Abstract
Acute zonal occult outer retinopathy (AZOOR) is an outer retinal disorder characterized by the acute loss of visual functions. Herein, we report a case of AZOOR presenting features mimicking optic neuritis. A 17-year-old healthy male reported fogginess in the right eye for 2 weeks. His best-corrected visual acuity was 20/20 in both eyes. Results of a color vision test and pupillary reaction were unremarkable. Funduscopic examination revealed a subtle hyperemic disc surrounded by hyperpigmentation in the right eye. Visual field examination confirmed an enlarged blind spot in the affected eye. Fundus autofluorescence imaging revealed zonal hyperautofluorescence around the optic disc. Fluorescein angiography showed optic disc staining and a window defect in the retinal pigment epithelium. Optical coherence tomography demonstrated loss of the ellipsoid line at the corresponding hyperautofluorescent region. All these characteristics indicated a diagnosis of AZOOR. However, the prolonged P100 wave observed through visual-evoked potential examination, hyperintensity T2 signal at the retrobulbar optic nerve through magnetic resonance imaging, and mild hyperemic optic disc along with optic disc staining through fluorescein angiography resemble the characteristics of optic neuritis. Because the clinical features of AZOOR are similar to those of optic neuritis, ophthalmologists should be able to differentiate between these two diseases to achieve a timely and correct diagnosis.
Keywords: Autofluorescence, acute zonal occult outer retinopathy, optic neuritis, optical coherence tomography
Introduction
Acute zonal occult outer retinopathy (AZOOR) was first reported by Gass in 1993.[1] He described 13 patients with AZOOR, who presented with acute-onset photopsia and scotoma. This condition was mostly seen in young, Caucasian women. However, its etiology remains undetermined till date. The death of retinal photoreceptors could lead to visual loss; however, central vision is usually preserved.[2] Although an association between AZOOR and central nervous system (CNS) demyelinating lesions has been suggested,[3] misdiagnosis of AZOOR as optic neuritis is not uncommon.[4] A few cases of AZOOR have been previously reported in Taiwan;[5,6] here, we present a case of AZOOR presenting clinical features mimicking optic neuritis.
Case Report
A 17-year-old healthy male was referred from a local eye clinic due to painless visual obscuration in the right eye for 2 weeks; white dot syndrome was suspected. His best-corrected visual acuity was 20/20 in both eyes with a refractive error of − 1.5 D in the right eye only. He denied preceding viral prodrome and any systemic disease. No concurrent neurological symptoms were noticed. No pupillary or color defects were observed. Slit-lamp examination indicated no inflammation in the aqueous or vitreous humor. Funduscopic examination showed mild hyperpigmentation around the optic disc and a mild hyperemic optic disc with indistinct margin in the right eye. Static perimetry examination revealed an enlarged blind spot in the affected eye [Figure 1]. Fundus autofluorescence (FAF) imaging revealed zonal hyperautofluorescence around the optic disc. Optic disc staining and a window defect in the retinal pigment epithelium (RPE) were found on fluorescein angiography. Optical coherence tomography (OCT) demonstrated loss of the ellipsoid line at the corresponding hyperautofluorescent region [Figure 2]. A pattern visual-evoked potential (VEP) test recorded a delayed response of P100 in the right eye (normal P100 latency in our laboratory is approximately 110 ms; [Figure 3]. Despite the detection of T2-hyperintense signals at the retrobulbar optic nerve through magnetic resonance imaging, no contrast enhancement was found [Figure 4]. He showed a mildly decreased Arden ratio in the right eye (1.84) compared with that in the left eye (1.97), but both values remained within the normal limit. Electroretinogram (ERG) results showed that the amplitude of the photopic and scotopic a-wave was slightly reduced in the right eye compared with that in the left eye [Figure 5].
Figure 1.
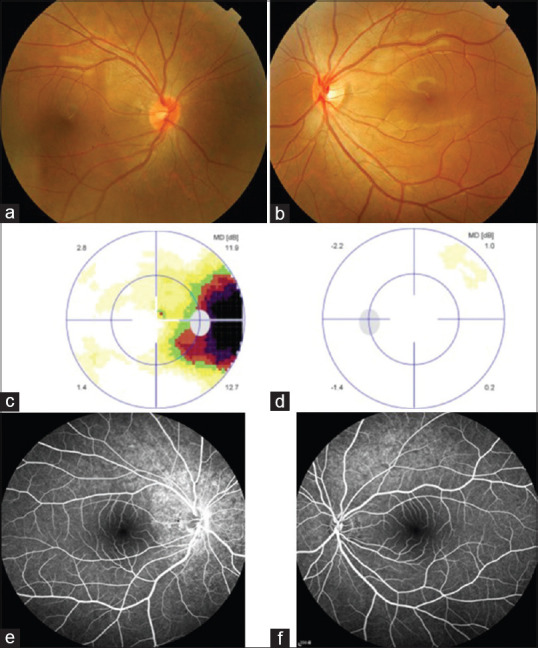
Funduscopic examination at presentation showed a mild change in peripapillary pigmentation and a hyperemic optic disc in the right eye, (a) fundus image of the left eye was unremarkable, (b) visual field examination revealed blind spot enlargement in the right eye, (c) normal visual field was recorded in the left eye, (d) fluorescein angiography showed a window defect in the retinal pigment epithelium at the corresponding area of hyperautofluoresence and optic disc staining at the mid-to-late phase, (e) fluorescein angiography in the left eye was unremarkable, (f)
Figure 2.
(a) Fundus autofluorescent imaging revealed peripapillary hyperautofluoresence in the right eye at presentation. (b) Fundus autofluorescent image of the right eye at the 6-month follow-up revealed no changes in hyperautofluoresence compared with that at presentation. Normal fundus autofluorescence was observed in the left eye at presentation (c) and at the 6-month follow-up, (d) optical coherence tomography showed loss of the ellipsoid line in the right eye at presentation, (e) optical coherence tomography at the 6-month follow-up showed no further loss of the ellipsoid line in the right eye, (f) optical coherence tomography in the left eye was unremarkable at presentation (g) and at the 6-month follow-up (h)
Figure 3.
Visual evoked potential examination showed a significant delayed P100 component in the right eye (a). Electrooculography showed a mildly decreased Arden ratio in the right eye (b)
Figure 4.

Magnetic resonance imaging showed an increased T2 signal in the retrobulbar optic nerve (a). (b) No contrast enhancement was found at the T1 mode
Figure 5.
Electroretinogram showed slight reduction in the amplitude of the photopic and scotopic waves in the right eye compared with the left eye
His chest radiograph, routine blood cell counts, erythrocyte sediment rate, C-reactive protein, immunological profile (including antinuclear antibody, anti-double stranded DNA, antineutrophil cytoplasmic antibodies, rheumatoid factor, C3, and C4), serological test for Syphilis rapid plasma, Treponema pallidum particle agglutination assay, human immunodeficiency virus screening, and screening of antibodies related to viral infection (including herpes simplex virus, cytomegalovirus, toxoplasma, rubella virus, and Epstein–Barr virus) were all normal.
AZOOR was diagnosed in this patient, and he was started on 30 mg oral prednisolone daily (body weight: 70 kg; 7 weeks after symptom onset). Subsequently, his symptoms subjectively improved. However, 2 weeks after treatment, he developed skin folliculitis on both his arms. Because his parents were concerned about this and other side effects of steroid use, prednisolone was discontinued immediately. Apart from steroids, no other medication was administered. A visual field (VF) test, OCT, and autofluorescence imaging performed 6 months later, revealed no disease progression.
Discussion
AZOOR is typically seen in young, Caucasian women with sudden-onset VF defects along with photopsia. Because 90% of patients with AZOOR have a normal fundus appearance at presentation,[4] early diagnosis becomes difficult.[7] Gass et al. found that the median delay in the diagnosis of AZOOR was 17 months.[2] AZOOR may be misdiagnosed as a wide range of other disorders including white dot syndromes, inflammatory/toxic/paraneoplastic retinopathies, and retinal dystrophies. Jiang et al. analyzed 26 patients (38 eyes) with retinal disorders, who were initially diagnosed as having retrobulbar optic neuritis. Among the retinal diseases, AZOOR was most commonly misdiagnosed because of the normal fundus appearance or minimal changes in the fundus, abnormal VEP, and positive relative afferent pupillary defects (RAPDs) in some patients.[8] However, with the advances in autofluorescence imaging and OCT, additional information can be obtained for diagnosis. In the early stages of AZOOR, hyperautofluorescence is present due to outer retinal dysfunction, loss of photopigments, and increased excitation of fluorescent signals emitted from the preserved RPE. In the later stages, retinal and choroidal atrophy occurs, which leads to hypoautofluorescence.[9,10] OCT can detect demonstrate loss or disruption of the ellipsoid line (inner segment–outer segment junction) at the lesion.[11]
Several reports have highlighted the possible association between AZOOR and CNS demyelinating disease.[3,12] The etiology of AZOOR remains unclear; however, autoimmune dysfunction has been suggested to play a critical role. Both AZOOR and demyelinating disease were associated with other autoimmune disorders such as Hashimoto's thyroiditis and relapsing transverse myelitis.[2] In addition, they exhibit similar clinical features such as a relapsing course, predominantly seen in female Caucasian patients, which may have an underlying autoimmune mechanism.[3,12,13] Although no visual symptom of photopsia and vitreous inflammation was observed in the present case, all other electrophysiological and morphological findings support the diagnosis of AZOOR. The mild optic disc swelling could have resulted from primary inflammation at the posterior segment and secondary, the involvement of the optic nerve.
Delayed P100 response of the VEP was observed not only in patients with optic neuropathy but also in those with retinal diseases, including AZOOR.[2,7,14] Therefore, ERG and OCT examinations are crucial in distinguishing AZOOR from optic neuritis when patients present with abnormal VEP. Chai et al. reported a diagnosis of AZOOR in a woman with a visual acuity of 20/20 but with an extinguished P100 wave of VEP. OCT revealed an irregular ellipsoid line over the nasal fovea. Reduced macular sensitivity was suspected as the reason for abnormal VEP.[15]
RAPD is a principal parameter for differentiating optic neuropathies from retinal disorders, and it has been identified in 96% of patients with optic neuritis.[16] However, RAPD was recorded in 24% and 42.9% of patients with AZOOR in the series of Gass and Jiang et al., respectively.[2,8] In a case report by Chai et al., the patient exhibited an RAPD along with normal visual acuity (20/20) and an enlarged blind spot.[15] Because the patient in our case did not exhibit an RAPD, we ruled out optic neuritis.
In an observation by Gass et al. of 51 patients with AZOOR, 72% of the patients had stable VF 6 months after initial presentation, 4% had worsened VF, and 24% had partly improved VF.[2] Steroids have been reported to be effective for treating AZOOR.[5,6,17] Chen et al. reported satisfactory visual outcomes after systemic steroid treatment in nine patients with AZOOR. The early initiation of therapy was speculated as to the reason for satisfactory outcomes compared with other studies.[6] Our patient received short-term oral steroid treatment. His perimetry, OCT findings, and area of hyperautoflurescence remained s[table 6] months after treatment.
In conclusion, numerous clinical aspects of our patients resemble those of optic neuritis. AZOOR has been commonly misdiagnosed as optic neuritis in the past. Through FAF imaging and OCT, additional information can be obtained for distinguishing between these two diseases. Because early intervention with systemic steroids appears to yield better visual improvement in patients with AZOOR, ophthalmologists should know how to differentiate the characteristics of the two diseases to make a prompt diagnosis and take appropriate management measures at the earliest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this article.
References
- 1.Gass JD. Acute zonal occult outer retinopathy.Donders lecture: The Netherlands ophthalmological society, Maastricht, Holland, June 19, 1992. J Clin Neuroophthalmol. 1993;13:79–97. [PubMed] [Google Scholar]
- 2.Gass JD, Agarwal A, Scott IU. Acute zonal occult outer retinopathy: A long-term follow-up study. Am J Ophthalmol. 2002;134:329–39. doi: 10.1016/s0002-9394(02)01640-9. [DOI] [PubMed] [Google Scholar]
- 3.Jacobson DM. Acute zonal occult outer retinopathy and central nervous system inflammation. J Neuroophthalmol. 1996;16:172–7. [PubMed] [Google Scholar]
- 4.Khaleeli Z, Tucker WR, Del Porto L, Virgo JD, Plant GT. Remember the retina: Retinal disorders presenting to neurologists. Pract Neurol. 2018;18:84–96. doi: 10.1136/practneurol-2016-001534. [DOI] [PubMed] [Google Scholar]
- 5.Kuo YC, Chen N, Tsai RK. Acute zonal occult outer retinopathy (AZOOR): A case report of vision improvement after intravitreal injection of Ozurdex. BMC Ophthalmol. 2017;17:236. doi: 10.1186/s12886-017-0638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen SN, Yang CH, Yang CM. Systemic corticosteroids therapy in the management of acute zonal occult outer retinopathy. J Ophthalmol. 2015;2015:1–6. doi: 10.1155/2015/793026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shindo A, Kokubo Y, Taniguchi A, Kuze M, Kuzuhara S. Case of acute zonal occult outer retinopathy (AZOOR): A 15 years' mislabeling as retrobulbar optic neuritis. Rinsho Shinkeigaku. 2007;47:116–8. [PubMed] [Google Scholar]
- 8.Jiang LB, Shen CY, Chen F, Yan WY, Lai TY, Wang NL. Clinical features of retinal diseases masquerading as retrobulbar optic neuritis. Chin Med J (Engl) 2013;126:3301–6. [PubMed] [Google Scholar]
- 9.Mrejen S, Khan S, Gallego-Pinazo R, Jampol LM, Yannuzzi LA. Acute zonal occult outer retinopathy: A classification based on multimodal imaging. JAMA Ophthalmol. 2014;132:1089–98. doi: 10.1001/jamaophthalmol.2014.1683. [DOI] [PubMed] [Google Scholar]
- 10.Fujiwara T, Imamura Y, Giovinazzo VJ, Spaide RF. Fundus autofluorescence and optical coherence tomographic findings in acute zonal occult outer retinopathy. Retina. 2010;30:1206–16. doi: 10.1097/IAE.0b013e3181e097f0. [DOI] [PubMed] [Google Scholar]
- 11.Li D, Kishi S. Loss of photoreceptor outer segment in acute zonal occult outer retinopathy. Arch Ophthalmol. 2007;125:1194–200. doi: 10.1001/archopht.125.9.1194. [DOI] [PubMed] [Google Scholar]
- 12.Hintzen RQ, van den Born LI. Acute zonal occult outer retinopathy and multiple sclerosis. J Neurol Neurosurg Psychiatry. 2006;77:1373–5. doi: 10.1136/jnnp.2006.090415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang JC, Finn AP, Grotting LA, Sobrin L. Acute zonal occult outer retinopathy associated with retrobulbar optic neuritis. J Neuroophthalmol. 2017;37:287–90. doi: 10.1097/WNO.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 14.Lennerstrand G. Delayed visual evoked cortical potentials in retinal disease. Acta Ophthalmol (Copenh) 1982;60:497–504. doi: 10.1111/j.1755-3768.1982.tb00594.x. [DOI] [PubMed] [Google Scholar]
- 15.Chai Y, Yamazaki H, Fujinami K, Tsunoda K, Yamamoto S. Case of acute zonal occult outer retinopathy with abnormal pattern visual evoked potentials. Clin Ophthalmol. 2011;5:1235–41. doi: 10.2147/OPTH.S23194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cox TA, Thompson HS, Corbett JJ. Relative afferent pupillary defects in optic neuritis. Am J Ophthalmol. 1981;92:685–90. doi: 10.1016/s0002-9394(14)74662-8. [DOI] [PubMed] [Google Scholar]
- 17.Barnes AC, Lowder CY, Bessette AP, Baynes K, Srivastava SK. Treatment of acute zonal occult outer retinopathy with intravitreal steroids. Ophthalmic Surg Lasers Imaging Retina. 2018;49:504–9. doi: 10.3928/23258160-20180628-06. [DOI] [PubMed] [Google Scholar]





