Abstract
Background
General surgey is a specialty of high demand and relevance. We aimed to collect the opinions of the residents and their tutors and heads of department, regarding the impact that this COVID-19 pandemic is having - and will probably have - on the training of future general surgeons in Peru.
Methods
We conducted a cross-sectional study in Lima, Peru. We surveyed residents of general surgery, as well as their tutors and heads of surgery departments from 14 Peruvian hospitals.
Results
The impact of COVID-19 was considered severe in approximately 60% of first-year residents, 100% of second-year residents, 40% of third-year residents and about 80% of attending physicians. The 68.8% of the residents considered that the loss of surgical training opportunities during the pandemic would negatively affect their job performance. In addition, as of 03/16/2020, no residents had performed more than 25 elective surgeries, trauma surgeries or laparoscopic procedures. All the participants (including tutors and heads of departments) highlighted the need to extend the residency period.
Conclusion
The COVID-19 pandemic has affected the training of the general surgery residents. Deficiencies need to be identified in order to evaluate extending the period of the medical residency program in Peru.
Keywords: General surgery, Internship and residency, Education, Medical, COVID-19
Highlights
-
•
The COVID-19 pandemic has had a significant impact on medical education.
-
•
COVID-19 has forced rapid changes in the Peruvian Residency Training Program.
-
•
More than half of the residents considered that the loss of surgical training opportunities would negatively affect their job performance.
-
•
In Peru, as of 03/16/2020, no residents had performed more than 25 laparoscopic procedures or trauma or elective surgeries.
1. Introduction
In December 2019, the first cluster of cases of the Coronavirus disease 2019 (COVID-19) was reported [1]. Since then, its rapid spread caused a collapse of many healthcare systems worldwide [2], along with negative consequences in the economic, social and educational fields [3].
In Peru, the first confirmed case was on March 6, and on March 16, the state of emergency became official along with quarantine and social distancing measures [4]. Like other countries, there has been a negative impact in different sectors, including medical education [3,[5], [6], [7]]. In this sense, COVID-19 has forced rapid changes at both undergraduate and graduate levels, including the Residency Training Program [3]. Reduction of residents in the hospital setting, relocation to places for the management of COVID-19 patients and program withdrawals are some of the situations that have been evident in different countries [[8], [9], [10], [11]], including ours. However, no studies have yet assessed this reality in our country or its impact on the residency program.
Surgical specialties were probably the most affected during the pandemic [12]. Some procedures usually performed by residents have been postponed or canceled, including elective surgeries, interventional procedures and endoscopies [7,[13], [14], [15]]. Similarly, many surgery residents have been relocated to non-surgical units, shifting to clinical care of COVID-19 patients [[5], [6], [7]].
Because general surgery is a specialty of high demand and relevance, it is crucial to know the perspective of those protagonists who are currently in training: the residents. Likewise, we consider it pertinent to collect the opinions of their tutors and heads of department, regarding the impact that this pandemic is having - and will probably have - on the training of future general surgeons in Peru.
2. Methods
2.1. Study design and context
We conducted a cross-sectional study in Lima, Peru. Lima is the capital city and has the highest number of cases and deaths related to COVID-19 in the country. This work has been reported in line with the STROCSS criteria [16].
2.2. Population and sample
We included residents of General surgery, as well as their tutors and heads of surgery departments from 14 Peruvian hospitals. Nine of the hospitals belonged to the Ministry of Health (MINSA): Hospital Vitarte, Hospital María Auxiliadora, Hospital Nacional Arzobispo Loayza, Hospital Nacional Dos de Mayo, Hospital Carlos Lanfranco La Hoz, Hospital José Agurto Tello de Chosica, Hospital Regional de Huacho, Hospital San José del Callao and Hospital de Ventanilla. Three belonged to the Social Security (EsSalud): Hospital Nacional Guillermo Almenara Irigoyen, Hospital Edgardo Rebagliati Martins and Hospital Luis Negreiros Vega. The last two were the Hospital Central de la Policía Nacional del Perú and the Hospital Militar Central del Perú. Tutors and heads of departments were also recruited from those hospitals.
2.3. Study procedures
We developed a questionnaire to collect residents, tutors and heads of departments' perceptions of the impact of COVID-19 on the general surgery residency program. We based our questionnaire in a previous study conducted by Gupta et al. (2020), in which the perceptions of US interventional cardiology fellows were collected [7]. Initially, the adaptation of the questionnaire was conducted by the research team (a physician with a master's degree in medicine and a master's degree in epidemiological research, a physician and a bachelor of medicine (MBBS) with a background in epidemiology and scientific publishing, a hospital pharmacist with a master's degree in higher education and a general surgeon).
Initially, relevance and comprehension were assessed through a Delphi methodology. We sent the instrument by e-mail to four health professionals: a surgeon with a postgraduate degree in higher education, an epidemiologist and two heads of surgery departments. All of them chose the items of the questionnaire that they considered the most important and ranked them according to its relevance. The final questionnaire had items that were selected by the three experts. Subsequently, it was pilot-tested in a random sample of 10 surgery residents who were working in hospitals not located in Lima. Respondents were asked to score the comprehension of each item on a 5-point Likert scale ranging from 1 (“Not clear at all”) to 5 (“Completely clear”). We included items. We include those items that had a score of 4 or more.
The final questionnaire was e-mailed to general surgery residents using a snowball sampling method. Furthermore, each participant was asked to forward an e-mail invitation to other residents with an embedded anonymous survey link.
2.4. Statistical analysis
The data collected from the online survey was downloaded in a Microsoft Excel spreadsheet and codified following an independent double-typing method. The final dataset was then entered into the Stata v16.0 (StataCorp, TX, US) statistical package. For descriptive analysis, variables were presented with frequencies, percentages and graph bars. Opinions and perceptions of residents, their tutors and heads of departments were summarized as narrative statements in an independent table.
3. Results
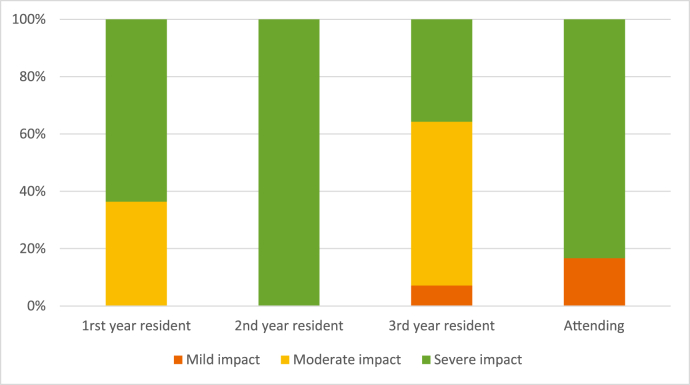
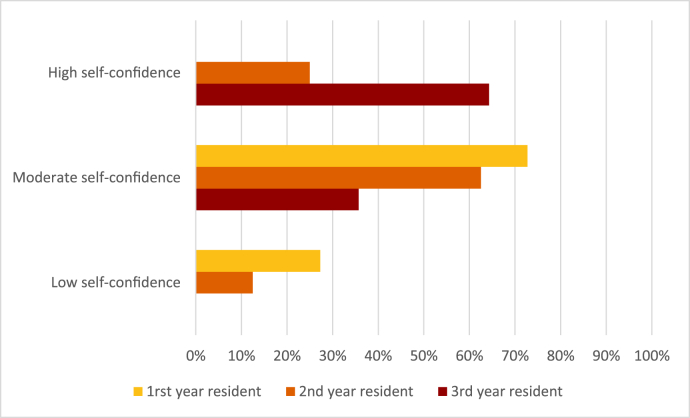
We included 32 general surgery residents, 11 were first-year residents, 8 were second-year residents and 13 were third-year residents. The impact of COVID-19 was considered severe in approximately 60% of first-year residents, 100% of second-year residents, 40% of third-year residents and about 80% of attending physicians (Fig. 1). Also, no first-year residents and only 25% of the second-year residents had high self-confidence in their surgical skills (Fig. 2).
Fig. 1.
Impact of coronavirus disease 2019 (COVID-19) pandemic on general surgery residency training according to the participants.
Fig. 2.
Level of self-confidence of being appropriately trained in surgical technique skills.
Most of the surgery residents mentioned that the impact of the COVID-19 pandemic negatively affected their training. We also surveyed six residents’ tutors and heads of departments, whose opinions regarding the impact of COVID-19 pandemic on the residents' training were divided into positive and negative aspects. They highlighted the current context as an opportunity for residents to improve their knowledge in the management of communicable diseases. However, they also pointed out that learning in surgical techniques would be limited due to pandemic, and it is needed to extend the residency period (Table 1).
Table 1.
Narrative impressions of the impact of COVID-19 on General surgery residency program.
| Comments |
|
|---|---|
| Heads of surgery departments & Tutors of residents (attending physicians) | |
| Negative statements | “The duration of the general surgery residency program is already short and often limited. During the pandemic, learning in surgical techniques has been limited. If the duration of the residency program is not extended, training will be deficient." |
| Positive statements | “Residents had to learn and deepen concepts related to communicable diseases, their management and the importance of cleaning and disinfection processes in the operating room (OR)." |
| “Taking advantage of virtual media, attending physicians have been more involved in medical resident meetings." | |
| General surgery residents | |
| Negative statements | “Training in surgical procedures and techniques has been poor during the pandemic." |
| “All surgical specialties have been affected. The duration of the residency program should be extended." | |
| “There has been a negative psychological impact of the COVID-19 pandemic on all medical residents." | |
| “Many of us had to provide medical assistance to patients with COVID-19 without adequate personal protective equipment." | |
| “The number of elective and emergency surgeries have decreased. This seriously affects our training." | |
| “At my hospital, we are not allowed to participate in surgeries. We are dedicated solely to filling medical records and preparing the patients." | |
| “The number of complex surgeries has been reduced. In addition, important rotations have been suspended, then, I consider the residency program should be extended for a minimum of four months.” | |
| Neutral statements | “Current situation evidences that we should have surgical simulation training (e.g. bench-top models, laparoscopic simulators and simulation for new surgical techniques)" |
| Positive statements | “This could be an opportunity to train us in the management of patients with communicable diseases (e.g. Covid-19) in the emergency room, operating room and in the postoperative period." |
The 68.8% of the residents considered that the loss of surgical training opportunities during the pandemic would negatively affect their job performance. Similarly, more than half of the participants mentioned that neither their hospitals nor their universities implemented a complimentary virtual training program for general surgery residents. Furthermore, 62.5% of the residents suggested extending their training after graduation. The 66.7% of the tutors of residents and heads of surgery departments suggested the same (Table 2).
Table 2.
Impact of COVID-19 Pandemic on general surgery residency training as perceived by Heads of surgery departments, tutors of residents and residents.
| Question |
n (%) |
||
|---|---|---|---|
| Heads of surgery departments & Tutors of residents | |||
| The number of emergency surgical patients has decreased? | |||
| Yes | 6 (100.0) | ||
| The number of trauma patients that need emergency surgical management has decreased? | |||
| Yes | 6 (100.0) | ||
| Lost of surgical training opportunities during the COVID-19 pandemic will negatively impact the job performance of your residents? | |||
| Yes | 5 (83.3) | ||
| No | 1 (16.7) | ||
| Suggest extending training after graduation? | |||
| Yes | 4 (66.7) | ||
| No or Uncertain | 2 (33.3) | ||
| General surgery residents | |||
| Lost of surgical training opportunities during the COVID-19 pandemic will negatively impact your job performance?* | |||
| Yes | 22 (68.8) | ||
| No or Uncertain | 10 (31.3) | ||
| Had to cancel your participation in events? (e.g., workshop, congresses, symposia or others)* | |||
| Yes | 30 (93.8) | ||
| No | 2 (6.3) | ||
| Has your hospital implemented any protocol for surgical care of patients with suspected or confirmed COVID-19?* | |||
| Yes | 22 (68.8) | ||
| No | 6 (18.8) | ||
| Don't know | 4 (12.5) | ||
| Has your hospital implemented any training protocol for the surgical team to management of suspected or confirmed surgical patients with COVID-19?* | |||
| Yes | 16 (50.0) | ||
| No | 14 (43.8) | ||
| Don't know | 2 (6.3) | ||
| Has your hospital implemented a complementary virtual tutoring or training program for General Surgery residents? | |||
| Yes | 13 (40.6) | ||
| No | 19 (59.4) | ||
| Has your university implemented a complementary virtual tutoring or training program for General Surgery residents? | |||
| Yes | 7 (21.9) | ||
| No | 25 (78.1) | ||
| Suggest extending training after graduation? | |||
| Yes | 20 (62.5) | ||
| No or Uncertain | 12 (37.5) | ||
*Percentages rounded off to one decimal may total 100.1%
The impact of COVID-19 pandemic on the residents’ participation in surgical procedures is presented in Table 3. The 34.4% performed between 26 and 100 elective surgeries before the pandemic. However, as of 03/16/2020, no residents had performed more than 25 elective surgeries. Similarly, no residents had performed more than 25 trauma surgeries or laparoscopic procedures as of this date (Table 3).
Table 3.
Impact of COVID-19 Pandemic on the participation in surgical procedures as perceived by residents.
| Question |
n (%) |
||
|---|---|---|---|
| Before 03/16/2020 | |||
| Approximately, how many elective surgeries did you perform per month? | |||
| 0–25 | 21 (65.6) | ||
| 26–50 | 6 (18.8) | ||
| 51–100 | 5 (15.6) | ||
| Approximately, how many emergency surgeries did you perform per month? | |||
| 0–25 | 25 (78.1) | ||
| 26–50 | 5 (15.6) | ||
| 51–100 | 2 (6.3) | ||
| Approximately, how many trauma surgeries did you perform per month? | |||
| 0–25 | 31 (96.9) | ||
| 26–50 | 1 (3.1) | ||
| Approximately, how many laparoscopic procedures did you perform per month?* | |||
| 0–25 | 23 (71.9) | ||
| 26–50 | 6 (18.8) | ||
| 51–100 | 3 (9.4) | ||
| As of 03/16/2020 | |||
| Approximately, how many elective surgeries had you performed? | |||
| 0–25 | 32 (100) | ||
| Approximately, how many emergency surgeries had you performed?* | |||
| 0–25 | 30 (93.8) | ||
| 26–50 | 2 (6.3) | ||
| Approximately, how many trauma surgeries had you performed? | |||
| 0–25 | 32 (100) | ||
| Approximately, how many laparoscopic procedures had you performed? | |||
| 0–25 | 32 (100) | ||
*Percentages rounded off to one decimal may total 100.1%
4. Discussion
4.1. Main findings
To our knowledge, this is the first study that evaluated the impact of COVID-19 in the training of general surgery residents, as well as the first study that included Latin American residents. The impact of COVID-19 has been reflected in a decreased number of elective surgical procedures, daily activities in the surgery department and the suspension of rotations. In consequence, the majority of residents reported that the impact of COVID-19 in their training was severe.
4.2. Comparison with other studies
Previous studies have evaluated the impact of COVID-19 in the resident's training in surgical [7,[17], [18], [19]] and clinical [20,21] specialties in the United States, Asia and Europe. However, the impact of the pandemic has not been evaluated in general surgery residents, who have suffered notably as well as other surgical specialty residents. In this study, we found a decrease in the number of elective surgical procedures performed by residents during the pandemic, also described in previous studies including residents of interventional cardiology [7], urology [17], neurosurgery [19], plastic surgery, which would affect the development of necessary skills in their training as future attending physicians. It is important to consider alternatives and solutions, especially because many of the laparoscopic procedures are considered standards and there are currently international recommendations to perform them safely.
Previous studies have described the changes produced in daily activities of general surgery residents due to the pandemic, such as a reduction in the number of elective surgeries, the implementation of protocols in hospitals to prevent physicians from getting COVID-19, as well as modifications in the triage system of the surgical patient [22,23]. However, no studies have evaluated the impact of the pandemic on reducing the surgical procedures of general surgery residents, which would affect their training, self-confidence and subsequent job performance. This situation is evidenced in our findings, in which both the Heads of surgical departments and residents’ tutors considered that the negative impact produced by the pandemic would affect their abilities as specialists.
4.3. Relevance and implications
Due to the decrease in activities in surgical departments, residents have been reassigned in other services with a higher COVID-19 patients’ affluence, such as the emergency room or intensive care unit (ICU) [24,25]. This would make it difficult for residents to complete the minimum number of procedures they are asked to perform at the end of each yearly program and would affect their future performance [7]. Accordingly, the residents' opinions included in this study showed their concern over the decrease in procedures carried out after the establishment of the Peruvian state of emergency, and their desire to extend the residency program. However, the National Council of Medical Residents (CONAREME, for its initials in Spanish), the entity that regulates the training of medical residents, has not made any statement regarding their current situation.
Due to quarantine, universities have suspended their presential activities; therefore, the residents’ education has been affected. Given this situation, virtual educational sessions have been implemented in other countries. These sessions consist of discussion of clinical cases, review of specialty related articles and the use of surgical procedures simulators to improve the residents' education outside the hospital [21,26,27]. However, virtual learning in surgical education is very limited in Peru, and evidence of this is that the majority of residents reported not having educational sessions by the university or the surgery department staff during the COVID-19 pandemic. Furthermore, due to the state of sanitary emergency, residency rotations have been suspended, which are essential to strengthen medical skills in other fields related to the specialty of interest [28]. For this reason, in previous studies, it has been suggested to extend the period of medical residency to recover the pending rotations [17], which agrees with the residents' opinions described in the present study. This situation could enhance the self-confidence perception of their capacities as future specialists.
4.4. Limitations
This study has some limitations: 1) The results were obtained from the voluntary responses of the residents evaluated, for which there could be voluntary response bias; 2) We used a non-probabilistic sampling, then, the results obtained could not be extrapolated to the population of surgery residents in Peru; however, this is the first report that has evaluated the impact of the COVID-19 pandemic in general surgery residents' training; 3) The questionnaire used does not constitute a previously validated scale; however, it went through experts’ validation and pilot-tested.
5. Conclusion
The COVID-19 pandemic has affected the training of the residents, especially those with surgical specialties. Training outside the hospital should be reinforced through virtual tools along with the support of universities and surgical department staff. Moreover, the primary deficiencies in the residents' training after the pandemic should be identified to evaluate extending the period of the medical residency program in Peru.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Funding
None to declare (This study was self-funded).
Ethical approval
The Institutional Review Board of the Instituto de Evaluación de Tecnologías en Salud e Investigación (IETSI) - EsSalud approved this study (N° 42-IETSI-ESSALUD-2020).
Research registration unique identifying number (UIN)
1. Name of the registry: Registro de Proyectos de Investigación en Salud (PRISA) A repository of the instituto Nacional de Salud del Perú (Peruvian National Institute of Health).
2. Unique Identifying number or registration ID: EI00000001433.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.ins.gob.pe/prisa/ver_investigacion.aspx?342FB929-131D-4C0E-AFAC-B2A2EB8ECF3F.
Author contribution
Carlos J. Toro-Huamanchumo, Paola K. Rodrigo-Gallardo and Medalit E. Huamanchumo-Suyon provided the idea and analysis of data. Pedro J. Ruiz-Perez and Diego Urrunaga-Pastor collected the data. All the authors discussed the results, critically commented on the manuscript at all stages, and prepared and approved its final version.
Guarantor
Carlos J. Toro-Huamanchumo.
Declaration of competing interest
None to declare.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2020.10.031.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bedford J., Enria D., Giesecke J., Heymann D.L., Ihekweazu C., Kobinger G. COVID-19: towards controlling of a pandemic. Lancet. 2020;395(10229):1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herrera-Añazco P., Toro-Huamanchumo C.J. Educación médica durante la pandemia del COVID-19: iniciativas mundiales para el pregrado, internado y el residentado médico. Acta Méd. Peru. 2020;37(2):169–175. [Google Scholar]
- 4.Presidente de la República, Decreto Supremo N 044-2020-PCM . Perú: El Peruano; Lima: 2020. Decreto Supremo que declara Estado de Emergencia Nacional por las graves circunstancias que afectan la vida de la Nación a consecuencia del brote del COVID-19. [Google Scholar]
- 5.Clark V.E. Impact of COVID-19 on neurosurgery resident research training. J. Neurosurg. 2020:1–2. doi: 10.3171/2020.4.JNS201034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amparore D., Claps F., Cacciamani G.E., Esperto F., Fiori C., Liguori G. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol. Nefrol. 2020 doi: 10.23736/S0393-2249.20.03868-0. [DOI] [PubMed] [Google Scholar]
- 7.Gupta T., Nazif T.M., Vahl T.P., Ahmad H., Bortnick A.E., Feit F. Impact of the COVID‐19 pandemic on interventional cardiology fellowship training in the New York metropolitan area: a perspective from the United States epicenter. Cathet. Cardiovasc. Interv. 2020 doi: 10.1002/ccd.28977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maguiña-Vargas C. Reflexiones sobre el COVID-19, el Colegio Médico del Perú y la Salud Pública. Acta Méd. Peru. 2020;37(1):8–10. [Google Scholar]
- 9.Scullen T., Mathkour M., Maulucci C.M., Dumont A.S., Bui C.J., Keen J.R. Impact of the COVID-19 pandemic on neurosurgical residency training in new orleans. World Neurosurg. 2020;139:718–719. doi: 10.1016/j.wneu.2020.04.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khosravi M.H., Sisakht A.M., Kiani D., Ahmadi S. Effects of covid-19 pandemic on neurological surgery care and education; our experience from Iran. World Neurosurg. 2020;139:376. doi: 10.1016/j.wneu.2020.05.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potts J.R. Residency and fellowship program accreditation: effects of the novel coronavirus (COVID-19) pandemic. J. Am. Coll. Surg. 2020;230(6):1094–1097. doi: 10.1016/j.jamcollsurg.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brindle M.E., Gawande A. Managing COVID-19 in surgical systems. Ann. Surg. 2020;272(1):e1–e2. doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maffia F., Fontanari M., Vellone V., Cascone P., Mercuri L.G. Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int. J. Oral Maxillofac. Surg. 2020;49(6) doi: 10.1016/j.ijom.2020.04.015. 827-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gralnek I.M., Hassan C., Dinis-Ribeiro M. COVID-19 and endoscopy: implications for healthcare and digestive cancer screening. Nat. Rev. Gastroenterol. Hepatol. 2020;17(8):444–446. doi: 10.1038/s41575-020-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.gha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Khusid J.A., Weinstein C.S., Becerra A.Z., Kashani M., Robins D.J., Fink L.E. Well‐being and education of urology residents during the COVID‐19 pandemic: results of an American national survey. Int. J. Clin. Pract. 2020:e13559. doi: 10.1111/ijcp.13559. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pelargos P.E., Chakraborty A., Yan D.Z., Smith Z.A., Dunn I.F., Bauer A.M. An evaluation of neurosurgical resident education and sentiment during the COVID-19 pandemic: a north American survey. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kapila A.K., Schettino M., Farid Y., Ortiz S., Hamdi M. The impact of COVID-19 on plastic surgery training: a representative perspective from residents. Plast. Reconstr. Surg. 2020 doi: 10.1097/GOX.0000000000003054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marasco G., Nardone O.M., Maida M., Boskoski I., Pastorelli L., Scaldaferri F. Impact of COVID-19 outbreak on clinical practice and training of young gastroenterologists: a European Survey. Dig. Liver Dis. 2020 doi: 10.1016/j.dld.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Odedra D., Chahal B.S., Patlas M.N. Impact of COVID-19 on Canadian radiology residency training programs. Can. Assoc. Radiol. J. 2020 doi: 10.1177/0846537120933215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He K., Stolarski A., Whang E., Kristo G. Addressing General Surgery residents' concerns in the early phase of the COVID-19 pandemic. J. Surg. Educ. 2020;77(4):735–738. doi: 10.1016/j.jsurg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferrario L., Maffioli A., Bondurri A.A., Guerci C., Lazzarin F., Danelli P. COVID-19 and surgical training in Italy: residents and young consultants perspectives from the battlefield. Am. J. Surg. 2020 doi: 10.1016/j.amjsurg.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meneses E., McKenney M., Elkbuli A. Reforming our general surgery residency program at an urban level 1 Trauma Center during the COVID-19 pandemic: towards maintaining resident safety and wellbeing. Am. J. Surg. 2020 doi: 10.1016/j.amjsurg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nassar A.H., Zern N.K., McIntyre L.K., Lynge D., Smith C.A., Petersen R.P. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the University of Washington experience. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.1219. [DOI] [PubMed] [Google Scholar]
- 26.Ricciardi G., Biondi R., Tamagnini G. Go back to the basics: cardiac surgery residents at the time of COVID‐19. J. Card. Surg. 2020;35(7):1400–1402. doi: 10.1111/jocs.14680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKechnie T., Levin M., Zhou K., Freedman B., Palter V., Grantcharov T.P. Virtual surgical training during COVID-19: operating room simulation platforms accessible from home. Ann. Surg. 2020;272(2):e153–e154. doi: 10.1097/SLA.0000000000003999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernardi L., Germani P., Del Zotto G., Scotton G., de Manzini N. Impact of COVID-19 pandemic on general surgery training program: an Italian experience. Am. J. Surg. 2020 doi: 10.1016/j.amjsurg.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.