Abstract
Introduction
Tumors of facial skin are common in upper part of central subunit of face. Defects after resection require a flap, which is pliable, thin, and has a good colour match. Among the various local flaps available paramedian forehead flap is a good option.
Patients and methods
Patients reconstructed with paramedian forehead flap during the period from January 2015 to March 2020 were included in the study. Data regarding the demographic, clinical characteristics, and treatment details was recorded, and analyzed for postoperative complications and cosmetic outcomes.
Results
Paramedian forehead flap reconstruction was performed in 37 patients who were resected for tumor involving upper central subunit of face. Median age of patients was 57 years. Male to female ratio was 1.4:1. All tumors were resected with a negative margin. Nodal disease was managed by superficial parotidectomy only (4/37), superficial parotidectomy along with supra-omohyoid neck dissection (6/37) and modified neck dissection (1/37). In five patients additional buccal mucosa graft was used to reconstruct conjunctiva. Additional flaps were required in two patients in whom nasolabial and mustarde flaps were used. Partial flap loss occurred in one patient. There was no major flap loss. Surgical site infection developed in only one patient, who had partial flap loss. On subjective assessment, nearly 60% patients described their appearance as good.
Conclusion
Facial reconstruction in area of dorsum of nose and medial aspect of both eyelids using paramedian forehead flaps is a simple and quick procedure.
Keywords: Forehead flap, Postoperative outcome, Local flap, Eyelid, Nose
Introduction
Tumors of facial skin are common in upper part of central subunit of face. Resection of these tumors leave defects, which cannot be primarily closed because of proximity and involvement of root/dorsum of nose and eyelids. These defects require a flap, which is pliable, thin, and has a good colour match. Even the best of microvascular tissue transfer will not be good for these defects. Local flaps are ideal. Among the various local flaps available paramedian forehead flap is good, versatile and simple, especially for defects involving dorsum of nose, medial aspect of both eyelids and adjacent skin.1, 2, 3 Use of paramedian flap does not require a plastic surgeon and can be done by the operating surgeon himself. This saves cost and time. Paramedian flap is ideal in resource constrained situation and hospitals where plastic surgeons are not available. We have been using the paramedian forehead flap for defects involving upper part of central subunit of face following resection of tumors. This article describes our experience with the paramedian forehead flap.
Patients and methods
We conducted this retrospective review of practice in the Department of Surgical Oncology, at a tertiary care hospital in North India. Patients undergoing surgery for skin cancer in area of central subunit of face and reconstructed with paramedian forehead flap during the period from January 2015 to March 2020 were included in the study. We have performed paramedian forehead flap reconstruction following resection in patients of cutaneous tumors involving central subunit of face including nose, eyelid and adjacent skin. Data regarding the demographic, clinical characteristics, and treatment details was recorded, and analyzed for postoperative complications and cosmetic outcomes.
Results
Paramedian forehead flap reconstruction was performed in 37 patients who were resected for tumor involving upper central subunit of face (Fig. 1, Fig. 2, Fig. 3, Fig. 4). Median age of patients was 57 years. Male to female ratio was 1.4:1. Details of the site of tumor and their histology are listed in Table 1. All tumors were resected with a negative margin. Wide excision of tumor also included orbital exenteration in two patients. Nodal disease was managed by superficial parotidectomy only (4/37), superficial parotidectomy along with supra-omohyoid neck dissection (6/37) and modified neck dissection (1/37). In five patients additional buccal mucosa graft was used to reconstruct conjunctiva. Additional flaps were required only in two patients in whom defects were large. In one patient in addition to median forehead, nasolabial flap and in another mustarde flap was used (Table 1).
Fig. 1.
Basal cell carcinoma involving central subunit of face.
Fig. 2.
Defect after resection.
Fig. 3.
Paramedian flap.
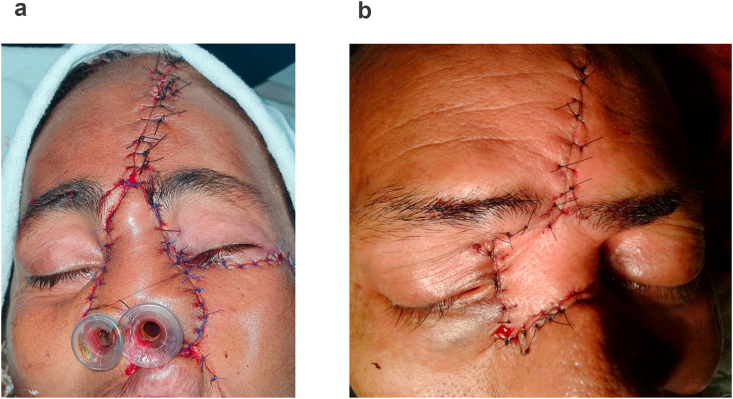
Fig. 4.
Aand b: Reconstruction after suturing the paramedian and mastarde flap.
Table 1.
Patient's details, tumor characteristics, and surgical details.
| Demographic characteristics (N = 37) | |
|---|---|
| Median Age | 57 year |
| Sex (M: F) |
22:15 |
| Tumor site | |
| Eyelid | |
| Lower | 11 (29.7%) |
| Upper | 05 (13.5%) |
| Medial canthus | 05 (13.5%) |
| Face | 09 (24.3%) |
| Nose |
07 (18.9%) |
| Histology | |
| Basal cell carcinoma | 15 (40.5%) |
| Squamous cell carcinoma | 13 (35.1%) |
| Sebaceous cell carcinoma | 06 (16.2%) |
| Adenoid cystic carcinoma | 01 (2.7%) |
| Melanoma | 01 (2.7%) |
| Sarcoma |
01 (2.7%) |
| Treatment of primary | |
| Wide local excision (WLE) alone | 35 (94.5%) |
| WLE with orbital exentration |
02 (5.5%) |
| Nodal dissection | |
| No | 26 (70.2%) |
| Superficial parotidectomy | 11 (29.7%) |
| Supraomohyoid neck dissection | 06 (16.2%) |
| Modified radical neck dissection |
01 (2.7%) |
| Additional flap/Graft | |
| Buccal mucosa graft | 05 (13.5%) |
| Split thickness skin graft | 03 (8.1%) |
| Nasolabial flap | 01 (2.7%) |
| Mustarde flap | 01 (2.7%) |
Immediate postoperative complications are described in Table 2. There was no major flap loss. Minor flap loss was encountered in one patient. Surgical site infection developed in only one patient, who had partial flap loss. This was managed conservatively and did not require any intervention. On subjective assessment, nearly 60% patients described their appearance as good (Fig. 5).
Table 2.
Postoperative complications and cosmesis.
| Post-Operative Complications | Number (%) |
|---|---|
|
Early | |
| Bleeding | 03 (8.1%) |
| Surgical site infection | 01 (2.7%) |
| Partial flap loss | 01 (2.7%) |
| Major flap loss |
0 |
|
Cosmesis | |
| Good | 22 (59.4%) |
| Satisfactory | 12 (32.4%) |
| Poor | 03 (8.1%) |
Fig. 5.
Final cosmetic outcome.
Discussion
There are various options available for cutaneous reconstruction of the central subunit of face after cancer resection and among them paramedian forehead flap is very useful. It has the advantage of being simple, quick and reliable and has minimal morbidity.
History of paramedian forehead flap dates back to 700 BCE in ancient Indian literature where its first description can be found in Sushruta Samhita.4 Centuries later, Kazanjian described the primary blood supply of the flap in the 1930s.The design of this flap was modified and popularized by Labat, Millard and most recently by Burget and Menick. Later described the method, of extending the incision below the orbital rim to add length to this flap5,6, which is used commonly nowadays.
The flap is elevated from cranio-caudal direction including skin, subcutaneous tissue, frontalis muscle and associated fascia or periosteum. There are some important anatomical points which must be considered for raising this flap. This flap is raised in the axial plane of its blood supply from the supratrochlear artery that runs vertically up from orbital rim to hairline,1.7–2.2 cm lateral to the midline at the level of the superior orbital rim.7
Because of superficial location of the blood vessel with extensive distal subdermal plexus, flap necrosis is unusual. The vessels lie in the subcutaneous plane just above the mid-forehead and hence this flap is raised in supraperiosteal plane. Later it can be trimmed of extra tissue to provide pliable skin. However, to protect the blood supply, the inferior aspect of the flap should be elevated deep to the frontalis muscle in subperiosteal plane to safely include the vessel. Base of the flap is generally 1.5 cm wide to include the blood supply safely but can be narrowed up to 1.3 cm. This helps in providing a better rotational arc to the flap. No effort is made to visualize and safeguard the supratrochlear nerve that provides sensation to the skin of the flap. Therefore, these flaps have no sensation. If required, additional length can be gained proximally by extending the incision below the orbital rim which helps to avoid including the hair bearing skin of forehead. The pedicle is generally divided 3 weeks later under local anaesthesia, once the flap has gained a local blood supply from the recipient site.8,9
In a recent large retrospective descriptive study of paramedian forehead flaps for nasal reconstruction the most common complication was postoperative infection in 2.9% patients, followed by postoperative bleeding and DVT in 1.4% and ≤0.5% patients respectively.10 In another series the infection rate was found to be statistically similar between patients undergoing 3 stage and 2 stage paramedian forehead flap reconstruction (5% vs 1%, P = 0.218). Similarly, the rate of partial forehead flap necrosis was similar in both groups (2-stage, 3.4%; 3-stage, 5%; P = 0.601). Authors concluded that there was no evidence to suggest that the use of a 3-stage forehead flap lowers the prevalence of necrosis.11 In a 2001 study of postoperative complications of paramedian flap by Collin L. Chin et al. infection rates were 2.9% and bleeding was1.4%, which is similar to our study.1 In another series of 41 patients of nasal defect, early postoperative complications occurred in 14.6% of patients undergoing paramedian forehead flap reconstruction. The cosmetic results were considered acceptable or excellent in 90.2% of cases.12
Conclusion
Facial reconstruction in area of dorsum of nose and medial aspect of both eyelids using paramedian forehead flaps is a simple and easy procedure. Skin of forehead has good match with the skin of this area in thickness as well as in colour. The result of this reconstruction is highly satisfactory along with good cosmesis. It is also ideal for hospitals where plastic surgeons are not available.
Funding
No funding received.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of competing interest
No conflict of interest.
Contributor Information
Shiv Rajan, Email: shivrajan.194@gmail.com.
Naseem Akhtar, Email: naseemakhtar97@gmail.com.
Vijay Kumar, Email: drvkumar2007@gmail.com.
Sameer Gupta, Email: sameerdr79@gmail.com.
Sanjeev Misra, Email: misralko@gmail.com.
Arun Chaturvedi, Email: drchatur@gmail.com.
Shashank Chaudhary, Email: shashankbmc@gmail.com.
Parijat Suryavanshi, Email: parijatsuryavanshi@gmail.com.
References
- 1.Chen C.L., Most S.P., Branham G.H., Spataro E.A. Postoperative complications of paramedian forehead flap reconstruction. JAMA Facial Plast Surg. 2019;21(4):298–304. doi: 10.1001/jamafacial.2018.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smart R.J., Yeoh M.S., Kim D.D. Paramedian forehead flap. Oral Maxillofac Surg Clin. 2014;26(3):401–410. doi: 10.1016/j.coms.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Genova R., Gardner P.A., Oliver L.N., Chaiyasate K. Outcome study after nasal alar/peri-alar subunit reconstruction: comparing paramedian forehead flap to nasolabial flap. Plast Reconstr Surg Glob Open. 2019;7(5) doi: 10.1097/GOX.0000000000002209. 2019 May 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conley J.J., Price J.C. The midline vertical forehead flap. Otolaryngol Head Neck Surg. 1981;89(1):38–44. doi: 10.1177/019459988108900108. [DOI] [PubMed] [Google Scholar]
- 5.Menick F.J. Aesthetic refinements in use of forehead for nasal reconstruction: the paramedian forehead flap. Clin Plast Surg. 1990;17(4):607–622. [PubMed] [Google Scholar]
- 6.MDe la Rhinoplastie Labat. Imprimerie de Ducessois; Paris, France: 1834. Art de Restaurer ou de Refaire Completement la Nez [Dissertation] [Google Scholar]
- 7.Baker S. Mosby; St. Louis, Missouri: 2007. Local Flaps in Facial Reconstruction. [Google Scholar]
- 8.Rudolph M.A., Walker N.J., Rebowe R.E., Marks M.W. Broadening applications and insights into the cross-paramedian forehead flap over a 19-year period. J Plast Reconstr Aesthetic Surg. 2019;72(5):763–770. doi: 10.1016/j.bjps.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Ni H.C., Wang J.C., Sun J.M., Guo N.Q. Expanded paramedian forehead flaps for nasal defects: beyond aesthetic subunits. Ann Plast Surg. 2018;81(6S Suppl 1):S54–S58. doi: 10.1097/SAP.0000000000001371. [DOI] [PubMed] [Google Scholar]
- 10.Chen C., Most S., Branham G., Spataro E. Postoperative complications of paramedian forehead flap reconstruction. JAMA Facial Plast Surg. 2019;21(4):298–304. doi: 10.1001/jamafacial.2018.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santos Stahl A., Gubisch W., Fischer H., Haack S., Meisner C., Stahl S. A cohort study of paramedian forehead flap in 2 stages (87 flaps) and 3 stages (100 flaps) Ann Plast Surg. 2015;75(6):615–619. doi: 10.1097/SAP.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 12.Blázquez-Sánchez N., Fernández-Canedo I., Repiso-Jiménez J.B., Rivas-Ruiz F., De Troya Martín M. Usefulness of the paramedian forehead flap in nasal reconstructive surgery: a retrospective series of 41 patients. Actas Dermosifiliogr. 2016;107(2):133–141. doi: 10.1016/j.ad.2015.09.004. [DOI] [PubMed] [Google Scholar]