Abstract
Background:
Asthenopia or eye strain is one of the major medical problems that students face during their academic years.
Objectives:
The aim of this study is to determine the prevalence of asthenopia among a sample of university students attending various majors and to identify the risk factors for its development.
Methods:
This is a cross sectional study conducted on students attending various faculties at the American University of Beirut during the spring semester of 2019. Students were asked to fill a self-administered anonymous questionnaire that inquired about demographics, use of digital devices, symptoms of asthenopia, possible risk factors and protective measures. A bivariate analysis was performed to correlate asthenopia with the different variables. A multivariate analysis was then conducted to determine the extent of contribution of the different variables to asthenopia after controlling for confounding variables.
Results:
The prevalence of asthenopia was found to be 67.8% with blurred vision being the most reported symptom (27.0%). A bivariate analysis was used to assess the association between asthenopia and the following variables: demographics, digital device use, reasons for using digital devices, and preventive methods. Age, being a continuous variable, was analyzed using an independent t- test. For the variables that were found to be have a p-value < 0.2, a multiple logistic regression was performed. Old age was found to be a protective factor for asthenopia, with 0.693 times reduction in asthenopia for every increase in year of age. Using the device for communication for less than four hours (p=0.012), using the device for less than four hours per day (p=0.000) and pattern of using the device for less than three years (p=0.023) were significant in being negatively associated with asthenopia. As for preventative measures that protect users from digital eyestrain, we found that using eye drops (p=0.004; OR=0.375) and taking regular breaks (p=0.000; OR= 0.399) were protective factors whereas using adjustable screens was a risk factor (p=0.000; OR=3.083).
Conclusion:
Asthenopia was found to be of non-negligible prevalence among this sample of university students. The results of this study highlight the importance of establishing awareness campaigns and encourage the introduction of targeted screenings for asthenopia among college students.
Keywords: asthenopia, digital device, Lebanon, prevalence, risk factors, university students
Introduction and Background
With the emergence of digital technology, digital devices such as desktops, laptops, tablets, and phones have become widely used by students for academic, leisure, and social purposes. Hence, students tend to suffer from asthenopia that is visual discomfort accompanied by other symptoms such as dizziness, headache, red or itchy eyes, and the inability to concentrate.[1]
The “Computer Vision Syndrome” is another term that has been defined by the American Optometric Association (AOA) as a combination of vision difficulties, ensuing from stress on the eyes due to digital screen usage. Overall effects depend upon the length of usage, the posture adapted during usage, and the kind of device used. The usage of digital devices might be correlated to the increasing prevalence of asthenopia.[2] The consequences of asthenopia can also interfere significantly with attention and academic performance and can limit work capacity making it a real public health concern.[3,4]
In Lebanon, as in other countries, much time is spent by students on digital devices. The aim of this study is to investigate the relationship between the use of digital devices and the prevalence of asthenopia among students studying at the American University of Beirut (AUB) and to assess its risk factors. To our knowledge, there are no published reports on this issue. The results of this study will provide a substantial ground for the establishment of future awareness campaigns and will help evaluate the need for targeted screening for asthenopia among college students in primary care centers.
Methodology
Study design
The study was conducted at the American University of Beirut (AUB), which is a private university that accommodates about 9000 students. This was a cross-sectional study that was conducted during the spring semester of 2019 using a self-administered anonymous questionnaire among university students from all faculties who are attending classes at the university.
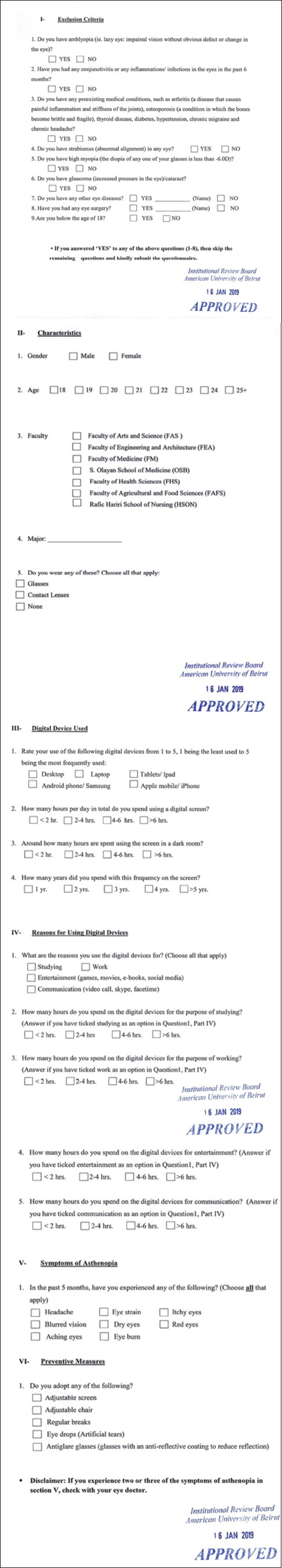
The questionnaire attached under “supplementary material” below inquired about: (1) demographics; (2) current major and faculty; (3) usage of digital device, type of device and time spent using it; (4) reason for using the digital device; (5) use of glasses or contact lenses; (6) symptoms of asthenopia and (7) preventive measures.
The study started after receiving the Institutional Review Board (IRB) acceptance from the university.
Sampling strategy
The study population included students enrolled at AUB from different faculties and years of study. The sample included only students attending classes on the campus.
Inclusion criteria included students who were ≥ 18 years of age, while exclusion criteria applied to all students who suffered from any of the following: amblyopia, conjunctivitis, eye inflammation/ infection, pre-existing medical conditions (arthritis, osteoporosis, thyroid disease, diabetes, hypertension, chronic migraine, and chronic headache), strabismus, high myopia (more than -6.0 diopters), glaucoma or cataract, retinal nerve damage, any eye disease, or history of eye surgery. Since the study aims to study headaches as a pure consequence of asthenopia, chronic migraines and chronic headaches were listed as exclusion criteria for participants.
A total of 622 students completed our questionnaire out of which, 165 participants (27%) met the exclusion criteria. The remaining 457 questionnaires were included in the analysis [Figure 1]. Since the students in our target population attended seven different faculties at AUB, stratified sampling was applied: the overall population in our sample was divided into seven different subgroups, for the following seven faculties: Arts and Sciences, Business, Medicine, Engineering and Architecture, Agriculture and Food sciences, Health sciences and Nursing. Subjects from the same faculty were targeted in large classes taken by students from different majors within that same faculty and surveys were filled voluntarily. These classes were picked accordingly to ensure a well-balanced and diversified sample of students in one faculty while avoiding potential bias from limiting the study to students from one specific major within that faculty.
Figure 1.
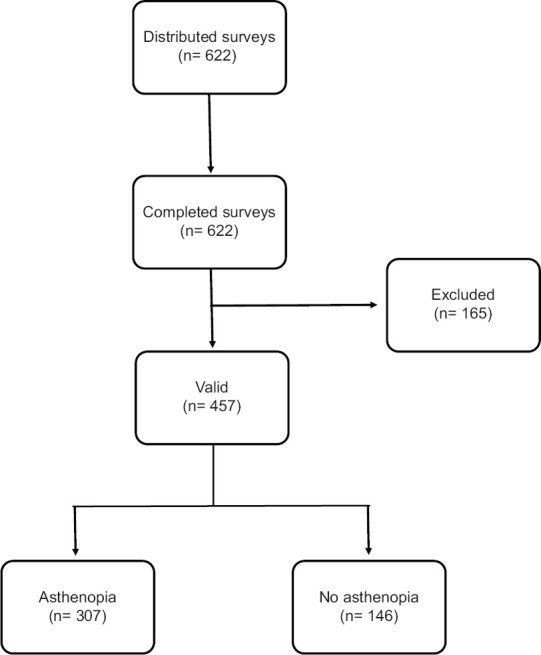
Flowchart of the student recruitment process
Data collection
Courses attended by students of different ages and faculties were looked up on the university website. Team members presented the questionnaire to students before, during, or after the specified classes on different days of the week and during different times of the day.
After securing the professor's permission, consent was read to the potential participants. Self-administered anonymous questionnaires in the English language were distributed to students. The aim of the project was explained to them and any queries were addressed and clarified.
Data analysis
The gathered data was analyzed using the Statistical Package for Social Sciences (version 19.0, SPSS IBM, Inc) software. Descriptive statistics included frequencies and percentages. Our primary outcome asthenopia is binary and its prevalence was calculated. Asthenopia was defined as one out of any of the following seven symptoms: blurred vision, dry eyes, red eyes, aching eyes, itchy eyes, eye strain, and eye burn. The following factors were regrouped: hours spent per day, hours spent in the dark, time spent studying, time spent working, time spent for entertainment, time spent for communication into two groups instead of four: less than four hours, and equal to or greater than four hours. This was done for sake of analysis since some of the categories had too small a number. A bivariate analysis was used to assess the association between asthenopia and the following variables: demographics, digital device use, reasons for using digital devices, and preventive methods. Age, being a continuous variable, was analyzed using an independent t- test. For the variables that were found to have a P-value < 0.2, a multiple logistic regression was then performed to analyze the ones that contribute the most to asthenopia and control for the effect of cofounding variables. For all our analyses, we used a P-value of 0.05 and 95% confidence interval (CI) to assess statistical significance. Since some faculties are larger than others, our samples were weighed according to each faculty size such that, the number of participants for each faculty in our sample is proportionate to the number of students for each faculty within the general population of students attending AUB.
Results
The 457 questionnaires were divided into sections looking into the participants' demographics [Table 1] and possible risk factors and protective factors for asthenopia [Table 2].
Table 1.
Descriptive characteristics of participating students
| Characteristics | Frequency (%) |
|---|---|
| Gender | |
| Male | 251(55.4%) |
| Female | 202 (44.6%) |
| Age | |
| 18 | 72 (15.9%) |
| 19 | 158 (34.9%) |
| 20 | 95 (20.9%) |
| 21 | 65 (14.3%) |
| 22 | 41(9.0%) |
| 23 | 14 (3.1%) |
| 24 | 2 (0.4%) |
| 25+ | 7 (1.5%) |
| Faculty | |
| Faculty of Arts and Science (FAS) | 183 (40.3%) |
| Faculty of Engineering and Architecture (FEA) | 137 (30.2%) |
| Faculty of Medicine (FM) | 27 (5.9%) |
| S. Olayan School of Business (OSB) | 58 (12.8%) |
| Faculty of Health Sciences (FHS) | 20 (4.4%) |
| Faculty of Agricultural and Food Sciences (FAFS) | 20 (4.4%) |
| Rafic Hariri School of Nursing (HSON) | 9 (2.0%) |
| Eyewear | |
| Wears only contacts | 13 (2.8%) |
| Wears only glasses | 144 (31.7%) |
| Wears both contacts and glasses | 87 (19.2%) |
| Does not wear either | 210 (46.3%) |
Table 2.
Frequency distribution of possible risk factors and protective factors
| Frequency (%) | |
|---|---|
| Most frequently used device (mostly rated as 4 or 5) | |
| Laptop | 290 (63.9%) |
| Hours spent per day | |
| Less than 2 hours | 8 (1.7%) |
| 2 - 4 hours | 59 (13%) |
| 4 - 6 hours | 182 (40.2%) |
| More than 6 hours | 205 (45.1%) |
| <4 hours | 67 (14.7%) |
| ≥4 hours | 387 (85.3%) |
| Hours spent in the dark | |
| Less than 2 hours | 302 (66.6%) |
| 2 - 4 hours | 96 (21.2%) |
| 4 - 6 hours | 39 (8.6%) |
| More than 6 hours | 17 (3.6%) |
| <4 hours | 398 (87.8%) |
| ≥4 hours | 56 (12.2%) |
| Years spent | |
| <3 years | 77 (16.9%) |
| ≥3 years | 377 (83.1%) |
| Reason for use | |
| Studying | |
| Yes | 449 (99%) |
| No | 5 (1%) |
| Work | |
| Yes | 190 (42%) |
| No | 263 (58%) |
| Entertainment | |
| Yes | 437 (96.3%) |
| No | 17 (3.7%) |
| Communication | |
| Yes | 388 (85.6%) |
| No | 65 (14.4%) |
| Time spent studying | |
| 0 hours (device not used) | 5 (1.1%) |
| Less than 2 hours | 75 (16.6%) |
| 2 - 4 hours | 154 (34.0%) |
| 4 -6 hours | 155 (34.2%) |
| More than 6 hours | 64 (14.1%) |
| 0 hours | 5 (1.1%) |
| <4 hours | 229 (50.6%) |
| ≥ 4 hours | 219 (48.3%) |
| Time spent working | |
| 0 hours (device not used) | 263 (58.1%) |
| Less than 2 hours | 100 (22.1%) |
| 2 - 4 hours | 60 (13.2%) |
| 4 -6 hours | 15 (3.3%) |
| More than 6 hours | 15 (3.3%) |
| 0 hours | 263 (58.1%) |
| < 4 hours | 160 (35.3%) |
| ≥ 4 hours | 30 (6.6%) |
| Time spent for entertainment | |
| 0 hours (device not used) | 17 (3.8%) |
| Less than 2 hours | 75 (16.6%) |
| 2 - 4 hours | 197 (43.4%) |
| 4 -6 hours | 86 (19%) |
| More than 6 hours | 78 (17.2%) |
| 0 hours | 17 (3.8%) |
| < 4 hours | 272 (60%) |
| ≥ 4 hours | 164 (36.2%) |
| Time spent for communication | |
| 0 hours (device not used) | 65 (14.4%) |
| Less than 2 hours | 119 (26.3%) |
| 2 - 4 hours | 160 (35.3%) |
| 4 -6 hours | 65 (14.3%) |
| More than 6 hours | 44 (9.7%) |
| 0 hours | 65 (14.4%) |
| <4 hours | 279(61.6%) |
| ≥ 4 hours | 109 (24%) |
| Symptoms of asthenopia | |
| Headache | 320 (70.6%) |
| Blurred vision | 122 (27.0%) |
| Dry eyes | 106 (23.3%) |
| Red eyes | 102 (22.5%) |
| Aching eyes | 86 (19.0%) |
| Itchy eyes | 79 (17.4%) |
| Eye strain | 70 (15.5%) |
| Eye burn | 68 (15.0%) |
| Asthenopia prevalence | |
| Yes | 307 (67.8%) |
| No | 146 (32.2%) |
| Preventive measures adopted | |
| Adjustable screen | 74 (16.3%) |
| Adjustable chair | 56 (12.4%) |
| Regular breaks | 164 (36.1%) |
| Eye drops (artificial tears) | 84 (18.5%) |
| Antiglare glasses | 81 (17.9%) |
| At least one protective measure | 273 (60.1%) |
1) Definition and Prevalence of Asthenopia
Students were considered to have asthenopia if they declared having experienced in the past 5 months at least one of the following: Eye strain/ itchy eyes/ blurred vision/ dry eyes/ red eyes/ aching eyes/ eye burn; OR headache plus at least one of the previous symptoms. Hence, a person having experienced the symptom of headache alone was not considered to suffer from asthenopia. A similar definition of asthenopia (where headache alone was not considered a defining symptom of asthenopia) was adopted in a study aiming at determining asthenopia prevalence among a population of high school students in Iran.[5]
Based on our adopted definition, 67.8% of the students were found to have asthenopia and the most commonly reported symptom was blurred vision as documented in Table 2.
2) Demographics and their relation to Asthenopia
Out of the valid questionnaires, 55.4% of the participants were males and 44.6% were females. Their mean age was 19.8 years and most students (55.8%) were 19 or 20 years old [Table 1]. The majority of the students (40.3%) were enrolled in the Faculty of Arts and Science. As for eyewear, 2.8% of the students wore only contacts, 31.7% wore only glasses, 19.2% wore both and 46.3% wore none [Table 1].
Our results revealed no significant association between any of gender, faculty, or eyewear with the development of asthenopia. However, we found that older age was protective with an odds ratio of 0.693 [Table 3].
Table 3.
Bivariate and Multivariate analysis of the variables contributing to Asthenopia
| Variable | Level | Unadjusted OR | Adjusted OR | P | 95% Confidence interval | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Gender | Female | 1 | - | - | - | |
| Male | 0.703 | 1.007 | 0.975 | 1.076 | 2.689 | |
| Age | 0.837 | 0.693 | 0.000* | 0.591 | 0.814 | |
| Arts and Sciences | 1.925 | - | 0.349 | 0.488 | 7.585 | |
| Engineering and Architecture | 1.266 | - | 0.737 | 0.319 | 5.018 | |
| Medicine | 1.642 | - | 0.534 | 0.344 | 7.833 | |
| Faculty | School of Business | 1.423 | - | 0.631 | 0.337 | 6.001 |
| Health Sciences | 2.156 | - | 0.369 | 0.403 | 11.527 | |
| Agricultural and Food Sciences | 1.279 | - | 0.764 | 0.256 | 6.388 | |
| School of Nursing | 1 | - | - | - | ||
| Laptop Rating | 1 | 1.128 | 1.406 | 0.808 | 0.090 | 21.878 |
| 2 | 0.491 | 0.641 | 0.427 | 0.215 | 1.916 | |
| 3 | 0.553 | 0.592 | 0349 | 0.197 | 1.774 | |
| 4 | 0.550 | 0.574 | 0.215 | 0.239 | 1.380 | |
| 5 | 1 | - | - | - | ||
| Reason: Studying | No | 1 | - | - | - | |
| Yes | 1.813 | - | 0.529 | 0.284 | 11.574 | |
| Reason: Work | No | 1 | - | - | - | |
| Yes | 0.702 | - | 0.081 | 0.472 | 1.045 | |
| Reason: Entertainment | No | 1 | - | - | - | |
| Yes | 1.071 | - | 0.895 | 0.386 | 2.969 | |
| Reason: Communication | No | 1 | - | - | - | |
| Yes | 3.057 | - | 0.158 | 0.356 | 1.182 | |
| Frequency: Studying | 0 hours | 1 | - | - | - | |
| < 4 hours | 1.353 | - | 0.750 | 0.210 | 8.710 | |
| ≥ 4 hours | 2.554 | - | 0.325 | 0.394 | 16.541 | |
| Frequency: Work | 0 hours | 1 | - | - | - | |
| < 4 hours | 0.647 | - | 0.039* | 0.427 | 0.979 | |
| ≥ 4 hours | 1.111 | - | 0.809 | 0.474 | 2.605 | |
| Frequency: Entertainment | 0 hours | 1 | - | - | - | |
| < 4 hours | 1.137 | - | 0.801 | 0.418 | 3.092 | |
| ≥ 4 hours | 1.782 | - | 0.271 | 0.636 | 4.991 | |
| Frequency: Communication | 0 hours | 1 | - | - | - | |
| < 4 hours | 0.579 | 0.426 | 0.012* | 0.219 | 0.830 | |
| ≥ 4 hours | 0.887 | 0.701 | 0.365 | 0.326 | 1.510 | |
| Hours of Use per Day | < 4 hours | 0.428 | 0.339 | 0.000* | 0.190 | 0.6079 |
| ≥ 4 hours | 1 | - | - | - | ||
| Hours of Use in the Dark | < 4 hours | 1.007 | - | 0.982 | 0.545 | 1.862 |
| ≥ 4 hours | 1 | - | - | - | ||
| Device use per year | < 3years | 0.733 | 0.588 | 0.023* | 0.372 | 0.929 |
| ≥3 years | 1 | - | - | - | ||
| Eyewear | Wears neither contacts nor glasses | 1 | - | - | - | |
| Wears glasses | 1.303 | 0.973 | 0.942 | 0.466 | 2.031 | |
| Wears contacts | 1.552 | 0.910 | 0.809 | 0.424 | 1.954 | |
| Wears both glasses and contacts | 1.519 | 1.184 | 0.826 | 0.262 | 5.349 | |
| Adjustable Screen | Do not use | 2.300 | 3.083 | 0.000* | 1.702 | 5.585 |
| Use | 1 | - | - | - | ||
| Adjustable chair | Do not use | 1.405 | - | 0.248 | 0.789 | 2.502 |
| Use | 1 | - | - | - | ||
| Regular breaks | Do not use | 0.644 | 0.399 | 0.000* | 0.238 | 0.667 |
| Use | 1 | - | - | - | ||
| Eye drops | Do not use | 0.330 | 0.375 | 0.004* | 0.192 | 0.732 |
| Use | 1 | - | - | - | ||
| Antiglare glasses | Do not use | 0.663 | 0.594 | 0.145 | 0.295 | 1.196 |
| Use | 1 | - | - | - | ||
*p-value < 0.05
3) Devices and their relation to Asthenopia
Of all devices, laptops were most frequently used according to 63.9% of our sample who rated their use as four or five out of five. As for the pattern of use, 85.3% of the students spend more than four hours on their devices per day and 12.2% spend more than four hours using the screen in a dark room. To note that 83.1 % of the students have used their devices for three years or more [Table 2].
Concerning the reason for use, most of the students (99%) reported using their devices for studying. Similar high prevalence was also found for entertainment (96.3%), communication (85.6%), but not for working (42%). Approximately half of those using their devices for studying spend more than four hours per day doing that, while most of the students using their devices for entertainment (60%) or communication (61.6%) or work (58.1%) spend less than four hours per day [Table 2].
Regarding digital device use, our results revealed that using the laptop was not significantly associated with asthenopia. Similarly, none of the four reasons for device use was significantly associated with asthenopia [Table 3].
We found a significant association between time spent on a digital device and asthenopia only when the device is used for working for less than four hours with a P-value of 0.039 and when the device is used for communication for less than four hours with a P-value of 0.012 [Table 3].
Moreover, a significant association was found between asthenopia and spending less than four hours per day on the device (P-value = 0.000), but not when the device was used in the dark. Similarly, students who have been using their devices for less than three years were significantly less likely to develop asthenopia (P-value= 0.023; adjusted OR = 0.588) compared to those who have been using their devices for three years or more [Table 3].
4) Preventive measures and their relation to asthenopia
Many preventive measures have been described as a way to decrease the risk of developing asthenopia among the users of digital devices. The results of our study revealed that 60.1% of the students adopt at least one of the following preventive measures: adjustable screens, adjustable chairs, regular breaks, eye drops or antiglare glasses; regular breaks being the most commonly adopted measure [Table 2].
Of these measures, using eye drops, adjustable screens and taking regular breaks were significantly associated with asthenopia in the multivariate analysis (P-values of 0.004, 0.000 and 0.000 respectively). Students using adjustable screens were three times more likely to develop asthenopia. However, those not using eye drops or not taking regular breaks were nearly three times less likely to develop asthenopia [Table 3].
Discussion
To our knowledge, this study is the first of its kind to determine the prevalence of asthenopia and assess its risk factors among university students in Lebanon. Our results revealed that the prevalence of asthenopia in our sample reached 67.8%. Hence, university students in Lebanon are not spared the adverse consequences of excessive digital device use.
In the study in Iran which adopted the same definition of asthenopia as ours, the prevalence of asthenopia was 49.4 %.[5] High prevalence of asthenopia was also found among many college students in various countries: China 53.5%,[6] Malaysia 89.9%,[7] Egypt 86%,[8] and very recently in Iran 70.9%.[9]
Concerning the symptoms, headache was the most prevalent in our population. This pattern was seen in many studies including recently among university students of different colleges in Saudi Arabia with a headache prevalence of 68%.[10] Unfortunately, no studies assessing the prevalence of headache among the Lebanese population were found in the literature making it an interesting point to explore in the future.
Due to the high prevalence of headache in our population, and despite having stringent exclusion criteria concerning migraines, headaches were not considered a defining symptom of asthenopia if present alone, similar to the study conducted in Iran.5 Out of the symptoms included in the definition of asthenopia, blurred vision turned out to have the highest prevalence (27.0%) [Table 2].
In this study, there was no significant difference between the prevalence of asthenopia among men and women. Some studies have shown that males and females are not equally at risk of developing symptoms of asthenopia. For instance, in Ajman (United Arab Emirates) and Jeddah (Saudi Arabia), females were more likely to develop asthenopia.[2,10]
There was a significant association between age and asthenopia (P = 0.000). In our sample, older age was a protective factor. This might be interpreted in the light of digital screen introduction into day to day life in Lebanon whereby older students who are more used to traditional ways of studying using books and pens are less likely to rely on modern digital devices compared to younger students who had an earlier introduction to these devices. Moreover, our findings could also be attributed to the lack of comparison with a control group of people of ages from 18 to 25, who do not use digital devices. The literature carries contradictory evidence when it comes to age hence, this complex connection between age and asthenopia has yet to be defined.[5] The relationship may become clearer in the coming years upon further research with bigger sample sizes, larger age ranges, and specific exposures to certain digital devices.
No significant correlation was found between asthenopia and the different faculties attended. Literature is scarce regarding enrolment in a particular faculty and the development of asthenopia. In Chennai, for example, engineering students were at a higher risk of developing asthenopia compared to medical students.[11]
Furthermore, no significant association was found between eyewear and asthenopia. Contrary to our results, contact lens users in India were found to be at a significant higher risk of experiencing headache, blurred vision and dry eyes in context of computer vision syndrome.[11] In Sri Lanka, wearing contact lenses was also significantly associated with CVS.[12] It might be that students who wear contact lenses avoid wearing their lenses when using digital devices. Knowing that contact lens wearers might suffer from dry eyes, it is possible that they are more aware of the preventative measures that alleviate their asthenopia symptoms.
As for the purpose of using the device, our results showed that it was not significantly correlated with asthenopia despite what has been reported online regarding oculomotor responses and task dependency. In one study, task type was shown to affect changes in pupil diameter, with more demanding tasks, such as faster on-screen presentation of figures and tracking (rather than reading or monitoring), causing greater increases in pupil diameter.[13] Different tasks may entail varying degrees of attention, which may exacerbate symptoms of eye strain and dryness in some instances more than others. A reason for this discrepancy could be the small sample size used in this study. As for the duration of the time spent using the device for communication, the relation was significant, but those using their device for less than four hours were less likely to have asthenopia than those who did not use their device for communication at all. The daily exposure time was significantly correlated with asthenopia. People who used the device for less than four hours were 2.3 times less likely to develop asthenopia than those who used it for longer (P= 0.000; Table 3). This finding is in line with the Shanghai study, which found that students using digital devices for three hours or more were at significantly higher risk of developing asthenopia compared to those who used the devices for less than three hours.[8] One could speculate that spending more time on the device may induce a greater degree of eye fatigue as the ocular muscles are forced to work for longer periods. Along the same token, the number of years spent using the device was significantly correlated to asthenopia as well. Those who have been using their device for less than three years were 1.7 times less likely to develop asthenopia than those who used electronics for longer (P=0.023; Table 3). Hence, more years of using a device translates into more accumulated stress on the eye, which in turn increases the risk of having asthenopia. Among a nationally representative sample of Sri Lankan computer workers, the duration of occupation was significantly higher in workers with CVS (5.1 ± 5.7 years) than that in patients without CVS (3.6 ± 4.8 years). Also, those with severe CVS had a longer duration of occupation compared to those with mild to moderate CVS.[14]
No significant correlation was found between asthenopia and digital device use in the dark despite contrary evidence. Despite the detrimental effect of blue light emitted from digital displays recently described by the optical chemistry research at the University of Toledo, the wavelength, intensity and duration of blue light exposure are all important factors yet to be considered when assessing the effect of this blue light.[15,16] Another consideration would be that the cohort using the device for less than four hours may include people who do not use their phone in the dark, therefore a more detailed assessment of the time spent on digital devices would be a consideration for future research.
In our sample, 60.1% of the students adopt at least one of the five preventive measures included in our survey [Table 2], of which only three were significantly associated with asthenopia: eye drops, breaks, and adjustable screens. Those using eye drops were 0.375 times more likely to have asthenopia than those who did not (p= 0.004; Table 3). A reduced blink rate and incomplete blinks are associated with increased symptoms of eye strain and dryness.[17] This reduction in blinking frequency is thought to decrease the thickness of the lipid layer covering the ocular surface, leading to increased evaporation of the aqueous layer of the tear film beneath it.[18] These symptoms of visual discomfort following a certain visual task were reduced by pre-application of a lubricating ocular solution prior to the task.[19] Our results also revealed a significant negative correlation between regular breaks and asthenopia (p = 0.000; Table 3). Hence, taking regular breaks is preventive for eye discomfort from digital device use, a finding which fits with the existing guidelines by the American Optometric Association that advocates the 20-20-20 rule.[20]
Finally, our results show that using adjustable screens is a risk factor for asthenopia (P = 0.000). This is contrary to reports showing the role of adequate adjustment of the workstation and viewing distances in decreasing asthenopia. One study showed that asthenopia was less in subjects whose viewing distance was more than 30 cm and highest when it was less than 30 cm.[21] Similarly, the viewing angle was another factor potentially contributing to asthenopia: a higher gaze angle results in reduced amplitude of accommodation thus placing greater strain on the eyes' focusing mechanism.[22] Given that only 16.3% of the students in our study use an adjustable monitor, this practice is not commonplace and it is possible that students who suffered most of eye strain were the ones who invested in adjustable screens in an attempt to minimize their eye symptoms. Also, given the fact that this study was cross-sectional, temporality could not be established meaning it is very likely these individuals had asthenopia before investing in a protective screen.
The use of preventative measures among the study group was not common. Regular breaks were more commonly used by 36.1% of our population [Table 2]. Despite the high prevalence of asthenopia in our population, these numbers show the lack of awareness about simple methods that are likely to mitigate their eye symptoms, hence the need to spread education about asthenopia and its relieving factors.
Strengths and Limitations
To our knowledge, this is the first study to determine the prevalence of asthenopia among university students in Lebanon. The response rate was high and this could be attributed to the curiosity of the students to know about this daily problem. Of the limitations, is the fact that the study was conducted in a private academic center where students are more likely to have access to the digital devices thus limiting the generalizability of the study. The responses were based on estimation of the hours used by the students and this could result in underestimation. As this is a cross-sectional study, temporality could not be established.
Future Recommendations
This study considered a number of risk factors associated with asthenopia; however, there are many more factors to be studied. Future research should target search for more risk factors to associate with asthenopia and should look at the prevalence of asthenopia nationwide in different socioeconomic groups and age groups. It would be imperative to include an objective tool which can help better decide on the need to screen for asthenopia.
Conclusion
Asthenopia is prevalent in this sample of students which reaches 67.8% and it is associated with younger age. Using the device for communication for less than four hours, using the device for less than four hours per day, and pattern of using the device for less than three years were significantly associated with asthenopia. Concerning preventative measures, using eye drops and taking regular breaks were protective factors against asthenopia, whereas using adjustable screens was a risk factor. This high prevalence of asthenopia highlights the importance of establishing awareness campaigns and encourages the introduction of targeted screenings for asthenopia among college students.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Supplementary material:
References
- 1.Neugebauer A, Fricke J, Russmann W. Asthenopia: Frequency and objective findings. Ger J Ophthalmol. 1992;1:122–4. [PubMed] [Google Scholar]
- 2.Shantakumari N, Eldeeb R, Sreedharan J, Gopal K. Computer use and vision-related problems among university students in Ajman, United Arab Emirate. Ann Med Health Sci Res. 2014;4:258–63. doi: 10.4103/2141-9248.129058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gowrisankaran S, Nahar NK, Hayes JR, Sheedy JE. Asthenopia and blink rate under visual and cognitive loads. Optom Vis Sci. 2012;89:97–104. doi: 10.1097/OPX.0b013e318236dd88. [DOI] [PubMed] [Google Scholar]
- 4.Benedetto S, Drai-Zerbib V, Pedrotti M, Tissier G, Baccino T. E-readers and visual fatigue. PLoS One. 2013 doi: 10.1371/journal.pone.0083676. doi: 101371/journalpone0083676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashemi H, Khabazkhoob M, Forouzesh S, Nabovati P, Yekta A, Ostadi moghaddam H. The Prevalence of Asthenopia and its Determinants Among Schoolchildren. J Comprehensive Pediatrics. 2017 doi: 105812/compreped43208. [Google Scholar]
- 6.Xu Y, Deng G, Wang W, Xiong S, Xu X. Correlation between handheld digital device use and asthenopia in Chinese college students: A Shanghai study. Acta Opthalmol. 2018 doi: 10.1111/aos.13885. doi: 101111/aos13885. [DOI] [PubMed] [Google Scholar]
- 7.Reddy SC, Low CK, Lim YP, Low LL, Mardina F, Nursaleha MP. Computer vision syndrome: A study of knowledge and practices in university students. NepJOL. 2013;5:161–8. doi: 10.3126/nepjoph.v5i2.8707. [DOI] [PubMed] [Google Scholar]
- 8.Iqbal M, El-Massry A, Elagouz M, Elzembely H. Computer vision syndrome survey among the medical students in Sohag University Hospital, Egypt. Ophthalmic Res. 2018;8:1–8. [Google Scholar]
- 9.Hashemi H, Saatchi M, Yekta A, et al. High Prevalence of Asthenopia among a Population of University Students? J Ophthalmic Vis Res. 2019;14:474–82. doi: 10.18502/jovr.v14i4.5455. doi:10.18502/jovr.v14i4.5455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altalhi A, Khayyat W, Khojah O, Alsalmi M, Almarzouki H. Computer Vision Syndrome Among Health Sciences Students in Saudi Arabia: Prevalence and Risk Factors? Cureus. 2020;12:e7060. doi: 10.7759/cureus.7060. doi:10.7759/cureus.7060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logaraj M, Madhypriya V, Hegde S. Computer vision syndrome and associated factors among medical and engineering students in Chennai. Ann Med Health Sci Res. 2014;4:179–85. doi: 10.4103/2141-9248.129028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ranasinghe P, Wathurapatha WS, Perera YS, Lamabadusuriya DA, Kulatunga S, Jayawardana N, et al. Computer vision syndrome among office workers in a developing country: An evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:2–9. doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishiyama K. Ergonomic aspects of the health and safety of VDT work in Japan: A review. Ergonomics. 1990;33:659–85. doi: 10.1080/00140139008927178. [DOI] [PubMed] [Google Scholar]
- 14.Ranasinghe P, Wathurapatha WS, Perera YS, Lamabadusuriya DA, Kulatunga S, Jayawardana N, Katulanda P. Computer vision syndrome among computer office workers in a developing country: An evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:150. doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Billau C. UT chemists discover how blue light speeds blindnessUTOLEDO, 2018 [Google Scholar]
- 16.Knels L, Valtink M, Roehlecke C, Lupp A, de la Vaga J, Mehner M, et al. Blue light stress in retinal neuronal (R28) cells is dependent on wavelength range and irradiance. EurJNeurosci. 2011;34:548–58. doi: 10.1111/j.1460-9568.2011.07790.x. [DOI] [PubMed] [Google Scholar]
- 17.Portello J, Rosenfield M, Chu C. Blink rate, incomplete blinks and computer vision syndrome. Optom Vis Sci. 2013;90:482–7. doi: 10.1097/OPX.0b013e31828f09a7. [DOI] [PubMed] [Google Scholar]
- 18.Pucker AD, Ng SM, Nichols JJ. Over the counter artificial tear drops for dry eye syndrome. Cochrane Database Sys Rev. 2016 doi: 10.1002/14651858.CD009729.pub2. doi:101002/14651858CD009729pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acosta MC, Gallar J, Belmonte C. The influence of eye solutions on blinking and ocular comfort ate rest and during work at video display terminals. Exp Eye Res. 1999;68:663–9. doi: 10.1006/exer.1998.0656. [DOI] [PubMed] [Google Scholar]
- 20.Computer Vision Syndrome (n.d.), from the American Optometric Association. website: https://www.aoa.org/
- 21.Bhanderi DJ, Choudhary S, Doshi VG. A community-based study of asthenopia in computer operators. Indian J Ophthalmol. 2008;56:51–5. doi: 10.4103/0301-4738.37596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.AOA. The Effect of Computer Use on Eye Health and Vision American Optometric Association. 1997 [Google Scholar]


