Abstract
Background and objectives
Growing evidence indicates that the nurse navigator-pivot (NN)*, is key to optimizing care processes and outcomes. However, large scale studies are needed to examine how patients exposed to NNs (as opposed to non-NN) differentially perceived their cancer care experiences.
Method
Participants (N = 2,858) treated for cancer in the last six months at university-affiliated cancer centres in Montréal, Québec, completed the Ambulatory Oncology Patient Satisfaction Survey (AOPSS).
Results
Cancer care experiences and satisfaction were significantly higher in the NN group (n = 2,003) for all six care domains (Ds from 3.32 to 8.95) and all four nursing functions (Ds from 5.64 to 10.39) when compared to the non-NN group (n = 855).
Discussion
The NN role is significantly related to enhanced cancer care experiences and higher patient satisfaction. Future research should explore potential causal effects between NNs and care processes, as well as patient outcomes.
Keywords: cancer, oncology, nurse navigator, nurse pivot, patient satisfaction, patient cancer care experiences
INTRODUCTION
A diagnosis of cancer and its treatment can be an over-whelming, life-changing experience that brings a host of emotions including fear, uncertainty, and distress, as well as an array of physical and social challenges (Canadian Cancer Society, 2018; Fenn et al., 2014; Meeker et al., 2016; Canadian Partnership Against Cancer, 2018). Individuals with cancer often report various unmet needs (Canadian Partnership Against Cancer [CPAC], 2018) and in response to these needs and challenges, person-centred care (PCC) is now part of routine clinical practice (Institute of Medicine [US] Committee on Approaching Death, 2015; Moody et al., 2018; CPAC, 2010; Robinson et al., 2008). PCC, defined as respectful, responsive and tailored approaches that meet patients’ needs and preferences, provides benefits such as improvement in the quality of patient care and higher patient satisfaction (Finney-Rutten et al., 2012; Kullberg et al., 2017; Loiselle et al., 2019; Westphal, 2016).
To adequately fulfil PCC’s goals, a key member of the multidisciplinary team is the nurse navigator (NN), also called nurse pivot in Québec (Koh et al., 2011; Yatim et al., 2017; Zibrik et al., 2016). NNs are now considered essential members of the oncology multidisciplinary team and their role includes four main functions: assessing patient needs, providing education and information, supporting patients and family members, and coordinating care (Lévesque-Boudreau & Champagne, 2008). Often, NNs readily connect patients to support services, help them overcome potential healthcare system barriers to access, as well as provide timely health education and support (Yatim et al., 2017; Zibrik et al., 2016; Cook et al., 2013; Shockney, 2015). Moreover, NNs often act as liaison agents with cancer care team members. As such, stakeholders in cancer care around the world acknowledge the key role that NNs play in optimizing PCC and health-related outcomes (Fillion et al., 2009; Lee et al., 2011; Tariman & Szubski, 2015; McMullen, 2013). Despite the importance of the NN within the care team (Tho & Ang, 2016; Case, 2011), more evidence is needed from the perspective of care recipients. Herein, with a survey design, we sought to document potential significant relationships between NN assignment and patient cancer care experiences and satisfaction.
More specifically, the main goals of this study were to:
Report on participants’ cancer care experiences and satisfaction according to their perceptions of being assigned a NN (or not).
Compare NN/non-NN groups across the AOPSS’s six cancer care domains: (1) emotional support, (2) coordination and continuity of care, (3) respect for patient preferences, (4) physical comfort, (5) information, communication and education, and (6) access to care; as well as four main nursing functions (i.e., assessment, education, support and coordination, as per Lévesque-Boudreau & Champagne, 2008) that we established by clustering relevant AOPSS items.
MATERIALS AND METHODS
Sample
The sample consisted of all patients with diverse cancer diagnoses who had been treated for cancer within the last six months. Out of 7,885 surveys mailed to eligible patients, 3,278 completed surveys were returned. Of these, 2,858 answered the NN assignment item (2,003 reported being assigned a NN and 855 did not). More specifically, inclusion criteria were being aged 18 years or older, having a confirmed cancer diagnosis and being treated (e.g., surgery, chemotherapy, and/or radiotherapy) as an outpatient in the participating cancer centres.
Setting
Three university-affiliated hospitals with integrated cancer centres in Montreal, Québec, took part in the study: (1) the Segal Cancer Centre at the Jewish General Hospital, (2) the Cedars Cancer Centre at the McGill University Health Centre, and (3) the Cancer Centre at St. Mary’s Hospital. The Rossy Cancer Network (https://www.mcgill.ca/rcr-rcn) worked closely with Ambulatory Oncology Patient Satisfaction Survey (AOPSS) license holders (NRC Picker) to facilitate survey administration including distribution and compilation of responses.
Design
A self-report survey was used to examine relationships between participants’ perceptions of being assigned a NN (or not) and cancer care experiences and patient satisfaction with care.
Procedures
As part of an ongoing quality improvement initiative, an institutional quality council, comprised of representatives from each of the cancer centres, provided oversight of the quality improvement study. Potential participants were randomly selected using hospital mailing lists that filtered out patient records that did not meet inclusion criteria. Every three months, a new wave of surveys was mailed to eligible participants. The survey package included a cover letter, the AOPSS with five additional items and a pre-paid postage return envelope. Participants were told that a mailed back completed survey (sent to NRC Picker) indicated voluntary consent to take part in the study. A follow-up letter and survey were sent again, approximately four weeks later, if no prior completed survey was received. Consistent with Québec’s privacy laws, no personally identifiable information was collected.
Measures
The Ambulatory Oncology Patient Satisfaction Survey (AOPSS) is a standardized self-report measure used in healthcare facilities across North America and elsewhere (National Research Corporation, 2003; Ferguson, 2012). The 83-item survey includes questions pertaining to patient experience and satisfaction with 45 core questions mapped to six care domains: (1) emotional support, (2) coordination and continuity of care, (3) respect for patient preferences, (4) physical comfort, (5) information, communication, and education, and (6) access to care. Five additional items were added, including two pertaining to the NN:
When you were diagnosed with cancer, was a specific nurse assigned to you to follow you over time? i.e., a pivot nurse or a primary nurse? (Yes, No, or I don’t know).
If yes, how useful was this nurse? Please circle the most appropriate number on this scale, from 1 (Not at all useful) to 7 (Extremely useful).
Statistical Analysis
All analyses were performed using SAS, Version 9.4 for Windows (SAS Institute Inc., 2013). AOPSS items were grouped according to each of the validated six care domains (Cronbach’s alphas ranged from 0.79 to 0.93) (National Research Corporation, 2003), including access to care (seven items), coordination (eight items), physical comfort (five items), emotional support (eight items), information (10 items), and respect for patients’ preferences (six items). We also grouped particular AOPSS items according to four previously established key nursing functions: patient assessment (five items), education (28 items), support (11 items), and coordination (six items). Participants’ satisfaction was assessed by comparing NN versus non-NN ratings across the six care domains and four NN functions using a two-step analytic procedure. First, the percentage of positive ratings to questions constituting each care domain and each NN function were calculated for each participant by adapting the NRC Picker methodology, where only the most positive answers contribute to the calculation: “Yes, completely” for an item with three choices (Yes completely, Yes somewhat, and No) or “Always” for an item with four potential responses (Never, Sometimes, Usually, and Always; Sizmur, 2012). Then, the aggregated ratings for care domains and NN functions were computed as averages for those percentages. Statistical adjustment for multiple tests was performed by using the Bonferroni correction method. Results were statistically significant if the confidence interval (CI) did not include the null hypothesis value (Joseph & Reinhold, 2005). Results were reported as mean group difference (D) with 99% CI.
RESULTS
Descriptive Statistics for NN and Non-NN Groups
Of the 7,885 study packages mailed to potential participants, 3,278 returned completed surveys (representing a 41% response rate). More than half of participants were female (59%) and half were aged 65 or older (51%). Nearly a third of participants reported having breast cancer (29%). Of the 2,858 participants who completed the NN assignment item, 2,003 (70%) reported being assigned a dedicated nurse or NN and 855 (30%) reported that they did not.
Table 1 shows participant sociodemographic characteristics according to NN and non-NN groups. Of note, participants with head and neck cancers were more likely to report being assigned a NN (87%) with the lowest percentage noted for prostate/testicular cancers (58%).
Table 1.
Participant characteristics according to total sample, non-NN and NN-groups
| Total N = 2858 | % | Non-NN n = 855 | % | NN n = 2003 | % | |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 1096 | 38.4 | 337 | 39.4 | 759 | 37.9 |
| Female | 1712 | 59.9 | 505 | 59.1 | 1207 | 60.3 |
| Missing | 50 | 1.7 | 13 | 1.5 | 37 | 1.8 |
| Age | ||||||
| 18–44 years | 164 | 5.7 | 45 | 5.3 | 119 | 5.9 |
| 45–54 years | 429 | 15.0 | 106 | 12.4 | 323 | 16.1 |
| 55–64 years | 775 | 27.1 | 199 | 23.3 | 576 | 28.8 |
| 65–74 years | 868 | 30.4 | 266 | 31.1 | 602 | 30.1 |
| 75+ years | 588 | 20.6 | 234 | 27.4 | 354 | 17.7 |
| Missing | 34 | 1.2 | 5 | 0.6 | 29 | 1.4 |
| Cancer Diagnosis | ||||||
| Breast | 839 | 29.4 | 267 | 31.2 | 572 | 28.6 |
| Hematology/Lymphoma | 397 | 13.9 | 112 | 13.1 | 285 | 14.2 |
| Melanoma/Sarcoma/Stomach/Brain | 354 | 12.4 | 104 | 12.2 | 250 | 12.5 |
| Colorectal/Bowel | 345 | 12.1 | 72 | 8.4 | 273 | 13.6 |
| Lung | 252 | 8.8 | 64 | 7.5 | 188 | 9.4 |
| Cervix/Uterine/Ovarian | 186 | 6.5 | 34 | 4.0 | 152 | 7.6 |
| Prostate/testicular | 165 | 5.8 | 96 | 11.2 | 69 | 3.4 |
| Head/Neck | 77 | 2.7 | 10 | 1.2 | 67 | 3.3 |
| Kidney/bladder | 87 | 3.0 | 51 | 6.0 | 36 | 1.8 |
| Missing | 156 | 5.4 | 45 | 5.3 | 111 | 5.5 |
Results Pertaining to the Six Cancer Care Domains
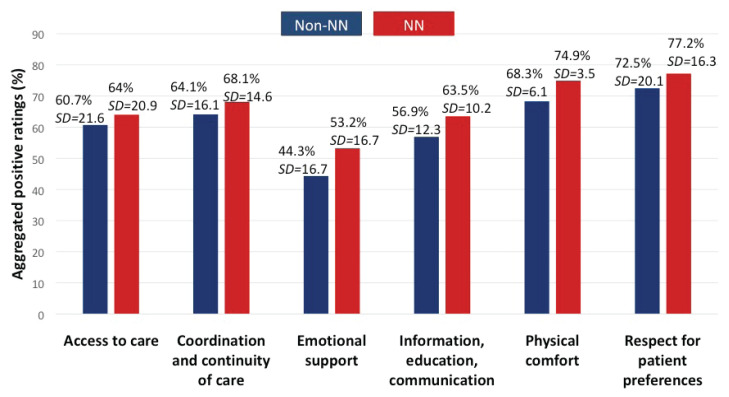
Complete data were available for 45% to 99% of all care domains. This was consistent across NN and non-NN groups. Compared to the non-NN group, participants with a perceived NN assignment gave higher positive ratings on all six care domains (Figure 1). The mean differences of the aggregated positive ratings between NN and Non-NN showed that emotional support had the highest difference (D = 8.95; 99% CI [7.19, 10.71]), followed by information, education, and communication (D = 6.60; 99% CI [5.37, 7.83]), physical comfort (D = 6.56; 99% CI [5.98, 7.14]), respect for patient (D = 4.70; 99% CI [2.69, 6.71]), and coordination (D = 4.02; 99% CI [2.37, 5.67]). The lowest difference was for access to care (D = 3.32; 99% CI [1.07, 5.57]). For both groups, respect for patients’ preferences had the highest ratings, whereas emotional support had the lowest ratings (Figure 1). Across all six care domains, positive ratings were, on average, 6% higher in the NN group.
Figure 1.
Percentages of positive ratings for the six domains of care according to non-NN (n = 855) and NN (n = 2,003) groups
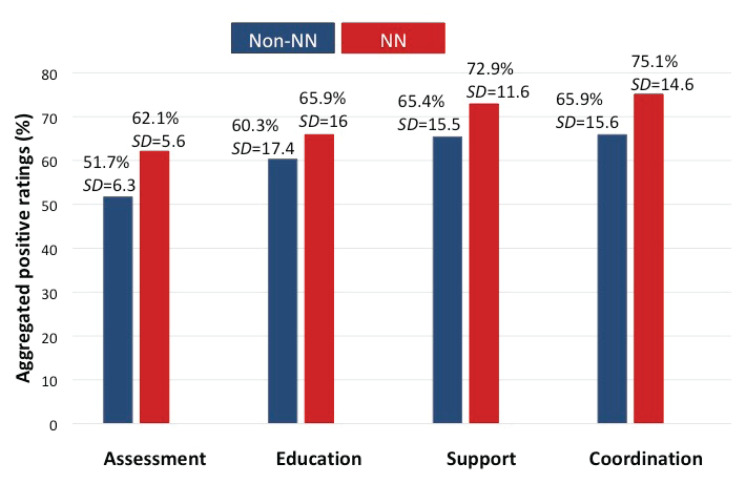
Results Pertaining to the Four Nursing Functions
Forty to 99% of complete data were available for calculating ratings across nursing functions. The NN group reported significantly higher ratings for all four nursing functions when compared to the non-NN group (Figure 2). The highest differences were for assessment (D = 10.39; 99% CI [9.78, 11.00]), followed by coordination (D = 9.23; 99% CI [7.62, 10.84]), support (D = 7.58, 99% CI [6.06, 9.10]), and education (D = 5.64, 99% CI [3.85, 7.43]). In the NN group, 83.5% reported the NN role to be “very” to “extremely useful.” For both groups, coordination had the highest ratings and assessment had the lowest ratings (Figure 2). Across all nursing domains, positive ratings were on average 8% higher for the NN group compared to the non-NN group.
Figure 2.
Percentages of positive ratings for the four nursing functions according to non-NN (n = 855) and NN (n = 2,003) groups
DISCUSSION
The goal of the present study was to document how perceived presence of NNs relates to cancer care experiences and patient satisfaction with care in three university-affiliated cancer centres. Participants in the NN group (compared to non-NN) were significantly more satisfied with all care domains and nursing functions. Whereas one other study reported higher patient satisfaction for cancer care domains when a nurse pivot/navigator is assigned (Dubé-Linteau, 2014), we contributed further by using confidence intervals and identifying key nursing functions and how these vary according to groups. We consistently found significantly higher ratings in the NN group. The largest differences between groups were in the emotional support domain with the NN group reporting higher satisfaction also corroborated by a Québec-wide survey (Dubé-Linteau, 2014). Emotional support includes being told of the cancer diagnosis in a sensitive manner, put in touch with other care providers who could help with anxieties and fears, receiving enough information on possible changes in emotions, sexual activities and relationship with their spouse or partner, and if care providers went out of their way to help patients feel better. Others have documented that emotional support remains the most frequent unmet need (Wang et al., 2018; Deshields et al., 2012), despite being considered an essential component of PCC (Wang et al., 2018). The NN seems particularly relevant in this area, as it readily addresses patients’ concerns while encouraging them to openly express emotions (Hébert & Fillion, 2011). A randomized controlled trial in the U.S. also demonstrated the positive influence of NNs and how patients felt more supported emotionally when compared to the usual care group (Wagner et al., 2014). Likewise, an improvement project aimed at evaluating the effectiveness of a breast cancer nurse navigator program reported that 98% of participants (n = 136) felt emotionally supported by the NN (Trevillion et al., 2015). Moreover, in our study, NNs were reported to be highly valuable with 83.5% of participants rating them “very” to “extremely useful”. This finding is in line with a previous study whereby 98% of participants valued the continuous guidance of a designated oncology nurse navigator (Hryniuk et al., 2014).
Among the four NN functions, patient assessment showed the lowest ratings, which might be explained by the complexity of assessment/evaluation activities in cancer care (Hébert & Fillion, 2011; Hryniuk et al., 2014; Fournier et al., 2015). In response to existing gaps in assessment (e.g., oncology referrals, delays in treatment), a pilot study by Zibrik et al. (2016) tested the benefit of the NN integration into the triage process for patients with cancer and found that early NN care involvement improved timely patient assessment, resource utilization and optimal treatment delivery.
CONCLUSIONS
The present findings provide much-needed large-scale evidence that the NN role is significantly related to more positive cancer experiences and higher patient satisfaction with care. Future studies should rely on more robust designs to systematically document potential causal effects between NNs and care processes, as well as patient outcomes.
Study Limitations
Because of its correlational nature, findings must be interpreted with caution. Also, the study groups (being assigned a NN or not) relied on participants’ self-report rather than objective documentation. Participants were asked to rate the quality of events that took place within the last six months, therefore potentially introducing recall bias.
Clinical Implications
To our knowledge, in addition to using more rigorous strategy to establish statistical importance through confidence intervals, this is the first study to compare patient satisfaction according to evidence-based nursing functions.
Various stakeholders in healthcare are increasingly committed to documenting whether specific professional roles and interventions make a significant difference clinically (i.e., above and beyond statistical significance) (Fethney, 2010; Griffiths et al., 2019). Herein, we provide further support for the clinical importance of NNs. If corroborated by future studies, these findings should serve to inform decisions about human resource allocation in cancer care.
ACKNOWLEDGMENT
We are indebted to the participants who took the time to complete study materials. We thank the Rossy Cancer Network and the three participating cancer centres for providing logistic and financial support for the conduct of this study. As Chair Recipient, CGL acknowledges financial support for her program of research through the Christine and Herschel Victor/Hope & Cope Research Chair in Psychosocial Oncology based at McGill University. SA is receiving a Hope & Cope doctoral fellowship. PSC and DT are supported by a FRQ-S Junior 1 research career award.
Footnotes
NN includes both terms: nurse navigator and nurse pivot
AUTHOR CONTRIBUTIONS
Conception and design: Carmen G. Loiselle, Samar Attieh, Caroline Rousseau
Data analysis: Doneal Thomas, Samar Attieh, Carmen G. Loiselle
Data analysis revisions and suggestions: Paramita Saha-Chaudhuri, Denis Talbot, Doneal Thomas, Samar Attieh, Carmen G. Loiselle
Manuscript writing: Carmen G. Loiselle and Samar Attieh
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
CONFLICT OF INTEREST
No conflict of interest to declare.
REFERENCES
- Canadian Cancer Society. Emotions and cancer [Internet] Toronto (ON): 2018. Nov 22, Available from http://www.cancer.ca/en/cancer-information/cancerjourney/recently-diagnosed/emotions-andcancer/?region=on. [Google Scholar]
- Canadian Partnership Against Cancer. Virtual navigation in cancer: A pilot study. Toronto: Author; 2010. [Google Scholar]
- Canadian Partnership Against Cancer. The 2014 Cancer System Performance Report. Toronto: Author; 2014. [Google Scholar]
- Canadian Partnership Against Cancer. Living with cancer: A report on the patient experience. Toronto: Author; 2018. [Google Scholar]
- Case MA. Oncology nurse navigator: Ensuring safe passage. Clin J Oncol Nurs. 2011;15(1):33. doi: 10.1188/11.CJON.33-40. [DOI] [PubMed] [Google Scholar]
- Cook S, Fillion L, Fitch MI, Veillette AM, Matheson T, Aubin M, de Serres M, Doll R, Rainville F. Core areas of practice and associated competencies for nurses working as professional cancer navigators. Can Oncol Nurs J. 2013;23(1):44–52. doi: 10.5737/1181912x2314452. [DOI] [PubMed] [Google Scholar]
- Deshields TL, Rihanek A, Potter P, Zhang Q, Kuhrik M, Kuhrik N, O’Neill J. Psychosocial aspects of caregiving: Perceptions of cancer patients and family caregivers. Supportive Care in Cancer. 2012;20(2):349–56. doi: 10.1007/s00520-011-1092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé-Linteau A. Enquête québécoise sur la qualité des services de lutte contre le cancer. L’infirmière pivot en oncologie et l’expérience patient. Québec: Institut de la statistique du Québec; 2014. [Google Scholar]
- Fenn KM, Evans SB, McCorkle R, DiGiovanna MP, Pusztai L, Sanft T, Hofstatter EW, Killelea BK, Knobf MT, Lannin DR, Abu-Khalaf M. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract. 2014;10(5):332–8. doi: 10.1200/JOP.2013.001322. [DOI] [PubMed] [Google Scholar]
- Ferguson D. Validation of the NRC Picker Canada Ambulatory Oncology Patient Satisfaction Survey. Ontario: NRC Picker Canada; 2012. [Google Scholar]
- Fethney J. Statistical and clinical significance, and how to use confidence intervals to help interpret both. Australian Critical Care. 2010;23(2):93–7. doi: 10.1016/j.aucc.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Fillion L, de Serres M, Cook S, Goupil RL, Bairati I, Doll R. Professional patient navigation in head and neck cancer. Semin oncol nurs. 2009;25(3):212–221. doi: 10.1016/j.soncn.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Finney-Rutten LJ, Davis T, Beckjord EB, Blake K, Moser RP, Hesse BW. Picking up the pace: Changes in method and frame for the health information national trends survey (2011–2014) J Health Commun. 2012;17(8):979–89. doi: 10.1080/10810730.2012.700998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier B, Simard S, Veillette AM, Fillion L. An integrative framework to support the assessment function of Québec’s pivot nurses in oncology. Can Oncol Nurs J. 2015;25(3):335–40. [Google Scholar]
- Griffiths P, Needleman J. Statistical significance testing and p-values: Defending the indefensible? A discussion paper and position statement. International journal of nursing studies. 2019;99:1033–84. doi: 10.1016/j.ijnurstu.2019.07.001. [DOI] [PubMed] [Google Scholar]
- Hébert J, Fillion L. Gaining a better understanding of the support function of oncology nurse navigators from their own perspective and that of people living with cancer: Part 1 & 2. Can Oncol Nurs J. 2011;21(1):33–38. doi: 10.5737/1181912x2113338. [DOI] [PubMed] [Google Scholar]; 21(2):114–21. [Google Scholar]
- Hryniuk W, Simpson R, McGowan A, Carter P. Patient perceptions of a comprehensive cancer navigation service. Current Oncology. 2014;21(2):69. doi: 10.3747/co.21.1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Approaching Death: Addressing Key End-of-Life Issues. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington: National Academies Press; 2015. [PubMed] [Google Scholar]
- Joseph L, Reinhold C. Fundamentals of clinical research for radiologists: Statistical inference for continuous variables. AJR. 2005;184:1047–56. doi: 10.2214/ajr.184.4.01841047. [DOI] [PubMed] [Google Scholar]
- Koh C, Nelson JM, Cook PF. Evaluation of a patient navigation program. Clin J Oncol Nurs. 2011;15(1) doi: 10.1188/11.CJON.41-48. [DOI] [PubMed] [Google Scholar]
- Kullberg A, Sharp L, Johansson H, Brandberg Y, Bergenmar M. Patient satisfaction after implementation of person-centred handover in oncological inpatient care–A cross-sectional study. PloS one. 2017;12(4):e0175397. doi: 10.1371/journal.pone.0175397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee T, Ko I, Lee I, Kim E, Shin M, Roh S, Yoon D, Choi S, Chang H. Effects of nurse navigators on health outcomes of cancer patients. Cancer Nurse. 2011;34(5):376–84. doi: 10.1097/NCC.0b013e3182025007. [DOI] [PubMed] [Google Scholar]
- Lévesque-Boudreau D, Champagne M. Ministère de la Santé et des Services sociaux. Rôle de l’infirmière pivot en oncologie. Direction de la lutte contre le cancer. 2008. Available from http://www.msss.gouv.qc.ca/inc/documents/ministere/lutte-contre-le-cancer/role-infirmiere-pivot_juil2008.pdf.
- Loiselle CG, Howell D, Nicoll I, Fitch M. Toward the development of a comprehensive cancer experience measurement framework. Supportive Care in Cancer. 2019;27(7):2579–2589. doi: 10.1007/s00520-018-4529-y. [DOI] [PubMed] [Google Scholar]
- McMullen L. Oncology nurse navigators and the continuum of cancer care. Semin oncol nurs. 2013;29(2):105–117. doi: 10.1016/j.soncn.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Meeker CR, Geynisman DM, Egleston BL, Hall MJ, Mechanic KY, Bilusic M, Plimack ER, Wong YN. Relationships among financial distress, emotional distress, and overall distress in insured patients with cancer. J Oncol Pract. 2016;12(7):e755–64. doi: 10.1200/JOP.2016.011049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody L, Nicholls B, Shamji H, Bridge E, Dhanju S, Singh S. The person-centred care guideline: From principle to practice. Journal of Patient Experience. 2018;4 doi: 10.1177/2374373518765792. 2374373518765792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Corporation. Development and Validation of the Picker Ambulatory Oncology Survey Instrument in Canada. Lincoln, NE: Author; 2003. [Google Scholar]
- Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: Definitions and applications to improve outcomes. Journal of the American Academy of Nurse Practitioners. 2008;20(12):600–7. doi: 10.1111/j.1745-7599.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. Base SAS® 9.4 Procedures Guide: High-Performance Procedures. 2nd ed. Cary NC: Author; 2013. [Google Scholar]
- Shockney LD. The evolution of breast cancer navigation and survivorship care. The Breast Journal. 2015;21(1):104–10. doi: 10.1111/tbj.12353. [DOI] [PubMed] [Google Scholar]
- Sizmur S. The reliability of trust-level survey scores: A comparison of three different scoring models. Picker Institute Europe; 2012. [Google Scholar]
- Tariman JD, Szubski KL. The evolving role of the nurse during the cancer treatment decision-making process: A literature review. Clin J Oncol Nurs. 2015;19(5) doi: 10.1188/15.CJON.548-556. [DOI] [PubMed] [Google Scholar]
- Tho PC, Ang E. The effectiveness of patient navigation programs for adult cancer patients undergoing treatment: A systematic review. JBI database of systematic reviews and implementation reports. 2016;14(2):295–321. doi: 10.11124/jbisrir-2016-2324. [DOI] [PubMed] [Google Scholar]
- Trevillion K, Singh-Carlson S, Wong F, Sherriff C. An evaluation report of the nurse navigator services for the breast cancer support program. Canadian Oncology Nursing Journal/Revue canadienne de soins infirmiers en oncologie. 2015;25(4):409–14. doi: 10.5737/23688076254409414. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Ludman EJ, Bowles EJ, Penfold R, Reid RJ, Rutter CM, Chubak J, McCorkle R. Nurse navigators in early cancer care: A randomized, controlled trial. J Clin Oncol. 2014;32(1):12. doi: 10.1200/JCO.2013.51.7359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T, Molassiotis A, Chung BP, Tan JY. Unmet care needs of advanced cancer patients and their informal caregivers: A systematic review. BMC Palliative Care. 2018;17(1):96. doi: 10.1186/s12904-018-0346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westphal EC, Alkema G, Seidel R, Chernof B. How to get better care with lower costs? See the person, not the patient. J Am Geriatr Soc. 2016;64(1):19–21. doi: 10.1111/jgs.13867. [DOI] [PubMed] [Google Scholar]
- Yatim F, Cristofalo P, Ferrua M, Girault A, Lacaze M, Di Palma M, Minvielle E. Analysis of nurse navigators’ activities for hospital discharge coordination: A mixed method study for the case of cancer patients. Support Care Cancer. 2017;25(3):863–8. doi: 10.1007/s00520-016-3474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibrik K, Laskin J, Ho C. Integration of a nurse navigator into the triage process for patients with non-small-cell lung cancer: Creating systematic improvements in patient care. Curr Oncol. 2016;23(3):e280. doi: 10.3747/co.23.2954. [DOI] [PMC free article] [PubMed] [Google Scholar]