Abstract
Objective
Goal of this study was to investigate, whether sialendoscopy in obstructive salivary gland disorders affects patients' oral health‐related quality of life compared to healthy individuals, and to determine factors that might influence this relationship.
Study design
Retrospective observational study.
Setting
University of Kiel, Department of Otorhinolaryngology, Head and Neck Surgery.
Subjects and methods
A group of 130 patients, undergoing sialendoscopy between 01/2004 and 06/2017 was considered. Oral health‐related quality of life was assessed using the OHIP‐G14 (Oral Health Impact Profile) in combination with a custom‐made questionnaire on satisfaction and success in relation to sialendoscopy.
Results
Oral health‐related quality of life of patients without dentures or with removable dentures was significantly worse than in the healthy population, whereas the necessity of multiple additional follow‐up treatments was associated with worse oral health‐related quality of life. No essential predisposing factors were identified. Average satisfaction with the intervention was observed to be x̅ = 4.33 (SD = 3.69) on a visual analogue scale from 1 (=very satisfied) to 10 (=very unsatisfied). A longer follow‐up period and a higher patients' age were positively related, whereas removal of salivary gland during follow‐up was negatively related to satisfaction. In 113 cases (86.9%) long‐term preservation was accomplished and 115 (88.5%) patients would repeat a sialendoscopy in case needed.
Conclusion
In summary, sialendoscopy resulted in long‐term high subjective and objective success rates. However, oral health‐related quality of life scores did not reach those levels found in the healthy population.
Keywords: OHIP‐G14, oral health‐related quality of life, outcome, Sialendoscopy
1. INTRODUCTION
Obstructive disorders of the major salivary glands manifest mainly by recurrent pain and swelling during food intake. Often, those symptoms are associated with recurrent inflammation requiring antibiotic treatment. As food intake is naturally a basic need but also part of social interactions, a decrease in quality of life appears reasonable. Sialendoscopy is a therapeutic procedure that gained increased popularity in minimally invasive gland‐preserving surgery. However, to date, almost no consistent and validated studies on the effect of sialendoscopy on quality of life of the affected patients combined with surveys on further course of treatment or satisfaction have been conducted. Especially an association between any predisposing factors and self‐reported quality of life and satisfaction with treatment should be analyzed.
2. MATERIAL AND METHODS
Retrospectively, a group of 477 patients, who underwent sialendoscopy during January 2004 and June 2017 at the University of Kiel, Department of Otorhinolaryngology, Head and Neck Surgery, was analyzed. Twelve patients (1.9%) who were underage during the time of procedure were excluded in the following analyses. On those 477 patients 612 surgeries were performed. 130 patients provided the requested questionnaires and signed declaration of consent. The study was approved by the ethics committee of the Faculty of Medicine of Kiel University (file number: D 533/17).
191 endoscopies were conducted on these 130 patients. Those were evaluated in respect of the detailed surgery procedures such as papillotomy, (extended) incision of the salivary duct, bougienage (by: balloon, probe, water pressure, guidewire with Seldinger‐technique and conical bougies, sialendoscope), methods of stone extraction, laser treatment, instillation of cortisone, the presence of sialolithiasis vs no sialolithiasis and local vs general anesthetics.
Above mentioned patients were requested to fill out and return two questionnaires by mail. Questionnaires were the OHIP‐G14 (Oral Health Impact Profile) inquiring oral health‐related quality of life (OHRQoL) and an additional self‐made questionnaire inquiring success measured by possible follow‐up treatment and subjective satisfaction with the endoscopic treatment (Figure 1, Figure 2).
FIGURE 1.

Second questionnaire (original version)
FIGURE 2.

Second questionnaire (translated version)
The OHIP‐G14 is a tool assessing the oral health‐related quality of life consisting of 14 items based on the English version of the Oral Health Impact with 53 items, which was originally developed by Slade et al in Australia. 1 John et al published the German version with 49 items in 2002 and soon afterwards shortened versions of 5, 14, and 21 items. 2 In this study, the 14‐item version is being used, incorporating two items respectively of the dimensions: functional limitation, physical pain, psychological discomfort, physical, psychological and social disability, and handicap. 3 The 14 questions refer to the period of the previous month and can be answered with “0 = never,” “1 = rarely,” “2 = sometimes,” “3 = often,” and “4 = very often.” Hence, the total score ranges between 0 and 56, with a higher score indicating poorer quality of life. For the sake of greater interpretability John et al also published normal population based scores, however because denture usage was strongly associated with OHIP‐summary scores the authors make a distinction between patients without, with removable and complete dentures. 3
The second questionnaire consists of four questions inquiring the following dimensions to obtain the course of disease and global subjective satisfaction: surgery success on the basis of follow‐up therapy, occurrence of salivary gland removal during the course of disease, willingness to undergo sialendoscopy for similar symptoms and satisfaction with the success of the endoscopic treatment on a visual analogue scale from 1 = very satisfied to 10 = very unsatisfied (Figure 1, Figure 2).
2.1. Statistics
The statistical software package IBM SPSS Statistics (version 22.0.0.2 for Windows, IBM, 2013) was used to calculate descriptive statistics and to perform inferential tests. For categorical and dichotomous variables we report absolute and relative frequencies. Differences between subgroups were compared with the chi‐squared test. For metric variables, mean and standard deviations were calculated and compared with a two‐sample t‐test for independent samples. Associations between variables were specified with correlation coefficients. For dichotomous variables like gender we applied Spearman's rank correlation coefficient. Pearson's correlation coefficient was used for variables with continuous scales. P‐values <.05 were regarded as statistically significant.
3. RESULTS
In 97 of 477 (20.3%) patients the survey letters could not be delivered as their addresses could not be located. Of the remaining 380 patients (79.7%), 130 did respond with completely filled‐out questionnaires and signed consent forms. Hence, a response rate of 34.2% (130 out of 380) was observed for potentially contactable patients.
Age of responders was significantly higher than nonresponders' age with an average of x̅ = 55.36 (SD = 14.24) vs x̅ = 47.70 (SD = 16.35, P < .001) and responders had a shorter follow‐up time (x̅ = 5.68 years, SD = 3.77; x̅ = 6.72 years, SD = 3.86, P = .009, for responders and nonresponders, respectively). No significant differences were detected regarding gender, affected gland and diagnosis.
An increasing trend in the number of sialendoscopies over the years can be observed. Sialendoscopic procedures raised from 24 (3.9%) in 2004, to 36 (5.9%) in 2009 and to 62 (10.1%) in 2016.
Of 130 patients, 78 (60%) were found to be female and 52 (40%) male. Mean age at the time of surgery was x̅ = 55.36 years (SD = 14.24). Average time between surgery and survey was x̅ = 5.68 years (SD = 3.77).
On those 130 patients 191 sialendoscopies were performed. Parotid gland (PG) was affected 104 times (54.5%) according to 51 patients and submandibular gland (SG) 97 times (45.5%) according to 79 patients. Postoperative diagnoses can be summarized into seven groups, whereby in most cases a combination of multiple pathologies was present and the individual patient might be operated on several times. Therefor the sum of sialendoscopies is higher than the absolute number of patients (Table 1). Individual patient characteristics is delineated in Table S1.
TABLE 1.
Diagnostic groups of the 191 sialendoscopies
| Diagnosis | Absolute frequency (%) | PG | SG |
|---|---|---|---|
| Acute sialadenitis | 3 (1.6) | 2 | 1 |
| Recurrent/chronical sialadenitis | 131 (68.6) | 69 | 62 |
| Sialolithiasis | 103 (53.9) | 33 | 70 |
| Duct stenosis | 78 (40.8) | 67 | 11 |
| Papilla stenosis | 20 (10.5) | 6 | 14 |
| Anatomical anomalies | 3 (1.6) | 3 | 0 |
| Other | 5 (2.6) | 3 | 2 |
Abbreviations: PG, parotid gland; SG, submandibular gland.
3.1. OHIP‐G14
Analyzing OHIP‐G14‐questionnaires an average score of x̅ = 6.65 (SD = 9.99) was detected. Of the subgroup without dentures (n = 91, 47.6%) the average score was x̅ = 6.33 (SD = 10.68), with removable dentures (n = 31, 16.2%), x̅ = 7.74 (SD = 8.47), and without own teeth but complete dentures (n = 8, 4.2%) x̅ = 6.13 (SD = 7.59). Since the published normal population based scores from John et al were displayed as percentile ranks of the frequency distribution, 3 a table was provided for easier visual comparison (see Table 2). The investigated group was older than the reference cohort (x̅ = 55.36 years, SD = 14.24, x̅ = 43.3 years, SD = 16.2, P < .001) and included more females (60% females, 52% females, P = .004, investigated cohort and reference cohort, respectively).
TABLE 2.
OHIP‐G14: population based norms vs post sialendoscopy cohort
| Percentile rank | Population‐based norms OHIP‐G14: without dentures | Post sialendoscopy OHIP‐G14: without dentures n = 91 | Population‐based norms OHIP‐G14: removable dentures | Post sialendoscopy OHIP‐G14: removable dentures n = 31 | Population‐based norms OHIP‐G14: complete dentures | Post sialendoscopy OHIP‐G14: complete dentures n = 8 |
|---|---|---|---|---|---|---|
| 10 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20 | 0 | 0 | 0 | 0 | 0 | 0 |
| 30 | 0 | 0 | 1 | 2 | 1 | 0 |
| 40 | 0 | 0 | 2 | 3.8 | 4 | 0.6 |
| 50 | 0 | 1 | 4 | 5 | 6 | 3.5 |
| 60 | 1 | 3 | 6 | 8.2 | 9 | 7.2 |
| 70 | 3 | 8 | 8 | 10.4 | 14 | 9.9 |
| 80 | 6 | 11.6 | 12 | 13.2 | 21 | 13.8 |
| 90 | 11 | 17.6 | 17 | 21.8 | 25 | n.e. |
| P‐value | <.0001 | <.00001 | .043 | |||
Abbreviation: OHIP‐G14, Oral Health Impact Profile.
In comparison of the percentiles, a significant effect of the subgroups on oral health‐related quality of life was revealed: Patients without (P < .0001) or respectively with (P < .00001) removable dentures showed significant worse OHRQoL compared to the healthy population. In our sample the eight patients with complete dentures achieved a better oral health‐related quality of life than healthy population (P = .043). However, no significant effect on the OHIP‐G14 scores was found for neither time of follow‐up, gender, age or affected gland nor for instillation of cortisone, diagnoses, location of any follow‐up treatments and salivary gland removal during the course of disease. Out of 130 patients, 31 (23.8%) underwent surgery multiple times. From those, patients with sialolithiasis (P = .018) and papilla stenosis (P = .024) underwent fewer multiple endoscopies compared to the other diagnoses. On the other hand, patients with multiple surgeries showed no significant worse oral health‐related quality of life or satisfaction.
3.2. Second questionnaire
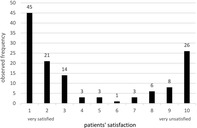
The second questionnaire was designed to investigate the success of sialendoscopy based on the follow‐up therapy and the subjective satisfaction of patients. On average, patients' satisfaction was x̅ = 4.33 (SD = 3.69) on a visual analogue scale from 1 (=very satisfied) to 10 (=very unsatisfied). In Figure 3, it is clearly noticeable that patients were biased toward extreme values and avoided moderate scores.
FIGURE 3.

Observed frequencies of patients' satisfaction regarding sialendoscopy
A significant negative, but weak, correlation between satisfaction and time of follow‐up (r = −0.19 P = .031) as well as satisfaction and age (r = −0.20, P = .025) was found. Consequently a longer follow‐up period and a higher patients' age were related to high satisfaction. No significant influence on satisfaction was detected with regard to gender, affected gland, instillation of cortisone, location of potential follow‐up treatments, anesthesia or diagnoses. Further, patients with extended incision of salivary duct (P = .014) and a salivary gland removal during follow‐up (P = .019) tended to be more unsatisfied.
Considering only the presence of sialolithiasis vs no sialolithiasis there is no significant influence with regard to gender, age, oral health‐related quality of life, satisfaction, removal of salivary gland or frequency of any further treatment in the course of disease or willingness to repeat sialendoscopy if necessary.
Overall, preservation of the affected salivary gland was achieved in 113 patients (86.9%). Removal of salivary gland in the course of the disease was significantly more frequently performed for longer follow‐up time (P = .002) for male patients (11 out of 17 = 64.7%) in comparison to females (6 out of 17 = 35.3%, P = .034), after initial sialendoscopy under general vs local anesthesia (P = .006), after marsupialization (P = .005) and in patients followed up externally (P = .006). No significant effect was yielded for the kind of affected gland (PG or SG), the diagnosis or age.
In 100 patients (76.9%) no further treatment was necessary, in 16.9% one‐single and in 6.2% multiple conservative or invasive treatments were necessary. No dependence on gender, age, different diagnoses or procedures or affected gland was observed. Patients with no any further treatment in the course of the disease showed a higher mean oral health‐related quality of life on the OHIP‐G14 (x̅ = 5.83, SD = 8.53) and satisfaction (x̅ = 4.10, SD = 3.66) than the average of all patients. Patients with a single additional treatment were below the total average OHIP‐score with an average score of x̅ = 6.00 (SD = 11.65). A significant higher OHIP‐score of x̅ = 18.75 (SD = 15.00) was obtained for patients with multiple further treatments (P = .005). Thus, those patients were associated with a worse oral health‐related quality of life. Further, lower patients' satisfaction was related to increased number of any (conservative or invasive) treatment.
A majority of 115 (88.5%) patients would repeat sialendoscopy for related symptoms. This correlated with a better oral health‐related quality of life (r = −0.25, P = .003) and satisfaction (r = −0.26, P = .003). No significant effect was found for gender, age, kind of gland, location of follow‐up treatments, diagnosis or surgery procedures.
4. DISCUSSION
Sialendoscopy is a low‐risk 4 minimally invasive method gaining more and more importance during the last years. This becomes apparent by the rising number of performed sialendoscopies, also be observed in this study. Kroll et al investigated this trend in German ENT clinics. 5 It was shown that the number of sialendoscopies tripled from 2009 to 2016 while at the same time the number of clinics performing it more than doubled.
Despite the response rate of 34.2%, it was possible to recruit a relatively large cohort of 130 patients, with a long average follow‐up time. Yet, some analysis within subgroups (especially concerning the instillation of cortisone and anesthetic procedure) suffered from small sample sizes, low power and, hence, poor statistical validity.
The existing literature with regard to sialendoscopic treatment is inconsistent and hardly comparable because of diverse methods and research questions. Fundamental similarities existed in demographic characteristics of the examined cohort compared to the literature such as an even gender distribution and an average patient age of x̅ = 50 years at the time of surgery.
Some studies showed that symptoms after sialendoscopy were improved in short‐, medium‐ and long‐term 6 follow‐up. 7 , 8 , 9 , 10 , 11 , 12 , 13 In most cases custom designed questionnaires relying on symptom improvement were utilized. Aubin‐Pouliot et al 12 used the “chronic obstructive sialadenitis symptoms questionnaire” (COSS) and observed symptom improvement at 3 and 12 months postoperatively. They were able to show that success was stable after a year. There is no validated German version of COSS. Therefor and because it investigates the symptom score and not specifically quality of life it is not used in the present study.
Very few studies referred to the effect of sialendoscopy on quality of life and rarely with measurement tools specific for salivary gland disorders. The reason for this is a lack of validated and practicable questionnaires on specific quality of life. No significant difference in overall health quality of life after sialendoscopy was found by Aubin‐Pouliot 12 using SF8. However, Kroll et al, 7 using SF36, found significant reduced vitality and psychological well‐being in patients undergoing sialendoscopy compared to healthy controls. Focusing less on overall health but more on oral health‐related quality of life, Gillespie et al 13 used a modified version of the OHIP‐14 which was tailored to capture salivary gland disorders. Due to the modification, the questionnaire does not remain validated and therefore cannot be compared with the normal population‐based scores of the OHIP. Until the present study, there was no study on oral health‐related quality of life after sialendoscopy using a validated measurement tool.
In this study with a long average follow‐up of x̅ = 5.68 years after sialendoscopy, the OHIP‐G14 score was used observing a mean score of x̅ = 6.65 and a median of MD = 2, similar to the results of Gillespie et al. 13 Thus, a significant worse oral health‐related quality of life was ascertained as compared to the healthy population. Demographic characteristics and diagnoses could be excluded to be influencing factors within the cohort of 130 patients who underwent sialendoscopy. Further, the present study can neither confirm a positive effect of sialolithiasis on satisfaction or quality of life, as opposed to Aubin‐Pouliot et al, 12 Gillespie et al 13 or Jokela et al, 14 nor a negative effect of inflammatory diseases on quality of life as opposed to Gillespie et al 13 As Gillespie et al demonstrated, 13 no difference in quality of life could be shown in patients with follow‐up salivary gland removals and patients with salivary gland preservation. However, this data demonstrates association of any frequent additional conservative or invasive therapies with worse quality of life.
The subjective satisfaction of patients with the success has been inquired by several studies. 4 , 6 , 7 Kopéc et al 4 found no effect of age or gender, while, according to Kroll et al, 7 younger patients were more dissatisfied. This was affirmed in the present study. Patients with a longer follow‐up time tend to be more satisfied with the success of the treatment. This is supported by the long‐term success and the high number of patients receiving no further necessary treatments.
On the other hand, patients with extended incision of salivary duct or salivary gland removal during follow‐up were significantly more dissatisfied. Yet, in 86.9% and thus the majority of patients, a long‐term preservation of the salivary gland was accomplished. Similar high success rates of sialendoscopy as salivary gland‐preserving surgery has been confirmed by other studies. 5 , 7 , 13
The higher frequency of removal of salivary gland in the course of disease in patients with longer follow‐up time could be caused by a learning effect of the team or just by longer follow‐up time. The higher satisfaction in these patients speaks against a learning effect.
The outlined tendency in Figure 3 toward extreme answers regarding the satisfaction could be explained by the positioning of the question at the end of the questionnaire, where patients possibly conveyed an unconscious overall summary of all previous questions.
The majority of patients (88.5%) would undergo sialendoscopy again if needed. Gillespie et al 13 reported a similar result of 90% of the patients recommending a therapy by sialendoscopy.
One limitation of the present study is the retrospective design and not to check medical findings compared to patients´ responses. A worse oral health‐related quality of life compared to the healthy population could be established but no claims about the preoperative condition and, thus, the influence on quality of life by sialendoscopy can be made. Therefor further prospective studies are necessary.
5. CONCLUSION
Sialendoscopy is a procedure that objectively and by subjective patients' perception achieves high success rates as measured by satisfaction, rate of gland‐preservation, and willingness to repeat sialendoscopy if necessary. However, OHRQoL of healthy population could not be achieved. The influence of the operational procedure by itself is uncertain because preoperative data for quality of life had not been collected. Except the necessity of multiple additional follow‐up treatments, no predisposing factors (pathology, patient characteristics, affected gland, kind of surgery procedures) concerning OHRQoL were found. Consequently all patients have the same probability of a good outcome independently of these criteria.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Supporting information
Table S1 1—acute sialadenitis. 2—recurrent/chronical sialadenitis. 3—sialolithiasis. 4—duct stenosis. 5—papilla stenosis. 6—anatomical anomalies. 7—other.
ACKNOWLEDGMENT
Open access funding enabled and organized by Projekt DEAL.
Weigelt F, Borzikowsky C, Hoffmann M, Laudien M. Success of minimally invasive salivary gland surgery—Quality of life, prognostic factors. Laryngoscope Investigative Otolaryngology. 2020;5:832–838. 10.1002/lio2.450
Correction added on 1 October 2020 after first online publication: Projekt Deal funding statement has been added.
REFERENCES
- 1. Slade GD, Spencer AJ. Development and evaluation of the Oral health impact profile. Community Dent Health. 1994;11(1):3‐11. 10.1111/j.1708-8240.2002.tb00161.x. [DOI] [PubMed] [Google Scholar]
- 2. John MT, Miglioretti DL, LeResche L, Koepsell TD, Hujoel P, Micheelis W. German short forms of the oral health impact profile. Community Dent Oral Epidemiol. 2006;34:277‐288. 10.1111/j.1600-0528.2006.00279.x. [DOI] [PubMed] [Google Scholar]
- 3. John MT, Micheelis W, Biffar R. Normwerte mundgesundheitsbezogener Lebensqualität für Kurzversionen des Oral Health Impact Profile. Schweiz Monatsschr Zahnmed. 2004;114(8):784‐791. [PubMed] [Google Scholar]
- 4. Kopeć T, Wierzbicka M, Piskadło K, Bednarek M, Szyfter W. Sialendoscopy—a diagnostic and therapeutic approach subjectively rated by patients. Videosurg Other Miniinvasive Tech. 2014;4:505‐510. 10.5114/wiitm.2014.44176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kroll T, Schwarz D, Sharma SJ, Wittekindt C, Wolf G. Stellenwert der Sialendoskopie an deutschen HNO‐Kliniken im Jahr 2016 Value of sialendoscopy in German ENT‐hospitals in 2016 Einleitung Material und Methoden Ergebnisse Diskussion. 2016:91‐95.
- 6. Koch M, Künzel J, Iro H, Psychogios G, Zenk J. Long‐term results and subjective outcome after gland‐preserving treatment in parotid duct stenosis. Laryngoscope. 2014;124(8):1813‐1818. 10.1002/lary.24534. [DOI] [PubMed] [Google Scholar]
- 7. Kroll T, Finkensieper M, Sharma SJ, Guntinas‐Lichius O, Wittekindt C. Short‐term outcome and patient satisfaction after sialendoscopy. Eur Arch Oto‐Rhino‐Laryngol. 2013;270(11):2939‐2945. 10.1007/s00405-013-2418-z. [DOI] [PubMed] [Google Scholar]
- 8. Choi JS, Choi YG, Kim YM, Lim JY. Clinical outcomes and prognostic factors of sialendoscopy in salivary duct stenosis. Laryngoscope. 2018;128(4):878‐884. 10.1002/lary.26897. [DOI] [PubMed] [Google Scholar]
- 9. Plonowska KA, Gurman ZR, Humphrey A, Chang JL, Ryan WR. One‐year outcomes of sialendoscopic‐assisted salivary duct surgery for sialadenitis without sialolithiasis. Laryngoscope. 2019;129(4):890‐896. 10.1002/lary.27433. [DOI] [PubMed] [Google Scholar]
- 10. Ryan WR, Plonowska KA, Gurman ZR, Aubin‐Pouliot A, Chang JL. One‐year symptom outcomes after sialolithiasis treatment with sialendoscopy‐assisted salivary duct surgery. Laryngoscope. 2019;129(2):396‐402. 10.1002/lary.27398. [DOI] [PubMed] [Google Scholar]
- 11. Delagnes EA, Zheng M, Aubin‐Pouliot A, Chang JL, Ryan WR. Salivary duct stenosis: short‐term symptom outcomes after sialendoscopy‐assisted salivary duct surgery. Laryngoscope. 2017;127(12):2770‐2776. 10.1002/lary.26665. [DOI] [PubMed] [Google Scholar]
- 12. Aubin‐Pouliot A, Delagnes EA, Chang JL, Ryan WR. Sialendoscopy‐assisted surgery and the chronic obstructive sialadenitis symptoms questionnaire: a prospective study. Laryngoscope. 2016;126(6):1343‐1348. 10.1002/lary.25759. [DOI] [PubMed] [Google Scholar]
- 13. Boyd Gillespie M, O'Connell BP, Rawl JW, McLaughlin CW, Carroll WW, Nguyen SA. Clinical and quality‐of‐life outcomes following gland‐preserving surgery for chronic sialadenitis. Laryngoscope. 2015;125(6):1340‐1344. 10.1002/lary.25062. [DOI] [PubMed] [Google Scholar]
- 14. Jokela J, Saarinen R, Mäkitie A, Sintonen H, Roine R. Costs of sialendoscopy and impact on health‐related quality of life. Eur Arch Oto‐Rhino‐Laryngol. 2019;276(1):233‐241. 10.1007/s00405-018-5196-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 1—acute sialadenitis. 2—recurrent/chronical sialadenitis. 3—sialolithiasis. 4—duct stenosis. 5—papilla stenosis. 6—anatomical anomalies. 7—other.


