Abstract
Introduction
The aim of this research was to describe a single-center practical experience in the management of traumatic carotid cavernous fistula (CCF).
Methods
There were a total of 31 patients between January 2005 and December 2019 with post-traumatic carotid cavernous sinus fistula (tCCF) who underwent treatment. We classified them into 2 types according to the flow of the CCF: patients with high flow CCF and patients with low flow CCF.
Results
Angiography revealed the high flow types on 21 patients (67.7%), the mean of patients ages are 31.5 years. Onyx embolization was performed in 1 patient (4.76%), transarterial balloon embolization was carried out in 10 patients (47.61%), transarterial coiling in 3 (14.28%) patients while 5 (28.8%) patients underwent transvenous routes to insert the coil and 2 patients (9.52%) were treated conservatively. Complete occlusion was achieved on all patients with coiling whereas the other treatment experiences the reducing flow of the fistula. We obtained 10 patients (32.2%) with a mean of 40.3 years as low flow type CCF. The patients with the low flow type mostly treated conservatively, because their symptoms were acceptable and intermittent.
Conclusion
The ballooning currently became the more affordable treatment in our center. Balloon embolization was recommended for medium- and large-size fistula. The coils should be recommended for small-size fistula. In some cases occlusion of the fistula cannot be obtained using the detachable balloon, a coil can be used to occlude the cavernous sinus via trans arterial or trans venous access. If the fistula failed to be treated in traditional ways using balloons or coils, occlusion of the parent vessels could be another option.
Keywords: trauma, carotid cavernous sinus fistula, angiography, embolization, transarterial, transvenous
Introduction
Carotid cavernous fistulas (CCFs) are uncommon vascular anomalies associated with head trauma. It may be classified either as direct type (containing the internal carotid artery) or indirect type (involving the dural branch). The direct type is typically traumatic and high flow, while the indirect type (also called a dural fistula) is typically accidental and low flow. CCF classification as direct versus indirect can be strengthened as the focus is relevant to its vascular anatomy and treatment modality. CCF is an unusual communication between the dural branches of the internal and external carotid artery to the intracranial venous pressure with the risk of venous infarction, neurological or intracranial dysfunction and the cavernous sinus.1
Clinical manifestations of post-traumatic CCF (tCCF) rely on venous drainage patterns. Reversing blood flow through the upper eye vein (superior orbital vein/SOV) leads to many eye symptoms, including proptosis, chemosis, conjunctival arterialization, a paresis in the eyes, retroorbital pain, elevated intraocular pressure (IOP) and visual acuity. Such clinical manifestations and signs are usually moderate to extreme, and at first life threatening, because the shunt is still high in flow and pressure.2–4 Manual carotid artery compression in some patients has been shown to be effective.5 TCCF can cause morbidity, especially when combined with retrograde cortical venous drainage, including blindness, seizure, stroke, and intracranial hemorrhage.6 More intensive care is needed in patients with intractable or worsening symptoms or in the case of retrograde cortical venous drainage.
Current management is predominantly endovascular and, due to higher clinical and anatomical cure levels and a lower incidence of complications, the venous (transvenous route) methods are preferred to the trans arterial route.5–7 Mullan8 and Hosobuchi9 first identified the technique of the transvenous embolization. Upon surgical exposure, both inserted small copper wires and thrombogenic material straight into the cavernous sinus. The endovascular routes were subsequently used to insert thrombogenic material, normally platinum coils, into the cavernous sinus.
In this article, we describe our experience in the endovascular treatment and the clinical outcomes in 31 patients with tCCF. We discuss the different techniques that have been used in our center to treatCCF with endovascular approaches.
Patients and Methods
We analyzed the data from patients records who were managed for CCF from January 2005 to December 2019. A total of 31 patients with tCCF were treated in Kariadi Hospital. The patients were classified into two types according to the flow of the fistula; patients with high flow CCF; and patients with low flow CCF.
Patients were examined by CT scan and cerebral angiography. The purposes of pre-treatment diagnostic cerebral angiography were to determine the terms, side, and flow rate of the fistula, the collateral circulation patency, the pattern of venous flow of the fistula and the best route to treat the fistula. The main purposes of treatment for the CCF was to reduce the flow or totally occlude the fistula.
In traumatic CCF cases, it is not easy to assess the exact position of the fistulous opening inside the ICA. During cerebral diagnostic angiography, a procedure that the ICA manually compress during vertebral injection with the intention of reversing the flow in the ICA through the posterior communication artery (P-com) that can help delineate the upper boundary of the fistula opening (Allcock maneuver). The slow injection technique of the ICA wounded during selective angiography may also help delineate the upper boundary of the fistula opening.
Our treatment guideline was embolization with coiling, onyx, gold balloon, or carotid ligation and some patients were treated conservatively by compressing the carotid artery with the contralateral hand. The patient was followed up after treatment and the clinical symptoms (exophthalmos, chemosis or an audible bruit) were evaluated. The decision to treat or not depended on the national insurance coverage of device. Private patients who could afford the coil were treated with coil embolization.
Therapeutic Approach
Trans arterial embolization was performed under local anaesthesia and via femoral arterial access. Systemic heparinization was obtained using un-fractionated heparin with a bolus of 5000 IU and a maintenance dose of 1000 IU/h to maintain activated coagulation time twice of normal. A 6-Fr guiding was placed in the ipsilateral ICA for transarterial coil embolization. The coils were deployed into the cavernous sinus to pack the cavernous sinus. In another approach, combination with onyx was considered. Onyx compatible Microcatheter was used in designated cases. The technique used was made up of two different steps. The coils were deployed into the cavernous sinus to make a scaffold inside the cavernous sinus. The coils were sized according to the diameter of the cavernous sinus. When the scaffold covered most of the sinus, injection of Onyx was started. Onyx was injected under radiographic control, until there was complete occlusion of the fistula. On observation that in the presence of high flow across the fistula, there was preferential antegrade flow of Onyx into the cavernous sinus, and there was no reflux towards the microcatheter; a balloon was not used in subsequent cases. In patients where a balloon was not used, great care was taken to stop the injection as soon as any reflux was noted towards the microcatheter. The microcatheter was always placed deep inside the cavernous sinus, away from site of the rent to minimize the chance of reflux of Onyx into ICA.
A 8-Fr guiding for transarterial balloon embolization was placed in the ipsilateral ICA. A Gold balloon embolization was applied into the cavernous sinus. Arteriography was performed for occlusion status after the balloon was deployed.
Transvenous embolization was achieved via the transfemoral route and inferior petrosal sinus (IPS) pathway. Under local anaesthesia, the femoral vein was punctured and a 6F sheath was introduced. A 6-F guide catheter was placed in the orifice of the inferior petrosal sinus. Through it, a microcatheter was navigated co-axially into the ipsilateral cavernous sinus. Thrombogenic micro coils were then placed within the sinus starting from superior ophthalmic vein (SOV). Embolization using GDC coils was performed.
Ethical Consideration
This research was approved by the Institution Review Board of Kariadi General Hospital, in accordance with the Helsinki declaration. Prior written informed consent was obtained from all patients to be included in this study. For patients under the age of 18 years, informed consent was obtained from a parent and/or legal guardian. Prior written informed consent was obtained from the patients in the figures. For patients in the figures under the age of 18 years, informed consent was obtained from a parent and/or legal guardian.
Results
A total of 31 patients have been evaluated (Table 1). Angiography revealed the type of CCF was high flow on 21 patients (67.7%), The patient ages ranged from 7 to 55 years, with a mean of 31.5 years. All patients had ocular symptoms consisting ofproptosis, chemosis, and conjunctival hypervascularity (Figure 1) and abnormality of the eye movement. The etiology of the CCF for all patients was traffic accident. The onset varies from 2 months until 24 months. In this high flow type, we were able to identify the fistula mostly on C3-C5 segment (Figure 2). Patients with high flow type of CCF treated with Onyx embolization was 1 patient (4.76%), Transarterial balloon embolization was carried out in 10 patients (47.61%) (Figure 3), transarterial coiling in 3 (14.28%) patients while 5 (23.8%) patients underwent transvenous routes to insert the coil (Figures 4–6), and 2 patients (9.52%) were treated conservatively. Complete occlusion was achieved on all patients treated with the coiling method. This result was evaluated using angiography after the treatment was given to the patient. The 12 patients who were treated with transarterial balloon embolization and by compressing the common carotid artery, experienced the reduced flow of the fistula.
Table 1.
Data from 31 Patient Treated in Kariadi Hospital from January 2005 to December 2019. The Patients with High Flow Types Were 21 Patients (65%), The Patient Ages Ranged from 7 to 55 Years, with a Mean of 31.5 Years
| No | Gender and Ages | Traumatic Onset | CCF Type | Treatment | Pre-Treatment DSA Identification | Treatment Output | |
|---|---|---|---|---|---|---|---|
| 1 | P | 43 | 4 | CCF high Flow | Coiling Transarterial | Fistula on right C4–5 segment | Complete Occlusion |
| 2 | L | 16 | 3 | CCF High Flow | Conservative | Fistula on left C4–5 segment patent collateral flow | Incomplete Occlusion |
| 3 | L | 17 | 3 | CCF High Flow | Detachable balloon embolization | Fistula on right C3–4 Segment | Complete Occlusion |
| 4 | L | 18 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on right C4–5 segment | Incomplete Occlusion |
| 5 | L | 20 | 18 | CCF High Flow | Detachable balloon embolization | Fistula on left C3–4 Segment | Complete Occlusion |
| 6 | L | 38 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on right C4–5 segment | Incomplete Occlusion |
| 7 | P | 22 | 4 | CCF High Flow | Onyx embolization | Fistula on right C3–4 Segment | Incomplete Occlusion |
| 8 | P | 28 | 3 | CCF High Flow | Coiling Transarterial | Fistula on right C4 segment | Complete Occlusion |
| 9 | P | 31 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on right C3–4 Segment | Complete Occlusion |
| 10 | L | 49 | 3 | CCF High Flow | Detachable balloon embolization | Fistula on right C3–4 Segment | Incomplete Occlusion |
| 11 | L | 37 | 5 | CCF High Flow | Detachable balloon embolization | Fistula on Left C3 segment | Incomplete Occlusion |
| 12 | L | 46 | 2 | CCF High Flow | Conservative | Fistula on left C3–4 Segment | Incomplete Occlusion |
| 13 | P | 22 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on left C4–5 Segment | Incomplete Occlusion |
| 14 | P | 33 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on left C4 Segment | Incomplete Occlusion |
| 15 | L | 35 | 3 | CCF High Flow | Coiling Transarterial | Fistula on right C3 segment | Complete Occlusion |
| 16 | L | 23 | 4 | CCF High Flow | Coiling Transvenous | Fistula on right C5 segment | Complete Occlusion |
| 17 | L | 45 | 2 | CCF High Flow | Coiling Transvenous | Fistula on left C5 segment | Complete Occlusion |
| 18 | P | 55 | 3 | CCF High Flow | Coiling Transvenous | Fistula on right C5 segment | Complete Occlusion |
| 19 | P | 38 | 2 | CCF High Flow | Coiling Transvenous | Fistula on right C4 segment | Complete Occlusion |
| 20 | L | 31 | 1 | CCF High Flow | Coiling Transvenous | Fistula on left C4 segment | Complete Occlusion |
| 21 | L | 40 | 2 | CCF High Flow | Detachable balloon embolization | Fistula on left C3 segment | Complete Occlusion |
| 22 | P | 19 | 18 | CCF Low Flow | Conservative | Fistula on right dural branches to cavernous sinus | Incomplete Occlusion |
| 23 | P | 54 | 5 | CCF Low Flow | Conservative | Fistula on right ICA branches in cavernous sinus | Incomplete Occlusion |
| 24 | P | 57 | 12 | CCF Low Flow | Conservative | Fistula from dural branches to left cavernous sinus | Incomplete Occlusion |
| 25 | P | 37 | 18 | CCF Low Flow | Conservative | Fistula from right meningeal branches from internal maxillary artery | Incomplete Occlusion |
| 26 | P | 26 | 6 | CCF Low Flow | Conservative | Fistula from right meningeal branches from internal maxillary artery | Incomplete Occlusion |
| 27 | P | 8 | 2 | CCF Low Flow | Conservative | Fistula on right ICA branches in cavernous sinus | Incomplete Occlusion |
| 28 | L | 55 | 8 | CCF Low Flow | Onyx embolization | Fistula from meningeal branches from internal maxillary artery | Incomplete Occlusion |
| 29 | L | 61 | 8 | CCF Low Flow | Conservative | Fistula from left meningeal branches from internal maxillary artery | Incomplete Occlusion |
| 30 | P | 34 | 17 | CCF Low Flow | Conservative | Fistula from left meningeal branches from internal maxillary artery | Incomplete Occlusion |
| 31 | P | 52 | 12 | CCF Low Flow | Conservative | Fistula on left ICA branches in cavernous sinus | Incomplete Occlusion |
Figure 1.
Sign exophthalmos, chemosis.
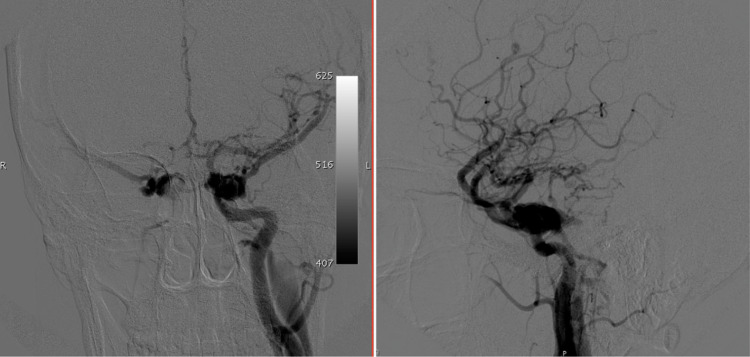
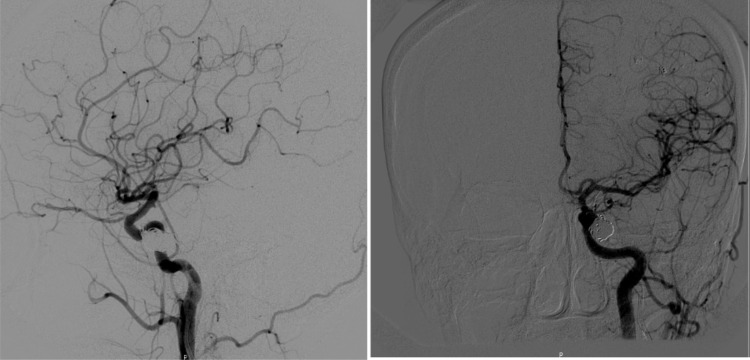
Figure 2.
Angiography showed CCF, fistula at C5–C4 internal carotid artery segment. The drainage of the vein was through the cavernous sinus, the upper or lower petrosal sinus to the sigmoid sinus, and via the variceal upper petrosal vein to the deep Galenic system.
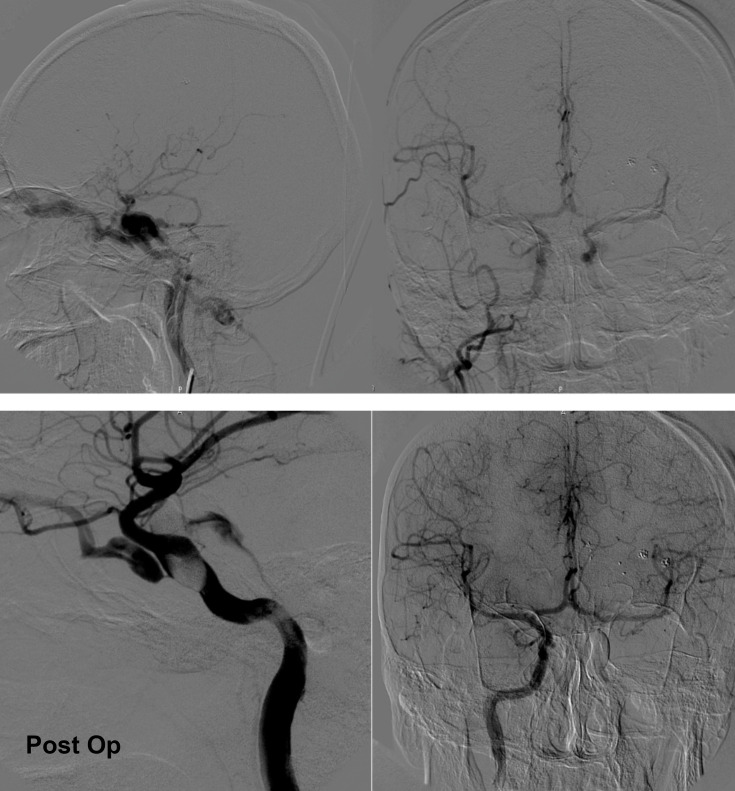
Figure 3.
Trans arterial Gold Ballon occlusion.
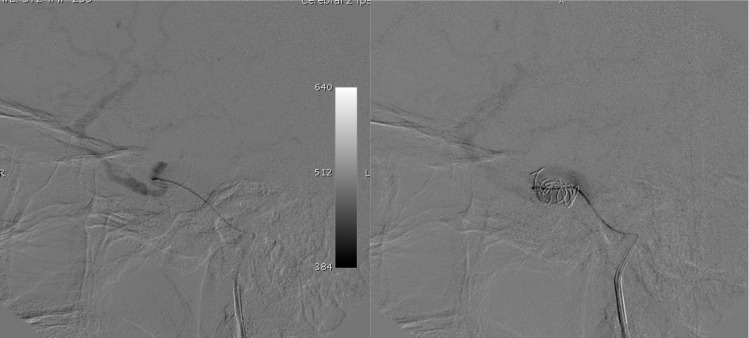
Figure 4.
A 7 F angiography catheter, Trans femoral venous entry, was located just below the jugular foramen. Then a microcatheter was directed to the cavernous sinus through jugular bulb and inferior petrosal sinus. The tip then was inserted in the upper orbital vein and the coils were removed in it and at the fistula to minimize shunt flow.
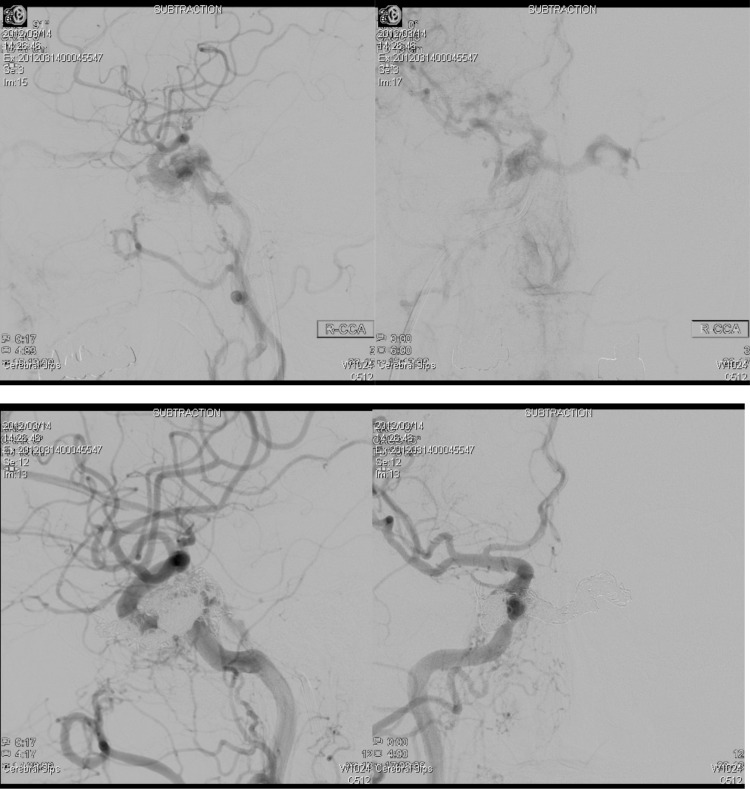
Figure 6.
Transarterial coil embolization. (Upper left and upper right) Showed the fistula come from ICA segment C3–4. (Lower left and lower right) revealed no more extravasation contrast on cavernous sinus after filled with detachable coils.
Eight patients were treated with coiling. We divided them into 2 types of approach, the transarterial approach (3 patients) and transvenous approach (5 patients). The patients who underwent CCF treatment with transarterial coiling approach were found to have fistula on right C4–5 segment (1 patient), 1 patient with Fistula on right C4 segment, and 1 patient Fistula on right C3 segment (Table 2). The patients with transvenous approach were 3 with fistula on C5 segment and 2 with fistula C4 segment (Table 3).
Table 2.
Data from Patient with Transarterial Approach
| No | Gender and Ages | Traumatic Onset | CCF Type | Treatment | Pre-Treatment DSA Identification | Treatment Output | |
|---|---|---|---|---|---|---|---|
| 1 | P | 43 | 4 | CCF high Flow | Coiling Transarterial | Fistula on right C4–5 segment | Complete Occlusion |
| 2 | P | 28 | 3 | CCF High Flow | Coiling Transarterial | Fistula on right C4 segment | Incomplete Occlusion |
| 3 | L | 35 | 3 | CCF High Flow | Coiling Transarterial | Fistula on right C3 segment | Complete Occlusion |
Table 3.
Data from Patient with Transvenous Approach
| No | Gender and Ages | Traumatic Onset | CCF Type | Treatment | Pre-Treatment DSA Identification | Treatment Output | |
|---|---|---|---|---|---|---|---|
| 1 | L | 23 | 4 | CCF High Flow | Coiling Transvenous | Fistula on right C5 segment | Complete Occlusion |
| 2 | L | 45 | 2 | CCF High Flow | Coiling Transvenous | Fistula on left C5 segment | Complete Occlusion |
| 3 | P | 55 | 3 | CCF High Flow | Coiling Transvenous | Fistula on right C5 segment | Complete Occlusion |
| 4 | P | 38 | 2 | CCF High Flow | Coiling Transvenous | Fistula on right C4 segment | Complete Occlusion |
| 5 | L | 31 | 1 | CCF High Flow | Coiling Transvenous | Fistula on left C4 segment | Complete Occlusion |
Ten patients had low flow types(32.2%). The patient ages ranged from 8 to 61 years, with a mean of 40.3 years. The patients with the low flow type were mostly treated conservatively because their symptoms were acceptable and intermittent, except for 1 patient; patient number 28 underwent onyx embolization because the symptoms were not tolerable for him. Embolization was applied to occlude the fistula and the patient gained incomplete occlusion of the fistula but the symptoms become tolerable.
Discussion
CCFs most often occur after head injuries. Direct high flow arteriovenous contact between the ICA and cavernous sinuses. Until recently, selective balloon embolism of the CCF with protection of the ICA was seen. However, this was released in just 60–88% of the series. The treatment is not risk-free and lifelong deficits can occur after therapy.
Since detachable balloons were first introduced in 1974 by Serbinenko, this endovascular approach has been recommended in treatment of CCF for a long time, before its use changed with the advent of new technologies, such as coils and stents. A detachable balloon will cover the fistula while maintaining the patency of ICA.10,11 This method is inflexible so it depends on the structure of the ICA. Beside that, there are some matters for consideration before choosing this technique to treatm tCCF: 1) The diameter of the fistula is about the same as the Inflated balloon, but big enough to use the balloon deflated or partly inflated; 2) The volume of blood via the fistula is adequate for the passage to the basket; and 3) The CS is big enough to accommodate the balloon for the full occlusion of the fistula. Technical failure to deploy the stent across the opening of the fistula would result in endoleak, which would result in preserving the fistula. Another disadvantage reported by some studies is the complication of this technique; such as it can occlude main venous drainage, and cause cranial nerves palsy. It is usually solved by inserting a larger size balloon, then re-dilatating the stent.10,12,13
The more thrombogenic agent, fiber platinum coils which are placed in the cavernous sinus, and transvenous coil embolization has been the preferred are protocol for CCF. The coil is an embolic substance that is tightly regulated. Coils have the advantages of quick movement, removal, exchange and recovery, and the catheter is easily transarterially or transvenously navigated to the cavernous sinus.14,15 The fistula was conveniently connected by placing the coils near the fistula from the arterial side without falling into the parent artery. It has also been demonstrated for a long time as a safe and successful treatment that can lead to symptoms being relieved in many patients.16 The IPS has been the route of choice since it is the fastest and simplest path to the cavernous sinus. In all of our transvenous approaches, we directed the coil through IPS as seen in one of our example procedures shown in Figures 4 and 5. A coil should be placed and rotated several times until the best position is found; the balloon or conventional micro coils are difficult to handle. For all high flow patients who have been coiled, we effectively occlude CCF. The transarterial or transvenous route typically approaches for tCCFs. Both, the transarterial and transvenous approach was satisfactory to us.
Figure 5.
Post coil embolization.
Onyx will overshadow CS fistulas completely and permanently, it has a strong radiographical representation, and there is also no chance of overpackaging and hence reduced cranial nerve defects are potentially correlated with Onyx. Onyx can be used as a single embolize for low flow fistulas and detachable coils as seen in our case.20,21 Their non-adhesive properties minimize the risk of a microcatheter sticking and allow long injecting into different areas, as well as into drying veins and branches. The onyx can be used as a single embolizing agent. This is rather beneficial in case of tortuous vein structures and small fistulas and rewind distal navigation and adequate coiling of the microcatheter.20,22,23
Conclusion
High flow CCFs are uncommon vascular lesion related to head injuries. Knowledge of complex angioarchitecture and multiple pathways of access is crucial for the correct treatment as its management. Techniques and methods of treatment are coils, GBs or liquid embolic; each technique has its advantages and disadvantages. Therefore, knowledge of the methods is essential for the treatment scheme and for choosing the approach. Due to health insurance coverage policy, not all the patient with CCF in our center have been permitted to undergo coil embolization. The ballooning currently becomes the more affordable treatment in our center for this issue. Balloon embolization was recommended for medium- and large-size fistulae. The coils should be recommended for small-size fistulae.
In cases occlusion of the fistula cannot be obtained using detachable balloon, a coil can be used to occlude the cavernous sinus via trans arterial or trans venous access. If the fistula cannot be treated in the traditional way by using balloons or coils, occlusion of the parent vessels could be another option.
Endovascular procedures are rapidly expanding the range of treatment options for cerebrovascular diseases. However, rigorous assessment and understanding of these procedures is necessary to ensure safe, effective, and appropriate use.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985;62(2):248–256. doi: 10.3171/jns.1985.62.2.0248 [DOI] [PubMed] [Google Scholar]
- 2.Adam CR, Shields CL, Gutman J, et al. Dilated superior ophthalmic vein: clinical and radiographic features of 113 cases. Ophthal Plast Reconstr Surg. 2017. doi: 10.1097/IOP.0000000000000872 [DOI] [PubMed] [Google Scholar]
- 3.Pashapour A, Mohammadian R, Salehpour F, et al. Long-term endovascular treatment outcome of 46 patients with cavernous sinus dural arteriovenous fistulas presenting with ophthalmic symptoms. A non-controlled trial with clinical and angiographic follow-up. Neuroradiol J. 2014;27(4):461–470. doi: 10.15274/NRJ-2014-10079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henderson A, Miller N. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye. 2018;32(2):164–172. doi: 10.1038/eye.2017.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrade G, Ponte de Souza MLP, Marques R, Silva JL, Abath C, Azevedo-Filho HRC. Endovascular treatment of traumatic carotid cavernous fistula with balloon-assisted sinus coiling. A technical description and initial results. Interv Neuroradiol. 2013;19(4):445–454. doi: 10.1177/159101991301900407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma K, Agarwal R, kanaujia V, et al. Carotid-Cavernous Fistula: natural history and clinical profile. Angiology. 2018;6:208. [Google Scholar]
- 7.Higashida RT, Hieshima GB, Halbach VV, Bentson JR, Goto K. Closure of carotid cavernous sinus fistulae by external compression of the carotid artery and jugular vein. Acta Radiol Suppl. 1986;369:580–583. [PubMed] [Google Scholar]
- 8.Ohlsson M, Consoli A, Rodesch G. Endovascular treatment of carotico-cavernous fistulas with acrylic glue: a series of nine cases. Neuroradiology. 2016;58(12):1181–1188. doi: 10.1007/s00234-016-1760-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mullan S. Treatment of carotid-cavernous fistulas by cavernous sinus occlusion. J Neurosurg. 1979;50(2):131–144. doi: 10.3171/jns.1979.50.2.0131 [DOI] [PubMed] [Google Scholar]
- 10.Halbach VV, Higashida RT, Hieshima GB, Hardin CW, Pribram H. Transvenous embolization of dural fistulas involving the cavernous sinus. AJNR Am J Neuroradiol. 1989;10(2):377–383. [PMC free article] [PubMed] [Google Scholar]
- 11.Wolpert SMIR. In re: Serbinenko FA. Balloon catheterization and occlusion of major cerebral vessels. J Neurosurg 1974;41:1974. AJNR Am J Neuroradiol. 2000;21(7):1359–1360. [PMC free article] [PubMed] [Google Scholar]
- 12.Li J, Lan Z-G, Xie X-D, et al. Traumatic carotid-cavernous fistulas treated with covered stents: experience of 12 cases. World Neurosurg. 2010;73(5):514–519. doi: 10.1016/j.wneu.2010.02.062 [DOI] [PubMed] [Google Scholar]
- 13.Wang C, Xie X, You C, et al. Placement of covered stents for the treatment of direct carotid cavernous fistulas. AJNR Am J Neuroradiol. 2009;30(7):1342–1346. doi: 10.3174/ajnr.A1583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosobuchi Y. Electrothrombosis of carotid-cavernous fistula. J Neurosurg. 1975;42(1):76–85. doi: 10.3171/jns.1975.42.1.0076 [DOI] [PubMed] [Google Scholar]
- 15.Alexander MD MD, Halbach VV MD, Hallam DK MD, et al. Long-term outcomes of endovascular treatment of indirect carotid cavernous fistulae: superior efficacy, safety, and durability of transvenous coiling over other techniques. Neurosurgery. 2019;85(1):E94–E100. doi: 10.1093/neuros/nyy486 [DOI] [PubMed] [Google Scholar]
- 16.Niu Y, Chen T *, Tang J, Jiang Z, Zhu G, Chen Z. Detachable balloon embolization as the preferred treatment option for traumatic carotid-cavernous sinus fistula? Interv Neuroradiol. 2019;1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kocer N, Kizilkilic O, Albayram S, et al. Treatment of iatrogenic internal carotid artery laceration and carotid cavernous fistula with endovascular stent-graft placement. AJNR Am J Neuroradiol. 2002;23(3):442–446. [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez F, Escobar W, Gomez AM, et al. Treatment of carotid cavernous fistulas using covered stents: midterm results in seven patients. AJNR Am J Neuroradiol. 2007;28(9):1762–1768. doi: 10.3174/ajnr.A0636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bink A, Berkefeld J, Luchtenberg M, et al. Coil embolization of cavernous sinus in patients with direct and dural arteriovenous fistula. Eur Radiol. 2009;19(6):1443–1449. doi: 10.1007/s00330-008-1278-1 [DOI] [PubMed] [Google Scholar]
- 20.Gandhi D, Ansari SA, Cornblath WT. Successful transarterial embolization of a Barrow type D dural carotid-cavernous fistula with ethylene vinyl alcohol copolymer (onyx). J Neuroophthalmol. 2009;29(1):9–12. doi: 10.1097/WNO.0b013e318199ce83 [DOI] [PubMed] [Google Scholar]
- 21.Hassan T, Rashad S, Aziz W, Sultan A, Ibrahim T. Endovascular modalities for the treatment of cavernous sinus Arteriovenous Fistulas: a single-center experience. J Stroke Cerebrovasc Dis. 2015;24(12):2824–2838. doi: 10.1016/j.jstrokecerebrovasdis.2015.08.016 [DOI] [PubMed] [Google Scholar]
- 22.Luo C-B, Teng MM-H, Chang F-C, et al. Traumatic indirect carotid cavernous fistulas: angioarchitectures and results of transarterial embolization by liquid adhesives in 11 patients. Surg Neurol. 2009;71(2):216–222. doi: 10.1016/j.surneu.2007.09.032 [DOI] [PubMed] [Google Scholar]
- 23.Mehrzad H, Alam K, Rennie A. The treatment of a dural carotid cavernous fistula (CCF) using Onyx via a transorbital approach: a technical note. Neuroradiology. 2011;53(11):895–898. doi: 10.1007/s00234-010-0799-x [DOI] [PubMed] [Google Scholar]