Abstract
Introduction
Gene expression association studies of tumor samples have uncovered several long non-coding RNAs (lncRNAs) closely related to various types of cancer. Several lncRNAs have been reported to play essential roles in the progression of papillary thyroid carcinoma (PTC). Novel lncRNA inhibiting proliferation and metastasis (lnc-NLIPMT) is a known regulator of mammary cell proliferation and motility, but its involvement in PTC is unclear.
Materials and Methods
We investigated the role of lnc-NLIPMT in PTC by quantitative real-time polymerase chain reaction (qRT-PCR) on various PTC tissue samples and cell lines. We assessed the effects of overexpression or knockdown of lnc-NLIPMT on the proliferation, migration, and invasion of PTC cells using CCK-8, cell clone formation, and transwell assays. Changes in the expression of N-cadherin and vimentin were detected by immunoblotting.
Results
Our results revealed a downregulation of the expression of lnc-NLIPMT in PTC and a negative correlation between lnc-NLIPMT expression and tumor size (P=0.006). Overexpression of lnc-NLIPMT in TPC-1 and B-CPAP cells significantly suppressed cell proliferation, migration, and invasion, while lnc-NLIPMT knockdown had the opposite effect. In addition, lnc-NLIPMT played an important role in the regulation of the expression of N-cadherin and vimentin.
Conclusion
lnc-NLIPMT inhibits cell proliferation and metastasis of PTC cells and is a potential diagnostic and prognostic biomarker in PTC.
Keywords: papillary thyroid carcinoma, long non-coding RNA, invasion, proliferation, metastasis
Introduction
Thyroid carcinoma (TC) has seen a steady increase in incidence and mortality worldwide and has become the most common malignant tumor of the endocrine system.1–3 During the last few decades, the morbidity of TC increased by 3% annually in the United States.4 Meanwhile, TC is the most prevalent cancer among women under the age of 30 in China.5 Differentiated thyroid cancer (DTC), derived from thyroid follicular epithelial cells, represents the majority (95%) of TC cases.6 In this category, papillary thyroid carcinoma (PTC) is the most common subtype followed by follicular TC.6 After comprehensive treatment, PTC shows favorable survival rates, but the recurrence rate and metastasis of PTC remain high.7,8 In recent years, molecular and genetic biomarkers gained importance in the diagnosis, therapy and observation of PTC.9 For example, the BRAF (V600E) mutation is present in nearly 80% of PTC, although the influence of the BRAF (V600E) mutation is still doubtful, some publications claiming that this mutation giving rise to an aggressive variant frequently associated with distant metastases.10,11 Although there are many basic research studies on PTC, the precise molecular mechanisms of TC remain elusive. Therefore, it is crucial to identify the underlying mechanisms of PTC and to develop novel biomarkers and targeted therapies.
Long non-coding RNAs (lncRNAs) are a class of RNA molecules of more than 200 nucleotides in length without protein-coding capacity. They constitute more than 90% of transcripts in human cells and were once regarded as transcriptional noise.12–14 Compared with messenger-RNAs (mRNAs), lncRNAs are usually characterized by lower abundance, increased nuclear localization, increased tissue-specific expression and less interspecies sequence conservation.15 However, more and more studies have revealed the biological implication of lncRNAs on genetic imprinting, including transcriptional, translational, and epigenetic regulation.16 It has been reported that lncRNAs are involved in the pathogenesis and progression of many diseases, especially in the invasion, metastasis, autophagy, and differentiation of tumor cells.17,18 For example, Li et al revealed that lncRNA ANCR could promote the phosphorylation of EZH2 and suppress the invasion and metastasis of breast cancer.19 Another study showed that LINC00473 is a potential biomarker and therapeutic target for LKB1-inactivated NSCLC by facilitating CRTC/CREB-mediated transcription.20 Moreover, Zhu et al found that lncRNA HOTAIR is an oncogene in PTC and its haplotype-tagging single nucleotide polymorphisms (htSNP) were associated with susceptibility to PTC.21
Lnc-NLIPMT is a newly reported lncRNA transcript of 681 bp with 6 exons which is localized on chromosome 7. We previously demonstrated that lnc-NLIPMT could inhibit the proliferation and motility of breast cancer cells by interacting with glycogen synthase kinase 3β (GSK-3β).22 In this study, we aimed to elucidate the expression and biological functions of lnc-NLIPMT in PTC. Our results indicated that lnc-NLIPMT expression levels are down-regulated in PTC compared with normal thyroid tissue. A negative correlation existed between lnc-NLIPMT expression and tumor size (P=0.006). Our in vitro results demonstrated that overexpression of lnc-NLIPMT suppresses the proliferation and invasion of PTC cells by regulating the expression of N-cadherin and vimentin. Therefore, lnc-NLIPMT may both be a diagnostic and prognostic biomarker in PTC as well as serve as a potential therapeutic target.
Materials and Methods
Tissue Samples
A total of 87 PTC samples and adjacent non-cancerous thyroid samples were collected from patients who underwent surgery at the First Affiliated Hospital of Wenzhou Medical University, China, from March to November in 2017. None of the patients had received radiotherapy or chemotherapy prior to the surgery and all were diagnosed with PTC via a pathological diagnosis. Tissue samples were rapidly snap-frozen in liquid nitrogen immediately after excision and stored at −80 °C until RNA extraction. This study was approved by the Institutional Research Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University and informed consent was provided by all patients.
RNA Extraction and Quantitative Real-Time PCR
Total RNA was extracted from tissue samples or cell lines using TRIzol reagent (Invitrogen Life Technologies, Carlsbad, CA) according to the manufacturer’s instructions. The concentration and purity of the RNA were determined using a NanoDrop ND‐1000 Spectrophotometer (NanoDrop Products, Wilmington, DE). The RNA samples were reverse transcribed into cDNA with ReverTra Ace qPCR RT Kit (Toyobo, Shanghai, China) following the manufacturer’s instructions. The expression levels of lnc-NLIPMT were quantified by qRT-PCR using a S1000 Thermal Cycler (BIO-RAD, CA, USA) with SYBR Green Realtime PCR Master Mix (Toyobo, Shanghai, China). The primer sequences for lncNLIPMT were as follows: 5′-GGCCCAGAGGCAGTAAAGTT-3′ (forward) and 5′-TGTCATGGTGCCAAACAGGA-3′ (reverse). β-actin was used as the internal reference when calculating the relative expression of lnc-NLIPMT by means of the 2-ΔΔCt method. The experiments were performed in triplicate.
Cell Culture and Transfection
Human papillary thyroid carcinoma cell lines TPC-1 and B-CPAP were generously donated by Professor Mingzhao Xing of the Johns Hopkins University School of Medicine, Baltimore, MA, USA. The use of the cell lines were approved by the ethics committee of the First Affiliated Hospital of Wenzhou Medical University. And B-CPAP were authenticated by STR profile. Cells were cultured in RPMI 1640 medium (GIBCO, USA) supplemented with 10% fetal bovine serum (FBS; GIBCO) and 100 U/mL penicillin and 100 µg/mL streptomycin (Invitrogen, Shanghai, China). All cells were cultivated in a standard cell culture incubator (Thermo Fisher, Waltham, MA, USA) at 37°C with 5% CO2.
Small interfering RNA (siRNA) used to silence the expression of lnc-NLIPMT was designed and synthesized by Shanghai Gene Pharma (Shanghai, China). TPC-1 cells were transfected with siRNA using Lipofectamine 2000 (Invitrogen, USA) according to the product’s specification. The si-NLIPMT sequence was as follows: Forward 5ʹ-GCACCCGGCUUACAUGAAATT-3ʹ and Reverse 5ʹ-UUUCAUGUAAGCCGGGUGCTT-3ʹ.
The primary sequence of lnc-NLIPMT was amplified through PCR and cloned into pCDNA 3.1 and retrovirus vector MSCV-puro (Clontech, Palo Alto, CA) to construct the plasmid that expressed lnc-NLIPMT in mammalian cells. TPC-1 and B-CPAP cells were transfected with that plasmid using Lipofectamine 3000 (Invitrogen, USA) to overexpress the lnc-NLIPMT. The empty plasmid was used as a negative control.
Cell Proliferation Assay
The cell growth was assessed by the Cell Counting Kit-8 (CCK-8, Dojindo Laboratories, Japan) following the manufacturer’s protocols. Briefly, TPC-1 cells (1×103 cells/well) or B-CPAP cells (1×103 cells/well) were seeded into a 96-well plate with 100µL complete medium of CCK-8 solution (10 μL) was added every 24 hours, followed by incubation for 2h in a dark cell incubator at 37°C with 5% CO2 afterward. Five multiple pores were conducted for every group. Absorbance was measured at 450 nm using a SpectraMax Plus 384 Microplate Reader (Molecular Devices, CA, USA). Each assay was performed in triplicate.
Cell Colony Formation Assay
Cells were trypsinized and resuspended in complete medium 48h following transfection. TPC-1 cells (1×103 cells/well) and B-CPAP cells (2×103 cells/well) were seeded in 6-well plates, cultured for 6–8 days and then fixed with methanol and stained with 0.1% crystal violet. Images were captured using a camera. Experiments were conducted in triplicate.
Cell Migration and Invasion Assays
Transwell chambers (8µm pore size; Costar, WA, USA) were used to assess the migration and invasion of PTC cells. 48h following transfection, TPC-1 and B-CPAP cells were detached with trypsin and resuspended with medium containing 10% FBS. 200µL suspension, containing 2×104 TPC-1 cells (migration) or 4×105 cells TPC-1 cells (invasion), 5×104 B-CPAP cells (migration) or 1×106 B-CPAP cells (invasion) were added to the upper chamber and 600µL medium containing 30% FBS in the lower compartment, respectively. Following 24h incubation, the cells were fixed with methanol and stained with 0.1% crystal violet. For the invasion assay, the pores were covered with a layer of Matrigel (Corning, NY, USA). Each assay was performed in triplicate. Images from four randomly selected fields of view under 20x magnification were obtained for calculation of cell migration and invasion.
Western Blot Assay
Total proteins were extracted from treated cells by RIPA lysis buffer (Beyotime Biotechnology, Haimen, China) containing 1mM PMSF. Protein concentrations were determined by BCA Protein Assay Kit (Beyotime Biotechnology). Proteins were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS‐PAGE) and transferred to polyvinylidene fluoride (PVDF) membranes (0.22 or 0.45μm; Millipore, Billerica, MA). After blocking with 5% skim milk, the membranes were incubated with primary antibodies at 4°C overnight, followed by secondary anti-rabbit immunoglobulin G antibody coupled to horseradish peroxidase. The signals were detected using the Western Bright ECL detection system (Bio-Rad, Hercules, CA). The primary antibodies used were anti-vimentin, anti-β-actin and anti-N-cadherin from Abcam (Cambridge, MA).
Statistical Analysis
The results were expressed as mean±SD from three independent experiments. Statistical analyses were carried out using SPSS 23.0 (IBM, Chicago, IL, USA). Differences between groups were assessed using Pearson’s χ2 test, paired sample t-test, Student’s t-test, or One-way ANOVA as appropriate. P < 0.05 was considered statistically significant, and two-tailed P values were assumed.
Results
lnc-NLIPMT Was Down-Regulated in Human PTC Tissues and Cells
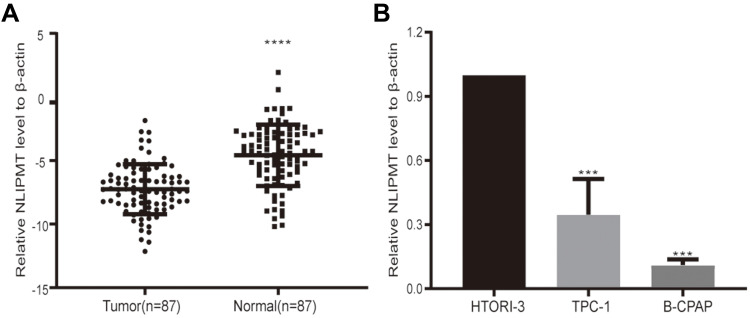
In a previous study, we demonstrated that lnc-NLIPMT inhibits the proliferation and motility of breast cancer cells.22 To identify the potential role of lnc-NLIPMT in PTC, we first measured lnc-NLIPMT expression in 87 pairs of PTC (Tumor) and adjacent normal tissues (Normal) using RT-qPCR. The results indicated that lnc-NLIPMT expression was significantly decreased in cancer tissues compared with the corresponding adjacent normal tissues (P<0.0001) (Figure 1A). Similarly, we employed qRT-PCR to assess lnc-NLIPMT expression in two PTC cell lines (TPC-1 and B-CPAP) and in the normal thyroid cell line HTORI3. The expression level of lnc-NLIPMT was lower in both PTC cell lines than in the normal thyroid cell line HTORI-3 (P<0.001) (Figure 1B). Together, these results suggested that lnc-NLIPMT is downregulated in PTC.
Figure 1.
lnc-NLIPMT expression in PTC tissues and cell lines. (A) lnc-NLIPMT transcripts in PTC tissues and corresponding noncancerous tissues were analyzed using RT‐PCR (****P<0.0001; Mann‐Whitney U-test). (B) Relative expression of lnc-NLIPMT in HTORI-3 human normal thyrocyte cell line compared with two PTC cell lines (***P<0.001). β-actin was used as an internal control.
Relationship Between lnc-NLIPMT Expression and Clinicopathological Features
To establish whether lnc-NLIPMT expression was involved in tumorigenesis and progression of PTC, we investigated the relationship between the lnc-NLIPMT expression and the clinical characteristics by collecting relevant clinicopathologic information of the 87 patients. Based on the median value of the lnc-NLIPMT expression level, we categorized the PTC tissues into a high-expression group (n=44) and a low-expression group (n=43). The results from the validation cohort showed that lower expression of lnc-NLIPMT corresponded to larger tumor size (P= 0.006) (Table 1).
Table 1.
The Relationship Between NLIPMT Expression and Clinicopathologic Features in the Validated Cohort
| Characteristics | Low Expression (n=43) | High Expression (n=44) | P value |
|---|---|---|---|
| Age at diagnosis, years | |||
| ≤ 45 years | 21 | 24 | 0.594 |
| >45 years | 22 | 20 | |
| Gender | |||
| Female | 35 | 35 | 0.828 |
| Male | 8 | 9 | |
| Tumor size in mm | |||
| ≤ 10 mm | 12 | 25 | 0.006* |
| > 10 mm | 31 | 19 | |
| Lymph node metastasis | |||
| YES | 7 | 9 | 0.294 |
| NO | 36 | 35 | |
| Clinical stage | |||
| I | 35 | 31 | 0.615 |
| II | 8 | 13 |
Notes: I: ≤ 45 years anyT anyN M0, >45 years T1N0M0. II: ≤ 45 years anyT anyN M1, >45 years T2N0M0. *P<0.05.
lnc-NLIPMT Inhibits PTC Cell Proliferation and Cell Colony Formation
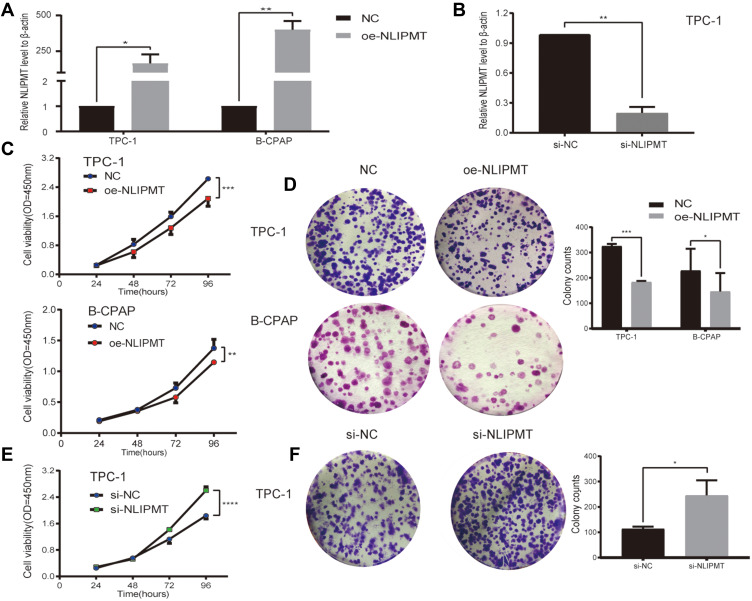
Based on the above results, we conjectured that lnc-NLIPMT may play a suppressor role in PTC initiation and progression. We then conducted a series of in vitro experiments to verify our hypothesis. Considering that lnc-NLIPMT expression is decreased in PTC tissues compared with normal tissues, we first tested the hypothesis that the lnc-NLIPMT overexpression would attenuate proliferation and metastasis. We prepared B-CPAP and TPC-1 cells over-expressing lnc-NLIPMT by transfection with an lnc-NLIPMT expression plasmid. In addition, we tested the impact of lnc-NLIPMT down-regulation on tumorigenesis and progression. TPC-1, which had higher expression of lnc-NLIPMT than B-CPAP, was transfected with siRNA. As confirmed by qRT-PCR, lnc-NLIPMT expression was effectively upregulated (Figure 2A) or downregulated (Figure 2B) in relevant TC cell lines. As shown, cell proliferation (Figure 2C) and colony formation (Figure 2D) were significantly inhibited compared to the control group when lnc-NLIPMT was overexpressed, while cell proliferation and colony formation were enhanced when lnc-NLIPMT expression was knocked down (Figure 2E and F, respectively). These results indicated that lnc-NLIPMT plays an inhibitory role in PTC germination and development.
Figure 2.
lnc-NLIPMT inhibits the growth of PTC cells in vitro. (A) The overexpression of lnc-NLIPMT(oe-NLIPMT) was confirmed by qRT-PCR. lnc-NLIPMT expression was dramatically increased in TPC-1 and B-CPAP transfected with the NLIPMT plasmid, compared with the negative control (NC). (B) The knockdown of lnc-NLIPMT in TPC-1 cell transfected with si-NLIPMT compared with NC was validated by qRT-PCR. (C) CCK-8 assays and (D) colony formation assays show growth inhibition of TPC-1 and B-CPAP cells overexpressing lnc-NLIPMT compared with their corresponding control cells. (E) CCK-8 assays and (F) colony formation assays showing down-regulation of lnc-NLIPMT in TPC-1 cell stimulates proliferation compared with control cells. (P-values were calculated by Student’s t-test, *P < 0.05; **P < 0.01; ***P < 0.001; ****P<0.0001).
lnc-NLIPMT Inhibits Migratory and Invasive Capacities of PTC Cell Lines in vitro
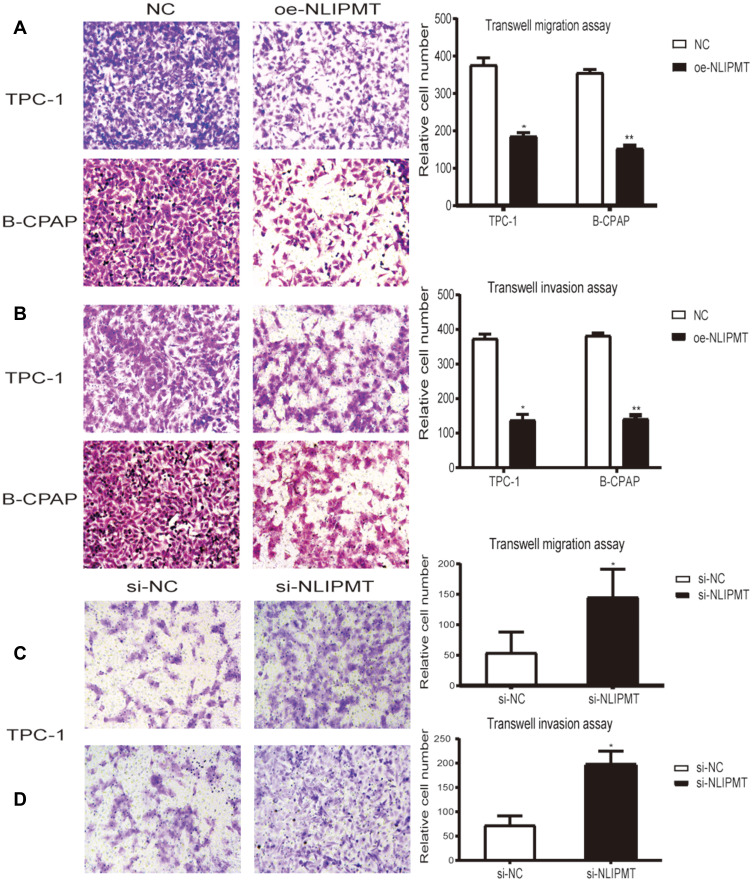
Next, we investigated the role of lnc-NLIPMT in the migratory and invasive potential of PTC cell lines. The results revealed that overexpression of lnc-NLIPMT in TPC-1 or B-CPAP cells dramatically suppressed their migration (Figure 3A) and invasion (Figure 3B). On the other hand, migration and invasion were enhanced when lncRNA-NLIPMT was silenced in TPC-1 (Figure 3C and D, respectively).
Figure 3.
lnc-NLIPMT inhibits the metastasis of PTC cells. (A, B) Up-regulation of lnc-NLIPMT expression in TPC-1 and B-CPAP cells inhibits migration (A) and invasion (B) compared with control cells (NC). (C, D) Down-regulation of lnc-NLIPMT expression by transfection of TPC-1 cells with si-NLIPMT enhances migration (C) and invasion (D) compared with NC Statistical analysis was performed using Student’s t-test. (*P < 0.05; **P < 0.01).
lnc-NLIPMT Suppresses Migration and Invasion via N-Cadherin and Vimentin
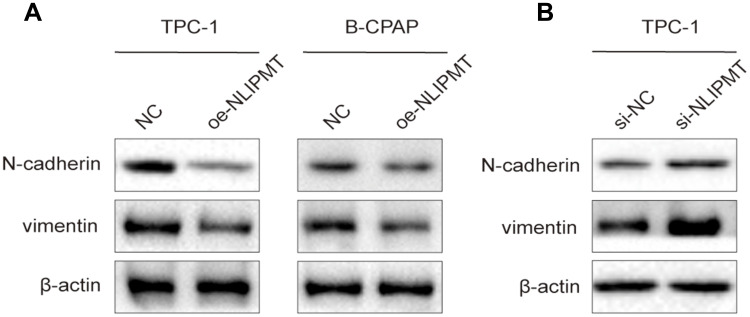
The above results indicated that lnc-NLIPMT is a potential tumor-suppressor factor which inhibits the migration and invasion of PTC cells. It has been reported that epithelial-mesenchymal transition (EMT) plays a key role in the process of tumor migration and invasion.23,24 To explore whether EMT was affected by lnc-NLIPMT in PTC, we examined the levels of epithelial and mesenchymal markers in TPC-1 and B-CPAP via Western blot. The results showed that lnc-NLIPMT overexpression was associated with an increase in N-cadherin and vimentin expression (Figure 4A), while silencing of lnc-NLIPMT reduced the expression levels of N-cadherin and vimentin (Figure 4B). Therefore, we demonstrated that lncRNA-NLIMPT inhibits cell motility by modulating the expression of N-cadherin and vimentin.
Figure 4.
lnc-NLIPMT regulates migration and invasion of PTC cell lines by modulating N-cadherin and vimentin expression. (A) The effect of the overexpression (oe) of lnc-NLIPMT on N-cadherin and vimentin expression in TPC-1 and B-CPAP was assessed by Western blot. (B) The effect of the downregulation of lnc-NLIPMT on N-cadherin and vimentin expression in TPC-1 was assessed by Western blot.
Discussion
LncRNAs play key roles in various biological processes, especially the occurrence and development of tumors.16–18 Recent studies have revealed several lncRNAs that are involved in PTC. For example, lncRNA FAL1, lncRNA MALAT-1, and LncRNA IQGAP1 were found tightly associated with the malignant behavior of PTC.25,26 High-throughput sequencing has become an important method to identify differentially expressed lncRNAs. We previously reported that the novel lnc-NLIPMT was repressed in breast cancer and showed that it can inhibit the aggressiveness of breast cancer by reducing phosphorylated glycogen synthase kinase 3β (GSK-3β).22 However, its impact on PTC remained unknown.
Here, our work focused on the role of lnc-NLIPMT dysregulation in PTC. Lnc-NLIPMT acts as a tumor suppressor in breast cancer. Overexpression of lnc-NLIPMT reduces the amount of phosphorylated glycogen synthase kinase 3β in breast cancer, thus repressing the proliferation and motility of breast cancer cells. The present study demonstrated that lnc-NLIPMT expression was significantly lower in PTC tissues and cell lines compared to normal counterparts. Moreover, lnc-NLIPMT overexpression remarkably restrained malignant behaviors of PTC cells, such as proliferation, colony formation, invasion, and migration. Additionally, knockdown of lnc-NLIPMT enhanced the proliferation and invasion of TPC-1 cells. Taken together, these results are consistent with a role of lnc-NLIPMT in PTC and mirror its role in breast cancer.
The underlying mechanisms of the inhibition of cellular proliferation and invasion by lnc-NLIPMT overexpression need further study. Certain lncRNAs have been reported to play important roles in the proliferation of PTC cells and their function and mechanism have been investigated in detail. For example, lncRNA AB074169 inhibits proliferation of PTC cells via modulation of KH‑type splicing regulatory protein‑mediated p21 expression.27 LncRNA HIT000218960 increases PTC cell proliferation by promoting high-mobility group AT‑hook2 expression.28 LncRNA RP11-476D10.1 promotes proliferation of PTC cells by downregulating miR-138-5p which is associated with upregulation of LRRK2 expression.29 LncRNA RPL34-AS1 inhibits cell proliferation and invasion while promoting apoptosis in PTC by competitively binding to miR-3663-3p/RGS4.30 Research has shown that epithelial-mesenchymal transition (EMT) plays a pivotal role in tumor invasion and metastasis.23,24 In addition, studies have shown that EMT is active in TC cells and this is closely associated with extensive invasion and distant metastasis of TC.31,32 The process of EMT is very complex involving a variety of growth factors, transcriptional regulators, and multiple signaling pathways and affected by the tumor microenvironment in the meantime.33,34 EMT is characterized by a deficiency of epithelial markers E-cadherin and β-catenin and by the up-regulation of the interstitial markers N-cadherin, vimentin, andα-smooth muscle actin (SMA), which results in decreased cellular adhesion and tumor metastasis.35,36 Similarly, we found that lncRNA-NLIPMT regulates the invasiveness of PTC through the process of EMT. The expression of mesenchymal markers N-cadherin and vimentin were reduced by lnc-NLIPMT overexpression, while their expression was increased when lnc-NLIPMT was silenced. This result demonstrated that lnc-NLIPMT may act as a tumor suppressor in TC and may reveal another potential mechanism for metastasis inhibition by lncRNA-NLIPMT.
MicroRNAs (miRNAs) are a class of endogenous non-coding RNAs of about 22 nucleotides in length that participate in tumorigenesis and development through various biological mechanisms.37 Numerous studies have found that lncRNAs can interact with miRNAs and thereby induce tumor occurrence and progression.38,39 LncRNA MALAT1 was shown to enhance the invasiveness of esophageal squamous carcinoma cells by inhibiting miR-101 and miR-207.40 Using the DIANA-lncBase website we identified the miRNAs that are predicted to interact with lncRNA NLIPMT. Our results suggested that lnc-NLIPMT may regulate multiple miRNAs, including miR-4778-3p, miR-17-3p, miR-593-3p and others. Xu et al found that miR-17-3p is associated with radiosensitivity of advanced prostate cancer, and that up-regulation of miR-17-3p significantly inhibits the activity of major antioxidant enzymes in mitochondria, thereby enhancing the sensitivity to radiotherapy in advanced prostate cancer.41 It has also been found that miR-17-3p may be a tumor suppressor in breast cancer.42 This may be another molecular mechanism by which lnc-NLIPMT inhibits TC tumorigenesis. We will explore the interaction between NLIPMT and miR-17-3p in future experiments.
In summary, our study found that the expression of lnc-NLIPMT was low in PTC compared with normal thyroid tissue and that lnc-NLIPMT may function as a tumor suppressor in PTC. Additionally, NLIPMT may inhibit tumor invasion in PTC via suppression of EMT. Therefore, we propose that lnc-NLIPMT is a reliable biomarker for the diagnosis and prognosis of PTC. Since lnc-NLIPMT plays an important role in the development and progression of PTC it might also be a potential therapeutic target.
Funding
This study was funded by the Natural Science Foundation of Zhejiang Province (LY20H160010).
Ethical Approval
Ethical approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. 2016;12:646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.La Vecchia C, Malvezzi M, Bosetti C, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015;136:2187–2195. [DOI] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 4.Lim H, Devesa SS, Sosa JA, et al. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017;317(13):1338–1348. doi: 10.1001/jama.2017.2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 6.Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet. 2016;388(10061):2783–2795. doi: 10.1016/S0140-6736(16)30172-6 [DOI] [PubMed] [Google Scholar]
- 7.Yin Y, Hong S, Yu S, et al. MiR-195 inhibits tumor growth and metastasis in papillary thyroid carcinoma cell lines by targeting CCND1 and FGF2. Int J Endocrinol. 2017;2017:6180425. doi: 10.1155/2017/6180425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ge M-H, Cao J, Wang J-Y, et al. Nomograms predicting disease-specific regional recurrence and distant recurrence of papillary thyroid carcinoma following partial or total thyroidectomy. Medicine (Baltimore). 2017;96(30):e7575. doi: 10.1097/MD.0000000000007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Penna GC, Vaisman F, Vaisman M, et al. Molecular markers involved in tumorigenesis of thyroid carcinoma: focus on aggressive histotypes. Cytogenet Genome Res. 2016;150:194–207. doi: 10.1159/000456576 [DOI] [PubMed] [Google Scholar]
- 10.Nikiforova MN, Kimura ET, Gandhi M, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003;88(11):5399–5404. doi: 10.1210/jc.2003-030838 [DOI] [PubMed] [Google Scholar]
- 11.Asioli S, Erickson LA, Sebo TJ, et al. Papillary thyroid carcinoma with prominent hobnail features: a new aggressive variant of moderately differentiated papillary carcinoma. A clinicopathologic, immunohistochemical, and molecular study of eight cases. Am J Surg Pathol. 2010;34:44–52. [DOI] [PubMed] [Google Scholar]
- 12.Mattick JS, Rinn JL. Discovery and annotation of long noncoding RNAs. Nat Struct Mol Biol. 2015;22(1):5–7. doi: 10.1038/nsmb.2942 [DOI] [PubMed] [Google Scholar]
- 13.Prensner JR, Chinnaiyan AM. The emergence of lncRNAs in cancer biology. Cancer Discov. 2011;1(5):391–407. doi: 10.1158/2159-8290.CD-11-0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lan X, Sun W, Zhang P, et al. Downregulation of long noncoding RNA NONHSAT037832 in papillary thyroid carcinoma and its clinical significance. Tumour Biol. 2016;37(5):6117–6123. doi: 10.1007/s13277-015-4461-4 [DOI] [PubMed] [Google Scholar]
- 15.Nakagawa S, Kageyama Y. Nuclear lncRNAs as epigenetic regulators—beyond skepticism. Biochim Biophys Acta. 2014;1839(3):215–222. doi: 10.1016/j.bbagrm.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 16.Khorkova O, Hsiao J, Wahlestedt C. Basic biology and therapeutic implications of lncRNA. Adv Drug Deliv Rev. 2015;87:15–24. doi: 10.1016/j.addr.2015.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hangauer MJ, Vaughn IW, McManus MT, Rinn JL. Pervasive transcription of the human genome produces thousands of previously unidentified long intergenic noncoding RNAs. PLoS Genet. 2013;9(6):e1003569. doi: 10.1371/journal.pgen.1003569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng G, Sui G. Noncoding RNA in oncogenesis: a new era of identifying key players. Int J Mol Sci. 2013;14:18319–18349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z, Hou P, Fan D, et al. The degradation of EZH2 mediated by lncRNA ANCR attenuated the invasion and metastasis of breast cancer. Cell Death Differ. 2017;24(1):59–71. doi: 10.1038/cdd.2016.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Z, Li J-L, Lin S, et al. cAMP/CREB-regulated LINC00473 marks LKB1-inactivated lung cancer and mediates tumor growth. J Clin Invest. 2016;126(6):2267–2279. doi: 10.1172/JCI85250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu H, Lv Z, An C, et al. Onco-lncRNA HOTAIR and its functional genetic variants in papillary thyroid carcinoma. Sci Rep. 2016;6(1):31969. doi: 10.1038/srep31969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang Y, Lin L, Zhong S, et al. Overexpression of novel lncRNA NLIPMT inhibits metastasis by reducing phosphorylated glycogen synthase kinase 3β in breast cancer. J Cell Physiol. 2019;234(7):10698–10708. doi: 10.1002/jcp.27738 [DOI] [PubMed] [Google Scholar]
- 23.Garber K. Epithelial-to-mesenchymal transition is important to metastasis, but questions remain. J Natl Cancer Inst. 2008;100(4):232–239. doi: 10.1093/jnci/djn032 [DOI] [PubMed] [Google Scholar]
- 24.Thiery JP, Acloque H, Huang RYJ, et al. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139(5):871–890. doi: 10.1016/j.cell.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 25.Jeong S, Lee J, Kim D, et al. Relationship of Focally Amplified Long noncoding on chromosome 1 (FAL1) lncRNA with E2F transcription factors in thyroid cancer. Medicine (Baltimore). 2016;95(4):e2592. doi: 10.1097/MD.0000000000002592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang J-K, Ma L, Song W-H, et al. MALAT1 promotes the proliferation and invasion of thyroid cancer cells via regulating the expression of IQGAP1. Biomed Pharmacother. 2016;83:1–7. [DOI] [PubMed] [Google Scholar]
- 27.Gou Q, Gao L, Nie X, et al. Long noncoding RNA AB074169 inhibits cell proliferation via modulation of KHSRP-mediated CDKN1a expression in papillary thyroid carcinoma. Cancer Res. 2018;78(15):4163–4174. doi: 10.1158/0008-5472.CAN-17-3766 [DOI] [PubMed] [Google Scholar]
- 28.Li T, Yang X-D, Ye C-X, et al. Long noncoding RNA HIT000218960 promotes papillary thyroid cancer oncogenesis and tumor progression by upregulating the expression of high mobility group AT-hook 2 (HMGA2) gene. Cell Cycle. 2017;16(2):224–231. doi: 10.1080/15384101.2016.1261768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao Y, Zhao L, Li J, et al. Silencing of long noncoding RNA RP11-476D10.1 enhances apoptosis and autophagy while inhibiting proliferation of papillary thyroid carcinoma cells via microRNA-138-5p-dependent inhibition of LRRK2. J Cell Physiol. 2019;234(11):20980–20991. doi: 10.1002/jcp.28702 [DOI] [PubMed] [Google Scholar]
- 30.Ji L, Fan X, Zhou F, et al. lncRNA RPL34-AS1 inhibits cell proliferation and invasion while promoting apoptosis by competitively binding miR-3663-3p/RGS4 in papillary thyroid cancer. J Cell Physiol. 2020;235(4):3669–3678. doi: 10.1002/jcp.29256 [DOI] [PubMed] [Google Scholar]
- 31.Wu J, Zhang Y, Cheng R, et al. Expression of epithelial-mesenchymal transition regulators TWIST, SLUG and SNAIL in follicular thyroid tumours may relate to widely invasive, poorly differentiated and distant metastasis. Histopathology. 2019;74:780–791. [DOI] [PubMed] [Google Scholar]
- 32.Montemayor-Garcia C, Hardin H, Guo Z, et al. The role of epithelial mesenchymal transition markers in thyroid carcinoma progression. Endocr Pathol. 2013;24(4):206–212. doi: 10.1007/s12022-013-9272-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaffer CL, San Juan BP, Lim E, et al. EMT, cell plasticity and metastasis. Cancer Metastasis Rev. 2016;35:645–654. [DOI] [PubMed] [Google Scholar]
- 34.Guarino M. Epithelial–mesenchymal transition and tumour invasion. Int J Biochem Cell Biol. 2007;39(12):2153–2160. doi: 10.1016/j.biocel.2007.07.011 [DOI] [PubMed] [Google Scholar]
- 35.Liu L-K, Jiang X-Y, Zhou -X-X, et al. Upregulation of vimentin and aberrant expression of E-cadherin/β-catenin complex in oral squamous cell carcinomas: correlation with the clinicopathological features and patient outcome. Mod Pathol. 2010;23(2):213–224. doi: 10.1038/modpathol.2009.160 [DOI] [PubMed] [Google Scholar]
- 36.Vosgha H, Ariana A, Smith RA, et al. miR-205 targets angiogenesis and EMT concurrently in anaplastic thyroid carcinoma. Endocr Relat Cancer. 2018;25(3):323–337. doi: 10.1530/ERC-17-0497 [DOI] [PubMed] [Google Scholar]
- 37.Rupaimoole R, Slack FJ. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat Rev Drug Discov. 2017;16:203–222. [DOI] [PubMed] [Google Scholar]
- 38.Zhou X, Gao Q, Wang J, et al. Linc-RNA-RoR acts as a “sponge” against mediation of the differentiation of endometrial cancer stem cells by microRNA-145. Gynecol Oncol. 2014;133(2):333–339. doi: 10.1016/j.ygyno.2014.02.033 [DOI] [PubMed] [Google Scholar]
- 39.Militello G, Weirick T, John D, et al. Screening and validation of lncRNAs and circRNAs as miRNA sponges. Brief Bioinform. 2017;18:780–788. [DOI] [PubMed] [Google Scholar]
- 40.Wang X, Li M, Wang Z, et al. Silencing of long noncoding RNA MALAT1 by miR-101 and miR-217 inhibits proliferation, migration, and invasion of esophageal squamous cell carcinoma cells. J Biol Chem. 2015;290(7):3925–3935. doi: 10.1074/jbc.M114.596866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Z, Zhang Y, Ding J, et al. miR-17-3p downregulates mitochondrial antioxidant enzymes and enhances the radiosensitivity of prostate cancer cells. Mol Ther Nucleic Acids. 2018;13:64–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shincy JS, Panagal M, Jereena J, et al. Computational identification of microRNA-17-3p in breast cancer cells. Microrna. 2017;6:208–212. [DOI] [PubMed] [Google Scholar]