Abstract
Background
Adherence to public health instructions for the COVID-19 is important for controlling the transmission and the pandemic’s health and economic impacts. The aim of this study was to determine the associated factors of non-adherence to public health and social measures instructions.
Methods
This was a cross-sectional study conducted with 1913 participants in two provinces of DRC, Mbuji-Mayi, and Kamina. Predictors of non-adherence to COVID-19 preventive measures were identified using binary logistic regression analysis. P-value<0.05 was considered as a significant predictor.
Results
Among 1913 participants (1057 [55.3%] male, age 34.1 [14.9] years), 36.6% were defined as non-adherents. Non-adherence was associated with never studied and primary education level [adjusted odds ratio (aOR)=1.63, CI=1.31–2.03], unemployed status [aOR=1.29, CI=1.01–1.67], living in Kamina (Haut-Lomami province) [aOR=1.63, CI=1.31–2.03], female gender of head of household [aOR=1.53, CI=1.16–2.03], no attending lectures/discussions about COVID-19 [aOR=1.61, CI=1.08–2.40], not being satisfied with the measures taken by the Ministry of Health [aOR=2.26, CI=1.78–2.81], not been regularly informed about the pandemic [aOR=2.25, CI=1.80–2.03], and bad knowledge about COVID-19 [aOR=2.36, CI=1.90–2.93].
Conclusion
The rate of non-observance of preventive measures for the COVID-19 pandemic is high, and different factors contributed. The government has to counsel the permanent updating of messages taking into account the context and the progress of the pandemic by using several communication channels.
Keywords: predictors, adherence, public health instructions, COVID-19 pandemic, DR Congo
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Coronaviruses (CoV) are zoonotic pathogens that can be transmitted via animal-to-human and human-to-human interactions. They are known to cause diseases including the common cold and Severe Acute Respiratory Syndrome (SARS).1
Originating from the city of Wuhan, Hubei Province, China, the 2019 novel coronavirus (2019-nCoV) is rapidly spreading to the rest of the world. The circumstantial evidence that links the first case of COVID-19 to the Huanan South Seafood Market that sells various exotic live animals suggests that the zoonotic Coronavirus crossed the barrier from animal to human at this wet market.2 It has since become a global public health emergency.3
The World Health Organization (WHO) designated COVID-19 a pandemic on March 11, 2020.4 The African region remains the least affected continent, with 99,433 cases and 3078 deaths, but the numbers are increasing. COVID-19 is majorly affecting many countries all over the world, whereas Africa is the last continent to be hit by the pandemic.
Many countries around the world are majorly affected by COVID-19, but Africa is the last continent to be hit by the pandemic.5 The first case of COVID-19 in Africa was confirmed in Egypt on February 14, 2020, and Nigeria reported the first confirmed case in sub-Saharan Africa, in an Italian patient who flew to Nigeria from Italy on February 25, 2020.6 The government response to the pandemic on the continent has not been without challenges. Airport screening has been implemented and mitigation efforts such as hand washing, social distancing, and stay‐at‐home lockdown measures have also been adopted. However, in the long-term these measures are unsustainable due to the socioeconomic dynamics in most African states.7
In the Democratic Republic of the Congo (DRC), the first COVID-19 case was reported on March 10, 2020.8 According to the latest report from the DRC COVID-19 Taskforce and Ministry of Health, the numbers of infected people in DRC reached 2660 on 27 May 2020, including 69 deaths.9 Since the first case of 2019-nCoV was registered in the DRC, no cases have been reported in Mbuji-Mayi and Kamina.
Vaccine may not be available in the early stages of a pandemic. So, non-medical measures such as the promotion of individual protection (hand hygiene and face masks), imposing travel restrictions, and social distancing of possibly infected cases are essential to reduce the possibility for new infections.10 The willingness of the general public plays an important and decisive role in achieving such measures recommended by public health authorities.11
It remains the health issues to lead the population to observe unconditionally these recommended preventive actions. However, it remains difficult to motivate people to adopt preventive behavior. Risk perception is identified as one of the factors contributing to an increase in public participation in adopting preventive measures.12,13 A high level of people’s risk perception can influence the intention to adopt protective measures. Effective risk communication is an essential element of outbreak management. Receiving information through different origins such as the ministry of health, frontline workers, and social media can affect the public’s knowledge about the risk perception and community engagement, thereby influencing their decision to adopt protective measures.14,15 It is therefore important to understand how the populations risk perception and their engagement. The best way to limit the spread of the COVID-19 depends on public adherence to the public health instructions. The aim of this study is to identify predictors of non-adherence to public health instructions.
Methods
Study Design, Site, and Participants
An analytical cross-sectional survey was conducted in the towns of Mbuji-Mayi (Kasai oriental province) and Kamina (Haut-Lomami province) in DRC, in May 2020.
Study Population, Inclusion, and Exclusion Criteria
The target was the female or male population, aged at least 18 years living in both cities for at least 6 months. We included all participants who gave consent to participate in the study and were found at home at the moment of the survey. We excluded those who did not give consent for participation in the study and were not found at home at the moment of the survey.
Sampling
The sample size was calculated using the following formula: n≥(Zα2.p.q)/d2, where the p represents the proportion of non-adherence to public health measures during the COVID-19 pandemic (we assumed that p=50% because this proportion in the DRC is unknown), q(1−p), z-value of the standard normal distribution corresponding to a significance level of alpha of 0.01 (2.58) and d the precision degree that we assumed to be 3% too. The minimal size computed was 1849 participants. A total of 1913 participants present in the health facilities were selected.
Data Collection
Data were collected with the use of a semi structured tablet-based questionnaire, which consisted of two parts: demographics and KAP. Demographic variables included age, gender of interviewee, gender of head of household, marital status, religion, current employment status, town, and the source information of COVID-19 related knowledge. The second part included 23 questions regarding COVID-19 related knowledge, and the last seven questions probing for observance to each of the instructions released to the public by the Ministry of Health. Participants were assured that the information collected would remain anonymous.
A correct answer was assigned 1 point, whereas an incorrect/unknown one was assigned 0 points. The total knowledge score ranged from 0–23, and a cut-off point for COVID-19 related knowledge level was 13: individuals with a score <13 were considered as having poor knowledge, whereas a score of 13 or higher indicated good knowledge. The dependent variable, non-adherence to the instructions, was measured by seven questions probing for observance to each of the instructions released to the public by the Ministry of Health.
The mean score on the non-adherence for each participant to the instructions scale was ≤4.
Ethical Approval
Ethical approval was obtained from the ethics committee of the School of Public Health (approval letter No UNILU/CEM/225/2020), University of Lubumbashi, and DRC in accordance with the Declaration of Helsinki. Participants were informed that participation was on a voluntary basis. Informed, verbal consent was obtained from each study participant, which was approved by the ethics committee, and that this study was conducted in accordance with the Declaration of Helsinki.
Statistical Analysis
Data were analyzed using SPSS 23.0 software. The continuous and categorical variables age, gender, marital status, level of education, religiousness, gender of head of household, City of residence, current employment status, exposure to media, heard about novel coronavirus, attended lectures/discussions about COVID-19, satisfied with the measures taken by the Ministry of Health, are presented as frequencies and proportions.
Binary logistic regression analysis was used to identify the predicting factors of non-adherence to the instructions for the COVID-19 pandemic. Variables that appeared to be associated (P<0.10) in the unadjusted analyses were further adjusted for demographic factors (ie, age, gender, education) using stepwise logistic regressions. Associations with a P-value<0.05 in the adjusted analyses were considered to be statistically significant.
Results
The overall data are described in Table 1. In summary, of the 1913 respondents, 44.0% were 25–45 years old and 21.7% were 46 years or older, 55.3% were men and 14.4% of head of household were women, 59.3% were married, 53.1% had a secondary education level, 87.6% identified as religious, 51.1% lived in Mbuji-Mayi, 21.5% were unemployed, and 92.6% were exposed to media. The majority of the participants (99.2%) had heard about Novel coronavirus and only 10.7% had attended lectures/discussions about COVID-19. More than a third of the participants (36.6%) were consequently defined as non-adherents to the instructions of the Ministry of Health for the COVID-19 pandemic.
Table 1.
Categorical Characteristics of the Sample
| Categorical Characteristics | Freq (%) | 95% CI |
|---|---|---|
| Gender | ||
| Male | 1057 (55.3) | 53.0–57.5 |
| Female | 856 (44.7) | 42.5–47.0 |
| Marital status | ||
| Never married | 640 (33.5) | 38.6–43.1 |
| Married | 1132 (59.3) | 56.9–61.4 |
| Others | 141 (7.4) | 6.2–8.6 |
| Age, mean±SD | 34.1±14.9 | |
| <25 years | 656 (34.3) | 32.2–36.5 |
| 25–45 years | 842 (44.0) | 41.8–46.3 |
| ˃45 years | 415 (21.7) | 19.9–23.6 |
| Education level | ||
| Never studied | 153 (8.0) | 6.8–9.3 |
| Primary | 414 (21.6) | 19.8–23.6 |
| Secondary | 1015 (53.1) | 50.8–55.3 |
| University | 331 (17.3) | 15.6–19.1 |
| City of residence | ||
| Kamina (Haut-Lomami province) | 936 (48.9) | 46.7–51.2 |
| Mbuji-Mayi (Kasai oriental province) | 977 (51.1) | 48.8–53.3 |
| Current employment status | ||
| Employed | 1502 (78.5) | 76.6–80.3 |
| Unemployed | 411 (21.5) | 19.7–23.4 |
| Gender of head of household | ||
| Male | 1637 (85.6) | 83.9–87.1 |
| Female | 276(14.4) | 12.9–16.1 |
| Religious | ||
| Yes | 1675 (87.6) | 86.0–89.0 |
| No | 238 (12.4) | 11.0–14.0 |
| Exposure to media | ||
| Yes | 1772 (92.6) | 91.3–93.7 |
| No | 141 (7.4) | 6.3–8.7 |
| Heard about novel coronavirus | ||
| Yes | 1897 (99.2) | 98.6–99.5 |
| No | 16 (0.8) | 0.5–1.4 |
| Attended lectures/discussions about COVID-19 | ||
| Yes | 204 (10.7) | 10.1–11.3 |
| No | 1709 (89.3) | 89.1–89.5 |
| Are you satisfied with the measures taken by the Ministry of Health | ||
| Yes | 1431 (74.8) | 72.9–76.7 |
| No | 482 (25.2) | 23.3–27.1 |
| Adherence to public health instructions for COVID-19 | ||
| ≤4 | 700 (36.6) | 34.7–38.8 |
| ˃4 | 1213 (63.4) | 61.2–65.6 |
Table 2 presents the analysis results for non-respect of the measures for the COVID-19 pandemic by people. The following background variables predicted non-adherence: female gender, age lower than 25 years, never studied, and primary education level, unemployed status, living in Kamina (Haut-Lomami province), female gender of head of household, non-media expose, not heard about Novel coronavirus, no attending of lectures/discussions about COVID-19, not been satisfied with the measures taken by the Ministry of Health, not been regularly informed about the pandemic, and bad knowledge about COVID-19.
Table 2.
Non-Adherence to the Instructions for the COVID-19 Pandemic by a Range of Categorical Characteristics of Participants
| Categorical Characteristics of Participants | N (%) | OR (95% CI) |
|---|---|---|
| Gender | ||
| Male | 341 (32.3) | Ref |
| Female | 359 (41.9) | 1.52 (1.26–1.83) |
| Marital status | ||
| Never married and others | 298 (38.2) | 1.12 (0.93–1.35) |
| Married | 402 (35.5) | Ref |
| Age | ||
| ˂25 | 268 (40.9) | 1.32 (1.09–1.60) |
| ≥25 | 432 (34.4) | Ref |
| Education level | ||
| Never studied and primary | 277 (48.9) | 2.08 (1.70–2.55) |
| Secondary and University | 423 (31.4) | Ref |
| City of residence | ||
| Kamina (Haut-Lomami province) | 419 (44.8) | 2.01 (1.66–2.43) |
| Mbuji-Mayi (Kasai oriental province) | 281 (28.8) | Ref |
| Current employment status | ||
| Unemployed | 175 (42.6) | 1.38 (1.10–1.72) |
| Employed | 525 (35.0) | Ref |
| Gender of head of household | ||
| Male | 559 (34.1) | Ref |
| Female | 141 (51.1) | 2.01 (1.56–2.61) |
| Religious | ||
| Yes | 620 (37.0) | Ref |
| No | 80 (33.6) | 0.86 (0.65–1.15) |
| Exposure to media | ||
| Yes | 626 (35.3) | Ref |
| No | 74 (52.5) | 2.02 (1.43–2.85) |
| Heard about Novel coronavirus | ||
| Yes | 688 (36.3) | Ref |
| No | 12 (75.0) | 5.27 (1.69–16.41) |
| Attended lectures/discussions about COVID-19 | ||
| Yes | 37 (18.1) | Ref |
| No | 663 (38.8) | 2.86 (1.98–4.14]) |
| Are you satisfied with the measures taken by the Ministry of Health | ||
| Yes | 430 (30.0) | Ref |
| No | 270 (56.0) | 2.97 (2.40–3.67) |
| Regularly informed about the pandemic | ||
| Yes | 384 (29.3) | Ref |
| No | 316 (52.5) | 2.67 (2.19–3.26) |
| Level of knowledge | ||
| Good | 363 (27.7) | Ref |
| Bad | 337 (55.9) | 3.31 (2.70–4.08) |
Table 3 presents the multivariate logistic regression analysis, the following variables predicted non-respect of the instructions for the COVID-19 pandemic: never studied and primary education level, unemployed status, living in Kamina (Haut-Lomami province), female gender of head of household, not attending lectures/discussions about COVID-19, not been satisfied with the measures taken by the Ministry of Health, not been regularly informed about the pandemic, and bad knowledge about COVID-19.
Table 3.
Factors of Non-Adherence to the Instructions of the Ministry of Health for the COVID-19 Pandemic by Multivariate Logistic Regression Analysis
| Factors of Non-Adherence | B | SE | Adjusted OR (95% CI) | P |
|---|---|---|---|---|
| Education level (Never studied and primary vs secondary & University) | 0.49 | 0.11 | 1.63 (1.31–2.03) | 0.000 |
| City of residence (Kamina vs Mbuji-Mayi) | 0.49 | 0.11 | 1.63 (1.31–2.03) | 0.000 |
| Current employment status (Unemployed vs Employed) | 0.26 | 0.13 | 1.29 (1.01–1.67) | 0.041 |
| Gender of head of household (female vs male) | 0.43 | 0.14 | 1.53 (1.16–2.03) | 0.003 |
| Attended lectures/discussions about COVID-19 (No vs yes) | 0.48 | 0.20 | 1.61 (1.08–2.40) | 0.018 |
| Level knowledge (Bad vs good) | 0.86 | 0.11 | 2.36 (1.90–2.93) | 0.000 |
| Regularly informed about the pandemic (No vs yes) | 0.81 | 0.11 | 2.25 (1.80–2.81) | 0.000 |
| Are you satisfied with the measures taken by the Ministry of Health (No vs yes) | 0.81 | 0.12 | 2.26 (1.78–2.87) | 0.000 |
| Constant | −2.32 | 0.21 | 0.000 |
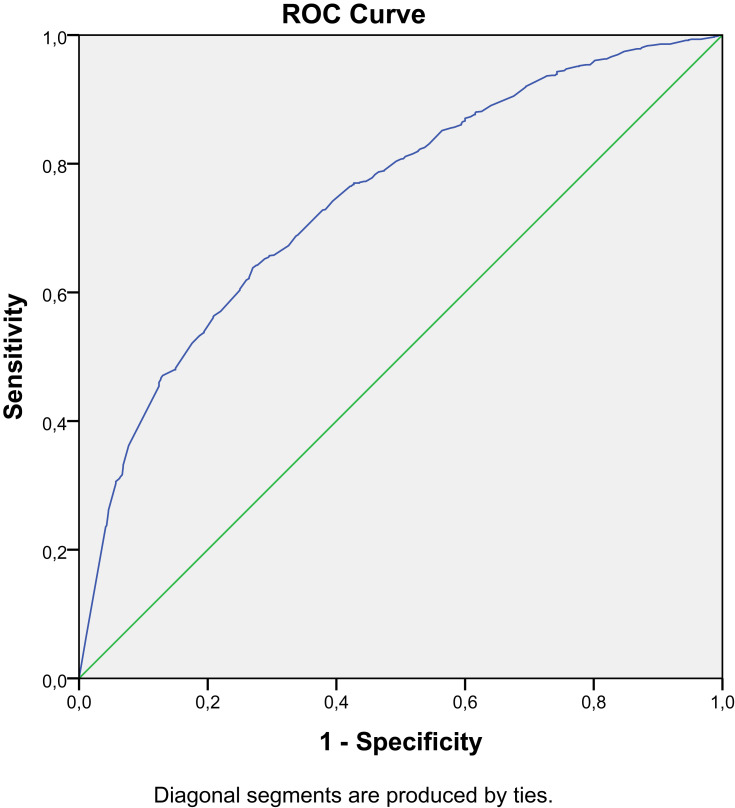
The discriminant analysis shows that the values of the area under the curve (AUC) indicate a predictive capacity on non-respect of the measures for the COVID-19 pandemic of 0.75 or 75% (AUC between 0.72 and 0.77) (Figure 1).
Figure 1.
ROC curve of factors of non-adherence to the instructions of the Ministry of Health for the COVID-19 pandemic.
Discussion
Understanding characteristics of people who do not comply with COVID-19-related public health measures is essential for developing effective public health campaigns in the current and future pandemics. To reduce the COVID-19 transmission and impact, in the context of absence of vaccines or curative medical treatment, high adherence to public health measures is crucial. The success of this approach is best measured by the public’s willingness to comply. A number of public opinion polls suggest that the public generally abides by these measures.16
The study shows that non-respect of public health measures for COVID-19 can be predicted by never studied and primary education level, unemployed status, living in Kamina (Haut-Lomami province), female gender of head of households, no attending lectures/discussions about COVID-19, not been satisfied with the measures taken by the Ministry of Health, not been regularly informed about the pandemic, and bad knowledge about COVID-19.
People's engagement to an effective public response to an emergency requires clear communication and trust.17–19 In the epidemic context, there is no sufficient time for dialog or feedback because immediate actions are required. In such conditions, the communication for development is no more a required approach than the risk communication and the community engagement. In democratic and non-democratic societies, risk reduction measures such as social distancing and lockdown cannot be coercive. People must understand what is required and be persuaded of the need to comply with it. Risk perception, behavioral changes, and trust in government information sources change when pandemics are progressing.20,21 Gender, income, geography, or social interactions are important determinants of recommended public health behavior.22–24 It should be noted that the population of Kamina did not non-adhere to public health instructions.
Our study shows that not been regularly informed about the pandemic and bad knowledge about COVID-19 are factors of non-adherence to public health instructions. While more information is available, the Ministry of Health has to update the messages to achieve effective risk communication in the outbreak context. This is essential not only to instruct and motivate the community to adopt preventive measures, but also to build trust in public health authorities and prevent misconceptions. Emotional aspects like anxiety play a role in decision-making. Health authorities have to recognize these emotional aspects and take them into account in their risk communication.
Concerning educational level, a person whom never studied and primary education level had non-respect of public health measures for COVID-19. No link is established between the education level and the behavior to be avoided. In the UK, during the swine flu pandemic, research showed that people without a diploma were more likely to adopt protective attitudes (for example, avoiding crowds or public transport),25 while in Hong Kong, higher educated people have been shown to be more likely to avoid public places during the SARS outbreak.26 In Australia, it was found that people with higher education were more likely to report expected compliance.27 On the whole, the instruction allows the adoption of protective and avoidant behaviors, while some results have remained inconclusive.
A strength of our study was represented by the fact that the survey was conducted quickly in the most critical period when health authorities recommended the compliance to various barrier measures anywhere and anytime. This study has also limitations. First, despite using probabilistic sampling so that personal characteristics of the sample broadly reflected those in the general population, we cannot be sure that survey respondents are representative of the general population in both provinces. Second, the data presented in this study are self-reported and partly dependent on the participants’ honesty and recall ability; thus, they may be subject to recall bias.
Conclusion
In conclusion, the present study indicates factors related to non-adherence on public health measures during the COVID-19 pandemic in the DRC. The non-adherence to these public health instructions can increase risk for the transmission of the pandemic. Effective risk communication and community engagement are important to protect the public during the COVID-19 pandemic.
Based on the results, we recommend the permanent updating of messages taking into account the context and the progress of the pandemic by using several communication channels (Radio, Newspapers, TV, Social networks, ETC). During these times, we believe that frontline workers, community health workers, and students in medical sciences can be useful as effective and trustworthy human resources against this pandemic. The change in declared willingness to comply with public health measures in the pandemic concern is necessary for the successful response and containment of the disease.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Bhagavathula A, Aldhaleei WA, Rahmani JR, Mahabadi MA, Bandari DK. Novel Coronavirus (COVID-19) knowledge and perceptions: a survey of healthcare workers (preprint). JMIR Public Heal Surveill. 2020. doi: 10.2196/19160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stübinger J, Schneider L. Epidemiology of Coronavirus COVID-19: forecasting the future incidence in different countries. Healthcare. 2020;8(2):99. doi: 10.3390/healthcare8020099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281–282. doi: 10.1111/pcn.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranney ML, Griffeth V, Jha AK. Critical supply shortages — the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382(18):28–30. doi: 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- 5.Lone SA, Ahmad A. COVID-19 pandemic – an African perspective. Emerg Microbes Infect. 2020;9(1):1300–1308. doi: 10.1080/22221751.2020.1775132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dzinamarira T, Dzobo M, Chitungo I. COVID ‐ 19: a perspective on Africa ’ s capacity and response. J Med Virol. 2020;(June):1–8. doi: 10.1002/jmv.26159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Senghore M, Savi MK, Gnangnon B, Hanage WP, Okeke IN. Leveraging Africa’s preparedness towards the next phase of the COVID-19 pandemic. Lancet Glob Heal. 2020;2019(20):2019–2020. doi: 10.1016/S2214-109X(20)30234-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehtar S, Preiser W, Lakhe NA, et al. Comment Limiting the spread of COVID-19 in Africa -: one size mitigation strategies do not fit all countries. Lancet Glob Heal. 2020;2019(20):2019–2021. doi: 10.1016/S2214-109X(20)30212-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DRC Ministry of Health, COVID-19 epidemiological status in Democratic Republic of Congo; 2020. Available from: https://www.stopcoronavirusrdc.info/. Accessed July28, 2020.
- 10.Raude J, Setbon M. Lay perceptions of the pandemic influenza threat Lay perceptions of the pandemic influenza threat. Eur J Epidemiol. 2000;24:339–342. doi: 10.1007/s10654-009-9351-x [DOI] [PubMed] [Google Scholar]
- 11.De Zwart O, Veldhuijzen IK, Elam G, Brug J. Perceived threat, risk perception, and efficacy beliefs related to SARS and other (emerging) infectious diseases: results of an international survey. Int J Behav Med. 2009;16:30–40. doi: 10.1007/s12529-008-9008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith RD. Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Soc Sci Med. 2006;63:3113–3123. doi: 10.1016/j.socscimed.2006.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khosravi M. Perceived risk of COVID-19 pandemic: the role of public worry and trust. Electron J Gen Med. 2020;17(4):1–2. doi: 10.29333/ejgm/7856 [DOI] [Google Scholar]
- 14.Sadique MZ, Edmunds WJ, Smith RD, et al. Precautionary behavior in response to perceived threat of pandemic influenza. Emerg Infect Dis. 2007;13(9):1307–1313. doi: 10.3201/eid1309.070372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Voeten HACM, De Zwart O, Elam G, Abraham T, Brug J. Sources of information and health beliefs related to SARS and avian influenza among Chinese communities in the United Kingdom and The Netherlands, compared to the general population in these countries. Int J Behav Med. 2009;16:49–57. doi: 10.1007/s12529-008-9006-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nivette A, Ribeaud D, Murray AL, et al. Non-compliance with COVID-19-related public health measures among young adults: insights from a longitudinal cohort study. SocArXiv. 2020;31(May):1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holmes BJ. Communicating about emerging infectious disease: the importance of research. Health Risk Soc. 2008;10(4):349–360. doi: 10.1080/13698570802166431 [DOI] [Google Scholar]
- 18.Taylor M, Raphael B, Barr M, Agho K, Stevens G, Jorm L. Public health measures during an anticipated in fl uenza pandemic: factors in fl uencing willingness to comply. Risk Manag Heal Policy. 2009;2:9–20. doi: 10.2147/RMHP.S4810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Der Weerd W, Timmermans DRM, Beaujean DJMA, Oudhoff J, van Steenbergen JE. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health. 2011;11(575):1–12. doi: 10.1186/1471-2458-11-575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibuka Y, Chapman GB, Meyers LA, Li M, Galvani AP. The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infect Dis. 2010;10(1):1–11. doi: 10.1186/1471-2334-10-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bults M, Beaujean DJMA, De Zwart O, Kok G, Van Empelen P. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. 2011;11(1):2. doi: 10.1186/1471-2458-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15:797–824. doi: 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chuang Y, Huang Y, Tseng K, Yen C, Yang L, Tang JW. Social capital and health-protective behavior intentions in an influenza pandemic. PLoS One. 2015;10(4):1–14. doi: 10.1371/journal.pone.0122970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gamma AE, Slekiene J, Von Medeazza G, Asplund F, Cardoso P, Mosler H-J. Contextual and psychosocial factors predicting Ebola prevention behaviours using the RANAS approach to behaviour change in Guinea-Bissau. BMC Public Health. 2017;17(1):1–12. doi: 10.1186/s12889-017-4360-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubin GJ, Amlot R, Page L, Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339(jul02 3):1–8. doi: 10.1136/bmj.b2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leung GM, Quah S, Ho L-M, et al. A tale of two cities: community psychobehavioral surveillance and related impact on outbreak control in hong kong and singapore during the severe acute respiratory syndrome epidemic. Infect Control Hosp Epidemiol. 2004;25(12):1033–1041. doi: 10.1086/502340 [DOI] [PubMed] [Google Scholar]
- 27.Barr M, Raphael B, Taylor M, et al. Pandemic influenza in Australia: using telephone surveys to measure perceptions of threat and willingness to comply. BMC Infect Dis. 2008;8(117):1–14. doi: 10.1186/1471-2334-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]