in an electrical circuit, determining a certain position or line of action, ‘opening other circuits', to activate new resources through proactive interdependence. In this way the action goes beyond the boundaries of direct support or resources that can be provided by the services offered.
The qualitative research was carried out from late 2016 to mid-2018, in collaboration with the HMP managers and professionals, in all about 80. Constructivist approach and qualitative techniques were used - 2 initial focus groups with 10 professionals in each one, 10 unstructured professionals' interviews, 10 half-day workshops with approximately 20–30 professionals in each one, 2 half-day Ateliers with 80 professionals, 5 half-day observations in AOR and discussion activities - to describe and analyse work practices, so as to perform an empirical examination of the logic of the actions taken by HMP professionals, their patients, relatives, friends and neighbours. The most significant stories that came to light during this study have been published in a volume entitled, ‘La città che cura. Micro-aree e periferie della salute’ (Gallio and Cogliati Dezza 2018). Some were also made into a film with the same title, directed by Erika Rossi, released in 2019 in selected Italian cinemas.
The chronological and logical analysis of these stories allowed for the identification of the most common adverse circumstances that potentially posed a health risk vulnerable people have to face in their everyday lives, as well as the social mechanisms promoted by the HPM professionals (H1) to allow these people to face them by enhancing their capabilities (H3), helped by the features of the newly generated social capital (H2).
2.4. The quantitative research phase
A controlled cross-sectional study was then carried out by interviewing a population sample. A semi-structured questionnaire was developed using operational definitions of problems and specific features of social capital, identified in the first phase, measuring:
-
1)
how critical problems had been faced by the individual over the previous 2 years, referring to 24 problems identified in the first phase (Table S1). The main features of the relationships experienced for each single problem were investigated and various aspects of the social capital created were assessed by different indices and techniques. These included types of activated agents, the chronology of the relationship with agents, the speed of the activation, the continuity of the support provided by neighbours and relationships, the increase in contacts with others, the ability to respond to and meet needs, satisfaction with the help received or given, and, lastly, the level of trust in future relationships and the intention of continuing them or not.
-
2)
the individual's mental health status, evaluated by the indexes of mental health (MSC-12, SF-12 questionnaire, Ware et al., 1996).
-
3)
the individual's social capital, assessed according to more traditional and consolidated theoretical perspectives: social position (Bourdieu, 1986), social cohesion and trust (Putnam, 1993).
-
4)
the individual's socioeconomic position, according to the main determinants of health: gender, age, family network (household typology), material resources (any economic difficulties, social class) and competencies (years of education).
The questionnaire took about 1 h and a half and was administered personally by social and health professionals involved in the HMP, together with some undergraduate students.
The study population was the whole population living in Trieste and in a small nearby municipality. A total of 600 individuals were sampled from the study population to allow for a comparison between individuals treated and non-treated by the HMP intervention. The population was divided into three groups (Table 1):
-
a)
treated by HMP: a random sample of 200 residents living in the Micro-areas who were provided care by the HMP at the time of the study (early 2018) (a random over-sample of 15% was added to balance all areas);
-
b)
untreated by HMP: a random sample of 200 residents living outside the Micro-Areas and matched to the 200 treated subjects, using a Propensity Score Matching (PSM) according to multiple factors measured at the beginning of the programme. These factors included gender, age, social characteristics (measured by an area social deprivation composite index, built using aggregated census-tract information on education, employment, home ownership, overcrowding, single-parent families, Caranci 2009), health characteristics (measured by the Charlson Comorbidity Index, Charlson 1987 and by the prescriptions of medicines for chronic disorders, including hypertension, peptic ulcer and diabetes);
-
c)
untreated but living in the treatment area: a random sample of 200 subjects residing in the intervention areas but not requiring care/help from the HMP. This group was matched only for gender and age to the treated group.
Table 1.
Population under study: descriptive indicators of the main characteristics of individual and living conditions in the three groups (treated in Micro-areas, untreated in MA, untreated out of MA).
| Demographic characteristics |
Resources and status |
Competencies |
Adverse events |
Health status |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Sample | Female (=1) | Age | Living alone (=1) | Economic difficulty (difficulty index growing in three areas) | Social prestige of work (increasing) Index TP1 | Education years | Total number of problems over the previous 2 years (24 areas) | Mental health index MCS_12 (increasing) | |
| number of residents treated residents in Microareas | Average | 0.72 | 69.74 | 0.57 | 1.13 | 23.57 | 9.12 | 9.29 | 41.58 |
| N | 231 | 231 | 229 | 231 | 231 | 227 | 231 | 216 | |
| std. Deviation | 0.451 | 15.038 | 0.496 | 1.036 | 15.323 | 2.360 | 3.763 | 12.940 | |
| Min-max | 26–96 | 0–3 | 10–87.70 | 8–18 | 0–18 | 11.64–70.50 | |||
| number of untreated residents in Micro-areas | Mean | 0.71 | 63.68 | 0.36 | 1.22 | 24.23 | 9.21 | 5.83 | 45.13 |
| N | 198 | 198 | 194 | 198 | 198 | 192 | 195 | 193 | |
| std. Deviation | 0.454 | 16.420 | 0.481 | 1.149 | 15.406 | 1.939 | 4.272 | 11.943 | |
| Min-max | 22–99 | 0–3 | 10–80.90 | 8–18 | 0–18 | 14.38–65.83 | |||
| N. non-treated residents outside Micro-areas | Average | 0.66 | 70.07 | 0.37 | 0.68 | 33.67 | 10.55 | 6.63 | 43.58 |
| N | 199 | 199 | 198 | 199 | 199 | 197 | 199 | 187 | |
| Std Deviation | 0.475 | 15.252 | 0.485 | 0.957 | 18.797 | 3.119 | 4.024 | 11.677 | |
| Min-max | 26–96 | 0–3 | 10–77.80 | 8–18 | 0–18 | 17.73–63.22 | |||
| Total | Average | 0.70 | 67.93 | 0.44 | 1.02 | 26.98 | 9.61 | 7.36 | 43.36 |
| N | 628 | 628 | 621 | 628 | 628 | 616 | 625 | 596 | |
| Std Deviation | 0.460 | 15.795 | 0.497 | 1.074 | 17.122 | 2.595 | 4.279 | 12.302 | |
| Min-max | 22–99 | 0–3 | 10–87.70 | 8–18 | 0–18 | 11.64–70.50 | |||
| ANOVA | F | 1.068 | 10.834 | 12.755 | 15.582 | 23.954 | 20.460 | 44.217 | 4.328 |
| p-value | 0.344 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.014 | |
The differential effects between treated and non-treated by the HMP as to the intervention on social capital were measured using two different sets of indicators of social capital properties: one was more specifically related to the HMP intervention, whilst the other represented the more traditional definitions of social capital (Table S2).
The first set of indicators was used to test whether the social mechanisms created the expected interdependence, i.e., the three specific properties of social capital of the framework reported in Fig. 1: an enhanced capability to overcome events deemed risky for the health amongst the treated individuals (SP1); a higher level of ‘empowerment’ for the treated individuals (SP2); a higher level of trust in close relationships amongst the treated individuals (SP3).
The second set tested whether the same social mechanisms influenced also the more traditional properties of social capital normally lacking in degraded urban areas, which were not expected to be modified by the HMP. These were principally social and political participation (TP2), the level of trust and ‘general’ social cohesion felt for the city (TP3) and social status (social desirability scale of occupations for Italy, Meraviglia 2007) indicator (TP1). Both sets of indicators were considered as outcomes in multiple regression models (Table 2). The indices are almost cardinal and were built through Principal Component Analysis, using sets of variables represented by Likert scales, or cardinal with count of specific sets of events (Table 2).
Table 2.
The association of treatment in Micro-areas with indicators of health and social capital traditional and specific properties (regression models).
| Determinant |
Level of Social Capital (Specific and Traditional Properties) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Risk event |
Close network (cooperation) |
Participation (cohesion) |
Trust in society (cohesion) |
|||||||||
|
Model D1 |
Model SP3 |
Model TP2 |
Model TP3 |
|||||||||
| Dependent variable: | Dependent variable: | Dependent variable: | Dependent variable: | |||||||||
| The reference is untreated, individuals residing outside a Micro-area, matched to treated individuals residing in a Micro-area, determined by Propensity Score Matching | I MCS_12 Index of mental health | SP3 Index of close and cooperation trust | TP2 Index of political and social participation | TP3 index of trust in others and in society | ||||||||
| N: 592 | N: 612 | N: 586 | N: 592 | |||||||||
| Model sig.: 0.000 | Model sig.: 0.000 | Model sig.: 0.000 | Model sig.: 0.000 | |||||||||
| Beta | t | Sig. | Beta | t | Sig. | Beta | T | Sig. | Beta | t | Sig. | |
| (Constant) | 16.190 | 0.000 | −2.817 | 0.005 | 1.645 | 0.100 | 7.588 | 0.000 | ||||
| Female | −0.049 | −1.211 | 0.226 | −0.033 | −0.852 | 0.395 | −0.090 | −2.107 | 0.036 | −0.138 | −3.367 | 0.001 |
| Age | −0.103 | −2.384 | 0.017 | −0.013 | −0.326 | 0.745 | −0.070 | −1.512 | 0.131 | −0.125 | −2.844 | 0.005 |
| Living alone | −0.085 | −2.107 | 0.036 | −0.051 | −1.331 | 0.184 | −0.018 | −0.417 | 0.676 | −0.050 | −1.214 | 0.225 |
| Economic difficulty (Index of the three areas) | −0.159 | −3.872 | 0.000 | 0.041 | 1.068 | 0.286 | 0.028 | 0.639 | 0.523 | −0.022 | −0.515 | 0.607 |
| Social prestige of work (index PT!) | −0.066 | −1.407 | 0.160 | 0.011 | 0.245 | 0.807 | 0.077 | 1.514 | 0.131 | 0.105 | 2.170 | 0.030 |
| Years of education | 0.010 | 0.226 | 0.821 | 0.051 | 1.183 | 0.237 | 0.138 | 2.801 | 0.005 | 0.102 | 2.160 | 0.031 |
| treated resident of the Micro-area. | 0.050 | 1.050 | 0.294 | 0.549 | 12.346 | 0.000 | −0.011 | −0.210 | 0.834 | −0.154 | −3.195 | 0,001 |
| untreated residents in a Micro-area. | 0.015 | 0.317 | 0.751 | 0.391 | 8.855 | 0.000 | −0.054 | −1.086 | 0.278 | 0.018 | 0.374 | 0,709 |
| Total n. Problems faced over the previous 2 years | −0.365 | −8.889 | 0.000 | |||||||||
|
Help action received |
Help given |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Model SP1A |
Model SP1B |
Model SP1C |
Model SP1D |
Model SP2 |
||||||||||||
| Dependent variable: | Dependent variable: | Dependent variable: | Dependent variable: | Dependent variable: | ||||||||||||
| The reference is untreated, individuals residing outside a Micro-area, matched to treated individuals residing in a Micro-area, determined by Propensity Score Matching | SP1A Index, quality of help received, timing, presence, spread, efficacy | SP1B Index, variety of help received (class of subjects who received help) | SP1C Index, satisfaction for the efficacy of the help received in context of the problem. | SP1D Index, Absence of help received (problems faced without help) | SP2 Index, Variety of help given to neighbours | |||||||||||
| N: 577 | N: 577 | N: 565 | N: 577 | N: 609 | ||||||||||||
| Model sig.: 0.000 | Model sig.: 0.000 | Model sig.: 0.000 | Model sig.: 0.158 | Model sig.: 0.000 | ||||||||||||
| Beta | t | Sig. | Beta | t | Sig. | Beta | t | Sig. | Beta | T | Sig. | Beta | t | Sig. | ||
| (Constant) | 8.376 | 0.000 | 5.335 | 0.000 | 8.769 | 0.000 | 1.887 | 0.060 | 3.181 | 0.002 | ||||||
| Female | 0.052 | 1.193 | 0.233 | 0.048 | 1.135 | 0.257 | 0.042 | 0.963 | 0.336 | 0.021 | 0.476 | 0.634 | −0.047 | −1.144 | 0.253 | |
| Age | 0.117 | 2.529 | 0.012 | −0.043 | −0.950 | 0.343 | 0.170 | 3.618 | 0.000 | −0.078 | −1.653 | 0.099 | −0.154 | −3.499 | 0.001 | |
| Lives alone | −0.072 | −1.638 | 0.102 | 0.030 | 0.706 | 0.480 | −0.093 | −2.091 | 0.037 | 0.069 | 1.543 | 0.123 | 0.005 | 0.114 | 0.910 | |
| Economic difficulty (Index of the three areas) | 0.023 | 0.527 | 0.598 | 0.078 | 1.803 | 0.072 | −0.049 | −1.086 | 0.278 | 0.067 | 1.476 | 0.140 | 0.136 | 3.255 | 0.001 | |
| Social prestige of work | −0.100 | −1.968 | 0.050 | 0.008 | 0.160 | 0.873 | −0.055 | −1.074 | 0.283 | 0.075 | 1.449 | 0.148 | −0.031 | −0.648 | 0.517 | |
| Years of education | −0.010 | −0.206 | 0.837 | 0.037 | 0.760 | 0.447 | 0.051 | 1.026 | 0.305 | −0.011 | −0.224 | 0.822 | 0.108 | 2.299 | 0.022 | |
| treated residents in a Micro-area. | 0.130 | 2.562 | 0.011 | 0.250 | 5.027 | 0.000 | 0.124 | 2.403 | 0.017 | 0.029 | 0.557 | 0.578 | 0.215 | 4.481 | 0.000 | |
| untreated residents in a Micro-area. | −0.050 | −0.998 | 0.319 | −0.048 | −0.981 | 0.327 | −0.005 | −0.097 | 0.923 | −0.016 | −0.317 | 0.751 | 0.116 | 2.454 | 0.014 | |
Moreover, additional composite outcome indicators were elaborated applying the Principal Component Analysis to test the H2 and H3 hypotheses: the Engagement Creation (EC) index assesses the HMP professionals’ role by asking the respondents who pushed them to help their neighbours (Table 2), the SP3 Index of close and cooperation trust evaluates faith in close neighbours (Table 2) and the Degradation of the living environment (D) index assesses the perception of degradation in an urban context: rubbish left in the street, parking difficulties, inadequate public transport, heavy traffic, air pollution, noise, criminality, unpleasant odours, poor street illumination and badly maintained pavements (Table 2).
The descriptive analyses compared the socio-demographic characteristics and the indices created for the three groups by the one-way analysis of variance (ANOVA).
Data were also analysed by multiple regression, setting as the reference group the non-treated individuals living outside the Micro-areas. The treated group and the untreated group resident in the Micro-areas are reported in the regression analysis as two specific independent variables. Indicators of the biological profile (gender and age), functional autonomy (living alone), competencies (years of education), material resources (economic difficulties over the previous two years), and social status (TP1 index) were included in each regression model to control for potential confounders.
No ethical approval was required for the study, because the assessment of HMP was committed by the Local Health Authority as part of the public health intervention and all analyses were carried out on anonymous datasets obtained from the same Authority.
3. Results
3.1. The results of the qualitative phase
The qualitative analysis revealed that the work of the HMP professionals was inspired by a common vision and line of action, with the conscious and constant use of various social mechanisms. The following eight mechanisms were identified and selected, as they responded to the aforementioned empirical criteria: activation, trust, recognition, inclusion, coordination, cooperation, integration and education.
An analysis of the real-life stories verified that each of these social mechanisms created new inter-dependence (Table S3) between professionals, vulnerable individuals, neighbours and others within the Micro-areas. More specifically, each of these social mechanisms included the three characteristics aforementioned as definition criteria, i.e., strategic, process and spatial-relational interdependence. They generated strategic interdependence, offering new material, symbolic and gratification advantages derived from the new relationships with others. These benefits derived from the involvement in collective processes, where individuals give gifts, exchange time and resources and together create new scenarios and alliances to face problems. In turn, the desirable and possible choice options, as well as the basic social norms which indicate appropriate behaviour within the community, were modified. Moreover, process inter-dependence was also created because collective practices are linked together, over time, due to the conditions they create, the synergies they predispose, etc. Step by step, they progressively allow experimenting the concrete practicality of reciprocity and an incremental growth in trust. Lastly, individuals systematically exploit spatial-relational inter-dependence, creating the physical and social conditions of closeness, as well as new means of representation. This gives meaning to the new behaviors and allows for the concrete use of physical and social spaces to share experiences in person.
During this phase we were able to verify that the way social mechanisms work and the new specific properties of social capital give a plausible explanation of most evident empirical phenomena (collaborative behaviour, exchange, aid, etc.) which have been narrated, observed and filmed by the actors, to tell others about the change that has taken place. These include going regularly to the collective spaces available in the Micro-area, the willingness to give and mutually help others, as well as the visible cooperation and sociability observed in these premises.
This is exactly the opposite to how things were before the HMP intervention, where these areas and their inhabitants were encompassed in sentiments like diffidence and abandonment.
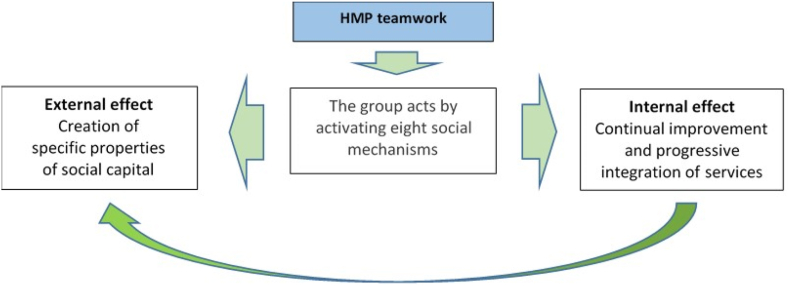
Moreover, it came to light that the coherent application of these social mechanisms also influenced the organization of public socio-health services in two ways (Fig. 2): 1) it engaged professionals in the continual improvement of services for vulnerable individuals, following the lean-organizational model, and 2) it allowed for progressive integration of the various processes and services supporting vulnerable individuals, in response to their needs.
Fig. 2.
HMP intervention: effects of social mechanisms.
The data obtained evidenced that the team running the programme was characterized by a shared concept of the mission. It was found that the HPM professionals had a strong sense of involvement and responsibility and the social-health services were strongly involved in the empathy created when listening to what the vulnerable individuals chose to share with them. The professionals stated that their special attention in this phase of feedback stemmed from the commitment to match the activities of the various services (integration mechanism) with the needs expressed or identified, and that this matching is constantly checked.
The team work was described by the professionals as a pivotal reference point (cooperation and trust mechanisms). Indeed, they were strongly motivated (recognition mechanism) and showed strong social and life skills, as well as expertise in the nursing-social area. They also had common training and intense peer review of work practices (inclusion and learning mechanisms). In fact, it emerged that, in order to activate the eight aforementioned social capital creation processes, they also need to share, in some way or another, the organizational experience and culture of the whole team.
Another qualifying element of the team work that emerged during the observation phases was that the inter-institutional group that manage the programme (coordination mechanism) operates with a clear commitment from the three organising institutions (ASUIT, the local health authority, the Trieste municipality, the local social authority and ATER, the local housing authority). Furthermore, close horizontal communication between these institutions is embedded within their organisations (integration mechanism), without barriers from the respective bureaucracies.
The way the HMP professionals operated within the territories differed greatly from mechanical applications of care pathways, where the process is focused more on individual pathology rather than on the individual's social contexts and health and where, more often than not, there is a strict separation between specialities and the responsibilities are distinguished precisely between professions and specialities.
3.2. Results of the quantitative phase
Phase two of the research was concentrated on a quantitative evaluation of the hypotheses H2 and H3.
The descriptive analysis (Table 1), as expected, evidenced that the treated group resident in the Micro-areas had a considerable disadvantage for most individual and contextual social indicators, compared to the untreated out of the Micro-areas (p-value <0.001 for living alone, economic difficulty, social status, years of education and p-value of = 0.014 for mental health), whilst neither age nor gender differed statistically between the two groups, due to the PSM sampling methodology. It is noteworthy that 10 years earlier, when the sampling was performed, these two groups had been matched for health and proxies of socio-economic conditions. After which, the treated group had 40% more adverse events in the 2 years before the interview than the other group. This may well explain the worse self-perceived mental health in this group, as evidenced by the SF-12 mental health index MCS-12. These differences also imply that the HMP intervention in the Micro-areas was effectively targeting vulnerable individuals in difficulty.
An additional question was put to the respondents i.e., “which three meeting places near your home would you be more willing to go to?” The replies to this question provided further evidence that the action triggered by the social mechanisms were linked to the use of social spaces able to enhance empowerment and trust (H2 and H3). This open question was then classified. A total of 77% of both genders treated residing in a Micro-area put the AOR open space of their Micro-area first, followed by a long list, including for males bars (Italian coffee shops-licensed for alcohol)/restaurants (33%), public gardens (15%) and shops (10%), while females' preferences were: bars (22%), gardens (12%), the parish (11%), day centres (10%) and neighbours' backyards (10%), leaving relatives’ homes, clubs and shopping centres at the bottom of the list.
Untreated males not residing in a Micro-area put bars first (52%), followed by gardens (26%), shopping centres (11%) and libraries (11%). A meaningful 13% did not indicate any area at all.
The untreated females not residing in a Micro-area chose bars first (29%), followed by the parish (27%) gardens (27%), shops (11%) and shopping centres (11%), while 14% of them did not indicate any place they would go to willingly.
The untreated individuals residing in a micro-area came somewhere between these two positions. The AOR open space within their micro-area was the first choice for almost 50% of both genders. This was followed for males by bars (42%), gardens and walks (29%), and for females by bars (34%), public gardens (27%), shops (15%) and the parish (11%).
The regression analysis revealed three findings concerning the extent of changing behaviour.
-
1)
The SP1 index showed that vulnerable individuals following the HMP programme had more capabilities to overcome events considered risk factors for their health.
This finding is evidenced in each of the models (see Table 2): model SP1A shows that the treated group had statistically significantly higher satisfaction (p-value = 0.011) with the quality of the help received (timing, presence, variety of actors and efficacy perceived in each of the 24 problematic areas); model SP1B shows that more treated individuals were involved in the processes of helping out (p-value <0.001); model SP1C shows that these treated individuals were more able to cope with, and overcome, risky events (p-value = 0.017).
Although there was no significant difference between the treated and untreated groups as to how often vulnerable individuals were left alone to face critical events without aid (Model SP1D) (p-value = 0.578), this result should be interpreted as a positive one, as the treated individuals had more unfavourable background conditions, i.e., with fewer resources and relationships to help them overcoming an adverse event. In summary, the HMP intervention empowered vulnerable individuals when facing risky events, giving them real additional responses and alternatives. This evidence should be considered together with the second point, which qualified the HMP still further.
-
2)
The intervention was associated with mobilisation and empowerment of these vulnerable individuals (index SP2).
The SP2 Model shows that the treated individuals were actually more active in helping their neighbours when they had to face problems they themselves had been helped to overcome (p-value <0.000). Interestingly, this helping behaviour spread to untreated individuals in close contact with treated ones (Model SP2: significant regression coefficient of non-treated residents in the Micro-area p-value = 0.014).
Yet another confirmation of the efficacy of this process comes from the engagement creation EC index (Table S4). The HMP professionals were recognised as players who mobilised the process (HMP professionals’ index: 1.896 against 0.005, p-value<0.001; other professionals: 0.087 against 0.020, p-value = 0.067), creating motivation, justification and effective reciprocity. Moreover, this role was also significantly recognised by neighbours in the intervention area (index 1.519 against 0.920, p-value = 0.004) and friends (0.506 against 0.307, p-value = 0.090). This point shows that the virtuous cooperation circle is no longer dependent only on the HMP professionals, but has rather become a widespread social practice involving neighbours.
Further confirmation of the cultural changes associated with the intervention comes from the social representation of the treated group regarding cooperation within their specific living context, as shown in the following point.
-
3)
The intervention was associated with a higher degree of trust in vulnerable individuals, i.e. counting on receiving help from others close to them.
The SP3 Index of close and cooperation trust (factor) shows a high degree of positive judgment among the responders residing in a Micro-area with the items on trust ‘where I live’. This positive image was more prevalent in the treated (Variable SP3, Table 5, p-value <0.001, treated = factor average 0.441, 72% of subjects above the average), compared to untreated individuals not resident in a Micro-area (untreated = factor average −0.669, 22% above the average), despite the fact that they shared worse socio-economic and health conditions and lived where degradation was more acute. The level of positive judgement also appears to have a ‘ripple effect’, as it spread to untreated individuals residing in the intervention area (Table 2, regression model SP3, treated p < 0.001, non-treated individuals residing in a Micro-area p-value <0.001).
This positive image of the living area contrasts with the negative perception of urban neglect. Indeed, the D index of the degradation of the living environment (Variable index D, Table S4, p-value = 0.002, treated = factor average 0.104), which does not depend on the intervention, shows an inverted trend and the treated individuals’ judgment is worse than the others (54.5% above the average against 53%). This would indicate that greater trust is very specific and is linked to close relationships, which were modified by the intervention.
The traditional measure of social capital gave a further confirmation of our hypothesis that more specific properties of social capital were created by social mechanisms. The first traditional indicator of social capital is the index of civic and association participation (TP2), according to Putnam's concepts of cohesion and civicness (1993). The second is an index of trust in others and in society (TP3), measuring the degree of trust in social cohesion. The first indicator did not seem to be affected by the intervention (Mod. TP2, Table 2, treated p-value = 0.834), while it was sensitive to gender (p-value = 0.036) and to the educational level (p-value = 0.005), with more males and higher educated people showing greater participation. On the other hand, the second indicator showed a strong divergence in the treated group between general mistrust in others (Mod TP3, Table 2, treated p-value = 0.001 and beta with a negative sign) and trust in those whose cooperation and reciprocity was experimented (Mod SP3, Table 2, treated p-value <0.001 and non-treated residents p-value <0.001), which would therefore seem acquired thanks to the intervention.
There were no statistically significant differences in mental health between treated individuals residing in Micro-areas and untreated ones residing outside Micro-areas (Table 2). However, applying the regression coefficients for mental health of the social determinants of those untreated to the prevalence of exposure to social determinants in the treated group in Micro-areas, the observed mental health level of those treated corresponded to an MSC-12 index of 41.67 (IC 95% 39.92–43.42). This was higher than the expected value based on the experience of the untreated peers (MCS-12 = 39.88), suggesting a higher degree of mental health protection among the treated group.
5. Discussion and policy implications
5.1. Research pros and cons
The local health authority requested an evaluation of the HMP impact only ten years after the programme had been implemented. This differs greatly from the randomized control trial paradigm that would be required for an efficacy evaluation of new technologies, including social and organizational innovations like the HMP.
Therefore, our study aimed at the recreation of quasi-experimental conditions of observation by comparing subjects in degraded Micro-areas targeted by the intervention with individuals from the rest of the city at the start of the study, by means of PSM techniques. It seems unlikely that the treated and untreated groups could have a different propensity to the creation of social relations, facing critical events a priori. However, only a few health and social variables available in the Regional Health Service information system were used for the PSM, meaning that the matching may not have been as complete as it could otherwise have been.
Furthermore, the interviews in the second phase were carried out by employees of the three local authorities engaged in the programme and in the qualitative part of the study. Due to the impossibility to blind the interviewers, each of them was assigned to interview only people he/she did not directly know or provide with care services. In any case the interviewers were not competent in the complex causal chain of mechanisms they were investigating with the questionnaire, so that knowing the treatment status of the interviewed should not have influenced their accuracy in the interview. For instance, as described in the results section, the fact that the two groups of untreated, residing inside and outside the micro-areas, showed different results, reassures that the interviews were able to detect plausible findings.
As to the health outcome of the intervention, the cross-sectional design of the research did not allow for a comparison of changes in mental health before and after the intervention in the three groups. However, it was possible to make an indirect estimation of the level of mental health expected amongst the treated individuals should they not have taken part in the programme and been treated, using the mental health experience of their pairs in the untreated group residing outside the Micro-areas. The differences in mental health observed from models adjusted for socio-economic conditions suggest that the treated groups had a more favourable health outcome than expected. Admittedly, it is hard to interpret this finding as attributable to the intervention without a pre-intervention assessment of mental health, even if it is quite unlikely that social inequalities in mental health vary between treated and untreated areas, whatever the intervention.
In spite of these limitations, the association observed between the intervention and the new specific properties of social capital could be interpreted as causal for several reasons. The control group of untreated individuals residing outside the Micro-areas had a traditional social capital (index TP1, Table 1), measured through social prestige linked to their profession, significantly more favourably than the other two groups. Quite the opposite, the treated group in the Micro-areas had the lowest values and the non-treated group in the Micro-areas had intermediate values. Conversely, all the indicators targeted by the intervention, i.e. the specific properties of social capital and the level of empowerment and trust in neighbours, showed that the treated individuals had higher levels.
Above all, the results are extremely coherent with the hypothesized chain of mechanisms that links intervention to social capital. The availability of a local premises (AOR) as a base for the social-health service modified the choice as where the individuals would like to go in theirs and their relatives' daily lives. It bridged a gap providing treatment, help and reciprocity within a wider social context. This could also explain the stability over time of the social mechanisms we observed, which, in turn, became cultural and social practices in the places used in everyday life. A need for reciprocity and expression emerged, which otherwise might not have come to light had it not been rooted within the relational neighbourhood. When we asked who held the keys for the premises, the professionals said that they really did not know as it was a ‘common home’ for the many people involved in contributing to its social life.
5.2. The change in health service organization
Noteworthy is the fact that the HMP organizational profile looks antithetical to traditional service bureaucracies (Laverack, 2016). A sharp distinction between the HMP intervention and the more common social assistance interventions emerges (see results of model SP2), where total inactivity (dependence) of the recipient would be justified. It also shows an enhancement of both capabilities and empowerment, as helping implies activating cognitive, technical and social abilities. The individuals assume active roles in this context, far from the stereotypes of ‘patient’, or ‘assisted subject’. This role can be considered preventive or curative, especially for the individuals themselves and their self-esteem. It can also be taken as a sign of changing attitudes and social norms in the neighbourhood.
This performance corresponds to a radical choice of managerial and innovative strategies in the organization of services (Andersen 2014; Galgano 2006; Ohno, 1988; Womack 1991). The team that jointly ran the programme essentially acted according to the principles of lean organisations and ‘distributed leadership’ (Barrett, 2012; Di Monaco 2016; Konradt, 2013), had strong social (Winterton, Delamare-Le Deist, & Stringfellow, 2006) and life skills (WHO, 1997), and a learning approach to work practices (Nahapiet 1998; Nonaka 1995; Wenger 2000).
Therefore, it seems that, if the aforementioned processes of social capital creation are to be activated, then the professionals involved should also introduce innovations in organization. This is consistent with studies that identify organizational culture as a qualifying element for the production of personalized and quality services for the customer (Normann, 1985; Schein, 2010; Weick, 1969).
Moreover, the two main directions of the team work action, i.e., - towards the person and the community and towards the organization and integration of services - are also the main areas of innovation promoted by the Chronic Care model (WHO, 2016) and by more Integrated Community Care/prevention interventions. We believe that our results can be considered an empirical assessment of some of the social mechanisms underlying these models.
5.3. The generation of social capital and the role of public services
This study suggests some conclusions for further research and policy implications. What type of social capital should be considered to improve health and reduce inequalities? There are various mechanisms for the creation of social capital: those deriving from having a strong social position, or belonging to historically cohesive communities characterized by a high degree of participation and trust, or becoming part of active or dynamic networks, and so on. Our data indicate that social infrastructures can be built in situations where individuals are outside these networks and are, therefore, more exposed to health risks, through increasing their capacity of control over adverse circumstances, both at an individual and collective level. It is in the light of this perspective that public services and their personnel may play a pivotal role. This involves continually feeding the social infrastructure by creating strategically specific social mechanisms. This research shows that this does not correspond to a ‘job change’ for the professionals, but rather means performing well their own social and health work within a service culture oriented towards the individual and health. This is not simply a matter of making investments in traditional organisations, but rather of adapting these investments and the culture of the organisations to determined priorities, which include the nurturing of specific social mechanisms within the activity of the public services in question, as well as of the third sector.
This puts questions concerning the productivity of social capital into sharp focus. Social capital should derive from the action of services aimed at promoting the value of the person and the social resources available. The recent history of many organisations involved in sustainability and corporate social responsibility shows that this is also the way to enhance professionals' value, within organisations capable of offering quality services in response to people's needs.
This strong link between how services work and the generation of social capital within the community is coherent with much of the recent published literature. This underlines the importance of social and organizational innovation, the integration of services (Hyde-Peters 2016, Seah 2018), and the inefficiency of transmission of codified best practices (Minkman, 2012) and technological solutions (Greenhalgh 2017) if these are not re-elaborated through learning processes, cultural change and service organization development. The same goes for actions aimed at enhancing the quality of the services by increasing investment in technology (even sophisticated), which does not have a coherent effect on the development of relationships between people and within the community.
The way social capital and its effects on health are measured is a critical point. This aspect should become part of how integrated health and social services continually assess and improve their own ability to create social infrastructures by engaging people. Systems to monitor and evaluate the quality of an impact, as in many other sectors, should all be functional to the processes of taking decisions and learning, so as to improve the quality of relationships amongst people. Numerous failures in the public services when attempting to establish and maintain good relationships with those who have social and health problems can be considered in this prospective. The vicious circle that connects social events risky for health, the lack of social capital and health events must be broken.
More generally, the process of change that emerges from our study is coherent with the theoretical and methodological approach of action research (Dubost, 1984), according to which subjects cooperate to transform their own reality as it is with Elinor Ostrom's concept that the management of common goods should be run through the activation of forms of self-mobilisation and self-organisation, aimed at obtaining permanent collective advantages, thus overcoming the opposition between rigid traditional functions of the state and the market (Ostrom, 1990; Roy 2014; Lang 2019).
Indeed, it seems that the HMP intervention has been able to develop a new ‘local’ model of generative welfare, even if it stemmed from an institutional context within a typically Mediterranean traditional welfare system (Esping-Andersen, 1999). In such a context, mutual aid relationships among people who are not kin are less frequent than in other European countries, and, above all, are considered a substitute for services and functions that the state and the market are unable to supply (Albano et al., 2010).
As it emerged from our research, these simplistic or even ‘dark-side’ interpretations of social capital (Villalonga-Olivesa 2017) can be modified. Socially shared relationships can evolve, creating innovative institutional ‘islands’ within existing contexts. These could be new ‘local models” of a universalistic welfare system, models that are both inclusive and able to increase people's capabilities at the same time, which could be disseminated and applied to other contexts.
Ethics
Ethical approval was not required, as analyses were carried out on completely anonymized anonymous datasets extrapolated from the Public Health Authority registers.
Authorship contributions
Please indicate the specific contributions made by each author (list the authors’ initials followed by their surnames, e.g., Y.L. Cheung). The name of each author must appear at least once in each of the three categories below.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgment
This work was undertaken with the contribution of the pubblic health service "Azienda sanitaria universitaria Giuliano Isontina - ASU GI", the Municipality of Trieste and the Agency for council housing "Azienda Territoriale per l'Edilizia Residenziale di Trieste" - ATER.The authors wish to acknowledge all the Habitat Micro-area Program managers and professionals for their willingness to contribute to the study and for their constructive feedback and suggestions, all of which added considerable value to the research.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ssmph.2020.100677.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Albano R., Barbera F. Social capital, welfare state, and political legitimacy. American Behavioral Scientist. 2010;53(5):677–690. [Google Scholar]
- Andersen H., Røvik K.A., Ingebrigtsen T. Lean thinking in hospitals: Is there a cure for the absence of evidence? A systematic review of reviews. BMJ Open4. 2014 doi: 10.1136/bmjopen-2013-003873. http://10.1136/bmjopen-2013-003873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astier M.A. Social capital and mental health: An interdisciplinary review of primary evidence. Social Science & Medicine. 2005;61:943–964. doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- Barbera F. Meccanismi sociali. Elementi di sociologia analitica. Il Mulino; Milano: 2004. [Google Scholar]
- Barrett F.J. Harvard Business Review Press; Boston: 2012. Yes to the mess: Surprising leadership lessons from jazz. [Google Scholar]
- Bird C., Conrad P., Fremont A., Timmermans S., editors. Handbook of medical sociology. 6th ed. Vanderbilt University Press; Nashville: 2010. [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson J.G., editor. The handbook of theory: Research for the sociology of education. Greenwood Press; New York: 1986. pp. 241–258. [Google Scholar]
- Caranci N., Costa G. Un indice di deprivazione a livello aggregato da utilizzare su scala nazionale: Giustificazioni e composizione dell’indice. In: Costa G., Cislaghi C., Caranci N., editors. VIII. Salute e Società; 2009. pp. 58–78. (Disuguaglianze sociali di salute. Problemi di definizione e di misura). [Google Scholar]
- Carpiano R. Actual or potential neighborhood resources for health. In: Kawachi I., Subramanian S.V., Kim D., editors. Social Capital and Health. Springer; Berlin: 2008. pp. 83–93. [Google Scholar]
- Centola D. How Behavior Spreads: The Science of Complex Contagions. Princeton University Press; Princeton: 2018. [Google Scholar]
- Charlson E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Coleman J.S. Harvard University Press; Massachusetts: 1990. Foundations of social theory. [Google Scholar]
- Craig P., Cooper C., Gunnell D., Haw S., Lawson K., Macintyre S., Ogilvie D., Petticrew M., Reeves B., Sutton M., Thompson S. Using natural experiments to evaluate population health interventions: New medical research council guidance. Epidemiology and Community Health. 2012;66:1182–1186. doi: 10.1136/jech-2011-200375. https://doi:10.1136/jech-20 11-200375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Monaco R., Pilutti S. Le azioni di correzione nel senso dell’equità delle politiche non sanitarie. In: Costa G., Bassi M., Gensini G.F., Marra M., Nicelli A.L., e Zengarini N., editors. (a cura di), L’equità nella salute in Italia, Fondazione. Smith Kline presso Franco Angeli; Milano: 2014. [Google Scholar]
- Di Monaco R., Pilutti S. Egea; Milano: 2016. Scommettere sulle persone. La forza della leadership distribuita. [Google Scholar]
- Dubost J. Une analyse comparative des pratiques dites de Recherche-Action. Connexions. 1984;43:8–28. [Google Scholar]
- Edwards K.L., Clarke G.P., Ransley J.K., Cade J. The neighbourhood matters: Studying exposures relevant to childhood obesity and the policy implications in leeds, UK. Epidemiology and Community Health. 2010;64:194–201. doi: 10.1136/jech.2009.088906. [DOI] [PubMed] [Google Scholar]
- Esping-Andersen G. Social foundation of postindustrial economies. Oxford University Press; Oxford: 1999. [Google Scholar]
- Gale N.K., Kenyon S., MacArthur C., Jolly K., Hope L. Synthetic social support: Theorizing lay health worker interventions. Social Science & Medicine. 2018;196:96–105. doi: 10.1016/j.socscimed.2017.11.012. [DOI] [PubMed] [Google Scholar]
- Galgano A., Galgano C. Guerini e associati; Milano: 2006. Il Sistema Toyota per la Sanità. Più qualità meno sprechi. [Google Scholar]
- Galster G. The mechanism(s) of neighbourhood effects: Theory, evidence, and policy implications. In: Van Ham M., Manley D., Bailey N., Simpson L., Maclennan D., editors. Neighbourhood effects research: Theory and evidence. Springer; Dordrecht: 2012. pp. 23–56. [Google Scholar]
- Greenhalgh T., Wherton J., Papoutsi C., Lynch J., Hughes G., A'Court C., Hinder S., Fahy N., Procter R., Shaw S. Beyond adoption: A new framework for theorizing and evaluating non adoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research. 2017;19(11):e367. doi: 10.2196/jmir.8775. https://doi: 10.2196/jmir.8775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedström P., Swedberg R., 1998Hendryx M.S., Ahern M.M., Lovrich N.P., McCurdy A.H. Vol. 37. 1998. Social mechanisms: An analytical approach to social …; p. 1. ((2002), access to health care and community social capital HSR: Health services research). (February 2002) [PubMed] [Google Scholar]
- Hyde-Peters Z., Simkiss D. Social capital and community development in child health. Paediatrics and Child Health. 2016;26:205–211. [Google Scholar]
- Jones R., Heim D., Hunter S., Ellaway A. The relative influence of neighbourhood incivilities, cognitive social capital, club membership and individual characteristics on positive mental health. Health & Place. 2014;28:187–193. doi: 10.1016/j.healthplace.2014.04.006. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Subramanian S.V., Kim D. Social Capital and Health. In: Kawachi I., Subramanian S.V., Kim D., editors. Social Capital and Health. Springer; Berlin: 2008. pp. 1–26. [Google Scholar]
- Konradt U. Toward a theory of dispersed leadership in teams: Model, findings, and directions for future research. Leadership. 2013;10:289–307. [Google Scholar]
- Lang R. Rural social entrepreneurship: The role of social capital within and across institutional levels. Journal of Rural Studies. 2019;70:155–168. [Google Scholar]
- Laverack G. Macmillan education; Palgrave: 2016. Public health, power, empowermet and professional practice. [Google Scholar]
- Marmot M. University College; London: 2010. The Marmot review final report: Fair society, healthy lives. [Google Scholar]
- Meraviglia C., Accornero L. La valutazione sociale delle occupazioni nell'Italia contemporanea: Una nuova scala per vecchie ipotesi. Quaderni di Sociologia. 2007;45:19–73. [Google Scholar]
- Minkman M.N. Developing integrated care. Towards a development model for integrated care. International Journal of Integrated Care. 2012;12:e197. PMCID: PMC3601512. [Google Scholar]
- Moore S., Kawachi I. Twenty years of social capital and health research: A glossary. Journal of Epidemiology & Community Health. 2017;71:513–517. doi: 10.1136/jech-2016-208313. https://doi:10.1136/jech-2016-208313 [DOI] [PubMed] [Google Scholar]
- Moore S., Stewart S., Teixeira A.J. Decomposing social capital inequalities in health. Epidemiology and Community Health. 2014;68:233–238. doi: 10.1136/jech-2013-202996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahapiet J., Ghoshal S. Social capital, intellectual capital, and the organizational advantage. Academy of Management Review. 1998;23(2):242–266. [Google Scholar]
- Nonaka I., Takeuchi H. Oxford University Press; Oxford: 1995. The knowledge creating company. [Google Scholar]
- Normann R. Etas; Milano: 1985. La gestione strategica dei servizi. [Google Scholar]
- Ohno T. Productivity Press; Portland, Oregon: 1988. Toyota production system: Beyond large-scale production. [Google Scholar]
- Ostrom E. Cambridge University Press; Cambridge: 1990. Governing the commons. The evolution of institutions for collective action. [Google Scholar]
- Pentland A. Università Bocconi Editore; Milano: 2015. Fisica sociale. Come si propagano le buone idee. [Google Scholar]
- Putnam R. Leonardi Editore; Milano: 1993. La tradizione civica nelle Regioni italiane. [Google Scholar]
- Roberts J., Bell R. UCL Institute of Health Equity; London: 2015. Social inequalities in the leading causes of early death. A life course approach. [Google Scholar]
- Roy M.J., Donaldson C., Baker R., KerrS The potential of social enterprise to enhance health and well-being: A model and systematic review. Social Science & Medicine. 2014;123:182e193. doi: 10.1016/j.socscimed.2014.07.031. https://10.1016/j.socscimed.2014.07.031 [DOI] [PubMed] [Google Scholar]
- Schein E. John Wiley & Sons; New York: 2010. Organizational culture and leadership. [Google Scholar]
- Sen A. Il Mulino; Bologna: 1986. Scelta, benessere, equità. [Google Scholar]
- Van Der Gaaga M., Snijdersb T.A.B. The resource generator: Social capital quantification with concrete items. Social Networks. 2005;27:1–29. [Google Scholar]
- Van Lenthe F.J., Borrell L., Costa G., Diez R., Kauppinen T., Marinacci C., Martikainen P., Regidor E., Stafford M., Valkonen T. Neighbourhood unemployment and all cause mortality: A comparison of six countries. Journal of Epidemiology & Community Health. 2005;59(3):231–237. doi: 10.1136/jech.2004.022574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villalonga-Olivesa E., Kawachi I. The dark side of social capital: A systematic review of the negative health effects of social capital. Social Science & Medicine. 2017;194:105–127. doi: 10.1016/j.socscimed.2017.10.020. [DOI] [PubMed] [Google Scholar]
- Villalonga-Olivesa E., Wind T.R., Kawachi I. Social capital interventions in public health: A systematic review. Social Science & Medicine. 2018;212:203–218. doi: 10.1016/j.socscimed.2018.07.022. [DOI] [PubMed] [Google Scholar]
- Ware J.E., Kosinski M., Keller S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Waverijn G., Heijmans M., Groenewegen P. Chronic illness self-management: A mechanism behind the relationship between neighbourhood social capital and health? The European Journal of Public Health. 2016;27(4):594–599. doi: 10.1093/eurpub/ckw185. [DOI] [PubMed] [Google Scholar]
- Weick K.E. Addison-Wesley; Reading: 1969. The social psychology of organizing. [Google Scholar]
- Wenger E.C., Snyder W.M. Communities of practice: The organizational frontier. Harvard Business Review. 2000;78(1):139–145. [Google Scholar]
- WHO . WHO; Geneva: 1997. Life skills education in schools. WHO/MNH/PSF/93.7A.Rev.2. [Google Scholar]
- WHO European review of social determinants of health and the health divide. The Lancet. 2012;380:1011–1029. doi: 10.1016/S0140-6736(12)61228-8. [DOI] [PubMed] [Google Scholar]
- WHO . Integrated care models: an overview. WHO Regional Office for Europe; Copenhagen: 2016. https://www.euro.who.int/__data/assets/pdf_file/0005/322475/Integrated-care-models-overview.pdf [Google Scholar]
- Wilmot N.A., Dauner K.N. Examination of the influence of social capital on depression in fragile families. Journal of Epidemiology & Community Health. 2017;71:296–302. doi: 10.1136/jech-2016-207544. [DOI] [PubMed] [Google Scholar]
- Winterton J., Delamare-Le Deist F., Stringfellow E. Vol. 64. Cedefop; Luxemburg: 2006. https://www.cedefop.europa.eu/files/3048_en.pdf (Typology of knowlwdge, skills and competencies: Clarification of the concept and prototype). [Google Scholar]
- Womack J.P., Jones D.T., Roos D. Free Press; Massachusetts: 1991. The machine that changed the world: The story of lean production. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.