Abstract
Background
Despite improvement in the coverage of most maternal, newborn, and child health services, inequality in the uptake of services still remains the challenge of health systems in most developing countries. This study was conducted to examine the degree of inequities and potential predictors of inequity in reproductive and maternal health services utilization in the Oromia region, Ethiopia.
Methods
The 2016 Ethiopian demographic and health survey data set was used. Utilization rate of four maternal health service categories (family planning, antenatal care, facility based delivery and postnatal care) was considered in the analysis. Equity in each of these indicators was assessed by residence (urban/rural), wealth index, and educational status. Inequality in service utilization was estimated using rate ratios, concentration curve, and concentration indices.
Results
Overall data of 5701 women were used in this analysis. The concentration index to all of the maternal health service utilization indicators showed significance. The concentration index of family planning, antenatal care, facility based delivery, and postnatal care was 0.136 (95% CI=0.099–0.173), 0.106 (95% CI=0.035–0.177), 0.348 (95% CI=0.279–0.418), and 0.348 (95% CI=0.279–0.418), respectively. Maternal age and all of the three socio-demographic factors (residence, education, and wealth) showed inequitable distribution of maternal health service utilization in the Oromia region. The majority of women who were in the favored groups utilized the key reproductive and maternal health services.
Conclusion
The utilization of maternal health services in the study area is grossly skewed to those who are well off, educated, and live in urban areas. Any action intended to improve utilization of maternal and child health services should aim to reduce the unnecessary and avoidable disparity demonstrated in our analysis. This of course demands multisectoral intervention to impact on the determinants.
Keywords: inequity, reproductive health, maternal health, utilization, Oromia, Ethiopia
Plain Language Summary
Although avoidable, inequities in the reproductive and maternal health service utilization remained the main challenge in effort towards ensuring universal health coverage in the middle and low income settings. This study was aimed to analyze the inequity in the utilization of four key maternal health services in the biggest regional state of Ethiopia. The current study findings showed that there was gross inequity in the utilization of family planning, antenatal care, facility birth and postnatal care services in the region. The socio-economic factors such as residence, level of education, and wealth index were the determinants of health service uptake. The current level of inequity significantly impacts the effort toward achieving universal health coverage and goal-related maternal health services in the Sustainable Development Goal (SDG). The results of this analysis will help policymakers, program designers, and managers to look for possible interventions that may narrow down the inequality gap.
Introduction
The concept of equity in health has been defined by various scholars demonstrating differing focus and approaches. Equity in health is the absence of systematic disparities in health or in the major social determinants of health between groups with different levels of underlying social advantage or disadvantage including wealth, power, or prestige.1 These differences are considered as unnecessary and avoidable, but also unfair and unjust. Equity in health implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential, if it can be avoided. Equity is concerned with creating equal opportunities for health and with bringing health differentials down to the lowest level possible.2
Globally there is increased emphasis to address inequities in maternal and child health services and this has led to a continual increase in relative equity of the coverage of reproductive and maternal health services across all countries over the past quarter of a century.3 However, evidence from low- and middle-income countries had revealed that inequity in coverage of health services persists in some countries more than others.4 There is uneven distribution of key health outcomes and access to key health services across different sub-groups of the population.5–11
Women and children in socioeconomically disadvantaged households are exposed to higher mortality rates and lower coverage and utilization of the key services than women and children from affluent households.12 For instance, the maternal mortality ratio in low income countries in 2017 was 462 per 100,000 live births vs 11 per 100,000 live births in high income countries. In 2017 alone, 295,000 women died, out of which 94% of all maternal deaths occured in low and middle income countries. Maternal deaths are nearly 50-times higher for women in Sub-Saharan Africa, and their babies are 10-times more likely to die in their first month of life, compared to high income countries.13
The factors such as maternal age, education, region of residence, and distance to health facilities were the determinants of inequity in the utilization of key reproductive and maternal health services. The utilization of key maternal health services was in favor of the youngest women, educated women, and women who were located in urban areas compared to their counterparts.7,–14–24 Likewise, accessibility was a major factor of inequity in the utilization of health services by women.25
The Government of Ethiopia has made a great effort in improving access and coverage of health services in the past few decades. As a result the coverage of essential maternal and child health services had been improved. Ethiopia still, however, had an unacceptable rate of maternal morbidity and mortality from preventable causes. This is partly related to the inequality in the coverage and uptake of key maternal health interventions among different regions and woredas within the country.6,7,19,26,27 National level surveys had shown disparity in the utilization of key reproductive and maternal health services across the regional states.20,26
Equity is the main agenda of Sustainable Development Goals (SDGs)28 and is a pillar of the Health Sector Transformation Plan (HSTP) of Ethiopia.29 It is also a means to realize the right to health, which is one of the goals in the pledge for universal health coverage by the international community.30,31 Achieving equity in health requires a commitment to monitor inequities which in turn necessitates generating evidences on equity of health services. Hence, this study was aimed at determining the degree of inequities in the utilization of key reproductive and maternal health services in the Oromia Regional State, the biggest of the regional states in Ethiopia. We had also analyzed the determinants of inequity in the utilization of reproductive and maternal health services in the region.
Methods
Study Setting
Oromia was one of the ten regional states in Ethiopia with the largest population and surface area. Oromia is comprised of 21 zonal administrations and 19 town administrations. In the region there were a total of 317 rural districts and 7021 kebeles. According to 2007 population and housing census projections, the total population of the region was 36,839,051 in 2017 and 38,170,034 in 2020. In 2020, there were 107 hospitals (95 public and 12 private hospitals), 1404 health centers, and 7090 health posts.
Data Source and Measurements
The 2016 Ethiopian demographic and health survey data set was used as a source of data to address the research questions.26
The survey was conducted from January 18 to June 27, 2016 and data were extracted from March 15 to April 2018. In the survey, all women in the reproductive age group (15–49) who were residing in the selected households were included.26 A sample of Enumeration areas (EA’s) was selected using a two stage stratified sampling strategy, where each region is stratified into urban and rural area. A census frame created during the 2007 population and housing census was used (comprising of a total of 84,915 EAs). In this study EA referred to a geographic area covering on average 181 households. In the first stage, 645 EA’s (202 in urban areas and 443 in rural areas) were selected with a probability proportional to each region’s size. In the second stage, 28 households per EA were selected with an equal probability systematic selection from the newly created household listing. A full description of the study method is available in the Ethiopian demographic and health survey (EDHS) 2016 full report.26
In this analysis, data of 5701 eligible women of the reproductive age group in the Oromia region were used. Data extracted for analysis included demographic variables (age), socioeconomic characteristics (residence, wealth index, educational status), and key indicators for reproductive and maternal health service uptake (family planning, antenatal care, delivery, postnatal care). These are key maternal services provided at the maternity unit of health facilities (health centers and hospitals) in Ethiopia. Furthermore, at the maternity unit screening and treatment of syphilis, hepatitis, HIV/AIDS, and acute malnutrition are undertaken by the health workers. At health posts maternal services including family planning, antenatal care (second and third visits), and postnatal care are provided. The health extension workers assigned at Ethiopian health posts link women to close health centers for antenatal care (first and fourth visits) and delivery services.
Study Variables
Residence (Urban/Rural)
Urban areas included all capitals of administrative zones and woredas. Areas with at least 1000 people primarily engaged in non-agricultural activities and/or localities were declared as urban areas by administrative officials. Rural areas were all areas which were not urban areas.26
Wealth Index
The wealth index in the survey was computed using household assets ranging from a television to a bicycle or a car, in addition to housing characteristics such as the source of drinking water, toilet facilities, and flooring materials. It was determined using principal component analysis (PCA).26 The wealth index was used as an indicator of level of wealth that is in line with income and expenditure measures.
The wealth index in the analysis was created in three steps. First, wealth scores were calculated using indicators common for both urban and rural areas. In the second step, using indicators specific to household’s in urban and rural areas separate factor scores were produced. Then in the third stage, separate area specific factor scores were combined to produce a nationally applicable wealth index by adjusting scores specific to the areas.26
Educational Status
In this analysis four categories of educational levels are utilized: no education, primary education, secondary education, and higher education. Women with no formal education were labeled as no education, while women with incomplete primary and complete primary education level were labeled as a primary education, and those with incomplete secondary and complete secondary were labeled as secondary education. Moreover, women who received more than secondary education were labeled as higher education.26
Skilled providers: skilled health service providers included doctors, nurses, midwives, health officers, and health extension workers.
Institutional deliveries: referred to a delivery that occurs in a health facility (health center or hospital).
Use of modern contraceptive methods: percentage of currently married women (15–49) who are currently utilizing a modern contraceptive method such as male and female sterilization, injectable, intrauterine devices (IUDs), contraceptive pills, implants, female and male condoms, standard days method, lactational amenorrhea method, and emergency contraception.
Antenatal care by skilled provider: the proportion of women aged 15–49 who had a live birth in the 5 years preceding the survey that received antenatal care from skilled providers (physicians, nurses or midwives, health officers, and health extension workers) at least once.
Birth at health facility: proportion of live births in the 5 years preceding the survey delivered in a health facility (private or public).
Postnatal care: proportion of women aged 15–49, with a live birth in the 2 years preceding the survey, who received a postnatal checkup in the first 2 days after giving birth.
Statistical Analysis
Four different equity analysis techniques were used to address the research questions. The techniques were equity gap, equity ratio, concentration curve, and concentration index.13–16 Equity gap was used to show absolute percentage point difference in service coverage between the highest wealth quintile and the lowest, between the highest educational levels achieved and the lowest, and between urban and rural residents. The equity ratio was calculated by dividing service coverage in the top wealth quintile by that in the bottom, and service coverage among urban by that of rural dwellers. The concentration curve plots the cumulative percentage of the population, ranked by wealth, beginning with the poorest, and ending with the richest (x-axis) against the cumulative percentage of the health service utilization (y-axis).
Concentration index (CI) was estimated to quantify the level of inequities in access and utilization for each maternal health service. The index takes a value between −1 and +1; 0 index indicates the presence of equality in utilization of the health variable. When the concentration index takes on a positive value, the line of concentration curve will be below the line of equity, implying a pro-rich uptake of the service and vice versa. The concentration index for t=1, …, T groups was computed in a spreadsheet program using the following formula.
 |
where  is the cumulative percentage of the sample ranked by economic status in group t, and
is the cumulative percentage of the sample ranked by economic status in group t, and  is the corresponding concentration curve ordinate.
is the corresponding concentration curve ordinate.
Results
Description of Study Participants
A majority (85%) of women were from rural areas, and half of them had no formal education (51%). The wealth quintile of the households of the respondents was about equally distributed (Table 1).
Table 1.
Demographic and Socio-Economic Characteristics of the Study Participants in Oromia Region, 2016
| Variables | Frequency | Percent (95% Confidence Interval) |
|---|---|---|
| Age (years) | ||
| 15–19 | 1234 | 21.7 (20.6–22.7) |
| 20–24 | 995 | 17.5 (16.5–18.5) |
| 25–29 | 1062 | 18.6 (17.6–19.7) |
| 30–34 | 924 | 16.2 (15.3–17.2) |
| 35–39 | 702 | 12.3 (11.5–13.2) |
| 40–44 | 428 | 7.5 (6.8–8.2) |
| 45–49 | 356 | 6.2 (5.6–6.9) |
| Urban–rural status | ||
| Urban | 869 | 15.2 (14.3–16.2) |
| Rural | 4832 | 84.8 (83.8–85.7) |
| Educational achievement | ||
| No education | 2914 | 51.1 (49.8–52.4) |
| Primary | 2097 | 36.8 (35.5–38.0) |
| Secondary | 471 | 8.3 (7.6–8.9) |
| Higher | 219 | 3.8 (3.4–4.4) |
| Household wealth index in quintile | ||
| Lowest | 853 | 15.0 (14.1–15.9) |
| Second | 1166 | 20.4 (19.4–21.5) |
| Middle | 1149 | 20.1 (19.1–21.2) |
| Fourth | 1252 | 22.0 (20.9–23.1) |
| Highest | 1281 | 22.5 (21.4–23.6) |
Utilization of Reproductive and Maternal Health Services
A majority of the women were not using any family planning method (79%). Half (51%) of the women had received prenatal care and three-quarters (76%) of them gave birth at home (Table 2).
Table 2.
Reproductive and Maternal Health Service Utilization Among Women in the Reproductive Age Group, Oromia Region, Ethiopia, 2016
| Variables | Frequency | Percent (95% Confidence Interval) |
|---|---|---|
| Current FP use by method type | ||
| No method | 4488 | 78.7 (77.7–79.8) |
| Traditional method | 20 | 0.4 (0.2–0.5) |
| Modern method | 1193 | 20.9 (19.9–22.0) |
| Total | 5701 | 100 |
| Received prenatal care (last birth) | ||
| No | 1522 | 48.6 (46.9–50.4) |
| Yes | 1607 | 51.4 (49.6–53.1) |
| Total | 3129 | 100 |
| Number of antenatal visits during the pregnancy (last birth) | ||
| 0 visit | 1522 | 48.7 (46.9–50.4) |
| 1 visit | 135 | 4.3 (3.7–5.1) |
| 2 visits | 234 | 7.5 (6.6–8.5) |
| 3 visits | 544 | 17.4 (16.1–18.8) |
| 4+ visits | 692 | 22.1 (20.7–23.6) |
| Total | 3127 | 100 |
| Place of delivery | ||
| Home | 2365 | 75.6 (74.0–77.0) |
| Health facility | 765 | 24.4 (22.9–25.9) |
| Total | 3130 | 100 |
| Doctor gave delivery care for last birth | ||
| No | 3032 | 96.9 (96.3–97.5) |
| Yes | 97 | 3.1 (2.5–3.8) |
| Total | 3129 | 100 |
| Nurse/midwife gave delivery care for last birth | ||
| No | 2095 | 66.9 (65.3–68.6) |
| Yes | 1034 | 33.1 (31.4–34.7) |
| Total | 3129 | 100 |
| Traditional birth attendant gave delivery care for last birth | ||
| No | 1837 | 58.7 (56.9–60.4) |
| Yes | 1292 | 41.3 (39.6–43.0) |
| Total | 3129 | 100 |
| No one gave delivery care (last birth) | ||
| No | 2554 | 81.6 (80.2–82.9) |
| Yes | 576 | 18.4 (17.1–19.8) |
| Total | 3130 | 100 |
| Woman’s health checked before discharge after delivery (last birth) | ||
| No | 543 | 70.9 (67.7–74.1) |
| Yes | 222 | 29.1 (25.9–32.3) |
| Total | 765 | 100 |
| Woman’s health checked after discharge/home delivery for last birth | ||
| No | 3017 | 96.4 (95.7–97.0) |
| Yes | 112 | 3.6 (2.9–4.3) |
| Total | 3129 | 100 |
Use of Modern Contraceptive Methods
There was inequity in the utilization of key reproductive and maternal health services by women in the region, where more women from urban areas (28% vs 20%) and in the higher education category (27% vs 23%) were utilizing modern contraceptive methods than their counterparts. The utilization of modern contraceptives among women in the highest wealth quintiles was about two times more than those in the lowest wealth quintiles (27% vs 14%) (Table 3).
Table 3.
Proportion of Women Using Reproductive and Maternal Health Services by Socio-Demographic Characteristics
| Study Variables | Use of Modern Contraceptive | Antenatal Care by Skilled Provider | Birth at Health Facility | Postnatal Care | ||||
|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | |
| Age in years | ||||||||
| 15–19 | 1234 | 4.6 | 179 | 69.3 | 179 | 34.1 | 179 | 5.6 |
| 20–24 | 995 | 21.5 | 645 | 56.3 | 645 | 29.1 | 644 | 7.6 |
| 25–29 | 1062 | 35.7 | 875 | 54.4 | 875 | 26.6 | 875 | 7.3 |
| 30–34 | 924 | 30.0 | 717 | 52.4 | 716 | 22.3 | 716 | 8.4 |
| 35–39 | 702 | 21.1 | 454 | 38.8 | 454 | 19.6 | 455 | 5.3 |
| 40–44 | 428 | 25.2 | 191 | 39.8 | 191 | 13.6 | 191 | 6.3 |
| 45–49 | 356 | 8.4 | 68 | 23.5 | 69 | 11.6 | 69 | 4.3 |
| Area of residence | ||||||||
| Urban | 869 | 28.3 | 213 | 85.4 | 214 | 93.5 | 214 | 23.8 |
| Rural | 4832 | 20.0 | 2916 | 48.9 | 2915 | 19.4 | 2915 | 5.9 |
| Educational status | ||||||||
| No education | 2914 | 22.9 | 2034 | 43.0 | 2034 | 14.1 | 2034 | 3.7 |
| Primary | 2097 | 18.5 | 924 | 62.4 | 924 | 36.4 | 924 | 10.9 |
| Secondary | 471 | 21.0 | 119 | 86.6 | 119 | 79.0 | 119 | 25.8 |
| Higher | 219 | 26.5 | 52 | 100.0 | 52 | 92.3 | 52 | 28.8 |
| Economic status | ||||||||
| Lowest | 853 | 13.5 | 627 | 40.2 | 627 | 5.9 | 627 | 2.6 |
| Second | 1166 | 16.0 | 736 | 43.1 | 735 | 17.3 | 735 | 5.2 |
| Middle | 1149 | 20.5 | 697 | 53.2 | 697 | 21.5 | 697 | 4.4 |
| Fourth | 1252 | 26.1 | 647 | 56.0 | 648 | 27.9 | 648 | 7.6 |
| Highest | 1281 | 27.2 | 422 | 72.3 | 422 | 64.0 | 422 | 21.1 |
| Overall | 5701 | 21.3 | 3129 | 51.4 | 3129 | 24.4 | 3129 | 7.1 |
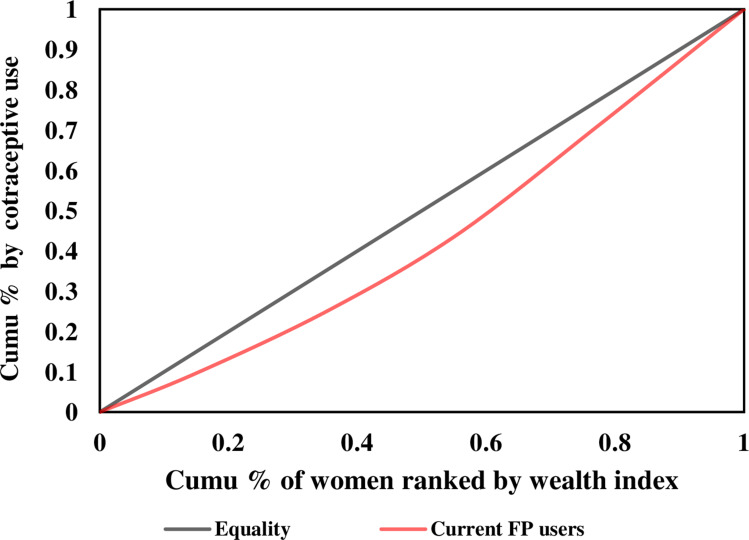
The concentration curve also confirmed that, with increasing wealth, the utilization of contraceptives also increased (concentration index=0.136) (Figure 1 and Table 4).
Figure 1.
Pro-rich uptake of modern contraceptives in the Oromia region, Ethiopia, 2016.
Table 4.
Rate Ratios and Concentration Indices for the Uptake of Reproductive and Maternal Health Services in the Oromia Region, Ethiopia, 2016
| Indicators | Rate-Ratio (Rich/Poor) | Concentration Indices | Standard Error | Confidence Interval (95%) | P-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Use of modern contraceptive | 2.0 | 0.136 | 0.019 | 0.099 | 0.173 | <0.001 |
| ANC by skilled provider | 1.8 | 0.106 | 0.036 | 0.035 | 0.177 | <0.001 |
| Early initiation of ANC | 2.3 | 0.137 | 0.041 | 0.057 | 0.217 | 0.001 |
| Antenatal care four and more visits | 3.1 | 0.261 | 0.089 | 0.087 | 0.435 | 0.005 |
| Facility based delivery | 10.8 | 0.348 | 0.035 | 0.279 | 0.418 | <0.001 |
| Home delivery | 0.38 | −0.048 | 0.0049 | −0.058 | −0.039 | <0.001 |
| Postnatal checkup | 8.1 | 0.348 | 0.035 | 0.279 | 0.418 | <0.001 |
Antenatal Care
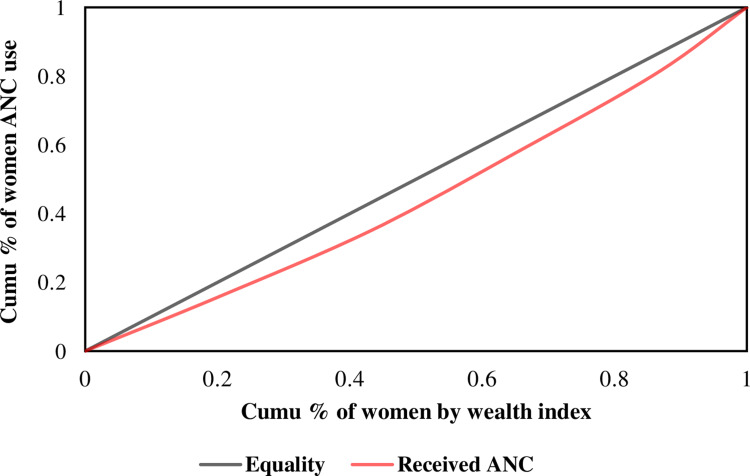
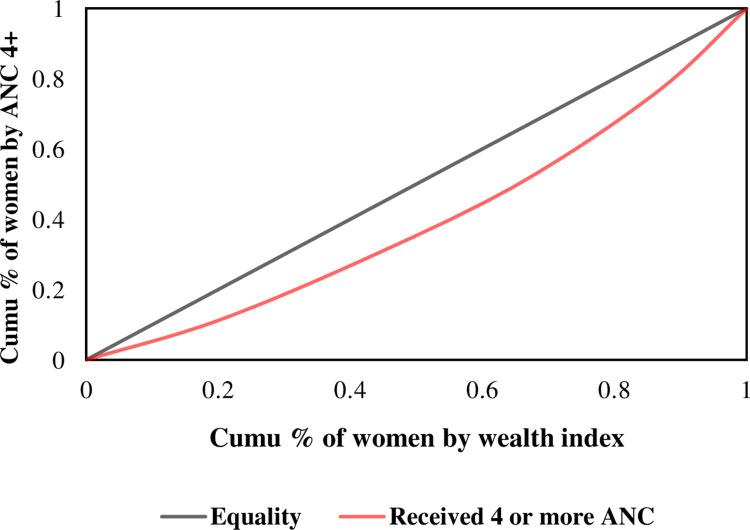
Antenatal care utilization (ANC) is one of the high impact interventions to avert risk to the life of pregnant women and their fetuses. In the study area, the utilization of ANC services from a skilled provider was highest among the more advantaged groups than their counterparts. More women from urban areas (85% vs 49%) and the highest education category (100% vs 43%) had received ANC service from a skilled provider compared to rural residents and women with no education, respectively. Similarly, more women in the highest wealth quintile had received ANC services than women in the lowest wealth quintile (72% vs 40%) (Tables 3 and 4). The concentration curve also revealed that ANC service utilization was concentrated among women in the richer households (Figures 2 and 3).
Figure 2.
Pro-rich uptake of Antenatal care first visit services in the Oromia region, Ethiopia, 2016.
Figure 3.
Pro-rich uptake of Antenatal care services four and more visits in the Oromia region, Ethiopia, 2016.
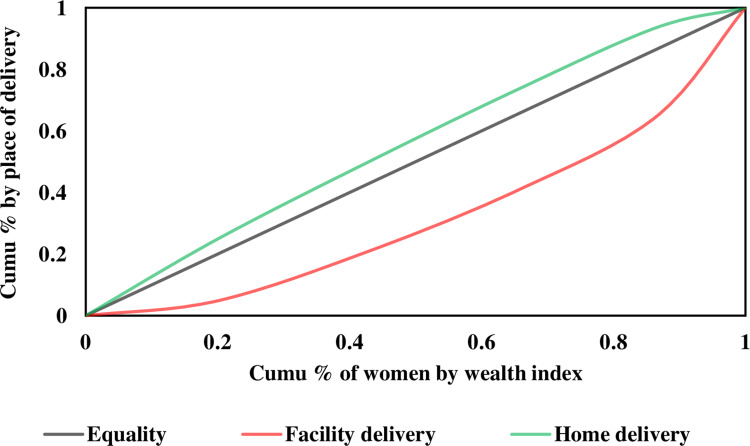
Place of Delivery
Women from urban areas had 5-times more births at a health facility than women from rural areas. Facility-based delivery was 6-times higher in higher-level education women than those with no education. The majority of the mothers (75.6%) gave birth to their child at home, mainly assisted by relatives and traditional birth attendants (TBA). Women from the richest quintile had about 11-times more births at a health facility than women from the lower wealth quintile (Tables 3 and 4). The concentration curve and index (concentration index=0.348) showed that more women from the richest wealth quintile gave birth at health facilities than women from the lower wealth quintile (Figure 4).
Figure 4.
Pro-rich uptake of delivery services in the Oromia region, Ethiopia, 2016.
Furthermore, skilled birth attendance was more likely among women in urban settings, educated women, and women in the highest wealth quintiles, whereas traditional birth attendance was higher among disadvantaged women (Table 5).
Table 5.
Delivery Assistance Services with Socio-Demographic Variables, Oromia Region, Ethiopia, 2016
| Background Characteristics | Delivery by Doctor | Delivery by Nurse/Midwifery | Delivery by TBA | No Care Giver During Delivery | SBA Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | Number | % | |
| Residence | ||||||||||
| Urban | 213 | 21.6 | 213 | 79.5 | 213 | 0.0 | 213 | 1.8 | 213 | 21.4 |
| Rural | 2916 | 1.6 | 2916 | 17.0 | 2916 | 44.3 | 2916 | 19.6 | 2916 | 8.4 |
| Education | ||||||||||
| No education | 2034 | 0.9 | 2034 | 12.9 | 2034 | 45.7 | 2034 | 23.7 | 2034 | 6.6 |
| Incomplete primary | 839 | 5.2 | 839 | 29.2 | 839 | 37.2 | 839 | 10.2 | 839 | 15.1 |
| Complete primary | 85 | 5.9 | 85 | 42.4 | 85 | 38.1 | 85 | 6.8 | 85 | 12.1 |
| Incomplete secondary | 104 | 9.2 | 104 | 65.8 | 104 | 17.1 | 104 | 2.2 | 104 | 12.2 |
| Complete secondary | 15 | 28.8 | 15 | 71.2 | 15 | 0.0 | 15 | 0.0 | 15 | 28.8 |
| Higher | 52 | 20.1 | 52 | 79.9 | 52 | 0.0 | 52 | 0.0 | 52 | 20.1 |
| Economic status | ||||||||||
| Lowest | 627 | 0.8 | 627 | 4.2 | 627 | 56.0 | 627 | 18.9 | 627 | 16.2 |
| Second | 735 | 0.8 | 735 | 16.9 | 735 | 46.6 | 735 | 23.8 | 735 | 4.4 |
| Middle | 697 | 1.8 | 697 | 16.7 | 697 | 39.4 | 697 | 22.0 | 697 | 9.5 |
| Fourth | 648 | 2.7 | 648 | 25.8 | 648 | 37.6 | 648 | 14.9 | 648 | 9.4 |
| Highest | 422 | 12.1 | 422 | 54.7 | 422 | 19.1 | 422 | 7.7 | 422 | 18.1 |
| Overall | 3129 | 3.0 | 3129 | 21.2 | 3129 | 41.3 | 3129 | 18.1 | 3129 | 24.2 |
Abbreviations: TBA, traditional birth attendant; SBA, skilled birth attendant.
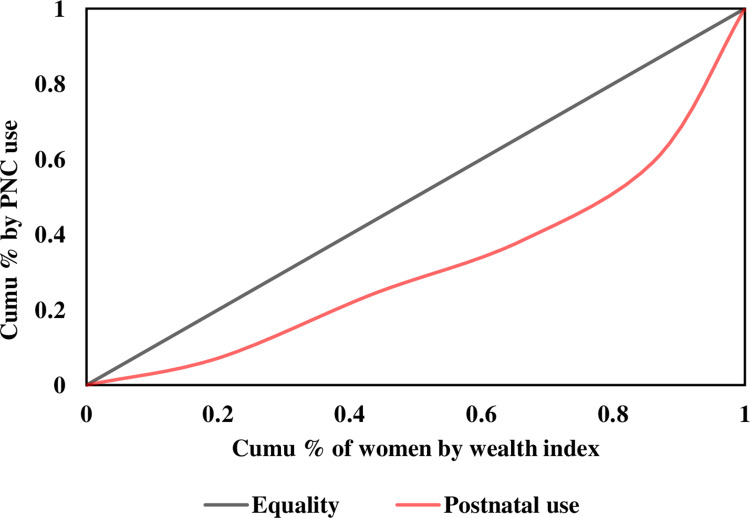
Postnatal Care
Utilization of Postnatal Care (PNC) services before discharge was higher among urban, educated, and highest wealth quintile women compared to their counterparts. Women in urban settings and those in the highest education category had utilized PNC services 4- and 8-times higher than their counterparts, respectively. PNC service utilization was highest among women of the highest wealth quintile by about 8-folds compared to the lowest wealth quintiles (Table 3). The concentration curve and indices also revealed that PNC use was more among the more favored women (Figure 5 and Table 4).
Figure 5.
Pro-rich uptake of postnatal care services in the Oromia region, Ethiopia, 2016.
Discussion
This study assessed the inequity in the utilization of key reproductive and maternal health services in the biggest regional state of Ethiopia. The findings of the study had indicated that there is significant disparity in the utilization of key reproductive and maternal health services in the region. Uptake of contraceptives, antenatal care, facility delivery, and postnatal care were concentrated in favor of the more advantaged women (urban residents, wealthiest, and more educated) of the region.
The highest degree of inequality in the uptake of modern contraceptives was observed when wealth quintile was considered as the variable of interest. We showed that women in the highest wealth quintile were 2-times more likely to use modern contraceptives than those in the lowest wealth quintile (concentration index=0.136). To a lesser extent, analysis with the lens of both educational status and area of residence had a similar pro-rich outcome. In Ethiopia, use of modern contraceptive methods has significantly increased from 6% in 2000 to 35% in 2016 and unmet need had declined by about 50% during the same period.27 However, a significant number of rural women have an unmet need for contraceptives compared to urban women (25% rural vs 11% urban).26 A similar pattern of disparity in the use of contraceptives was also reported in an earlier analysis from Ethiopia26 and other low and middle income countries.32
Systematic disparity in the uptake of maternal health services was also observed based on place of residence, education levels, and household wealth status. The utilization of antenatal care services from a skilled provider was higher among women from urban residences, higher education category, and highest wealth quintiles by about 37%, 57%, and 32% compared to women from rural areas, those who had lower education, or those from lower wealth quantiles. Equally, facility births and postnatal care utilization also showed huge disparity. These findings agreed with the state of inequality report by the WHO,32 the national reports,26 and another related study.19 Our study findings were also comparable with the findings reported in Bangladesh and other similar settings which showed the key reproductive and maternal health services were concentrated among wealthier, more educated, and women from urban areas.7–24,33–36
There is inter-regional disparity in the uptake of maternal health services worldwide, with the highest disparity being in Africa and Asia regions. This has huge implications in progress towards attaining SDG targets related to maternal health.15 Though there was a decline of inequity of maternal health services across Sub-Saharan Africa countries, absolute measures for geographical and wealth-based inequalities remained high invariably in most countries. Still, more favored groups have better access and utilize services demanding urgent actions to address the gaps aroused by the socio-economic factors.35,37
In Ethiopia, there was encouraging expansion of public health facilities and uptake of key reproductive and maternal health services in the past decades. Most of the maternal health services were provided free of charge at the public health facilities (hospital, health center, and health posts). The inequity in the utilization of these services, however, remained huge across the different factors.38,39 This could be explained by the poor quality of care provided in many of the health facilities as a result of failure of providers to adhere to guidelines and absence of required resources to deliver care.40 The variations in geographic accessibility of health facilities across residence (urban–rural) can also highly affects maternal health service utilization in Ethiopia.41 The role of culture and access to information should also be born in mind to fully understand the existing level of inequity.24 For instance, autonomy of women significantly influences decisions about service utilization and it has been shown that in Ethiopia male partners make decisions in this regard.26 The utilization of ANC, delivery, and PNC services is more among autonomous women than those whose spending is controlled by other people.42,43
Conclusions
The findings of the study showed that there was inequality in reproductive and maternal health service utilization in Oromia region. The socio-economic factors such as residence, educational status, and economic status were the determinants of inequity. Uptake of key reproductive and maternal health services was higher among the more privileged women in terms of socio-economies. In the region, women who were educated, in the highest wealth quintile, and living in urban settings were taking advantage of health services compared to their counterparts. Despite most maternal health services being free of charge at the public health facilities, there was variation in the uptake of facility delivery services by women. Most of the poor, uneducated, and rural women had received delivery services from traditional birth attendants in the region. This phenomenon significantly impacts the effort towards reducing maternal mortality in the country.
Beyond the observed inequities across socio-economic factors in the region, this study revealed that more women utilized antenatal care services than facility birth and postnatal care, implying significant dropout rate across the maternal care continuum. This is against the fact that antenatal care is an entry point for all maternal health services and requires enhancing the utilization of prenatal, delivery and postnatal care by women.
The efforts toward improving the coverage of key reproductive and maternal health interventions should consider equity in the distribution of services. If health is considered as the right of citizens, equity related targets should be given due attention.
Several approaches had been used to tackle inequity in access and utilization of maternal health services. Financial protection programs (eg, cash transfer and maternal vouchers schemes), inclusiveness programs (eg, youth friendly service centers), and task shifting of health professionals as an approach had been successful in improving maternal health services access and utilization in different countries. Maternity waiting homes approach is also used by countries to narrow geospatial inequalities in access and utilization of maternal healthcare. The global large scale approaches and multisector programs focused on maternal services are also successful ones.44 Evidence from rural Bangladesh indicated that, if effectively used, community level interventions similar to the Ethiopian health extension program could sustain equity in maternal health service utilization.45 Furthermore, disparity in health service access and utilization can be avoidable through tackling the socio-cultural and infrastructural barriers. Obviously, though, this demands multisectoral collaboration. More specifically, one area of focus should be women empowerment or improving household level women's decision-making power. Equity gaps caused by access and coverage of health services can be addressed through infrastructural expansion and also strengthening outreach service programs for some maternal health services, especially for those in the hard to reach areas.
Funding Statement
There is no funding to report.
Data Sharing Statement
The dataset was made available for public use after de-identification (data are available online at: https://www.idhsdata.org/idhs/).
Ethical Approval
Ethics approval was not required for the current analysis, as the data were from publicly available DHS data. The MEASURE DHS/ICF International, Rockville, Maryland, USA – granted access to data upon request.
Consent for Publication
Not applicable.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declared that they had no competing interests for this work.
References
- 1.Braveman P, Gruskin S. Defining equity in health, theory and methods. J Epidemiol Community Heal. 2003;57:254–258. doi: 10.1136/jech.57.4.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitehead M The concepts and principles of equity and health. WHO Regional office for Europe: Copenhagen; 1985. Available from: https://www.ncbi.nlm.nih.gov/pubmed/1644507. Accessed September28, 2020. [Google Scholar]
- 3.Alkenbrack S, Chaitkin M, Zeng W, Couture T, Sharma S, Leone T. Did equity of reproductive and maternal health service coverage increase during the MDG era? An analysis of trends and determinants across 74 low- and middle- income countries. PLoS One. 2015;10(9):e0134905. doi: 10.1371/journal.pone.0134905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Children’s Fund. Analysis of reproductive, maternal, newborn, child and adolescent health inequities in Latin America and the Caribbean to inform policymaking summary report. Health Equity Report 2016. 2016.
- 5.Wang W. Assessing Trends in Inequalities in Maternal and Child Health and Health Care in Cambodia. DHS Further Analysis Reports No. 86. Calverton. Maryland, USA: ICF International; 2013. [Google Scholar]
- 6.Karim AM, Tamire A, Medhanyie AA, Betemariam W. Changes in equity of maternal, newborn, and child health care practices in 115 districts of rural Ethiopia: implications for the health extension program. BMC Pregnancy Childbirth. 2015;15:238. doi: 10.1186/s12884-015-0668-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bobo FT, Yesuf EA, Woldie M. Inequities in utilization of reproductive and maternal health services in Ethiopia. Int J Equity Health. 2017;16:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barros AJD, Ronsmans C, Axelson H, et al. Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. 2012;379:1225–1233. [DOI] [PubMed] [Google Scholar]
- 9.Pradhan J, Arokiasamy P. Socio-economic inequalities in child survival in India: a decomposition analysis. Health Policy (New York). 2010;98(2–3):114–120. doi: 10.1016/j.healthpol.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 10.Houweling TA, Kunst AE. Socio-economic inequalities in childhood mortality in low- and middle-income countries: a review of the international evidence. Br Med Bull. 2010;93:7–26. doi: 10.1093/bmb/ldp048 [DOI] [PubMed] [Google Scholar]
- 11.Zere E, Oluwole D, Kirigia JM, Mwikisa CN, Mbeeli T. Inequities in skilled attendance at birth in Namibia: a decomposition analysis. BMC Pregnancy Childbirth. 2011;11:34. doi: 10.1186/1471-2393-11-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.USAID. Levels and trends in maternal and child health disparities by wealth and region in eleven countries with DHS surveys. DHS comparative reports 42; 2016. Available from: https://dhsprogram.com/pubs/pdf/CR42/CR42.pdf. Accessed September28, 2020.
- 13.WHO, UNICEF, UNFPA WBG and the UNP division. Trends in maternal mortality: 2000 to 2017. Geneva.2019. Licence: CC BY-NC-SA 3.0 IGO; 2019. Available from: http://documents.worldbank.org/curated/en/793971568908763231/pdf/Trends-in-maternal-mortality-2000-to-2017-Estimates-by-WHO-UNICEF-UNFPA-World-Bank-Group-and-the-United-Nations-Population-Division.pdf. Accessed September28, 2020.
- 14.Zhang R, Li S, Li C, et al. Socioeconomic inequalities and determinants of maternal health services in Shaanxi Province, Western China. PLoS One. 2018;13(9):e0202129. doi: 10.1371/journal.pone.0202129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yaya S, Ghose B. Global inequality in maternal health care service utilization: implications for sustainable development goals. Health Equity. 2019;3(1):145–154. doi: 10.1089/heq.2018.0082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saxena D, Vangani R, Mavalankar DV, Thomsen S. Inequity in maternal health care service utilization in Gujarat: analyses of district-level health survey data. Glob Health Action. 2013;6:1–9. doi: 10.3402/gha.v6i0.19652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nghargbu R, Olaniyan O. Inequity in maternal and child health care utilization in Nigeria. Afri Dev Rev. 2017;29(4):630–647. doi: 10.1111/1467-8268.12301 [DOI] [Google Scholar]
- 18.Yaya S, Uthman OA, Amouzou A, Ekholuenetale M, Bishwajit G. Inequalities in maternal health care utilization in Benin: a population based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):194. doi: 10.1186/s12884-018-1846-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ejeta E. Inequalities in the utilization of maternal health services by key indicators in Ethiopia. J Heal Med Nurs. 2017;39:96–103. [Google Scholar]
- 20.Memirie ST, Verguet S, Norheim OF, et al. Inequalities in utilization of maternal and child health services in Ethiopia: the role of primary health care. BMC Health Serv Res. 2016;16:51. doi: 10.1186/s12913-016-1296-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anwar I, Sami M, Akhtar N, et al. Inequity in maternal health-care services: evidence from home-based skilled-birth-attendant programmes in Bangladesh. Bull World Health Organ. 2008;86(4):252–259. doi: 10.2471/blt.07.042754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gebre E, Worku A, Bukola F. Inequities in maternal health services utilization in Ethiopia 2000–2016: magnitude, trends, and determinants. Reprod Health. 2018;15(1):119. doi: 10.1186/s12978-018-0556-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novignon J, Ofori B, Tabiri KG, Pulok MH. Socioeconomic inequalities in maternal health care utilization in Ghana. Int J Equity Health. 2019;18(1):141. doi: 10.1186/s12939-019-1043-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mezmur M, Navaneetham K, Letamo G, et al. Socioeconomic inequalities in the uptake of maternal healthcare services in Ethiopia. BMC Health Serv Res. 2017;17:367. doi: 10.1186/s12913-017-2298-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vadrevu L, Kanjilal B. Measuring spatial equity and access to maternal health services using enhanced two step floating catchment area method (E2SFCA) - a case study of the Indian Sundarbans. Int J Equity Health. 2016;15:87. doi: 10.1186/s12939-016-0376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Central Statistical Agency (CSA) and ICF. Ethiopia demographic and health survey; 2016. Available from: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf. Accessed September28, 2020.
- 27.CSA and ICF. Mini demographic and health survey 2019: key indicators [Internet]; 2019. Available from: https://dhsprogram.com/pubs/pdf/PR120/PR120.pdf. Accessed September28, 2020.
- 28.United Nations. Transforming our world: the 2030 agenda for sustainable development. Available from: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication. Accessed September28, 2020.
- 29.FMoH of Ethiopia. Health Sector Transformation Plan (HSTP) 2015/16–2019/20; 2015. Available from: https://www.globalfinancingfacility.org/ethiopia-health-sector-transformation-plan-201516-201920. Accessed September28, 2020.
- 30.WHO. Anchoring universal health coverage in the right to health: what difference would it make? Policy brief. p. 32 Available from: http://www.who.int/gender-equity-rights/knowledge/anchoring-uhc.pdf. Accessed September28, 2020.
- 31.Ooms G, Latif LA, Waris A, et al. Is universal health coverage the practical expression of the right to health care? BMC Int Health Hum Rights. 2014;14:3. doi: 10.1186/1472-698X-14-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization. State of inequality: reproductive, maternal, newborn and child health; 2015. Available from: https://www.who.int/docs/default-source/gho-documents/health-equity/state-of-inequality/state-of-inequality-reproductive-maternal-new-born-and-child-health.pdf?sfvrsn=f4034289_2. Accessed September28, 2020.
- 33.Hajizadeh M, Alam N, Nandi A. Social inequalities in the utilization of maternal care in Bangladesh: have they widened or narrowed in recent years? Int J Equity Health. 2014;13:120. doi: 10.1186/s12939-014-0120-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Makate M, Makate C. The evolution of socioeconomic status-related inequalities in maternal health care utilization: evidence from Zimbabwe, 1994–2011. Glob Health Res Policy. 2017;2:1. doi: 10.1186/s41256-016-0021-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alam N, Hajizadeh M, Dumont A, Fournier P, Carpenter DO. Inequalities in maternal health care utilization in Sub-Saharan African countries: a multiyear and multi-country analysis. PLoS One. 2015;10(4):e0120922. doi: 10.1371/journal.pone.0120922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Asamoah BO, Agardh A, Pettersson KO, et al. Magnitude and trends of inequalities in antenatal care and delivery under skilled care among different socio-demographic groups in Ghana from 1988 – 2008. BMC Pregnancy Childbirth. 2014;14:295. doi: 10.1186/1471-2393-14-295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abekah-Nkrumah G. Trends in utilisation and inequality in the use of reproductive health services in Sub-Saharan Africa. BMC Public Health. 2019;19:1541. doi: 10.1186/s12889-019-7865-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ethiopian Public Health Institute. Ethiopia service availability and readiness assessment 2016 summary report; 2016. Available from: https://www.ephi.gov.et/images/pictures/download2009/v6FinalSARAReportJan2017.pdf.
- 39.Ethiopian Public Health Institute. Services Availability and Readiness Assessment (SARA); 2018. Available from: https://www.researchgate.net/project/The-Ethiopian-health-Service-Provision-Assessment-SPA-service-availability-and-readiness-assessment-SARA-at-national-level-and-evaluation-of-the-optimization-of-health-extension-program-OHEP.
- 40.Yakob B, Gage A, Nigatu TG, et al. Low effective coverage of family planning and antenatal care services in Ethiopia. Int J Qual Heal Care. 2019;31(10):725–732. [DOI] [PubMed] [Google Scholar]
- 41.Zegeye K, Gebeyehu A, Melese T. The role of geographical access in the utilization of institutional delivery service in Rural Jimma Horro District, Southwest Ethiopia. Primary Health Care. 2014;4:150. doi: 10.4172/2167-1079.1000150 [DOI] [Google Scholar]
- 42.Ousman SK, Mdala I, Thorsen VC, Sundby J, Magnus JH. Social determinants of antenatal care service use in Ethiopia: changes over a 15-year span. Public Health. 2019;7:1–10. doi: 10.3389/fpubh.2019.00161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14:161. doi: 10.1186/1471-2393-14-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tull K. Inequity and Leave No One Behind: Approaches to Maternal and Newborn Healthcare. K4D: Knowledge, Evidence and Learning for Development. University of Leeds Nuffield Centre for International Health and Development; 2019. [Google Scholar]
- 45.Quayyum Z, Khan MNU, Quayyum T, et al. “Can community level interventions have an impact on equity and utilization of maternal health care” – evidence from rural Bangladesh. Int J Equity Health. 2013;12:22. doi: 10.1186/1475-9276-12-22 [DOI] [PMC free article] [PubMed] [Google Scholar]