Abstract
Objective
To evaluate the association of weather, seasons, months and holidays on the frequency and pattern of pediatric facial fractures.
Methods
Retrospective review of pediatric patients treated for facial fractures at two Level I trauma centers in a midsize Midwestern US city over a 5‐year period. Patients were included only if presentation was within 3 hours of inciting trauma, transfers from other facilities were excluded. Demographic characteristics, fracture patterns, operative interventions, weather data, and local public school schedules were acquired and associations were analyzed with unpaired t tests, χ2, multivariate and binomial regression model analyses.
Results
Two hundred and sixty patients were included. The average age (SD) was 11.8 (5.0) years, with 173 males and 87 females. The highest distribution of presentations occurred in the summer season (35.0%), on weekends and holidays (58.1%), and when the weather was described as clear (48.5%). The most common mechanisms of injury were motor vehicle collisions (25.8%), followed by sports—(21.5%) and assault—(16.5%) related injuries. Mechanisms were significantly associated with certain fracture patterns. Older age was associated with fewer orbital fractures (P < .01). Seventy‐five patients (28.8%) required operative intervention. Age was found to impact the likelihood of operative intervention (Exp(β) = 1.081, P = .03) while weather, temperature, and mechanism did not.
Conclusion
Pediatric facial fractures are linked to warmer weather with clear skies and warmer season. Age predicts some fracture patterns and need for operative intervention. These results can be used to inform public health interventions, policymaking, and trauma staffing.
Level of Evidence: Level 2b (retrospective cohort).
Keywords: facial fractures, holiday, pediatric facial trauma, pediatric fractures, weather
A retrospective review of 260 pediatric facial trauma patients found an association between the incidence of facial fractures and warmer weather, clear skies, weekends or holidays, and mechanism of injury. Older age is associated with operative intervention. These results can be used to guide public health interventions, policymaking, and facial trauma resource allocation.
1. INTRODUCTION
Trauma is the leading cause of pediatric morbidity and mortality. Pediatric maxillofacial fractures comprise up to 14.7% of all facial fractures in the United States 1 and can generate lasting and occasionally irreversible impairment in function and cosmesis. 2 Furthermore, pediatric trauma patients with facial fractures are more likely to have substantial injury, increased hospital length of stay, ICU admissions, need for mechanical ventilation, and health care cost burden. 3
Pediatric maxillofacial trauma most commonly affects boys who are involved in motor vehicle accidents, which accounts for up to 80.2% of pediatric facial fractures. 4 Various associations have been found between trauma admissions and factors such as weather, temperature, seasons, time of day, holidays, and weekends. A study of trauma admissions at three level I trauma centers in Minneapolis found weekends, summer, lack of rain, and snowfall to be predictive of daily trauma admissions. 5 These associations have not been firmly established with respect to maxillofacial trauma in either the adult or pediatric literature. Despite the burden of injury and health care burden associated with pediatric facial trauma, factors associated with the incidence of injury remain poorly studied. The goal of this retrospective analysis is to help identify and characterize associations between pediatric maxillofacial trauma at our institution and factors such as weather, seasons, time of day, holidays, and temperature. We hypothesize that pediatric maxillofacial trauma has the greatest incidence in warmer weather during daylight hours because this is when children are most likely to be active. The results may be used to guide public health and safety measures, policymaking, emphasize the importance of adherence to motor vehicle traffic laws and regulations, inform parents and caretakers, and optimize resource allocation for otolaryngologists, facial plastic and reconstructive surgeons, and oral‐maxillofacial surgeons at centers that manage pediatric trauma.
1.1. Geography and climate
Indianapolis, Indiana is a midsize Midwestern city with a population of 867 125. 6 Indianapolis rests at a latitude of 39.77° and an elevation of 732 ft above sea level, with an average low and high temperature range of 20 and 36°F respectively in the Winter, and 66 and 85°F respectively in the Summer, with on average 125 days per year with precipitation. 7 Regarding trauma care, the trauma centers included during the study period represented two of the three level I trauma centers serving the entire state of Indiana, and the only pediatric level I trauma center in the state. 8
2. MATERIALS AND METHODS
2.1. Patient aggregation
Formal institutional review board exemption was obtained for this study. A retrospective chart review was performed of pediatric patients seen at two level 1 trauma centers in Indianapolis, Indiana over a 4‐year period from 2012 to 2016. Patient records for all emergency room visits with documented facial and skull fractures (ICD‐9 codes 800.xx, 801.xx, 802.xx, 803.xx, 804.xx; ICD‐10 code S02.xx) were obtained, yielding 2845 total patients. Patients were excluded based on the following criteria: (a) 18 years of age or greater at the time of presentation (N = 2438); (b) first treated at or transferred from an outside hospital (N = 91); (c) delayed presentation to the emergency room >3 hours (N = 19); (d) no record nor evidence of maxillofacial fractures (N = 35); (e) and finally, duplicate records were removed (N = 2). Delayed presentations and transfers were excluded to allow direct correlation between injury and weather patterns in a timely (<3 hours) manner. A total of 260 subjects met the inclusion criteria for the 5‐year interval.
2.2. Data aggregation
Data extracted included basic demographics, mechanism of injury, fracture pattern, interventions, and temporal/calendar data such as the time of the encounter, day of the week, month, and season. All fracture radiology reports and images were reviewed and categorized into basic categories. Local public‐school calendars were used to mark the day as a “school day” or a “school‐free day.” Holiday dates were gathered, and encounters were marked for analysis if they coincided with New Year's, Martin Luther King Jr. Day, Presidents'Day, Memorial Day, Fourth of July, Labor Day, Halloween, Thanksgiving, and Christmas.
2.3. Weather and temperature data
Weather data was gathered from World Weather Online (http://us.worldweatheronline.com) using an Application Programming Interface (API). Weather data was acquired within a 3‐hour window leading up to the time of patient presentation, using the corresponding hospital zip code for location. The 3‐hour window was used because the actual time of injury was not always documented. Data extracted included temperature, sunrise, sunset, daylight (light vs dark) and weather descriptions. Weather descriptions were subsequently categorized into like conditions (Table 1) for statistical analyses. Multiple descriptive conditions were combined for analysis purposes: (a) clear and sunny; (b) cloudy, partly cloudy, and overcast; (c) light precipitous conditions; (d) fog and mist; (e) moderate, heavy, and torrential rain; and finally (f) snow and freezing precipitous conditions. Temperature was categorized into four groups: 32°F or less, 33 to 50°F, 51 to 70°F and above 70°F (Table 1).
TABLE 1.
Distribution of weather and temperature
| Weather description | Weather group | Trauma frequency, n | Overall frequency, f | P‐value |
|---|---|---|---|---|
| Clear/sunny | 1 | 126 | 6138 | .11 |
| Cloudy/overcast | 2 | 83 | 5397 | |
| Light drizzle/rain | 3 | 29 | 1290 | |
| Fog/mist | 4 | 12 | 965 | |
| Moderate/heavy/torrential rain | 5 | 4 | 359 | |
| Freezing/snowing/blizzard | 6 | 6 | 467 | |
| Total | All groups | 260 | 14 616 |
| Temperature (°F) | Weather group | Trauma frequency, n | Overall frequency, f | P‐value |
|---|---|---|---|---|
| ≤32 | 1 | 21 | 2776 | <.01 |
| 33 to 50 | 2 | 61 | 3678 | |
| 51 to 70 | 3 | 99 | 5303 | |
| ≥71 | 4 | 79 | 2859 | |
| Total | All groups | 260 | 14 616 |
Abbreviations: n, number of patients; f, frequency of weather/temperature at 3‐hour periods from 2012 to 2016.
The bolded p‐value of “<.01” signifies statistical significance.
2.4. Statistical analysis
The analytic dataset was compiled using Excel 2013 software (Microsoft Corp, Redmond, Washington). All statistical analyses were performed using IBM SPSS Statistics (version 24, IBM Corp., Armonk, New York). Unpaired t test, χ2, multivariate and binomial regression analysis was performed; we provide the β coefficient and Exp(β) value as an exponentiation of the β coefficient, which is an odds ratio. P‐values <.05 were considered statistically significant.
3. RESULTS
A total of 260 patients were included over the 5‐year period. The average age (SD) at the time of presentation for pediatric facial fractures was 11.8 (5.0) years with a 2:1 male to female ratio (Table 2). Most subjects were Caucasian (N = 190, 73.1%) and provided Medicaid or government‐based payment (N = 209, 80.4%). One hundred and seventy‐nine patients (68.8%) presented with facial fractures isolated to the nasal bone, midface, mandible, orbit, or frontal sinus. The most common facial fractures were nasal bone (N = 108, 38.4%), followed by the orbit (N = 102, 39.2%), midface (N = 91, 35.0%), and mandible (N = 50, 19.2%). The most common mechanisms of injury were motor vehicle collisions (N = 67, 25.8%), sport (N = 56, 21.5%), and assault or battery (N = 43, 16.5%). In sport‐related pediatric facial trauma (N = 57, 21.9%), the most common sports involved were baseball (N = 17, 6.5%), bicycling (N = 13, 5.0%), basketball (N = 7, 2.7%), and football (N = 6, 2.3%).
TABLE 2.
Distribution of patients
| Total | Sch+ | Sch− | P‐value (Sch+ vs −) | P‐value (category) | |
|---|---|---|---|---|---|
| n = 260 | n = 117 | n = 143 | |||
| Age, y (SD) | 11.8 (5.0) | 11.9 (5.2) | 11.6 (4.9) | 0.64 | |
| Time, hh:mm (SD, h) | 16:22 (5.6) | 16:57 (4.8) | 15:53 (6.2) | 0.13 | |
| Gender, n | .06 | ||||
| Male | 173 | 76 | 97 | 0.21 | |
| Female | 87 | 41 | 46 | 0.29 | |
| Race, n | .61 | ||||
| Black | 64 | 31 | 33 | 0.33 | |
| White | 190 | 85 | 105 | 0.50 | |
| Other | 6 | 1 | 5 | 0.16 | |
| Season, n | |||||
| Winter | 32 | 15 | 17 | ||
| Spring | 72 | 43 | 29 | ||
| Summer | 91 | 28 | 63 | ||
| Autumn | 65 | 31 | 34 | ||
| Weather group, n | |||||
| Clear/sunny | 126 | 52 | 74 | ||
| Cloudy/overcast | 83 | 42 | 41 | ||
| Light/patchy rain | 29 | 17 | 12 | ||
| Fog/mist | 12 | 3 | 9 | ||
| Moderate/heavy rain | 4 | 1 | 3 | ||
| Freezing/snowing | 6 | 2 | 4 | ||
| Temperature group, n | |||||
| ≤32°F | 21 | 13 | 8 | ||
| 33 to 50°F | 61 | 27 | 34 | ||
| 51 to 70°F | 99 | 44 | 55 | ||
| ≥71°F | 79 | 33 | 46 |
Note: P‐values are obtained comparing traumas for Sch + vs Sch− in the second to rightmost column, and comparing between categories (ie, male vs female) in the rightmost column. P‐values are excluded for several categories due to the significant confounders between weather category, temperature, season, and school days.
Abbreviations: n, number of patients; Sch+, school day; Sch−, nonschool day; y, years; hh:mm, hour:minute of day.
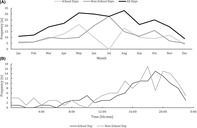
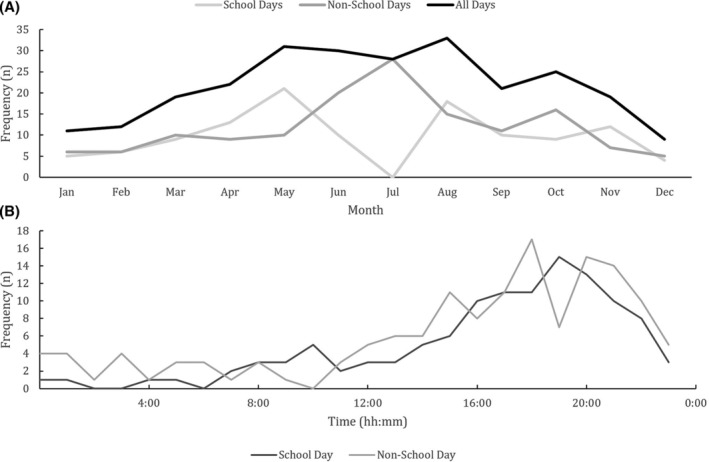
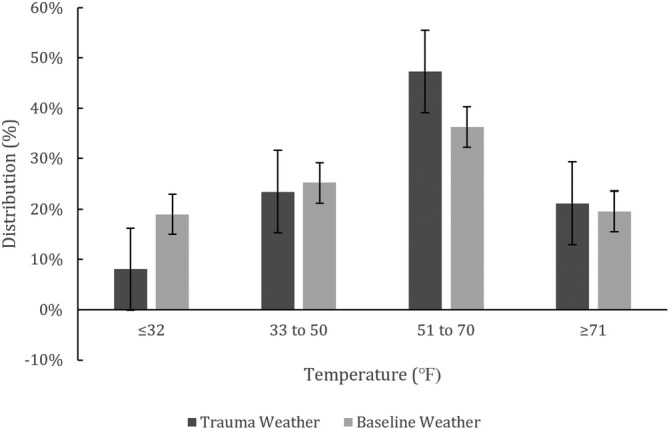
Facial fractures occurred most often in the summer, and least often in the winter (35% vs 12.3%, χ2 = 22.5, P < .01, Table 2, Figure 1). Facial fractures occurred with a greater frequency (0.16 vs 0.13 traumas per day) on nonschool days vs school days; however, this was not found to be significantly different (χ2 = 2.0, P = .16). The most common time of day for fractures to occur was the evening, with most fractures occurring between 4:00 pm and 11:00 pm (N = 177, 68.1%, Figure 1). There was no significant difference in average time of day for fractures taking place on nonschool days vs school days (16:57 vs 15:54, P = .13, Table 2). Facial fractures resulting from motor vehicle collisions were more common in Caucasian or White patients than Black or African American patients (30.0% vs 12.1%) while battery injuries were more in the Black or African American cohort (29.7% vs 10.9%, χ2 = 18.6, P < .01, Figure 2 ).
FIGURE 1.
Temporal distribution of pediatric maxillofacial trauma at a midsize US metropolitan city over a 5‐year period by month (top) and hour of day (bottom); N = 260. hh:mm, hour and minute of the day; n, number of patients
FIGURE 2.
Mechanism of Injury and Racial Distribution. White or Caucasian patients had significantly greater proportion of pediatric maxillofacial trauma by motor vehicle collision than Black or African American patients, who were more likely to present following battery. AA, African American; ATV, all‐terrain vehicle; GSW, gunshot wound; MVC, motor vehicle collision; n, number of patients; Ped, pedestrian. *P < .01
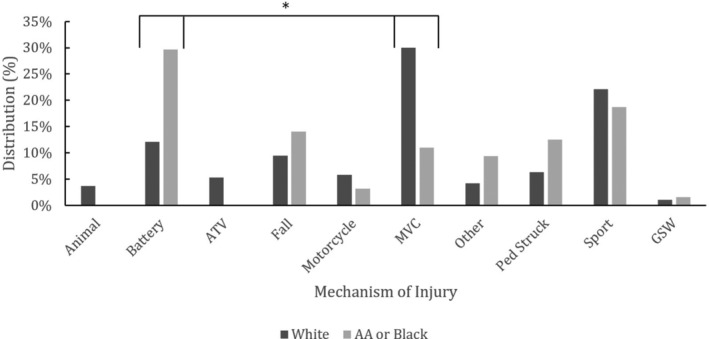
Facial fractures most often occurred with clear skies (N = 126, 48.5%). Overall, there was no significant difference in frequency of facial fractures related to weather descriptors over this 5‐year period (χ2 = 8.9, P = .11, Table 1). Fractures were shown to occur more frequently in temperature range of 51 to 70°F (χ2 = 25.3, P < .01, Table 1). Facial fractures generally occurred during daylight hours (N = 146, 56.2%), and occurred more frequently during the daylight in warmer temperatures while less frequently during colder temperatures (χ2 = 44.0, P < .01, Figure 3). All mechanisms of injury were more frequent during warmer temperatures.
FIGURE 3.
Temperature frequency and distribution. Comparison of relative distribution of weather temperature conditions in the preceding 3 hours of pediatric maxillofacial trauma occurrence (trauma weather) vs relative distribution of all weather conditions (baseline weather) over a 5‐year period in a Midwestern US metropolitan city. Trauma occurred with greater relative frequency in the 51‐ to 70°F range. Error bars shown represent SE
Multivariate regression analysis was performed to evaluate predictors of fracture patterns. Freezing temperatures (≤32°F) significantly predicted risk of nasal fractures (P = .03). No other fracture patterns were identified to be influenced by weather nor temperature‐related patterns. Less predicted risk of orbital fractures was found with increased age (F = 14.28, P < .01). The mechanism of injury also significantly predicted injury patterns including orbit, midface, and frontal sinus fractures. Children struck by vehicles were significantly predicted to acquire orbital (14 of 20 patients, P = .02) and midface (10 of 20 patients, P < .01) fractures. Moreover, midface fractures (P < .01) were significantly predicted in mechanisms involving animals (5 of 7 patients), all‐terrain vehicles (7 of 10 patients), and motor vehicle collisions (28 of 67 patients). Finally, frontal sinus fractures were predicted by animal related trauma with fractures in 3 of the 6 horse caused injuries (P = .04).
The rate of operative intervention was 28.8% (75 patients). Binary Logistic Regression analysis revealed increased age was predictive of intervention (Exp(β) = 1.08, P = .03) as well as mandible, orbit, and midface fractures. Mandible fractures greatly increased risk of intervention vs orbit and midface fractures which were less likely to need intervention (Table 3). Other factors including mechanism of injury, weather, temperature as well as frontal sinus and midface fracture did not increase risk of intervention.
TABLE 3.
Binary logistic regression for predicting operative intervention
| Factor | β | SE | Wald | P‐value | Exp(β) |
|---|---|---|---|---|---|
| Age (y) | 0.079 | 0.036 | 4.783 | .03 | 1.083 |
| Orbit Fx | 1.276 | 0.481 | 7.044 | <.01 | 3.581 |
| Nasal Fx | 1.283 | 0.442 | 8.428 | <.01 | 3.608 |
| Midface Fx | 0.298 | 0.384 | 0.606 | .44 | 1.348 |
| Mandible Fx | 3.556 | 0.557 | 40.704 | <.01 | 35.036 |
| Frontal sinus Fx | −0.051 | 0.565 | 0.008 | .93 | 0.950 |
| Mechanism of injury | 0.016 | 0.062 | 0.063 | .80 | 1.016 |
| Temperature | −0.075 | 0.177 | 0.179 | .67 | 0.928 |
| Weather | 0.029 | 0.143 | 0.043 | .84 | 1.030 |
| Constant | −3.791 | 0.962 | 15.517 | .00 | 0.023 |
Abbreviations: Exp(β), exponentiation of the β coefficient; Fx, fracture; Wald, Wald χ2; β, intercept.
The bolded values signify a p‐value of less than 0.05, which signifies statistical significance.
4. DISCUSSION
Pediatric facial trauma incurs significant morbidity and mortality in the United States. Our study confirms that the most common mechanism of pediatric facial fractures is motor vehicle collisions (MVCs), with sports and violence among the next most common etiologies. 2 , 4 , 9 , 10 , 11 , 12 , 13 , 14 This was not the case in African American or Black patients for whom battery related facial fractures were the most common cause, followed by sports. There is a higher incidence of facial fractures in male vs female children, ranging from 1.1:1 to 8.5:1 male to female ratio, and this disparity has a positive correlation with age. 4 , 9 , 12 , 14
In our study, weather patterns were found to predict fracture occurrence. The distribution of weather over this 5‐year period did not significantly differ from the distribution of weather during fracture presentation. Temperature patterns seemed to play a much more significant role in facial fractures. The most common presentation was during warm temperatures and clear skies. Similarly, it has been observed in the emergency medicine and trauma surgery literature that days with higher temperatures correlate with increased trauma admissions, with lower rates of trauma on days with rainfall. 15 , 16 , 17 There was an increased distribution of fractures in the 51 to 70°F group vs other temperatures, although not significantly increased compared to the >70°F group. One postulate is that this range indicates a sudden change in temperature, either relative warming or cooling, that could be linked with an increase in outdoor activities. We also found that during the warmest temperatures (≥71°F), facial fractures occurred much more commonly during the daylight hours; this may be related to both outdoor activity at these temperatures and the increased number of daylight hours during the summer in Indiana, which peaks at 15 hours in the Summer compared to 9 hours in the Winter. 18 We found that the majority of facial trauma occurred during the summer months, which supports findings from previous studies. 13 In our study population, these months coincide with the local public‐school system's summer break and have the highest average temperatures.
Peak facial trauma hours were in the early evening, specifically 5 to 9 pm; conversely, the nadir occurred in the early morning hours around 4 am These results agree with previous trauma study findings, 15 and correspond with the level of activity in the typical American pediatric population. These hours also correspond with peak daylight hours and daily temperatures.
Increased leisure time during holidays and school‐free days appears to contribute to the incidence of pediatric trauma. In a massive epidemiologic study detailing over 5.7 million pediatric emergency room presentations between 1997 and 2006, incidence of injury related to holiday‐specific activities increased during US holidays and their surrounding dates. Specifically, the holidays included were Labor Day, Memorial Day, Independence Day, Halloween, Easter, Thanksgiving, Christmas, and New Year. Most of these injuries were related to sports and recreation as opposed to holiday activities. 19 Similarly, we found that a greater number of facial traumas occurred on school‐free days, although this was not statistically significant. The concept of how holidays and weekends affect trauma incidence depends on cultural norms specific to a locale. For instance, a study in Israel identifying Friday evenings and Saturdays as the weekend found that all emergency departments visits were decreased on weekends due to the tendency for religious observers to not use motorized transport to travel to the hospital. As a result, Thursdays and Sundays had a what was thought to be a compensatory increase in the number of emergency department visits. Similarly, they experienced the lowest volume on holidays. 20 In comparing this to the experience in the United States, it is clear that cultural factors play a significant role in how and when patients access health care.
We acknowledge that the factors of weather and temperature, season, and months all have some confounding effect with the school‐free days due to summer break. Our study is also limited in that it is a single‐institution experience over two Level 1 trauma centers in central Indiana. However, given that the institution represents the only pediatric level I trauma center in the state of Indiana, nearly all high acuity pediatric trauma is transported to this institution. Our weather data is exclusive to our 5‐year experience in our geographic area and may not be applicable to other trauma centers in the United States or other countries. Societal behavioral patterns likely also vary between metropolitan centers. There exists no natural control group for this study, as it is difficult to compare incidence of trauma to “potential” trauma subjects within the general pediatric population. Studies investigating trauma incidence, such as this one, are inherently retrospective in nature. Despite these limitations, no study to our knowledge has investigated the specific weather conditions in the 3 hours preceding the patient's hospital presentation. Our methodology of only including trauma incurred within the three‐hour window at the time of presentation and excluding transfers and delayed presentations can be applied to a variety of studies, and is particularly useful for time‐stamped weather analysis. Our findings emphasize the importance of physicians counseling their patients on the importance of activity‐directed facial protection, adherence to traffic safety regulations, and screening for violence in the household. Resource allocation can be optimized in anticipation of increased facial trauma volume in the summer and warmer months and on holidays.
5. CONCLUSION
Pediatric facial fractures are generally more common during warmer weather, clear skies, weekends, and days off from school. Age, mechanism of injury, and temperature are associated with fracture patterns and race. White/Caucasian patients were more likely to present after motor vehicle collisions, while Black or African American patients were more likely to present after battery. Age and fracture pattern were predictive of operative intervention in the pediatric population. Further studies may be valuable in assessing temporal, temperature, and weather patterns related to facial trauma.
CONFLICT OF INTEREST
The authors disclose no conflicts of interest and have no financial disclosures.
ACKNOWLEDGMENTS
We thank George Eckert, MAS (Department of Biostatistics, Indiana University‐Purdue University, Indianapolis, IN) for assistance with data analysis and statistical calculations as well as Ricardo Tuason, MHA, RN (Clinical Research Information Services, Indiana University Health, Indianapolis, IN) for assistance in the original patient search.
Rabbani CC, Kao R, Shin TJ, et al. The association of weather, temperature, and holidays on pediatric maxillofacial trauma. Laryngoscope Investigative Otolaryngology. 2020;5:846–852. 10.1002/lio2.457
Presented at TRIO annual meeting April 28‐29, 2017 in San Diego, CA, USA, the annual meeting for the Triological Society—manuscript submission #253.
BIBLIOGRAPHY
- 1. Vyas RM, Dickinson BP, Wasson KL, Roostaeian J, Bradley JP. Pediatric facial fractures: current national incidence, distribution, and health care resource use. J Craniofac Surg. 2008;19(2):339‐349. 10.1097/SCS.0b013e31814fb5e3. [DOI] [PubMed] [Google Scholar]
- 2. Mukherjee CG, Mukherjee U. Maxillofacial trauma in children. Int J Clin Pediatric Dent. 2012;5(3):231‐236. 10.5005/jp-journals-10005-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Imahara SD, Hopper RA, Wang J, Rivara FP, Klein MB. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207(5):710‐716. 10.1016/j.jamcollsurg.2008.06.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(2):126‐134. 10.1067/moe.2000.107974. [DOI] [PubMed] [Google Scholar]
- 5. Friede KA, Osborne MC, Erickson DJ, et al. Predicting trauma admissions the effect of weather, weekday, and other variables. Minn Med. 2009;92(11)47‐49. [PubMed] [Google Scholar]
- 6. U.S. Census Bureau QuickFacts: Indianapolis city (balance), Indiana. https://www.census.gov/quickfacts/indianapoliscitybalanceindiana. Accessed May 13, 2020.
- 7. Climate Indianapolis—Indiana and Weather averages Indianapolis. https://www.usclimatedata.com/climate/indianapolis/indiana/united-states/usin1068. Accessed May 13, 2020.
- 8. Trauma Hospitals in Indiana. https://www.ihaconnect.org/member/resources/Pages/Trauma-Hospitals-in-Indiana.aspx. Accessed May 13, 2020.
- 9. Alcalá‐Galiano A, Arribas‐García IJ, Martin‐Pérez MA, Romance A, Montalvo‐Moreno JJ, Juncos JMM. Pediatric facial fractures: children are not just small adults. Radiographics. 2008;28(2):441‐461. 10.1148/rg.282075060. [DOI] [PubMed] [Google Scholar]
- 10. Anderson PJ. Fractures of the facial skeleton in children. Injury. 1995;26(1):47‐50. 10.1016/0020-1383(95)90552-9. [DOI] [PubMed] [Google Scholar]
- 11. de Souza D, Santili C, de Freitas R, Akkari M, de Figueiredo M. Epidemiology of children's facial fractures in the emergency room of a tropical metropolis. Acta Ortop Bras. 2010;18(6):335‐338. [Google Scholar]
- 12. Costa Ferreira P, Amarante JM, Natividade Silva P, et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115(6):1500‐1508. 10.1097/01.PRS.0000160268.20294.FD. [DOI] [PubMed] [Google Scholar]
- 13. Pron GE. Pediatric facial fractures: evolving patterns of treatment. J Oral Maxillofac Surg. 1993;51(8):836‐844. 10.1016/S0278-2391(10)80098-9. [DOI] [PubMed] [Google Scholar]
- 14. Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2006;35(1):2‐13. 10.1016/j.ijom.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 15. Bhattacharyya T, Millham FH. Relationship between weather and seasonal factors and trauma admission volume at a level I trauma center. J Trauma. 2001;51(1):118‐122. 10.1097/00005373-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 16. Masterson E, Borton D, O'Brien T. Victims of our climate. Injury. 1993;24(4):247‐248. 10.1016/0020-1383(93)90179-A. [DOI] [PubMed] [Google Scholar]
- 17. Rising WR, O'Daniel JA, Roberts CS. Correlating weather and trauma admissions at a level I trauma center. J Trauma. 2006;60(5):1096‐1100. 10.1097/01.ta.0000197435.82141.27. [DOI] [PubMed] [Google Scholar]
- 18. Sunrise and sunset times in Indianapolis; December 2020. https://www.timeanddate.com/sun/usa/indianapolis?month=12. Accessed May 13, 2020.
- 19. D'Ippolito A, Collins CL, Comstock RD. Epidemiology of pediatric holiday‐related injuries presenting to US emergency departments. Pediatrics. 2010;125(5):931‐937. 10.1542/peds.2009-0307. [DOI] [PubMed] [Google Scholar]
- 20. Rotstein Z, Wilf‐Miron R, Lavi B, Shahar A, Gabbay U, Noy S. The dynamics of patient visits to a public hospital ED: a statistical model. Am J Emerg Med. 1997;15(6):596‐599. 10.1016/S0735-6757(97)90166-2. [DOI] [PubMed] [Google Scholar]


