Abstract
Emerging epidemiological data suggest that white Americans have a lower risk of acquiring COVID-19. Although many studies have pointed to the role of systemic racism in COVID-19 racial/ethnic disparities, few studies have examined the contribution of racial segregation. Residential segregation is associated with differing health outcomes by race/ethnicity for various diseases, including HIV. This commentary documents differing HIV and COVID-19 outcomes and service delivery by race/ethnicity and the crucial role of racial segregation. Using publicly available Census data, we divide US counties into quintiles by percentage of non-Hispanic white residents and examine HIV diagnoses and COVID-19 per 100,000 population. HIV diagnoses decrease as the proportion of white residents increase across US counties. COVID-19 diagnoses follow a similar pattern: Counties with the highest proportion of white residents have the fewest cases of COVID-19 irrespective of geographic region or state political party inclination (i.e., red or blue states). Moreover, comparatively fewer COVID-19 diagnoses have occurred in primarily white counties throughout the duration of the US COVID-19 pandemic. Systemic drivers place racial minorities at greater risk for COVID-19 and HIV. Individual-level characteristics (e.g., underlying health conditions for COVID-19 or risk behavior for HIV) do not fully explain excess disease burden in racial minority communities. Corresponding interventions must use structural- and policy-level solutions to address racial and ethnic health disparities.
Keywords: COVID-19, HIV, disparities, segregation, race, counties
Introduction
Ten weeks after the states began reopening in the wake of the White House's “Opening Up America Again” guidelines, daily COVID-19 cases have been increasing rapidly again in the United States.1 Sustained spikes in COVID-19 cases in the South and the West have resulted in the doubling of US cases nationally in a matter of weeks.2,3 Much of the corresponding press coverage has highlighted differing state and local public health responses based upon partisan divisions with differing observed trajectories of COVID-19 in red and blue counties,4 or the degree to which the surge in new infections is occurring among young adults.5 Mostly missing from the media narrative is the durability of racial disparities as COVID-19 cases gain traction beyond the northeast. Although an analysis recently linked the nationwide relaxation of public health restrictions to increases in COVID-19 cases among Latinx populations,6 a more illuminating question is what is the trajectory of COVID-19 cases nationally in overwhelmingly non-Hispanic white counties since the reopening of the economy?
Some observers have been surprised by the rapid emergence of clear disparities in COVID-19 acquisition and poor health outcomes along the lines of race/ethnicity for an infectious agent that can infect anyone. One approach to making sense of these disparities is to assess the impact of race and ethnicity in the context of HIV. Like COVID-19, HIV is an infectious disease that can infect anyone, yet for which large and persistent racial and ethnicity disparities exist. One important starting point is to acknowledge that race and ethnicity often not only determine where people live in the United States but their health status as well.
Redlining by the federal Home Owner's Loan Corporation in the 1930s not only codified racial segregation nationally by excluding specific communities from key financial and other resource investments, but also continues to determine current racial segregation patterns by Census tract and subsequent health outcomes for various conditions, including COVID-19 and HIV.7,8 A recent analysis reported an association between greater COVID-19 mortality in primarily black neighborhoods and redlining practices in Chicago.9 Racial segregation in another study explained 19% of HIV infection among black people who inject drugs (PWID) as opposed to 3% of HIV infections in white or Latinx PWID;10 and a New York City analysis found that 65% of black men diagnosed with HIV and 68% of new HIV diagnoses among black men occurred in specific zip codes.11
Using publicly available Census data, we divided US counties into quintiles by percentage of non-Hispanic white residents (quintile 1: <60.18%, quintile 2: 60.19–77.39%, quintile 3: 77.40–88.11%, quintile 4: 88.11–93.80%, and quintile 5: >93.80%). COVID-19 diagnoses were standardized per 100,000 population, and graphs depicting the 7-day moving average of diagnoses through June 25, 2020, were generated. We hypothesized that counties with the greatest percentage of non-Hispanic whites (hereafter “white”) would have the least COVID-19 cases before and after reopening the economy (most states partially reopened by May 15, 2020).12 Conversely, counties with the fewest white residents would have the greatest COVID-19 cases. Utilizing the CDC Atlas HIV data per 100,000 population, we also hypothesized that HIV diagnoses data would follow a similar pattern as COVID-19 cases as per county demographics.
COVID-19 and HIV Diagnoses Are Lowest in Primarily White Counties Across the United States
COVID-19 diagnoses are much lower in US counties with a high proportion of whites (even when assigning equal population sizes per quintile) than counties that are more racially diverse. Both the rate of COVID-19 diagnoses and cumulative COVID-19 diagnoses decline across US counties as the proportion of white residents increase: quintile 1: 913.67 cases per 100,000 (1,361,190 cumulative cases); quintile 2: 798.06 (690,889); quintile 3: 469.36 (242,609); quintile 4: 292.34 (71,781); and quintile 5: 187.53 (27,168).
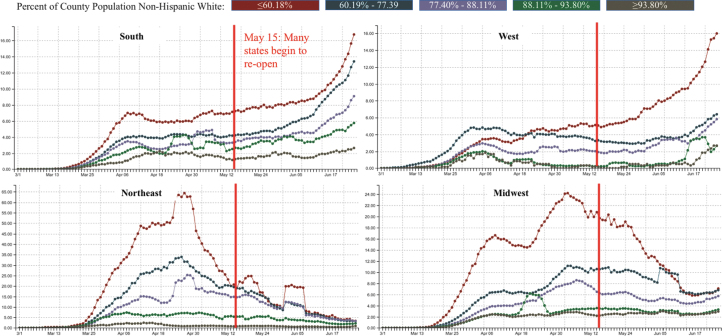
The same pattern is evident by region. Irrespective of US region, COVID-19 cases were lowest in counties with the most number of white residents (Fig. 1). Despite the increasing COVID-19 pandemic across all quintiles in the South and West, infections remain lowest in counties with the highest proportion of white residents; whereas the declining COVID-19 pandemic in the Northeast and Midwest was driven by the decline in cases among more racially diverse counties. Remarkably, COVID-19 diagnoses in Northeastern and Midwestern counties with primarily white residents have remained fairly low and stable throughout the entirety of the COVID-19 crisis.
FIG. 1.
Seven-day moving average of new COVID-19 cases per 100,000 by percentage of white residents in US counties by region (March 1–June 25, 2020). Since re-opening, COVID-19 cases have remained lowest in primarily white counties across region and increased sharply in the most racially diverse counties in the South and West. (Additional data available at https://ehe.amfar.org/inequity/)
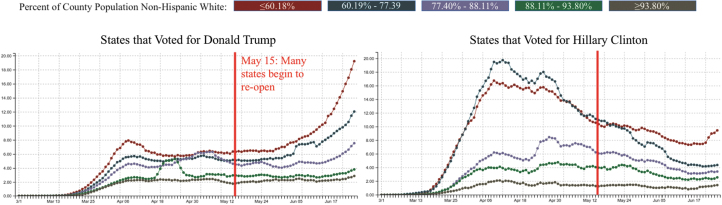
Surveys and studies have found differences by political parties in the acceptance of and adherence to COVID-19 prevention measures such as social distancing13 or wearing face masks,14 as well as comfort in resuming daily activities as the nation opens.15 It has been widely reported that there are increasing COVID-19 cases in states that voted for Donald Trump in 2016, while cases are declining in states that voted for Hillary Clinton.16 We find the same pattern, but the previous analysis misses two crucial details (Fig. 2): First, irrespective of the 2016 presidential candidate preference, COVID-19 cases remain lowest in the whitest counties in blue or red states relative to more diverse counties even after reopening. Second, even though COVID-19 cases have declined or remained stable in states that voted for Hillary Clinton, infections are increasing in the most diverse counties after reopening.
FIG. 2.
Seven-day moving average of new COVID-19 cases by percentage of white residents in US counties by the 2016 State Presidential Election Winner. Since re-opening, COVID-19 cases have remained lowest in primarily white counties and highest among the most racially diverse counties. (Additional data available at https://ehe.amfar.org/inequity/)
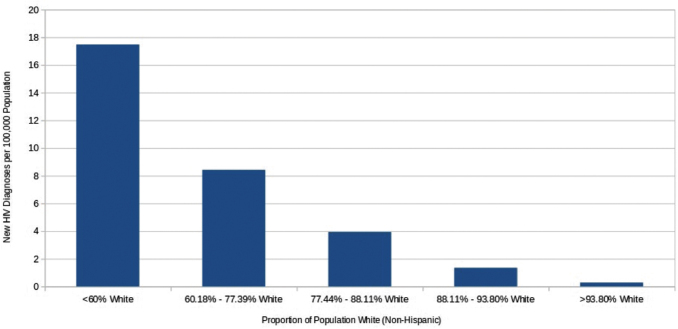
Lower infectious disease burden in primarily white communities is not confined to COVID-19. We found the same stark differences in HIV diagnoses per 100,000 (Fig. 3), with the greatest prevalence in more diverse counties. As with COVID-19 diagnoses, HIV diagnoses decrease progressively across counties nationally as the population of white residents increases.
FIG. 3.
New HIV diagnoses per 100,000 by proportion of county population, white (non-Hispanic) (2018).
COVID-19, Like HIV, Remains Stubbornly Concentrated in Communities of Color
The burden of the COVID-19 pandemic in the United States has not been borne equally. We published the first national study of COVID-19 in black communities and found that both cases and deaths increased as the proportion of black residents increased across counties in the United States.17 Counties with a higher proportion of black Americans (only 22% of counties nationwide and 35% of the US population) account for 47% of COVID-19 cases and 54% of deaths nationally as of June 25, 2020.18 These disparities are not confined to urban areas. We found the same racial disparity among counties in the small metropolitan and rural areas of the United States.
Communities other than black Americans are at elevated risk for COVID-19.19 Latinx households are more likely than other groups to report a myriad of symptoms associated with COVID-19,20 polls have found that more black and Latinx Americans than white Americans know someone who has died of COVID-19,21 and in late May, the Navajo Nation surpassed New York and New Jersey in per capita COVID-19 cases.22
There are multiple factors that contribute to the greater COVID-19 burden in communities of color, but all stem from systemic racism. Our published epidemiological analyses point to specific factors that exacerbate COVID-19 diagnoses in black17 and Latino23 communities, including poverty and living in densely occupied households, living in localities with greater air pollution, lack of health insurance, and being employed in jobs that increase exposure to SARS-COV-2. Our data also show that monolingual Spanish speakers (an economically and politically vulnerable community) have an elevated risk of being diagnosed with COVID-19,23 possibly due to the same systemic inequities that place this same population at a higher risk for HIV opportunistic infections.24
Conversely, fewer white Americans feel at risk for COVID-19 as the demographics of those stricken by the pandemic have become clearer. A Pew poll between April and June 2020 found increasing majorities of black and Latinx respondents being very or somewhat concerned of being hospitalized for COVID-19. Only 43% of white respondents expressed the same concern in the June 2020 poll, which was an 8-point drop from the April poll.25 This racial divide in COVID-19 risk translated into diverging beliefs around reopening businesses during the pandemic. Another poll conducted in March 2020 found that most black, Latinx, and white Americans believed that it was important to keep businesses closed for the sake of public safety (76–83%).26 By June 2020, anxiety remained high among black and Latinx Americans (82% and 65%, respectively), but dropped to only 50% among white Americans.
Focusing on Individual-Level Risks Misses the Larger Narrative That Propels Health Disparities
Many point to underlying health conditions (e.g., obesity, hypertension, diabetes, heart disease) as the source of COVID-19 racial disparities. Although underlying health conditions are greater in communities of color, our study and other studies show that these conditions are not driving COVID-19 racial disparities.27 We found that employment status, access to health insurance, and overcrowded homes were better predictors of COVID-19 than any underlying condition.17,23 Another recent analysis reported greater COVID-19 cases among black Americans despite the fact that social distancing behavior was more common among African Americans.28 Attributing racial disparities to underlying conditions implicitly blames communities of color for COVID-19 disparities due to poor health decisions; but there is ample literature showing how social determinants contribute to worse health outcomes in communities of color,29 including well-cited HIV research studies of youth, gay men, and PWID, which show that HIV disparities persist in black communities despite similar or fewer behavioral risks than whites.30–32 Existing reports underline the contributions of segregation and privilege to race-specific COVID-19 and HIV outcomes.
Studies in Tennessee,33 Texas,34 Philadelphia,35 and New York35 have repeatedly found that COVID-19 testing centers were initially located in white and wealthy rather than poorer or browner neighborhoods. Similarly, an analysis found that whiter and wealthier neighborhoods in New York City witnessed a 40% decline in residents between March and May who fled the city to the safety of country homes, neighboring states, or other locales with fewer COVID-19 diagnoses.36 Those left behind to weather the worst of the COVID-19 crisis in NYC were disproportionately poor, less educated, black, Latinx, or Asian.
Another consequence of residential segregation is proximity to health care facilities. Nationally representative surveys have found that racial minorities on average travel farther than whites to access health care and spend more time in a waiting room to see a health care provider.37 Moreover, the disproportionate number of black and brown workers who cannot work from home during the pandemic38 and must take public transportation poses another risk for COVID-19 infection after reopening the economy.39
Traveling further for care is associated with being uninsured among people living with HIV,40 and distance to care is linked to poor HIV outcomes in communities of color. A cohort study of 3623 respondents (77% non-Hispanic black and 6.2% Latinx) receiving HIV care in the DC area outpatient clinics found that patients who had to travel 5 or miles had a 30% lower retention and care and viral load.41 A separate study of people living with HIV in Birmingham, Alabama, reported that both lack of fuel and lack of a vehicle approached statistical significance in predicting late presentation to HIV care among African American clinic attendees.42
HIV and COVID-19 Racial Disparities Are Not a Fait Accompli…
Systemic inequities that have accrued over hundreds of years, and residential segregation in particular, are not subject to change overnight. This does not mean that these disparities are a fait accompli. There are lessons learned from the HIV literature in reducing health disparities, such as greater access to health care under Medicaid expansion for communities of color, targeted testing, and the provision of wrap-around services.
A higher proportion of blacks (45%) versus whites (35%) living with HIV receive care via Medicaid nationally,43 and states with expanded Medicaid have lower rates of being uninsured as well as fewer hospitalizations among people living with HIV.43,44 Most of the 12 states that have not expanded Medicaid are in the southern United States, a region where 55% of the black community resides. The COVID-19 crisis and the accompanying economic downturn are prompting referenda in various red states to consider the adoption of Medicaid expansion,45 which may increase health care access in communities of color and improve overall health outcomes. Moreover, scaling up testing in communities of color can reduce disparities. A CDC demonstration project that scaled up HIV testing efforts in black and Latino communities in the District of Columbia dramatically reduced the proportion of concurrent AIDS diagnoses at first positive test;46 and encouraging data from a recent study35 show shifts in COVID-19 testing from wealthier and white neighborhoods to poorer and more diverse neighborhoods in cities initially hit by the COVID-19 pandemic. Scaling up services that help blunt the social determinants of health are likewise useful. Local and national studies of the Ryan White Program have found declining HIV-related disparities by race due to the provision of wraparound services,47,48 which may have implications for effectively addressing COVID-19 disparities.
Equity in health care access and delivery can also reduce health-related disparities. Although far from perfect, the US military has endeavored to meaningfully address institutional racism.49 These efforts have also impacted health. A recent CDC study of active US service members living with HIV reported uniformly high rates of viral suppression irrespective of race or ethnicity,50 and studies from the Veterans Administration (VA) have found less pronounced health disparities by race in the VA system compared with the US population overall.51 Similarly, a preprint of nearly 6000 veterans found greater COVID-19 diagnoses among black and Latinx veterans, but no difference by race in COVID-19 deaths.52 In other words, unlike what we have witnessed nationally, black and Latinx COVID-19 patients in the VA's care are not experiencing excess deaths compared with whites.
The premature reopening of our economy has only worsened the COVID-19 crisis among communities of color irrespective of region or blue or red voting patterns. However, there are immediate steps that can be taken to achieve greater health equity and improve health outcomes among all Americans.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
There was no funding provided for this article.
References
- 1. Wu J, Muccari R, Sundberg A, et al. Reopening America: All 50 states have begun to reopen. See what that means for your state. NBC News. 2020. Available at: https://www.nbcnews.com/news/us-news/reopening-america-see-what-states-across-u-s-are-starting-n1195676 (Last accessed July9, 2020).
- 2. CBC News: The National. COVID-19 cases rise in U.S. south, west [YouTube]. 2020. Available at: https://www.youtube.com/watch?v=X6Kr6X1iYLM (Last accessed July9, 2020).
- 3. Infections Swamp the U.S. Which recorded 42% of all its coronaviruses cases in July. New York Times. 2020. Available at: https://www.nytimes.com/2020/08/01/world/coronavirus-covid-19.html (Last accessed August2, 2020).
- 4. Medina J, Gebeloff R The coronavirus is deadliest where democrats live. New York Times. 2020. Available at: https://www.nytimes.com/2020/05/25/us/politics/coronavirus-red-blue-states.html (Last accessed July9, 2020).
- 5. Bosman J, Mervosh S As virus surges, younger people account for ‘disturbing’ number of cases. New York Times. 2020. Available at: https://www.nytimes.com/2020/06/25/us/coronavirus-cases-young-people.html (Last accessed July9, 2020).
- 6. Hubler S, Fuller T, Singhvi A, Love J. Many Latinos couldn't stay home. Now virus cases are soaring in their communities. New York Times. 2020. Available at: https://www.nytimes.com/2020/06/26/us/corona-virus-latinos.html (Last accessed July9, 2020).
- 7. Krieger N, Van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017, Am J Pub Health 2020;110:1046–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krieger N, Wright E, Chen JT, et al. Cancer Stage at diagnosis, historical redlining, and current neighborhood characteristics: Breast, cervical, lung, and colorectal cancers, Massachusetts, 2001–2015. Am J Epidemiol 2020; kwaa045. [Epub ahead of print]; DOI: 10.1093/aje/kwaa045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bertocchi G, Arcangelo. COVID-19, Race, and Redlining. [preprint]. medRxiv 2020. [Epub ahead of print]; DOI: 10.1101/2020.07.11.20148486 [DOI] [Google Scholar]
- 10. Cooper HLF, Linton S, Kelley ME, et al. Risk environments, race/ethnicity, and HIV status in a large sample of people who inject drugs in the United States. PLoS One 2016;11:e0150410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wiewel EW, Hanna DB, Begier EM, et al. High HIV prevalence and diagnosis rates in New York City Black Men. J Community Health 2011;36:141–149 [DOI] [PubMed] [Google Scholar]
- 12. Lee JC, Mervosh S, Avila Y, et al. See how all 50 states are reopening (and closing again). New York Times. 2020. Available at: https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html (Last accessed July9, 2020).
- 13. Danner C. Trump campaign removed social-distancing stickers from seats at Tulsa rally1. New York Magazine. 2020. Available at: https://nymag.com/intelligencer/2020/06/trump-staff-removed-social-distance-stickers-at-tulsa-rally.html (Last accessed July9, 2020).
- 14. Weissert W, Lemire J. Face masks make a political statement in era of coronavirus. Associated Press News. 2020. Available at: https://apnews.com/7dce310db6e85b31d735e81d0af6769c (Last accessed July9, 2020).
- 15. Pew Research Center. Republicans, Democrats move even further apart in coronavirus concerns. 2020. Available at: https://www.pewresearch.org/politics/2020/06/25/republicans-democrats-move-even-further-apart-in-coronavirus-concerns (Last accessed July9, 2020)
- 16. Bump P. The shift of the coronavirus to primarily red states is complete—but it's not that simple. Washington Post. 2020. Available at: https://www.washingtonpost.com/politics/2020/06/24/shift-coronavirus-primarily-red-states-is-complete-its-not-that-simple (Last accessed July9, 2020).
- 17. Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol 2020;47:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. amfAR, The Foundation for AIDS Research. COVID-19 Racial Disparities in U.S. Counties [database]. Available at: https://ehe.amfar.org/inequity (Last accessed July9, 2020)
- 19. McGrath J, Kessler J, Cook A Coronavirus is decimating racially diverse communities large and small. ThirdWay. 2020. Available at: https://www.thirdway.org/memo/coronavirus-is-decimating-racially-diverse-communities-large-and-small (Last accessed July9, 2020).
- 20. Jacoby K, della Cava M. Latino homes report serious COVID-19 symptoms nearly twice as often, survey of 1.6 million shows. USA Today. 2020. Available at: https://www.usatoday.com/story/news/nation/2020/06/01/latino-homes-report-serious-covid-19-symptoms-nearly-twice-often/5243160002 (Last accessed July9, 2020).
- 21. Goldstein A, Guskin E. Almost one-third of black Americans know someone who died of covid-19, survey shows. Washington Post. 2020. Available at: https://www.washingtonpost.com/health/almost-one-third-of-black-americans-know-someone-who-died-of-covid-19-survey-shows/2020/06/25/3ec1d4b2-b563-11ea-aca5-ebb63d27e1ff_story.html (Last accessed July9, 2020).
- 22. Silverman H, Toropin K, Sidner S, Perrot L. Navajo Nation surpasses New York state for the highest Covid-19 infection rate in the US. CNN. 2020. Available at: https://www.cnn.com/2020/05/18/us/navajo-nation-infection-rate-trnd/index.html (Last accessed July9, 2020).
- 23. Rodriguez-Diaz C, Guilamo-Ramos V, Mena L, et al. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Ann Epidemiol 2020. [preprint]. [Epub ahead of print]; DOI: 10.1016/j.annepidem.2020.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Levy V, Prentiss D, Balmas G, et al. Factors in the delayed HIV presentation of immigrants in Northern California: Implications for Voluntary Counseling and Testing Programs. J Immigrant Health 2007;9:49–54 [DOI] [PubMed] [Google Scholar]
- 25. Begley S. To understand who's dying of Covid-19, look to social factors like race more than preexisting diseases. STAT News. 2020. Available at: https://www.statnews.com/2020/06/15/whos-dying-of-covid19-look-to-social-factors-like-race (Last accessed July9, 2020).
- 26. Thomson-DeVeaux A, Cox D, Best R. Many white Americans are ready to reopen the economy. Black Americans aren't. FiveThirtyEight. 2020. Available at: https://fivethirtyeight.com/features/black-americans-were-hit-hard-by-state-shutdowns-but-are-worried-about-reopening-too (Last accessed July9, 2020).
- 27. Williams DR, Pamela BJ. Social sources of racial disparities in health. Health Aff 2005;24:325–334 [DOI] [PubMed] [Google Scholar]
- 28. Huang VS, Sutermaster S, Caplan Y, Kemp H, Schmutz D, Sgaier SK. Social distancing across vulnerability, race, politics, and employment: How different Americans changed behaviors before and after major COVID-19 policy announcements. [preprint]. medRxiv 2020. [Epub ahead of print]; DOI: 10.1101/2020.06.04.20119131 [DOI] [Google Scholar]
- 29. Farmer B. The coronavirus doesn't discriminate, but U.S. health care showing familiar biases. National Public Radio. 2020. Available at: https://www.npr.org/sections/health-shots/2020/04/02/825730141/the-coronavirus-doesnt-discriminate-but-u-s-health-care-showing-familiar-biases (Last accessed July9, 2020).
- 30. Hallfors DD, Iritani BJ, Miller WC, et al. Sexual and drug behavior patterns and HIV/STD racial disparities: The need for new directions. Am J Public Health 2007;97:125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet 2012;380:341–348 [DOI] [PubMed] [Google Scholar]
- 32. Friedman SR, Young PA, Snyder FR, et al. Racial differences in sexual behaviors related to AIDS in a nineteen city sample of street-recruited drug injectors. AIDS Ed Prev 1993;5:196–211 [PubMed] [Google Scholar]
- 33. Jaspers B. Texas cities experience disparities in access to the coronavirus testing [transcript]. National Public Radio. 2020. Available at: https://www.npr.org/2020/06/12/876293224/texas-cities-experience-disparities-in-access-to-the-coronavirus-testing (Last accessed July9, 2020).
- 34. Reid A. Coronavirus Philadelphia: Positive tests higher in poorer neighborhoods sespite six times more testing in higher-income neighborhoods, researcher says. CBS Philly. 2020. Available at: https://philadelphia.cbslocal.com/2020/04/06/coronavirus-philadelphia-positive-tests-higher-in-poorer-neighborhoods-despite-six-times-more-testing-in-higher-income-neighborhoods-researcher-says/?fbclid=IwAR1DaW1OlV5bccNW-AYdlUqFyud4DQkItg8i3IS0TdososUEU62QOrRj7WU (Last accessed July9, 2020).
- 35. Bilal U, Barber S, Diez-Roux AV. Spatial Inequities in COVID-19 outcomes in three US Cities [preprint]. medRxiv 2020. DOI: 10.1101/2020.05.01.20087833 [DOI] [Google Scholar]
- 36. Quealy K. The Richest Neighborhoods Emptied Out Most as Coronavirus Hit New York City. New York Times. May 15, 2020. Accessed July9, 2020 Available at: https://www.nytimes.com/interactive/2020/05/15/upshot/who-left-new-york-coronavirus.html
- 37. Ray KN, Chari AV, Engberg J, et al. Disparities in time spent seeking medical care in the United States. JAMA Intern Med 2015;175:1983–1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ivanova I. As states reopen, black workers are at greater risk for COVID-19. CBS News. 2020. Available at: https://www.cbsnews.com/news/black-workers-lives-essential-frontline-jobs-risk-coronavirus-reopening (Last accessed July9, 2020).
- 39. Hughes T. Poor, essential and on the bus: Coronavirus is putting public transportation riders at risk. USA Today. 2020. Available at: https://www.usatoday.com/story/news/nation/2020/04/14/public-transportation-users-risk-coronavirus-spreads-across-us/2979779001 (Last accessed July9, 2020).
- 40. Eberhart MG, Voytek CD, Hillier A, et al. Travel distance to HIV Medical Care: A geographic analysis of weighted survey data from the medical monitoring project in Philadelphia, PA. AIDS Behav 2014;18:776–782 [DOI] [PubMed] [Google Scholar]
- 41. Terzian AS, Younes N, Greenberg AE, et al. Identifying spatial variation along the HIV care continuum: The role of distance to care on retention and viral suppression. AIDS Behav 2018;22:3009–3023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Leeper C, Mugavero M, Willig J, Chamot E, Kerbawy S, Zinski A. Social determinants of late presentation to HIV Care. J Health Dispar Res Pract 2014;7:1 [Google Scholar]
- 43. Dawson L, Kates J. Insurance Coverage and Viral Suppression among People with HIV in the United States, 2015-2018. Kaiser Family Foundation 2020. Available at: https://www.kff.org/slideshow/insurance-coverage-and-viral-suppression-among-people-with-hiv-in-the-united-states-2015-2018 (Last accessed July28, 2020).
- 44. Hellinger FJ. In four ACA expansion states, the percentage of uninsured hospitalizations for people with HIV declined, 2012–14. Health Aff 2015;34:2061–2068 [DOI] [PubMed] [Google Scholar]
- 45. Wiersema A. Red state votes to expand Medicaid—Even as GOP tries to kill Obamacare amid pandemic. ABC News 2020. Available at: https://abcnews.go.com/Politics/red-state-votes-expand-medicaid-gop-kill-obamacare/story?id=71557490 (Last accessed July28, 2020).
- 46. West-Ojo T, Samala R, Griffin A, et al. Expanded HIV testing and trends in diagnoses of HIV infection—District of Columbia, 2004–2008. MMWR Morb Mortal Wkly Rep 2010;59:737–741 [PubMed] [Google Scholar]
- 47. Mandsager P, Marier A, Cohen S, Fanning M, Hauck H, Cheever LW. Reducing HIV-related health disparities in the health resources and services administration's Ryan White HIV/AIDS Program, Am J Pub Health 2018;108:S246–S250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Moore RD, Keruly JC, Bartlett JG. Improvement in the health of HIV-infected persons in care: Reducing disparities. Clin Infect Dis 2012;55:1242–1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kamarck KN. Diversity Inclusion, and Equal Opportunity in the Armed Services: Background and Issues for Congress. 2017. (CRS Report R44321). Washington, D.C.: Congressional Research Service. Available at: https://digitalcommons.ilr.cornell.edu/cgi/viewcontent.cgi?article=2968&context=key_workplace (Last accessed July28, 2020)
- 50. Stahlman S, Hakre S, Scott PT, et al. Antiretroviral therapy and viral suppression among active duty service members with incident HIV infection—United States, January 2012–June 2018. MMWR Morb Mortal Wkly Rep 2020;69:366–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wong MS, Hoggatt KJ, Steers WN, et al. Racial/ethnic disparities in mortality across the Veterans Health Administration. Health Equity 2019;3:99–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rentsch CT, Kidwai-Khan F, Tate JP, et al. Covid-19 by race and ethnicity: A national cohort study of 6 million United States veterans [preprint]. medRxiv 2020. [Epub ahead of print]; DOI: 10.1101/2020.05.12.20099135 [DOI] [Google Scholar]