Introduction
Obesity is a thriving health problem, and failure to achieve weigh loss through lifestyle changes is common. Consequently, weight-loss supplements have become increasingly popular, and raspberry ketones (RK) are one such example. Animal studies suggest that RK enable weigh loss through various mechanisms, including norepinephrine-induced lipolysis (1). However, there is limited literature evaluating its effect on humans (2, 3). Despite unproven efficacy, RK are easily acquired, and may pose a potential toxicity risk, especially as dosing regimens and long-term effects are uncertain (4).
Case Report
A 47-year-old woman presented with sudden onset of diarrhea, sweating and feeling unwell. She had taken two tablets of RK, for the first time, approximately two hours earlier. She was a smoker with a body mass index of 31 kg/m2 and no other coronary risk factors. Her physical examination revealed a heart rate of 137 beats/minute and blood pressure (BP) of 197/130, but no focal clinical signs. A 12-lead electrocardiogram (ECG) showed sinus rhythm. Blood tests revealed a normocytic anemia with a hemoglobin count of 93 g/L and urea of 13.9 mmol/L. Her BP gradually normalized without treatment. However, on the following day, her hemoglobin reduced to 69 g/L, with increased reticulocyte count of 133x109/L. She was transfused three units of blood. During transfusion, she felt sudden chest pain radiating to the left arm. ECG displayed ST elevation in the inferoposterolateral territory (Fig. 1). Within five minutes, the chest pain spontaneously improved with resolution of ST changes (Fig. 2); her troponin level minimally increased to 66 ng/L. She experienced five further episodes of transient chest pain with similar ECG changes in the next two days; all of which were treated with nitrates and resolved within 10 minutes. Computed tomography (CT) coronary angiography revealed unobstructed coronary arteries with a calcium score of zero (Fig. 3).
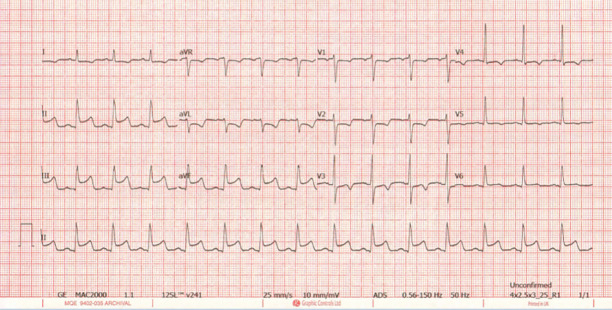
Figure 1.
An ECG showing ST elevation in leads II, III, aVF, and V6; ST depression in leads V1-4, I, and aVL; and T-wave inversion in V5 suggestive of an acute coronary occlusion involving the inferoposterolateral territory
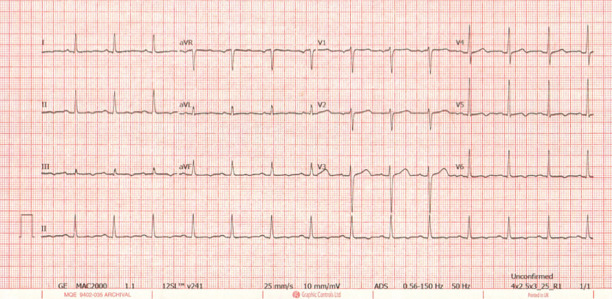
Figure 2.
An ECG taken within 10 minutes of the previous showing resolution of the ST changes. There is a remaining T-wave inversion in leads II, III, aVL, aVF, and V5-6
Figure 3.
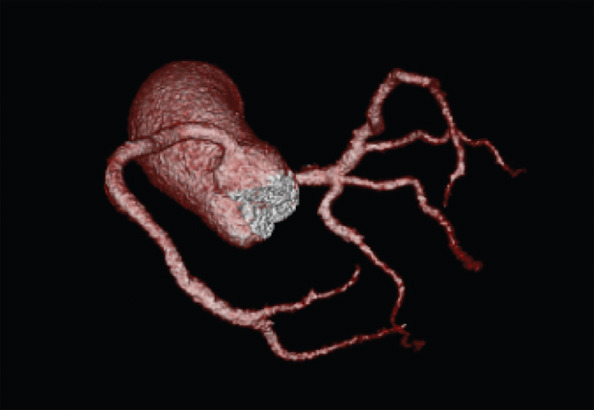
A CT coronary angiogram (spider view) demonstrating no significant plaque or stenosis in the coronary arteries and a calcium score of 0 (Agatston method)
Oesophago-gastro-duodenoscopy displayed gastritis and duodenal ulceration with Helicobacter pylori positivity but no recent bleeding. An incidental finding of bilateral subsegmental pulmonary emboli was noted on CT coronary angiogram. The patient gave an account of several recent long-haul flights, and this, in combination with obesity and smoking, were considered to be predisposing factors for pulmonary embolism. The patient was treated with anticoagulation; diltiazem and ferrous sulfate were also commenced.
Discussion
This patient’s pattern of symptoms and ECG changes were indicative of intermittent acute coronary occlusion. The normal CT coronary angiogram together with the transient, episodic, and nitrate-responsive nature of chest pain was highly suggestive of coronary vasospasm.
Multiple case reports have associated weight-loss supplements to adverse cardiac effects, such as synephrine (5, 6) and capsaicin-containing (7) supplements, both having sympathomimetic properties. An increased adrenergic tone is thought to be important in the pathogenesis of coronary vasospasm. The molecular structure of RK is similar to that of synephrine, an alpha-adrenergic agonist. One of the effects of RK is the augmentation of sympathetic activity (1). Our patient’s presenting symptoms of diarrhea, sweating, tachycardia, and hypertension are consistent with increased sympathetic activity and occurred soon after the ingestion of RK. Consequently, there is a possibility that excessive dosage or increased sensitivity to RK may have caused the presenting symptoms and episodes of coronary vasospasm.
Two case reports have investigated the association of blood transfusion with ST changes. One case was considered to be the result of an anaphylactic reaction (8), and the other was consistent with an acute coronary syndrome due to atherosclerosis (9). In our case, although the first episode occurred during blood transfusion, there was no allergic response and further episodes occurred after completing the transfusion, making a causal connection unlikely.
The patient had multiple active comorbidities, which may have predisposed to coronary vasospasm. However, the manifestations of initial symptoms soon after ingestion of RK, and the fact that the chest pain episodes stopped after two days, enhance the likelihood of RK as the main contributing factor. It is also important to acknowledge that numerous hospitalized patients have multiple acute medical conditions but associated coronary vasospasm is extremely rare. A diagnostic challenge with re-exposure to RK would have been of interest but was not performed for safety reasons. Instead, the patient was empirically treated with calcium antagonists and to date has not experienced any further recurrence of symptoms.
Conclusion
Based on our case, we propose that the ingestion of RK, with its known sympathomimetic effects and unclear therapeutic dosage and pharmacokinetics, may be associated with coronary vasospasm.
Acknowledgments:
We thank Dr. Oliver Wignall, Radiology Consultant, for providing the imaging that was used in this case report.
Footnotes
Informed consent: This patient gave consent for submission of this case report after being informed of the content.
References
- 1.Morimoto C, Satoh Y, Hara M, Inoue S, Tsujita T, Okuda H. Anti-obese action of raspberry ketone. Life Sci. 2005;77:194–204. doi: 10.1016/j.lfs.2004.12.029. [DOI] [PubMed] [Google Scholar]
- 2.Arent SM, Walker AJ, Pellegrino JK, Sanders DJ, McFadden BA, Ziegenfuss TN, et al. The Combined Effects of Exercise, Diet, and a Multi-Ingredient Dietary Supplement on Body Composition and Adipokine Changes in Overweight Adults. J Am Coll Nutr. 2018;37:111–20. doi: 10.1080/07315724.2017.1368039. [DOI] [PubMed] [Google Scholar]
- 3.Lopez HL, Ziegenfuss TN, Hofheins JE, Habowski SM, Arent SM, Weir JP, et al. Eight weeks of supplementation with a multi-ingredient weight loss product enhances body composition, reduces hip and waist girth, and increases energy levels in overweight men and women. J Int Soc Sports Nutr. 2013;10:22. doi: 10.1186/1550-2783-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bredsdorff L, Wedebye EB, Nikolov NG, Hallas-Moller T, Pilegaard K. Raspberry ketone in food supplements--High intake, few toxicity data--A cause for safety concern? Regul Toxicol Pharmacol. 2015;73:196–200. doi: 10.1016/j.yrtph.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Gange CA, Madias C, Felix-Getzik EM, Weintraub AR, Estes NA., 3rd Variant angina associated with bitter orange in a dietary supplement. Mayo Clin Proc. 2006;81:545–8. doi: 10.4065/81.4.545. [DOI] [PubMed] [Google Scholar]
- 6.Nykamp DL, Fackih MN, Compton AL. Possible association of acute lateral-wall myocardial infarction and bitter orange supplement. Ann Pharmacother. 2004;38:812–6. doi: 10.1345/aph.1D473. [DOI] [PubMed] [Google Scholar]
- 7.Sogut O, Kaya H, Gokdemir MT, Sezen Y. Acute myocardial infarction and coronary vasospasm associated with the ingestion of cayenne pepper pills in a 25-year-old male. Int J Emerg Med. 2012;5:5. doi: 10.1186/1865-1380-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osugi T, Ueki R, Shimode N, Tatara T, Tashiro C. Blood transfusion-induced anaphylaxis and coronary artery spasm during general anesthesia. J Anesth. 2008;22:457–9. doi: 10.1007/s00540-008-0658-7. [DOI] [PubMed] [Google Scholar]
- 9.Velibey Y, Erbay A, Ozkurt E, Usta E, Akin F. Acute myocardial infarction associated with blood transfusion:case report and literature review. Transfus Apher Sci. 2014;50:260–2. doi: 10.1016/j.transci.2014.01.009. [DOI] [PubMed] [Google Scholar]