Abstract
Parkinson’s disease (PD) is a progressive neurological disorder primarily affecting motor function resulting in tremor at rest, rigidity, bradykinesia, and postural instability. The physical severity of PD impairments can be quantified through the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), a widely used clinical rating scale. Accurate and quantitative assessment of disease progression is critical to developing a treatment that slows or stops further advancement of the disease. Prior work has mainly focused on dopamine transport neuroimaging for diagnosis or costly and intrusive wearables evaluating motor impairments. For the first time, we propose a computer vision-based model that observes non-intrusive video recordings of individuals, extracts their 3D body skeletons, tracks them through time, and classifies the movements according to the MDS-UPDRS gait scores. Experimental results show that our proposed method performs significantly better than chance and competing methods with an F1-score of 0.83 and a balanced accuracy of 81%. This is the first benchmark for classifying PD patients based on MDS-UPDRS gait severity and could be an objective biomarker for disease severity. Our work demonstrates how computer-assisted technologies can be used to non-intrusively monitor patients and their motor impairments. The code is available at https://github.com/mlu355/PD-Motor-Severity-Estimation.
Keywords: Movement Disorder Society Unified Parkinson’s Disease Rating Scale, Gait Analysis, Computer Vision
1. Introduction
Parkinson’s disease (PD) is a progressive neurological disorder that primarily affects motor function. Early, accurate diagnosis and objective measures of disease severity are crucial for development of personalized treatment plans aimed to slow or stop continual advancement of the disease [27]. Prior works aiming to objectively assess PD severity or progression are either based on neuroimages [1,4] or largely rely on quantifying motor impairments via wearable sensors that are expensive, unwieldy, and sometimes intrusive [12,13]. With the rapid development of deep learning, video-based technologies now offer non-intrusive and scalable ways of quantifying human movements [16,7], yet to be applied to clinical applications such as PD.
PD commonly causes slowing of movement, called bradykinesia, and stiffness, called rigidity, that is visible during the gait and general posture of patients. The Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) [10] is the most commonly used method in clinical and research to assess the severity of these motor symptoms. Specifically, the MDS-UPDRS gait test requires a subject to walk approximately 10 meters away from and toward an examiner. Trained specialists assess the subject’s posture with respect to movement and balance (e.g., ‘stride amplitude/speed’, ‘height of foot lift’, ‘heel strike during walking’, ‘turning’, and ‘arm swing’) by observation. MDS-UPDRS item 3.10 is scored on a 5-level scale that assesses the severity of PD gait impairment, ranging from a score of 0 indicating no motor impairments to a score of 4 for patients unable to move independently (see Fig. 1).
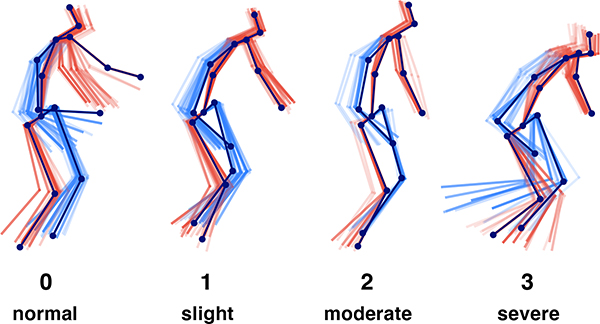
Fig.1:
Progressive PD impairments demonstrated by 3D gait (poses fade over time; left/right distinguished by color) with MDS-UPDRS gait score shown below each skeleton. Participants are taken from our clinical dataset. Classes 0 to 2 progressively decrease in mobility with reduced arm swing and range of pedal motion (i.e., reduced stride amplitude and footlift) while class 3 becomes imbalanced.
We propose a method based on videos to assess PD severity related to gait and posture impairments. Although there exist a few video-based methods which assess gait for PD diagnosis [8,30,11], we define a new task and a principled benchmark by estimating the standard MDS-UPDRS scores. There are several challenges to this new setting: (1) there are no baselines to build upon; (2) since it is harder to recruit patients with severe impairments, the number of participants in our dataset is imbalanced across MDS-UPDRS classes; (3) clinical datasets are typically limited in the number of participants, presenting difficulty for training deep learning models; (4) estimating MDS-UPDRS scores defines a multi-class classification problem on a scale of scores from 0 to 4, while prior work only focused on diagnosing PD vs. normal. To address these challenges, our 3D pose estimation models are trained on large public datasets. Then, we use the trained models to extract 3D poses (3D coordinates of body joints) from our clinical data. Therefore, estimation of the MDS-UPDRS scores is only performed on low-dimensional pose data which are agnostic to the clinical environment and video background. To deal with data imbalance, we propose a model with a focal loss [20], which is coupled with an ordinal loss component [26] to leverage the order of the MDS-UPDRS scores.
Our novel approach for automatic vision-based evaluation of PD motor impairments takes monocular videos of the MDS-UPDRS gait exam as input and automatically estimates each participants’s gait score on the MDS-UPDRS standard scale. To this end, we first identify and track the participant in the video. Then, we extract the 3D skeleton (a.k.a. pose) from each video frame (visualized in Fig. 1). Finally, we train our novel temporal convolutional neural network (TCNN) on the sequence of 3D poses by training a Double-Features Double-Motion Network [31] (DD-Net) with the new hybrid ordinal-focal objective, which we will refer to as hybrid Ordinal Focal DDNet (OF-DDNet) (see Fig. 2).
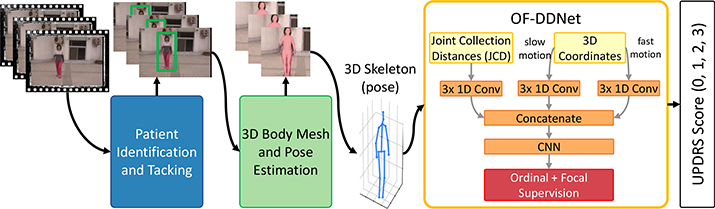
Fig.2:
The proposed framework: we first track the participant throughout the video and remove other persons, e.g., clinicians. Then, we extract the identified participants’ 3D body mesh and subsequently the skeletons. Finally, our proposed OF-DDNet estimates the MDS-UPDRS gait score based on only the 3D pose sequence.
The novelties of our work are three-fold: (1) we define a new benchmark for PD motor severity assessment based on video recordings of MDS-UPDRS exams; (2) for the first time, we propose a framework based on 3D pose acquired from non-intrusive monocular videos to quantify movements in 3D space; (3) we propose a method with a hybrid ordinal-focal objective that accounts for the imbalanced nature of clinical datasets and leverages the ordinality MDS-UPDRS scores.
2. Method
As shown in Fig. 2, the input consists of a monocular video of each participant walking in the scene. First, we track each participant in the video using the SORT (Simple Online and Realtime Tracking) algorithm [3] and identify the bounding boxes corresponding to the participant. These bounding boxes along with the MDS-UPDRS exam video are passed to a trained 3D pose extraction model (denoted by SPIN) [18], which provides pose input to OF-DDNet.
2.1. Participant Detection and Tracking
We first detect and track the participant since videos may contain multiple other people, such as clinicians and nurses. To do this, we track each participant in the video with SORT, a realtime tracking algorithm for 2D multiple object tracking in video sequences [31]. SORT uses a Faster Region CNN (FrRCNN) as a detection framework [25], a Kalman filter [15] as the motion prediction component, and the Hungarian algorithm [19] for matching the detected boxes. The participant is assumed to be in all frames, hence we pick the tracked person who is consistently present in all frames with the greatest number of bounding boxes as the patient.
2.2. 3D Body Mesh and Pose Extraction
Next, we extract the 3D pose from each frame by feeding the corresponding image and the bounding box found in the previous step as input to SPIN (SMPL oPtimization IN the loop) [18]. SPIN is a state-of-the-art neural method for estimating 3D human pose and shape from 2D monocular images. Based on a single 2D image, the Human Mesh Recovery (HMR) regressor provided by [16] generates predictions for pose parameters θreg, shape parameters βreg, camera parameters Πreg, 3D joints Xreg of the mesh and their 2D projection Jreg = Πreg(Xreg). Following the optimization routine proposed in SMPLify [5], these are initial parameters for the SMPL body model [21], a function M(θ, β) of pose parameters θ and shape parameters β that returns the body mesh. A linear regressor W performs regression on the mesh to find 3D joints Jsmpl. These regressed joint values are supplied to the iterative fitting routine, which encourages the 2D projection of the SMPL joints Jsmpl to align with the annotated 2D keypoints Jreg by penalizing their weighted distance. The fitted model subsequently provides supervision for the regressor, forming an iterative training loop. In our proposed method, we generate 3D pose for each video frame by performing regression on the 3D mesh output from SMPL, which has been fine-tuned in the SPIN loop. SPIN was initialized with pretrained SMPL [21] and HMR pretrained on the large Human3.6M [14] and MPI-INF-3DHP [22] datasets, providing over 150k training images with 3D joint annotations, as well as large-scale datasets with 2D annotations (e.g., COCO [20] and MPII [2]).
2.3. Gait Score Estimation with OF-DDNet
Our score estimation model, OF-DDNet, builds on top of DD-Net [31] by adding a hybrid ordinal-focal objective. DD-Net [31] was chosen for its state-of-the-art performance at orders of magnitude smaller in parameter size than comparable methods. OF-DDNet takes as input 3D joints and outputs the participant’s MDS-UPDRS gait score. Our model has a lightweight TCNN-based architecture that prevents overfitting. To address the variance of 3D Cartesian joints to both location and viewpoint, two new features are calculated: (1) Joint Collection Distances (JCD) and (2) two-scale motion features. JCD is a location-viewpoint invariant feature that represents the Euclidean distances between joints as a matrix M, where for joints Ji and Jj at frame k of total K frames. Since this is a symmetric matrix, only the upper triangular matrix is preserved and flattened to a dimension of for n joints. A two-scale motion feature is introduced for global scale invariance which measures temporal difference between nearby frames. To capture varying scales of global motion, we calculate slow motion and fast motion
| (1) |
where denotes the set of joints for the kth frame. The JCD and two-scale motion features are embedded into latent vectors at each frame through a series of convolutions to learn joint correlation and reduce the effect of skeleton noise. Then, the embeddings are concatenated and run through a series of 1D convolutions and pooling layers, culminating with a softmax activation on the final layer to output a probability distribution for each class.
2.4. Hybrid Ordinal-Focal Loss
To leverage the ordinal nature of MDS-UPDRS scores and to combat the natural class imbalance in clinical datasets, we propose a hybrid ordinal focal loss with a trade-off hyperparamter λ as . Although many regression or threshold-based ordinal loss functions exist [26,23], this construction allows its use in conjunction with our focal loss.
Focal Loss is introduced to combat class imbalance [20]. It was initially proposed for binary classification, but it is naturally extensible to multi-class classification (e.g., C > 2 classes). We apply focal loss for predicting label y with probability p:
| (2) |
The modulating factor (1 − pi)γ is small for easy negatives where the model has high certainty and close to 1 for misclassified examples. This combats class imbalance by down-weighting learning for easy negatives, while preserving basic cross-entropy loss for misclassified examples. We set the default focusing parameter of γ = 2 and weighting factor α = 0.25 as suggested by [20].
Ordinal Loss is used to leverage the intrinsic order in the MDS-UPDRS scores. We implement a loss function that penalizes predictions more if they are violating the order. This penalization incorporates the actual labels to indicate order instead of the probability vectors used in cross-entropy. Given the estimated label , we calculate the absolute distance and incorporate this with categorical cross-entropy to generate our ordinal loss:
| (3) |
3. Experiments
3.1. Dataset
We collected video recordings from 30 research participants who met UK Brain Bank diagnostic criteria of MDS-UPDRS exams scored by a board-certified movement disorders neurologist. All videos of PD participants were recorded during the off-medication state, defined according to previously published protocols [24]. All study procedures were approved by the Stanford Institutional Review Board and written informed consent was obtained from all participants in this study. We first extracted the sections of the video documenting the gait examination, in which participants were instructed to walk directly toward and away from the camera twice. The gait clips range from 17 seconds to 54 seconds with 30 frames per second. Our dataset includes 21 exams with score 1, 4 exams with score of 2, 4 exams with score of 3 and 1 exam with score 0. Participants who cannot walk at all or without assistance from another person are scored 4, thus we exclude this class from our analysis due to the difficulty in obtaining videos recordings of their gait exam.
To augment the normal control cohort (i.e., score 0), we include samples from the publicly available CASIA Gait Database A [28], a similar dataset with videos of 20 non-PD human participants filmed from different angles. We extracted corresponding videos where participants walk directly toward and away from the camera, with length of minimum 16 and maximum 53 seconds. The underlying differences between the datasets should not bias our analyses because all score estimation algorithms operate on pose data with similar characteristics (same view points and duration) across all classes and we normalize and center the pose per participant by aligning temporal poses based on their hip joint.
3.2. Setup
We preprocess our dataset by 1) clipping each video into samples of 200 frames each, where the number of clips per exam depends on its length, 2) supplying two additional cropped videos per exam for sparse classes 2 and 3 and 3) joint normalization and centering at the mid-hip. To address the subjective nature of MDS-UPDRS scoring by clinicians, we incorporate a voting mechanism. Each sub-clip is labeled same as the exam itself for training to independently examine each sub-part of the exam. This voting mechanism adds robustness to the overall system and allows us to augment the dataset for proper training of the TCNN. To account for the limited dataset size, all evaluations in this study were performed using a participant-based leave-one-out cross-fold validation on all 50 samples. We note that the clips and crops for each exam are never separated by the train/test split. Optimal hyperparameters for the gait scoring model were obtained by performing a grid search using inner leave-one-out cross validation and the Adam optimizer (β1 = 0.9, β2 = 0.999) [17]. Best performance was achieved at 600 epochs, batch size of 64, filter size of 32 and an annealing learning rate from 1−3 to 1−6. For evaluation, we report per-class and macro average F1, area under ROC curve (AUC), precision (Pre), and recall (Rec).
3.3. Baseline Methods and Ablation Studies
We compare our results with several baselines: 1) we feed raw 3D joints from SPIN directly into a 1D CNN modeled after DD-Net architecture sans double features and embedding layer (see Fig. 2), 2) OF-CNN, the same as (1) but with our OF loss, and 3) the original DD-Net [31] with basic cross-entropy loss. We also conduct an ablation study on the choice of pose extraction method by 4) using 2D joints (instead of 3D) extracted with OpenPose [6] as input to OF-DDNet. To evaluate the hybrid loss function, we separately examine our method 5) without the focal loss component and 6) without the ordinal component. We further examine our ordinal component by replacing it with 7) a regression loss (MSE) for DD-Net with an extra sigmoid-activated dense output layer and finally with 8) DeepRank [23], a ranking CNN which cannot be combined with focal loss.
3.4. Results
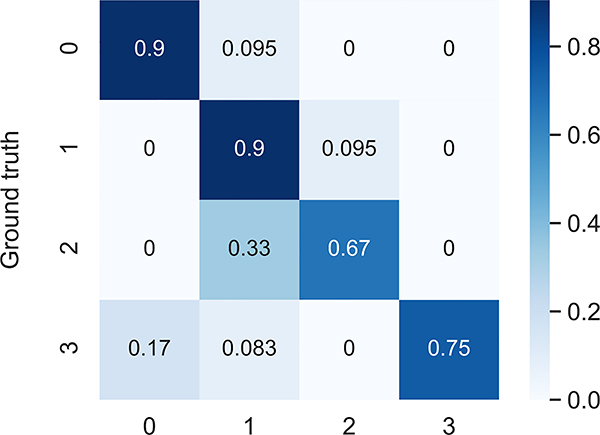
The results of our proposed OF-DDNet are summarized in Table 1. Our method sets a new benchmark for this task with macro-average F1-score of 0.83, AUC of 0.90, precision of 0.86, and balanced accuracy (average recall) of 81%. As seen in the confusion matrix (Fig. 3), the overall metrics for well-represented classes control and class 1 are fairly high, followed by class 3 and then class 2. We observe that class 2 is strictly misclassified as lower severity. The results of comparisons with baseline and ablated methods are summarized in Table 2. Our proposed method achieves significantly better performance than many other methods based on the Wilcoxon signed rank test [29] (p < 0.05), and consistently outperforms all other methods. Our results show that all methods have higher performance on 3D joints input than 2D input, as even a baseline 1D CNN has better performance than the full DD-Net model with 2D joints. This demonstrates that 3D joints provide valuable information for the prediction model, which has not been explored before. Similarly, we note that on 3D joint input, all classification methods outperformed the regression model, suggesting that classification outperforms regression at this task. Regarding the loss function, OF-DDNet significantly outperforms our baseline CNN with categorical cross-entropy. Adding ordinal (Method 5 in the Table) and focal (Method 6) losses to baseline DD-Net both improve accuracy, but their combined performance (OF-DDNet) outperforms all. DeepRank (Method 7) had high confidence on predictions and poor performance on sparse classes, suggesting an overfitting problem that encourages the use of a simple ordinal loss for our small dataset.
Table 1:
Per-class MDS-UPDRS gait score prediction performance of our method.
| Gait Score | F1 | AUC | Pre | Rec |
|---|---|---|---|---|
| 0 | 0.91 | 0.93 | 0.91 | 0.91 |
| 1 | 0.81 | 0.91 | 0.73 | 0.91 |
| 2 | 0.73 | 0.87 | 0.80 | 0.67 |
| 3 | 0.86 | 0.90 | 1.00 | 0.75 |
| Macro Average | 0.83 | 0.90 | 0.86 | 0.81 |
Fig. 3:
Confusion matrix of OF-DDNet.
Table 2:
Comparison with baseline and ablated methods.
| Method | F1 | AUC | Pre | Rec | Method | F1 | AUC | Pre | Rec |
|---|---|---|---|---|---|---|---|---|---|
| OF-DDNet (Ours) | 0.83 | 0.90 | 0.86 | 0.81 | 5) Ours w/o focal | 0.79 | 0.83 | 0.83 | 0.76 |
| 1) Baseline CNN* | 0.73 | 0.86 | 0.79 | 0.69 | 6) Ours w/o ordinal | 0.78 | 0.88 | 0.84 | 0.74 |
| 2) Baseline OF-CNN* | 0.74 | 0.83 | 0.79 | 0.71 | 7) Regression* | 0.67 | n/a | 0.70 | 0.65 |
| 3) DD-Net* [31] | 0.74 | 0.84 | 0.80 | 0.69 | 8) DeepRank* [23] | 0.74 | 0.80 | 0.79 | 0.71 |
| 4) 2D joints* [6] | 0.61 | 0.77 | 0.61 | 0.62 |
indicates statistical difference at (p < 0.05) compared with our method, measured by the Wilcoxon signed rank test [29]. Best results are in bold. See text for details about compared methods.
4. Discussion
Our method achieves compelling results on automatic vision-based assessment of PD severity and sets a benchmark for this task. We demonstrate the possibility of predicting PD motor severity using only joint data as the input to a prediction model, and the efficacy of 3D joint data in particular. Furthermore, we show the effectiveness of a hybrid ordinal-focal loss for tempering the effects of a small, imbalanced dataset and leveraging the ordinal nature of the MDS-UPDRS. However, it is necessary to note that there is inherent subjectivity in the MDS-UPDRS scale [9] despite attempts to standardize the exam through objective criterion (e.g., stride amplitude/speed, heel strike, arm swing). Physicians often disagree on ambiguous cases and lean toward one score versus another based on subtle cues. Clinical context suggests our results are consistent with physician experience. As corroborated in the results of OF-DDNet, the most difficult class to categorize in clinical practice is score 2 since the MDS-UPDRS defines its distinction from score 1 solely by “minor” versus “substantial” gait impairment, shown in Fig. 1. Control (class 0) exhibits high arm swing and range of pedal motion while classes 1 and 2 have progressively reduced mobility and increased stiffness (i.e., reduced arm swing and stride amplitude/foot lift). Class 3 exhibits high imbalance issues with stooped posture and lack of arm swing, which aids mobility, presenting a high fall risk. In practice, class 3 is easier to distinguish from the other classes because it only requires identifying that a participant requires an assisted-walking device and cannot walk independently. Likewise, our model performs well for class 3 except in challenging cases which may require human judgement, such as determining what constitutes “safe” walking.
This study presents a few notable limitations. A relatively small dataset carries risk of overfitting and uncertainty in the results. We mitigated the former through data augmentation techniques and using simple models (DD-Net) instead of deep or complex network architectures; and the latter with leave-one-out cross validation instead of the traditional train/validation/test split used in deep learning. Similarly, our classes are imbalanced with considerably fewer examples in classes 2 and 3 than in classes 0 and 1, which we attempt to address through our custom ordinal focal loss and by augmenting sparse classes through cropping. Additionally, due to a shortage of control participants in our clinical dataset, we include examples of non-PD gait from the public CASIA dataset. The data is obfuscated by converting to normalized pose, which has similar characteristics across both datasets. However, expanding the clinical dataset by recruiting more participants from underrepresented classes would strengthen the results and presents a direction for future work.
5. Conclusion
In this paper, we presented a proof-of-concept of the potential to assess PD severity from videos of gait using an automatic vision-based approach. We provide a first benchmark for estimating MDS-UPDRS scores with a neural model trained on 3D joint data extracted from video. This method works even with a small dataset due to data augmentation, the use of a simple model and our hybrid ordinal focal loss and has opportunity for application to similar video classification problems in the medical space. Our proposed method is simple to set up and use because it only requires a video of gait as input; thus, in remote or resource-limited regions with few experts it provides a way to form estimates of disease progression. In addition, such scalable automatic vision-based methods can help perform time-intensive and tedious collection and labelling of data for research and clinical trials. In conclusion, our work demonstrates how computer-assisted intervention (CAI) technologies can provide clinical value by reliably and unobtrusively assisting physicians by automatic monitoring of PD patients and their motor impairments.
Acknowledgment
This research was supported in part by NIH grants AA010723, AA017347, AG047366, and P30AG066515. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study was also supported by the Stanford School of Medicine Department of Psychiatry Behavioral Sciences 2021 Innovator Grant Program and the Stanford Institute for Human-centered Artificial Intelligence (HAI) AWS Cloud Credit.
References
- 1.Adeli E, Shi F, An L, Wee CY, Wu G, Wang T, Shen D: Joint feature-sample selection and robust diagnosis of parkinson’s disease from mri data. NeuroImage 141, 206–219 (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andriluka M, Pishchulin L, Gehler P, Schiele B: 2d human pose estimation: New benchmark and state of the art analysis. In: Proceedings of the IEEE Conference on computer Vision and Pattern Recognition pp. 3686–3693 (2014) [Google Scholar]
- 3.Bewley A, Ge Z, Ott L, Ramos F, Upcroft B: Simple online and realtime tracking In: ICIP. pp. 3464–3468. IEEE (2016) [Google Scholar]
- 4.Bharti K, Suppa A, Tommasin S, Zampogna A, Pietracupa S, Berardelli A, Pantano P: Neuroimaging advances in parkinson’s disease with freezing of gait: A systematic review. NeuroImage: Clinical p. 102059 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bogo F, Kanazawa A, Lassner C, Gehler P, Romero J, Black MJ: Keep it smpl: Automatic estimation of 3d human pose and shape from a single image In: ECCV. pp. 561–578. Springer; (2016) [Google Scholar]
- 6.Cao Z, Simon T, Wei SE, Sheikh Y: Realtime multi-person 2d pose estimation using part affinity fields. In: CVPR (2017) [DOI] [PubMed] [Google Scholar]
- 7.Chiu H.k., Adeli E, Wang B, Huang DA, Niebles JC: Action-agnostic human pose forecasting In: 2019 IEEE Winter Conference on Applications of Computer Vision (WACV). pp. 1423–1432. IEEE; (2019) [Google Scholar]
- 8.Cho CW, Chao WH, Lin SH, Chen YY: A vision-based analysis system for gait recognition in patients with parkinson’s disease. Expert Systems with applications 36(3), 7033–7039 (2009) [Google Scholar]
- 9.Evers LJ, Krijthe JH, Meinders MJ, Bloem BR, Heskes TM: Measuring parkinson’s disease over time: The real-world within-subject reliability of the mdsupdrs. Movement Disorders 34(10), 1480–1487 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, et al. : Movement disorder society-sponsored revision of the unified parkinson’s disease rating scale (mds-updrs): scale presentation and clinimetric testing results. Movement disorders: official journal of the Movement Disorder Society 23(15), 2129–2170 (2008) [DOI] [PubMed] [Google Scholar]
- 11.Han J, Jeon HS, Jeon BS, Park KS: Gait detection from three dimensional acceleration signals of ankles for the patients with parkinson’s disease. In: Proceedings of the IEEE The International Special Topic Conference on Information Technology in Biomedicine, Ioannina, Epirus, Greece vol. 2628 (2006) [Google Scholar]
- 12.Hobert MA, Nussbaum S, Heger T, Berg D, Maetzler W, Heinzel S: Progressive gait deficits in parkinson’s disease: A wearable-based biannual 5-year prospective study. Frontiers in aging neuroscience 11, 22 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hssayeni MD, Jimenez-Shahed J, Burack MA, Ghoraani B: Wearable sensors for estimation of parkinsonian tremor severity during free body movements. Sensors 19(19), 4215 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ionescu C, Papava D, Olaru V, Sminchisescu C: Human3. 6m: Large scale datasets and predictive methods for 3d human sensing in natural environments. IEEE transactions on pattern analysis and machine intelligence 36(7), 1325–1339 (2013) [DOI] [PubMed] [Google Scholar]
- 15.Kalman RE: A new approach to linear filtering and prediction problems (1960) [Google Scholar]
- 16.Kanazawa A, Black MJ, Jacobs DW, Malik J: End-to-end recovery of human shape and pose. In: CVPR. pp. 7122–7131 (2018) [Google Scholar]
- 17.Kingma DP, Ba J: Adam: A method for stochastic optimization. arXiv preprint arXiv:1412.6980 (2014) [Google Scholar]
- 18.Kolotouros N, Pavlakos G, Black MJ, Daniilidis K: Learning to reconstruct 3D human pose and shape via model-fitting in the loop. In: ICCV (2019) [Google Scholar]
- 19.Kuhn HW: The hungarian method for the assignment problem. Naval research logistics quarterly 2(1–2), 83–97 (1955) [Google Scholar]
- 20.Lin TY, Goyal P, Girshick R, He K, Dollár P: Focal loss for dense object detection. In: CVPR. pp. 2980–2988 (2017) [DOI] [PubMed] [Google Scholar]
- 21.Loper M, Mahmood N, Romero J, Pons-Moll G, Black MJ: Smpl: A skinned multi-person linear model. ACM Trans on graphics 34(6), 1–16 (2015) [Google Scholar]
- 22.Mehta D, Sridhar S, Sotnychenko O, Rhodin H, Shafiei M, Seidel HP, Xu W, Casas D, Theobalt C: Vnect: Real-time 3d human pose estimation with a single rgb camera. vol. 36 (2017), http://gvv.mpi-inf.mpg.de/projects/VNect/ [Google Scholar]
- 23.Pang L, Lan Y, Guo J, Xu J, Xu J, Cheng X: Deeprank: A new deep architecture for relevance ranking in information retrieval. In: Proceedings of the 2017 ACM on Conference on Information and Knowledge Management pp. 257–266 (2017) [Google Scholar]
- 24.Poston KL, YorkWilliams S, Zhang K, Cai W, Everling D, Tayim FM, Llanes S, Menon V: Compensatory neural mechanisms in cognitively unimpaired p arkinson disease. Annals of neurology 79(3), 448–463 (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Redmon J: Darknet: Open source neural networks in c. http://pjreddie.com/darknet/ (2013–2016)
- 26.Rennie JD, Srebro N: Loss functions for preference levels: Regression with discrete ordered labels. In: IJCAI workshop advances in preference handling (2005) [Google Scholar]
- 27.Venuto CS, Potter NB, Ray Dorsey E, Kieburtz K: A review of disease progression models of parkinson’s disease and applications in clinical trials. Movement Disorders 31(7), 947–956 (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang L, Tan T, Ning H, Hu W: Silhouette analysis-based gait recognition for human identification. PAMI 25(12), 1505–1518 (2003) [Google Scholar]
- 29.Wilcoxon F: Individual comparisons by ranking methods In: Breakthroughs in statistics, pp. 196–202. Springer; (1992) [Google Scholar]
- 30.Xue D, Sayana A, Darke E, Shen K, Hsieh JT, Luo Z, Li LJ, Downing NL, Milstein A, Fei-Fei L: Vision-based gait analysis for senior care. arXiv preprint arXiv:1812.00169 (2018) [Google Scholar]
- 31.Yang F, Wu Y, Sakti S, Nakamura S: Make skeleton-based action recognition model smaller, faster and better. In: ACM Multimedia Asia, pp. 1–6 (2019) [Google Scholar]