Abstract
This scientific commentary refers to ‘Diabetes medications and risk of Parkinson’s disease: a cohort study of patients with diabetes’, by Brauer etal. (doi:10.1093/brain/awaa262).
This scientific commentary refers to ‘Diabetes medications and risk of Parkinson’s disease: a cohort study of patients with diabetes’, by Brauer etal. (doi:10.1093/brain/awaa262).
A variety of genetic, environmental and demographic risk factors contribute to a person’s risk of Parkinson’s disease. The development, validation and refinement of prodromal Parkinson’s disease research criteria grounded in evidence-based risk factors (Berg etal., 2015; Heinzel etal., 2019) has improved our ability to identify individuals at risk. Diabetes mellitus increases the risk of Parkinson’s disease and accelerates disease progression through various molecular mechanisms (Pagano etal., 2018), and is included in the updated prodromal Parkinson’s disease criteria. The link between diabetes and Parkinson’s disease extends to antidiabetic drugs. To date, small clinical trials repurposing antidiabetic drugs in Parkinson’s disease have yielded positive results with exenatide [a glucagon-like-peptide 1 receptor (GLP-1) agonist], but not with pioglitazone (a glitazone) (Aviles-Olmos etal., 2013; Simuni etal., 2015; Athauda etal., 2017). However, few studies have compared the biological effects of other antidiabetic drugs in Parkinson’s disease. In this issue of Brain, Brauer and co-workers investigate whether different antidiabetic drugs are associated with different risk levels for Parkinson’s disease in patients with type 2 diabetes (Brauer etal., 2020).
In their retrospective longitudinal population-based study, Brauer etal. examined whether Parkinson’s disease risk differs for individuals with type 2 diabetes treated with GLP-1 agonists, dipeptidyl peptidase 4 (DPP4) inhibitors, or glitazones (referred to as index medications) versus other antidiabetic agents (referred to as control medications). Exposure was classified on the basis of whether patients had ever or never used the index medications, regardless of therapy changes during the study period. Using ‘The Health Improvement Network’ database, an anonymized primary care data registry in the UK, Brauer etal. identified 329 patients who developed Parkinson’s disease over a ∼3-year period from among 100 288 patients with diabetes.
As this was not a prospective case-control study, the results may be confounded by differences between the groups in other Parkinson’s disease risk factors such as age, sex, smoking, coffee intake, and genetics, or by differences in rates of Parkinson’s disease misdiagnosis. To partially overcome this limitation, the authors used propensity scores to account for confounding demographic variables (age, sex, and non-smoking). In addition to the primary analysis comparing Parkinson’s disease risk across patients taking index and control medications, they also conducted secondary analyses to evaluate Parkinson’s disease incidence in association with diabetes, the overall effect of diabetes treatment compared to no treatment, and the impact of insulin taken in combination with index and control medications. To establish the robustness of the primary results, they evaluated the differences between current and past use of the index medications and the effect of continuous use of an index medication. They also conducted similar analyses using a stricter outcome definition (Parkinson’s disease diagnosis with at least two antiparkinsonian medications), and stricter classification approaches by restricting the sample to those over the age of 40 years, non-smokers, and obese patients.
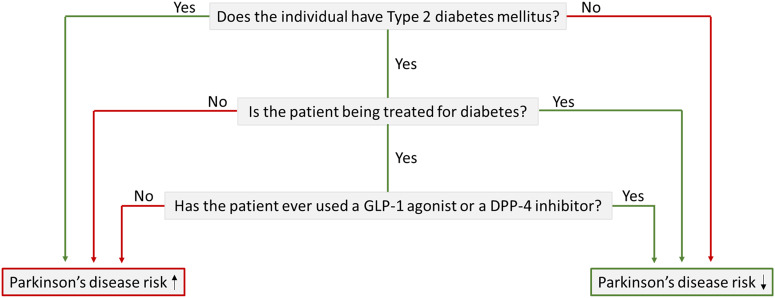
Brauer etal. found strong evidence for a lower incidence of Parkinson’s disease in users of DPP4 inhibitors and GLP-1 agonists compared to users of control medications, and an inverse association between use of these drugs and onset of Parkinson’s disease (Fig. 1). As expected, there were several demographic and clinical differences between the groups, although propensity score weighting suggested that the effect of these differences was minor. Parkinson’s disease incidence was lower in the GLP-1 agonist and DPP4 inhibitor groups than in the control group in analyses adjusting for several confounders (age, smoking, duration of diabetes before the index medication date). These results were seen in both short-term and long-term (>3 years) users of GLP-1 agonists and DPP4 inhibitors. Although glitazone usage was associated with a lower Parkinson’s disease risk, this finding was not significant in the adjusted models. Secondary analyses showed a lower Parkinson’s disease risk for current glitazone users, but not past users. Additional analyses showed that diabetes is associated with increased Parkinson’s disease risk; the risk was highest for untreated diabetic patients, and did not vary significantly between index and control medication groups for insulin user diabetics.
Figure 1.
Schematic showing key results from Brauer etal. (2020). Findings suggest that increased Parkinson’s disease risk owing to type 2 diabetes mellitus may be modified by use of specific antidiabetic drugs.
The most important finding of Brauer etal. is that even short periods of exposure to GLP-1 agonists and DPP4 inhibitors can lower the risk of Parkinson’s disease for patients with diabetes. Phase 2 clinical trials in Parkinson’s disease have shown beneficial effects of exenatide, a GLP-1 agonist. Of note, GLP-1 agonists can cross the blood–brain barrier and influence neuronal pathways associated with neuroinflammation and mitochondrial function (Mousa and Ayoub, 2019). Beneficial effects of DPP4 inhibitors have also been shown previously in an epidemiological study with a smaller sample size and shorter follow-up (Svenningsson etal., 2016), although the benefit from GLP-1 agonists did not reach significance. Even if oral DPP4 inhibitors cannot cross the blood–brain barrier, they may still have indirect effects on the brain (Mousa and Ayoub, 2019). Thus, there remains a need to investigate the effects of DPP4 inhibitors in patients with Parkinson’s disease, given the benefits found in studies involving animal models and other diseases. None of the analyses in the current study suggested a reliable protective effect of the third index medication, glitazone. These results are supported by the failure of a Parkinson’s disease clinical trial with pioglitazone (Simuni etal., 2015).
Before we jump to conclusions and claim disease-modifying effects for these antidiabetic drugs, we need appropriately designed clinical trials, which ideally will include individuals with prodromal Parkinson’s disease. Epidemiological studies provide the opportunity to assess large samples without the large budget and expansive data collection needed in case-control studies. However, their major problem is in dealing with confounding variables, which can be controlled for in well-matched case-control studies. Although Brauer etal. used statistical methods to account for some confounders, they did not control for other potentially confounding factors, including coffee consumption, environmental exposures (e.g. pesticides), and Parkinson’s disease markers (e.g. rapid eye movement sleep behaviour disorder, hyposmia, constipation, depression) outlined in the prodromal Parkinson’s disease criteria (Heinzel etal., 2019). The interaction between these confounders (e.g. smokers who are also coffee drinkers) may further impact the risk level for Parkinson’s disease, and statistical methods cannot easily control for these factors in epidemiological designs. The potential use of multiple index medications by patients included in the GLP-1 agonist, DPP4 inhibitor or glitazone user groups is another important confounder. Moreover, retrospective epidemiological and even case-control studies show associations that do not always translate to the clinic. This is illustrated by the failure of anti-inflammatory medications in Parkinson’s and Alzheimer’s disease clinical trials, despite the significant associations shown in epidemiological studies.
Since the main mechanism of action of both GLP-1 agonists and DPP4 inhibitors is to enhance insulin levels, it would be worthwhile analysing patients who were treated with insulin monotherapy. This is particularly relevant given that there was no further benefit of adding insulin to the indexagents, likely owing to the analysis being underpowered. Hyperglycaemia could explain the increased Parkinson’s disease incidence in untreated diabetic patients compared to treated patients, as it is known to have a particularly detrimental effect on dopaminergic neurons because of their vulnerability to mitochondrial dysfunction, oxidative stress and degeneration (Sergi etal., 2019). However, a simple reduction in hyperglycaemia cannot explain the study findings, because all of the antidiabetic agents are hypoglycaemic, although their efficacy may differ. In addition, different antidiabetic agents exert different effects on neurodegeneration through a variety of cellular and molecular mechanisms, which would need to be taken into account in clinical trials.
Both the current study and the prior literature support the inclusion of GLP-1 agonists in future updates of the Parkinson’s disease prodromal research criteria for estimating the likelihood ratio of Parkinson’s disease in diabetic patients. Although the Parkinson’s disease prodromal criteria are currently intended only for use in research, increasing the number of risk factors allows better prediction of Parkinson’s disease, as shown in studies of carriers of genetic mutations. By identifying Parkinson’s disease patients during the prodromal stage, we will eventually be able to intervene before the onset of motor symptoms, and before substantial numbers of dopamine neurons and axon terminals have degenerated, which should increase the effectiveness of disease-modifying agents.
Findings from epidemiological research such as the study by Brauer etal. emphasize the importance of investing in electronic healthcare registries and carefully documenting treatments in patients with chronic diseases. In view of the fact that the current study supports prior animal and human studies in suggesting the potential disease-modifying effect of GLP-1 agonists, physicians should consider preferential use of these agents when treating diabetic patients at high risk of Parkinson’s disease. A multicentre phase 3 trial using exenatide in patients with Parkinson’s disease is currently underway. If this study shows benefit, it will be important to conduct a randomized GLP-1 agonist versus placebo control study in patients with prodromal Parkinson’s disease—who will have less neurodegeneration than those already diagnosed. We expect that results from such studies will show better disease-modifying effects. However, caution is needed before interpreting the findings of Brauer etal. as definite. The potential disease-modifying effect of DPP4 inhibitors also needs to be confirmed by a case-control study, and, more importantly, by clinical therapeutic trials. Compared with the development of new agents, the repurposing of drugs for which we already have safety and tolerability data not only accelerates the clinical trial process, but also significantly decreases study cost and hastens approval for commercial use.
Competing interests
E.B. reports no competing interests. I.L.’s research is supported by the National Institutes of Health grants: 5P50AG005131-33, 2R01AG038791-06A, U01NS090259, U01NS100610, U01NS80818, R25NS098999, P20GM109025; U19 AG063911-1; Parkinson Study Group, Michael J Fox Foundation, Parkinson Foundation, Lewy Body Association, Roche, Abbvie, Biogen, EIP-Pharma and Biohaven Pharmaceuticals. She was a member of a Lundbeck Advisory Board. She receives her salary from the University of California San Diego and as Chief Editor of Frontiers in Neurology.
References
- Athauda D, Maclagan K, Skene SS, Bajwa-Joseph M, Letchford D, Chowdhury K, et al. Exenatide once weekly versus placebo in Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet 2017; 390: 1664–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aviles-Olmos I, Dickson J, Kefalopoulou Z, Djamshidian A, Ell P, Soderlund T, et al. Exenatide and the treatment of patients with Parkinson’s disease. J Clin Invest 2013; 123: 2730–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois B, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord 2015; 30: 1600–11. [DOI] [PubMed] [Google Scholar]
- Brauer R, Wei L, Ma TT, Athauda D, Girges C, Vijiaratnam, et al. Diabetes mediations and risk of Parkinson’s disease: a cohort study of diabetes patients. Brain 2020; 143: 3067–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinzel S, Berg D, Gasser T, Chen H, Yao C, Postuma RB.. Update of the MDS research criteria for prodromal Parkinson’s disease. Mov Disord 2019; 34: 1464–70. [DOI] [PubMed] [Google Scholar]
- Mousa SA, Ayoub BM.. Repositioning of dipeptidyl peptidase-4 inhibitors and glucagon like peptide-1 agonists as potential neuroprotective agents. Neural Regen Res 2019; 14: 745–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano G, Polychronis S, Wilson H, Giordano B, Ferrara N, Niccolini F, et al. Diabetes mellitus and Parkinson disease. Neurology 2018; 90: E1654–62. [DOI] [PubMed] [Google Scholar]
- Sergi D, Renaud J, Simola N, Martinoli M-G.. Diabetes, a contemporary risk for Parkinson’s disease: epidemiological and cellular evidences. Front Aging Neurosci 2019; 11: 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simuni T, Kieburtz K, Tilley B, Elm JJ, Ravina B, Babcock D, et al. Pioglitazone in early Parkinson’s disease: a phase 2, multicentre, double-blind, randomised trial. Lancet Neurol 2015; 14: 795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svenningsson P, Wirdefeldt K, Yin L, Fang F, Markaki I, Efendic S, et al. Reduced incidence of Parkinson’s disease after dipeptidyl peptidase-4 inhibitors-A nationwide case-control study. Mov Disord 2016; 31: 1422–3. [DOI] [PubMed] [Google Scholar]