Abstract
Objectives:
Toxoplasmosis is one of the neglected parasitic disease in humans and animals that produced via toxoplasma gondii. This study we implemented an umbrella review of all existing systematic reviews, meta-analyzing studies to apprise, and summarize seroprevalence of human toxoplasmosis in worldwide.
Methods:
The search was carried out in databases including: Pub Med, Google Scholar, Science Direct, Scopus, Web of Science, Cochrane, and global health from their start dates until December 2018 in Persian and English language. A total of 21 systematics review and meta-analysis met the inclusion criteria of umbrella review. The Q test and the I2 statistic were used to evaluate heterogeneities. Quality assessment were performed and made use of the AMSTAR tool.
Results:
The estimated pooled seroprevalence of T. gondii infection in blood donors, Immunocompromised patients, childbearing age women, general population, newborns and children, pregnant women and overall was 33% (95% CI, 29.0–38.0%), 42.0% (95 CI, 34.0–49.0%), 32.0% (CI, 26.0–38.0%), 42.0% (CI, 38.0–45.0%), 4.0% (CI, 2.0–5.0%), 40.0% (CI,37.0–44.0%), and 36% (CI, 24.0–48.0%), respectively.
Conclusion:
The results of our umbrella review show a higher seroprevalence of T. gondii infection in immunocompromised patients, general population, pregnant women, blood donors, childbearing age women, and newborn groups, respectively. Routine serologic screening test and health education by primary care physicians for Toxoplasmosis is recommended to be conducted in high-risk groups in the endemic region.
Keywords: Meta-analysis, prevalence, review, toxoplasma gondii, toxoplasmosis
Introduction
Toxoplasmosis is one of the neglected parasitic disease in humans and animals that produced via Toxoplasma gondii.[1,2,3]
Felids are the definitive hosts and repel oocysts in their feces. The oocyst load in areas where cats selectively excrete feces is high.[4,5]
Seroprevalence of T. gondii fluctuates from 30% to 60%, as at least one third of the world's population is infected, which predominantly happens in districts with poor sanitation.[6]
Human are dead-end host for T. gondii with up to 80% given chronic asymptomatic disease.[7,8] Women during pregnancy and immunocompromised persons (cancer, Rheumatoid arthritis, transplant, and HIV/AIDS infected) include the high risk groups for T. gondii.[9,10,11,12]
There have been research about association of T. gondii with mental disorders for example epilepsy,[13,14] bipolar disorder, and schizophrenia.[15,16]
Because of the toxoplasma propensity to the brain and eye, poor prognoses, and sequels for example glaucoma, chorioretinitis, retinal detachment, brain abscess, and encephalitis can happen during severe or recurrent infection.[17,18]
Prevention of T.gondi infection via screening is compulsory in some countries and is suggested in some others such as the United States and Canada.[19,20]
The seroprevalence of toxoplasmosis in human is diverse in different district relevant on variables such as sex, age, immunity status, food behaviors, culture, keeping the cat at home, geographic area, the percentage, and humidity.[19,21]
In recent years, several systematic review and meta-analysis studies have been published exploring the seroprevalence of T. gondii in different country and various groups such as: blood donors, immunocompromised patients, psychosis patients, pregnant women, girls, newborn, and general population and their results indicate different findings.
Therefore, in this study, we implemented an umbrella review of all existing systematic reviews, meta-analyzing studies to apprise and summarize seroprevalence of human toxoplasmosis worldwide. We thus hope to provide both primary care physicians and policy makers with strong data in an easy-to-access and inclusive format to inform guidelines for control and prevention practice.
Methods
Study design
Umbrella reviews (also known as overview of reviews)[22] are a newly developed technique to précis, and analyze systematic reviews. Umbrella review is based on a planned and designed complete search, parallel to traditional systematic reviews, but it searches systematic reviews instead of observational or clinical research (e.g., Cross-Sectional or Clinical Trials).[23]
Now, no generally used guidelines exist to do this type of review. Nevertheless, we followed the references of the PRISMA statement for search approach scheme and made use of the Assessing the Methodological Quality of Systematic Reviews (AMSTAR) tool for quality assessment.[24]
Search strategy
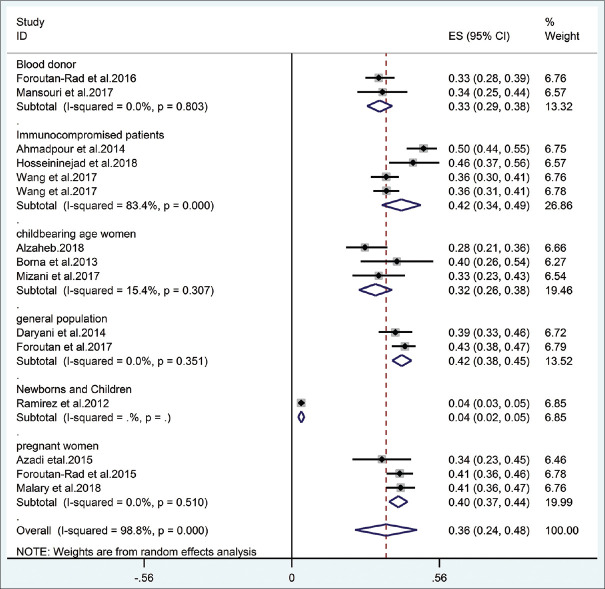
The search was carried out in databases including: Pub Med, Google Scholar, Science Direct, Scopus, Web of Science, Cochrane, and global health from their start dates until December 2018 in Persian and English language. Duplicates and animal-based studies were excluded. All systematic review and meta-analysis studies in human toxoplasmosis were concerned. We included systematic reviews and meta-analyses of observational studies that gave a seroprevalence of Toxoplasmosis. The process is shown in Figure 1.
Figure 1.
Flowchart showing the selection of studies analyzed in Umbrella review
This umbrella review was accomplished using medical subject heading (MeSH) terms and combination of numerous keywords including: “Toxoplasma”, “Toxoplasma gondii”, “Toxoplasmosis,” “Prevalence,” “Seroprevalence,” “Epidemiology,” individually in combination with “meta-analysis,” “systematic review.”
Quality assessment
Rahmanian(V) and Bokaie(S) evaluated quality for totally included papers separately using the AMSTAR checklist.[24] A third author removed disagreement. The assessment base on the AMSTAR tool was done as follow: if the answer is “Yes”, a grade was stated, if “No” or “Can't answer” were signed no grade was stated. When “Not applicable” was signed, no grade was stated but the item was removed from the feasible maximum score.
”If the ultimate score was 80-100% quality was marked as 3 (high quality or very low risk of bias), 65-80% as 2 (acceptable quality or low risk of bias), 50-65% as 1 (low quality or high risk of bias), and ≤50% as 0 (unacceptable quality or very high risk of bias).”[22]
Data collection
Based on the mentioned strategy, the search was performed in six databases. Subsequently, the collected systematics review and meta-analysis were carefully evaluated for epidemiological parameters; finally, 21 reviews had study inclusion criteria, including the accessibility of full text, the study of human toxoplasmosis seroprevalence. Exclusion criteria were data inconsistencies, the use of inappropriate statistical methods, low-quality based on the AMSTAR tool and toxoplasmosis in non-human cases. The data extracted from the review were the name of the author, date of study, demographic information such as types of study groups as well as the geographical area of the study, the number of subjects examined, the seropositive number, and the seroprevalence and the laboratory method used to study [Table 1].
Table 1.
Baseline features of included studies in umbrella review of seroprevalence of Toxoplasma gondii and Quality assessment using the AMSTAR checklist
| Study/authors | Place of study | study group | Number of studies included in the meta-analysis | Population | %Seroprevalence, (95% CI) | % seroprevalence (95% CI) | Quality score | References | |
|---|---|---|---|---|---|---|---|---|---|
| IgM | IgG | ||||||||
| Mansouri et al. 2017 | Iran | Blood donor | 10 | 4538 | 31.84 (20.61-43.08) | 2.74 (0.55-4.92) | 34.4 (24.9-43.9) | 3 | [25] |
| Foroutan-Rad et al. 2016 | worldwide | Blood donor | 43 | 20964 | NA | 1.8 (1.1-2.4) | 33 (28-39) | 3 | [26] |
| Jiang et al. 2015 | china | Population with Cancer | 19 | 4493 | NA | NA | 20.59 (20.11-21.06) | 3 | [11] |
| Borna et al. 2013 | Iran | childbearing age women | 22 | 13480 | 34.5 (28.5-40.5) | NA | 39.9 (26.1-53.7) | 3 | [27] |
| Gebremedhin and Tadesse. 2015 | Etiopia | general population | 19 | 5718 | 74.73 (61.85-84.36) | NA | NA | 3 | [28] |
| Daryani et al. 2014 | Iran | general population | 35 | 52294 | NA | NA | 39.3 33-45.7 | 2 | [29] |
| Mizani et al. 2017 | Iran | childbearing age women | 38 | 17512 | 31 21-41 | 5 3.00-6.00 | 33 23-43 | 3 | [30] |
| Wang et al. 2017 | worldwide | HIV-infected | 74 | 25989 | NA | NA | 35.8 (30.8-40.7) | 3 | [31] |
| Foroutan et al. 2018 | Iran | hemodialysis patients | 10 | 1048 | 58 (46-70) | 2 (0-6) | NA | 3 | [32] |
| Ahmadpour et al. 2014 | Iran | immunocompromised patients | 22 | 2805 | NA | NA | 50.01 (43.85-56.17) | 1 | [33] |
| Wang et al. 2017 | worldwide | Immunocompromised patients | 72 | 17780 | NA | NA | 35.9 (31-40.8) | 3 | [34] |
| Foroutan et al. 2017 | Iran | general population | 117 | 105139 | NA | NA | 43 (38-47) | 3 | [35] |
| Ramirez et al. 2012 | Mexico | general population | 132 | 70123 | NA | NA | 19.27 (18.97-19.56) | 2 | [36] |
| Ramirez et al. 2012 | Mexico | Newborns and Children | 10 | 5728 | NA | NA | 3.63 (2.29-4.935) | 2 | [37] |
| Deng et al. 2017 | China | pregnant women | 72 | NA | 4.37 (2.22-8.1) | NA | NA | 2 | [38] |
| Malary et al. 2018 | Iran | pregnant women | 43 | 22644 | 39.2 (33.3-45.1) | 3.1-4.9 | 41.3 (35.8-46.8) | 3 | [39] |
| Wang et al. 2018 | China | Blood donor | 40 | 49784 | 6.26 (4.62-8.13) | NA | NA | 3 | [40] |
| Foroutan-Rad et al. 2016 | Iran | pregnant women | 50 | 20221 | 38 (34-42) | 4 (3-5) | 41 (36-45) | 3 | [41] |
| Hosseininejad et al. 2018 | worldwide | rheumatoid arthritis patients | 9 | 4168 | NA | NA | 46 (37-56) | 3 | [9] |
| Azadi et al. 2015 | Iran | pregnant women | 28 | 12818 | NA | NA | 34.2 (23-45.3) | 1 | [42] |
| Alzaheb. 2018 | Saudi Arabia | women of reproductive age | 20 | 13597 | NA | NA | 27.8 (20.6-36.3) | 2 | [43] |
Statistical analyses
Point estimates and their 95% confidence intervals of seroprevalence of all included studies were calculated. The seroprevalence (P) and standard error (Se) of each study estimated with respect of binomial distribution and studies combined according to sample size and variance. Forest plot was employed to visualize the heterogeneity among studies. The heterogeneity was expected in advance, and statistical methods, I2 and Q test (with significance of P < 0.05) were used to quantify the variations. All systematic review and meta- analyses included this umbrella review were used a random effects model, and thus a random effects model was employed. Proportions of individual studies and overall seroprevalence were presented by forest plots. Statistical analyses were implemented using Stata, version 12.0 (Stata Corp, College Station, TX, USA). Furthermore, the Arc GIS 10.3 software was applied to map the distribution of T.gondi infection.
Results
In total, 330 systematics review and meta-analysis were obtained by searching the databases referred to in the period from their start dates until December 2018; after reviewing the inclusion criteria and their study, 21 systematics review and meta-analysis met the inclusion criteria of umbrella review. All 21 studies included in the umbrella review evaluated the seroprevalence of T.gondi infection in blood donors, immunocompromised patients, pregnant women, childbearing age women, newborns, and children and general population. A total of 470,843 people were evaluated in 885 primary study in 21 systematics review and meta-analysis met the inclusion criteria of this Umbrella review [Table 1].
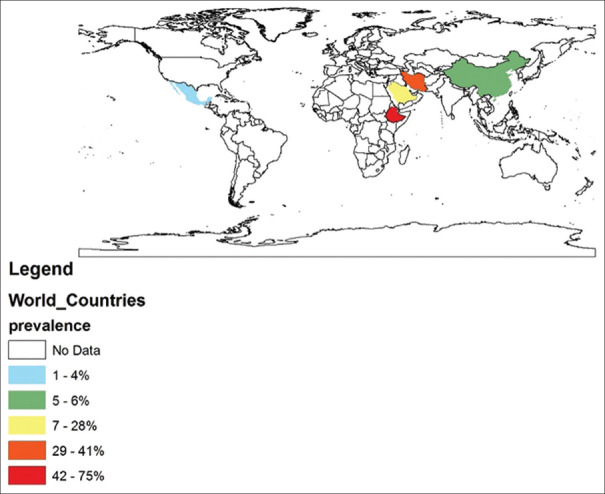
Pooled seroprevalence estimates of (IgM + IgG) T. gondii Infection by study groups
The estimated pooled seroprevalence of T. gondii infection in immunocompromised patients and general population were highest 42% and newborns and children were lowest 4%, respectively [Table 2]. There was high degree of heterogeneity in estimating the seroprevalence of studies in meta-analysis, in which the heterogeneity was I2 = 83.4% (Q test: P < 0.001) in Immunocompromised patient groups and I2 = 98.8% (Q test: P < 0.001) in overall, but there was no heterogeneity in estimated pooled seroprevalence in blood donor, childbearing age women, general population, newborn, and pregnant women groups (P > 0.05) [Figure 2].
Table 2.
Pooled seroprevalence estimates of T. gondii Infection by study groups
| study groups | seroprevalence of T. gondii with positive antibody (%) | ||
|---|---|---|---|
| IgG | IgM | IgM +IgG | |
| blood donors | 18 (8 -43) | 2 (1-2) | 33 (29-38) |
| Immunocompromised patients | 48 (31-66) | 2 (1-5) | 42 (34-49) |
| childbearing age women | 34 (28 -39) | 5 (4-6) | 32 (26-38) |
| general population | - | - | 42 (38-45) |
| newborns and children | - | - | 4 (2-5) |
| pregnant women | 29 (10-48) | 4(3-5) | 40 (37-44) |
| overall | 35 (24-47) | 4 (3-5) | 36 (24-48) |
Figure 2.
Forest plot diagram of Systematic Reviews and Meta-Analyses studies showing seroprevalence (IgM + IgG) of human toxoplasmosis by group population Three meta-analyses reported the seroprevalence of T. gondi infection worldwide and not shown in the map
Pooled seroprevalence estimates of IgG antibodies by study groups
The estimated pooled seroprevalence of IgG in immunocompromised patient was highest %48 and blood donors was lowest 18%, respectively [Table 2]. There was high degree of heterogeneity in estimating the seroprevalence of studies in meta-analysis, in which the heterogeneity was I2 = 94.90% (Q test: P < 0.001) in blood donors' groups, I2 = 86.4% (Q test: P = 0.007) in Immunocompromised patients, I2 = 98.90% (Q test: P < 0.001) in pregnant women and I2 = 98.6% (Q test: P < 0.001) in overall, but there was no heterogeneity in estimated pooled seroprevalence in childbearing age women (P > 0.05).
Pooled seroprevalence estimates of IgM antibodies by study groups
The estimated pooled seroprevalence of IgM in pregnant women was highest 4% and blood donors and immunocompromised patients were lowest 2%, respectively [Table 2].
There was no heterogeneity in estimated pooled seroprevalence in blood donor and pregnant women groups (P > 0.05), but the heterogeneity was I2 = 85.9% (Q test: P < 0.001) in overall.
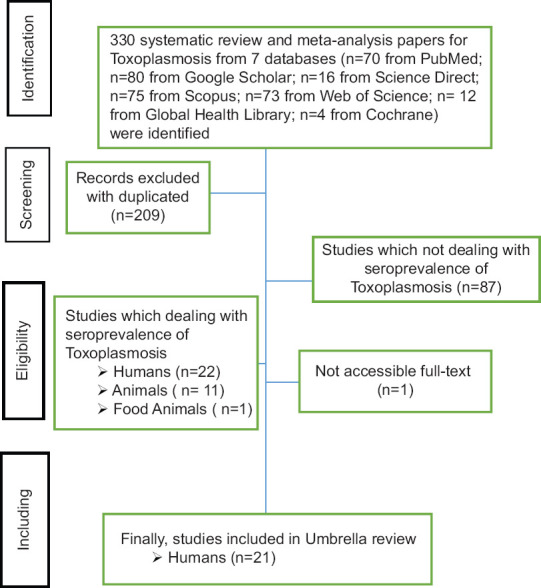
In addition, a schematic image of the T gondii distribution has been made based on studies conducted over the past years among different geographical locations are shown in Figure 3.
Figure 3.
Pooled percentage seroprevalence of Toxoplasma gondii Infection in human of different geographical regions in this umbrella review. This map was created using ArcGIS software by Esri (http://www.esri.com)
Discussion
We have presented an overview of seroprevalence from 21 meta-analyses based on over 470,843 individuals. To our knowledge, this is the first quantitative umbrella review of updated systematic reviews and meta-analyses of the field.
T. gondii infection has been known as a significant opportunistic pathogen in immunocompromised patients.[44] This infection in healthy individuals (immunocompetent) is commonly self-limited and subclinical Infection, consequential in chronic infection of tissue cysts that can status latent, possibly for the full lifetime of the hosts. But, immunocompromised patients, such as HIV-infected, cancer patients with chemotherapy, hemodialysis patients, transplant recipients, rheumatoid arthritis patients with consuming immunosuppressive drugs are at risk of increasing, myocarditis, or pneumonitis, Toxoplasma encephalitis due to recrudescence of the chronic infection.[45] For instance, almost 30-40% of HIV co-infected immunocompromised persons with T. gondii expand encephalitis.[46]
This current study showed that pooled seroprevalence, seroprevalence of IgG and IgM anti-Toxoplasma gondii antibodies in immunocompromised patients was 42%, 48%, and 2%, respectively. Toxoplasmosis is an opportunistic infection in immunocompromised patients with a high mortality rate, causing encephalitis, pneumonitis, and myocarditis due to relapses and chronic reactivation (latent) disease followed by rupture of the cyst of the tissue.
Jiang et al. reported in a systematic review and meta-analysis 20.59% (95% CI: 20.11-21.06%) seroprevalence of T. gondii in the population with cancer in China.[47] Also, Wang et al.[48] and Hosseininejad et al.[9] reported 35.8% and 46% in a meta-analysis of HIV-infected and rheumatoid arthritis patients in worldwide, respectively. In a meta-analysis of IgG antibodies of T. gondii infection in hemodialysis patients was 58% in Iran.[49]
Females commonly do not appear any symptom for Toxoplasmosis infection within pregnancy. In maternal infection, the fetus is possible to be exposed to the mother-to-child transmissions. The complications resulting the mother-to-child transmissions are focal necrosis and inflammation plus congenital abnormalities like eye and brain injuries. In the event of such a serious infection, many sequelae may be created containing deafness, mental retardation, hydrocephalus, and microcephalus.[17]
This umbrella review indicated pooled seroprevalence, seroprevalence of IgG and IgM anti-Toxoplasma gondii antibodies in pregnant women was 40%, 29%, and 4%, respectively. Deng et al.[1] and Malary et al.[39] reported in a systematic review and meta-analysis of pregnant women that 4.37% and 39.2% seroprevalence of IgG anti-Toxoplasma gondii antibodies in china and Iran, respectively.
Two different studies, reported the seroprevalence of Korean pregnant women as 3.7%[50] and 0.8%.[51] Seroprevalence of IgG and IgM among Indian pregnant women was 45% and 3.3%, respectively[52] corresponding values for 1149 Turkish pregnant women were 60.4% and 3.0%, respectively.[53]
Seroprevalence of Toxoplasmosis in Iranian pregnant women like its seroprevalence in other pregnant women around the world is dependent on many factors such as keeping a cat at home or contact with stray infected cats, varied eating habits such as eating raw meat, failing to comply with hygiene principles of storing fruits and vegetables. These factors that directly and indirectly cause of toxoplasmosis in individuals and especially in the sensitive group of pregnant women.
Also, women in childbearing age are the most important group to pay attention to toxoplasmosis infection. This study showed pooled seroprevalence and seroprevalence of IgG anti-Toxoplasma gondii antibodies in women in reproductive age was 32.0% and 34.0%, respectively. Alzaheb reported in a systematic review and meta-analysis that 27.8 seroprevalence of T. gondii in women of reproductive age in Saudi Arabia.[43]
It is necessarily important to realize the status of T. gondii infection in the general population because this infection has heavy socioeconomic effects on people. Families suffer many costs during the care of sick children, particularly those with mental retardation and blindness.[21,54]
Ramirez et al. in one systematic review and meta-analysis reported that 3.63% seroprevalence of Toxoplasma gondii infection in Mexican Newborns and Children.[37]
This overview of reviews indicated pooled seroprevalence of Toxoplasma gondii infection in general population was 42%. Gebremedhin and Tadessein a systematic review and meta-analysis of the general population in Etiopia reported that 74.73% seroprevalence of IgG anti-Toxoplasma gondii antibodies.[28] The Significant high seroprevalence of T. gondii infection in Ethiopian humans can be due to uncontrolled cat movement, abnormal living conditions, and lifestyle and unsanitary behaviors that favor the transmission of parasites from cats or food animals.[28]
Furthermore Ramirez et al.[36] and Foroutan et al.[35] in the two study of systematic review and meta-analysis studies in Mexico and Iran population reported that 19.27% and 43% seroprevalence of T gondii infection, respectively.
Despite the fact that technical betterment in blood donation monitoring and evaluation, transfusion-transmitted T gondii infection remains a possible risk for immune-compromised recipients of transfusions. This study showed that pooled seroprevalence, seroprevalence of IgG and IgM anti-Toxoplasma gondii antibodies in blood donors was 33%, 18.0% and 2%, respectively. Mansouri et al.[25] and Foroutan-Rad et al.[55] in systematic review and meta-analysis in Iran and worldwide reported seroprevalence 34.4% and 33%. Also, Wang et al.[40] reported in a systematic review and meta-analysis that 6.26% seroprevalence of IgG antibodies of T. gondii in blood donors in china.
A limitation of our analyses is the often high levels of doubtful heterogeneity (I2). In our 21 meta-analysis, one study did not report heterogeneity and fourteen meta-analyses had I2 values greater than 60%, which meta-regression of sample size only partly explained in five of these 14 cases. Heterogeneity can be addressed via means of a meta-regression, and sub-group or sensitivity analyses.[56,57] Nevertheless, meta-regressions failed to recognize a factor that could describe the observed heterogeneity,[22] suggesting that the cause was a non-described variable.
This is the first umbrella review of updated systematic reviews and meta-analyses that provides a general view of the seroepidemiology of Toxoplasmosis in the worldwide subgroups population. The results of our umbrella review show a higher seroprevalence of T. gondii infection in immunocompromised patients, general population, pregnant women, blood donors, childbearing age women, and newborn groups, respectively. So, Health education and health promotion, especially toward avoiding consumption raw and uncooked meat and avoiding contact with felines' feces advised. Furthermore, the screening and monitoring for Toxoplasmosis by primary care physicians is recommended to be conducted in high-risk groups in the endemic region.
Ethics in Systematic Reviews
The authors of this study followed the ethical principles of Systematic Reviews, including guidance on authorship, avoiding redundant (duplicate) publication, avoiding plagiarism, transparency, ensuring accuracy that potential complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors hereby would like to express their gratitude and appreciation to Dr. Mohammad Heidari, Assistant Professor of Epidemiology at Urmia University of Medical Sciences, to advise and collaborate on implementing this study in different stages and sections.
References
- 1.Deng H, Devleesschauwer B, Liu M, Li J, Wu Y, van der Giessen JWB, et al. Seroprevalence of Toxoplasma gondii in pregnant women and livestock in the mainland of China: A systematic review and hierarchical meta-analysis. Sci Rep. 2018;8:6218. doi: 10.1038/s41598-018-24361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davami MH, Pourahmad M, Baharlou R, Jahromi AS, Vasmejani AA, Solhjoo K, et al. Seroepidemiology of Toxoplasma infection in blood donors in Jahrom District, Southern Iran. Asian Pac J Trop Biomed. 2015;5:1060–4. [Google Scholar]
- 3.Davami MH, Pourahamd M, Jahromi AR, Tadayon SM. Toxoplasma seroepidemiology in women who intend to marry in Jahrom, Islamic Republic of Iran. East Mediterr Health J. 2014;19(Suppl 3):S71–5. [PubMed] [Google Scholar]
- 4.Fux B, Covre K, Estevan Nazar Lopes R, Bresciani Salaroli L, Wagner De almeida Vitor R, et al. Seroprevalence of toxoplasmosis in cats in Espirito Santo State, Brazil. Curr Devel Nutr. 2020;4:186. [Google Scholar]
- 5.Brennan A, Hawley J, Dhand N, Boland L, Beatty JA, Lappin MR, et al. Seroprevalence and risk factors for Toxoplasma gondii infection in owned domestic cats in Australia. Vector-Borne Zoonotic Dis. 2020;20:275–80. doi: 10.1089/vbz.2019.2520. [DOI] [PubMed] [Google Scholar]
- 6.Wei HX, Wei SS, Lindsay DS, Peng HJ. A systematic review and meta-analysis of the efficacy of anti-toxoplasma gondii medicines in humans. PLoS One. 2015;10:e0138204. doi: 10.1371/journal.pone.0138204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desmettre T. Toxoplasmosis and behavioural changes. J Fr Ophtalmol. 2020;43:89–93. doi: 10.1016/j.jfo.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Molan A, Nosaka K, Hunter M, Wang W. Seroprevalence and associated risk factors of Toxoplasma gondii infection in a representative Australian human population: The Busselton health study. Clin Epidemiol Global Health. 2020;8:1–7. [Google Scholar]
- 9.Hosseininejad Z, Sharif M, Sarvi S, Amouei A, Hosseini SA, Nayeri Chegeni T, et al. Toxoplasmosis seroprevalence in rheumatoid arthritis patients: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12:e0006545. doi: 10.1371/journal.pntd.0006545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y, Huang Y, Chang A, Wang J, Zeng X, Wu J. Is toxoplasma gondii infection a risk factor for leukemia? An evidence-based meta-analysis. Med Sci Monit. 2016;22:1547–52. doi: 10.12659/MSM.897155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang C, Li Z, Chen P, Chen L. The seroprevalence of Toxoplasma gondii in Chinese population with cancer a systematic review and meta-analysis. Medicine (United States) 2015;94:e2274. doi: 10.1097/MD.0000000000002274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmadpour E, Daryani A, Sharif M, Sarvi S, Aarabi M, Mizani A, et al. Toxoplasmosis in immunocompromised patients in Iran: A systematic review and meta-analysis. J Infect Dev Ctries. 2014;8:1503–10. doi: 10.3855/jidc.4796. [DOI] [PubMed] [Google Scholar]
- 13.Palmer BS. Meta-analysis of three case controlled studies and an ecological study into the link between cryptogenic epilepsy and chronic toxoplasmosis infection. Seizure. 2007;16:657–63. doi: 10.1016/j.seizure.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Ngoungou EB, Bhalla D, Nzoghe A, Dardé ML, Preux PM. Toxoplasmosis and epilepsy — systematic review and meta analysis. PLoS Negl Trop Dis. 2015;9:e0003525. doi: 10.1371/journal.pntd.0003525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sutterland AL, Fond G, Kuin A, Koeter MW, Lutter R, van Gool T, et al. Beyond the association. Toxoplasma gondii in schizophrenia, bipolar disorder, and addiction: Systematic review and meta-analysis. Acta Psychiatr Scand. 2015;132:161–79. doi: 10.1111/acps.12423. [DOI] [PubMed] [Google Scholar]
- 16.de Barros JLVM, Sutterland AL, Fond G, Kuin A, Koeter MW, Lutter R, van Gool T, et al. Is there any association between Toxoplasma gondii infection and bipolar disorder? A systematic review and meta-analysis. J Affect Disord. 2017;209:59–65. doi: 10.1016/j.jad.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Montoya JG, Boothroyd JC, Kovacs JA. 280 - Toxoplasma gondii. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Eighth Edition. Philadelphia: Content Repository Only!; 2015. pp. 3122–53. [Google Scholar]
- 18.Bresciani KDS, Da Costa AJ. Congenital Toxoplasmosis in Humans and Domestic. Animals Bentham Science Publishers; 2018. [Google Scholar]
- 19.Daryani A, Sarvi S, Aarabi M, Mizani A, Ahmadpour E, Shokri A, et al. Seroprevalence of Toxoplasma gondii in the Iranian general population: A systematic review and meta-analysis. Acta Tropica. 2014;137:185–94. doi: 10.1016/j.actatropica.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 20.Makiani MJ, Davoodian P, Golsha R, Dehghani M, Rajaee M, Mahoori K, et al. Seroepidemiology and risk factors of toxoplasmosis in the first trimester among pregnant women. Int Electron J Med. 2012;1:12–7. [Google Scholar]
- 21.Roberts T, Frenkel J. Estimating income losses and other preventable costs caused by congenital toxoplasmosis in people in the United States. J Am Vet Med Assoc. 1990;196:249–56. [PubMed] [Google Scholar]
- 22.Martin-Saavedra JS, Vergara-Mendez LD, Talero-Gutierrez C. Music is an effective intervention for the management of pain: An umbrella review. Complement Ther Clin Pract. 2018;32:103–14. doi: 10.1016/j.ctcp.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 24.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mansouri A, Adhami Mojarad MR, Badfar G, Abasian L, Rahmati S, Kooti W, et al. Epidemiology of Toxoplasma gondii among blood donors in Iran: A systematic review and meta-analysis. Transfusion Apheresis Sci. 2017;56:404–9. doi: 10.1016/j.transci.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Foroutan-Rad M, Majidiani H, Dalvand S, Daryani A, Kooti W, Saki J, et al. Toxoplasmosis in blood donors: A systematic review and meta-analysis. Transfus Med Rev. 2016;30:116–22. doi: 10.1016/j.tmrv.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Borna S, Majidiani H, Dalvand S, Daryani A, Kooti W, Saki J. Prevalence of immunity to toxoplasmosis among Iranian childbearing age women: Systematic review and meta-analysis. Iran J Reprod Med. 2013;11:861–8. [PMC free article] [PubMed] [Google Scholar]
- 28.Gebremedhin EZ, Tadesse G. A meta-analysis of the prevalence of Toxoplasma gondii in animals and humans in Ethiopia. Parasites Vectors. 2015:8. doi: 10.1186/s13071-015-0901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daryani A, Sarvi S, Aarabi M, Mizani A, Ahmadpour E, Shokri A, et al. Seroprevalence of Toxoplasma gondii in the Iranian general population: A systematic review and meta-analysis. Acta Tropica. 2014;137:185–94. doi: 10.1016/j.actatropica.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Mizani A, Alipour A, Sharif M, Sarvi S, Amouei A, Shokri A, Rahimi MT, et al. Toxoplasmosis seroprevalence in Iranian women and risk factors of the disease: A systematic review and meta-analysis. Trop Med Health. 2017;45:7. doi: 10.1186/s41182-017-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang ZD, Wang SC, Liu HH, Ma HY, Li ZY, Wei F, et al. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people: A systematic review and meta-analysis. Lancet HIV. 2017;4:e177–88. doi: 10.1016/S2352-3018(17)30005-X. [DOI] [PubMed] [Google Scholar]
- 32.Foroutan M, Rostami A, Majidiani H, Riahi SM, Khazaei S, Badri M, et al. A systematic review and meta-analysis of the prevalence of toxoplasmosis in hemodialysis patients in Iran. Epidemiol Health. 2018;40:e2018016. doi: 10.4178/epih.e2018016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmadpour E, Daryani A, Sharif M, Sarvi S, Aarabi M, Mizani A, et al. Toxoplasmosis in immunocompromised patients in Iran: A systematic review and meta-analysis. J Infect Dev Ctries. 2014;8:1503–10. doi: 10.3855/jidc.4796. [DOI] [PubMed] [Google Scholar]
- 34.Wang ZD, Liu HH, Ma ZX, Ma HY, Li ZY, Yang ZB, et al. Toxoplasma gondii infection in immunocompromised patients: A systematic review and meta-analysis. Front Microbiol. 2017;8:389. doi: 10.3389/fmicb.2017.00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Foroutan M, Dalvand S, Daryani A, Ahmadpour E, Majidiani H, Khademvatan S, et al. Rolling up the pieces of a puzzle: A systematic review and meta-analysis of the prevalence of toxoplasmosis inIran. Alexandria journal of medicine. 2018;54:189–96. [Google Scholar]
- 36.Galvan-Ramirez Mde L, Troyo R, Roman S, Calvillo-Sanchez C, Bernal-Redondo R. A systematic review and meta-analysis of Toxoplasma gondii infection among the Mexican population. Parasit Vectors. 2012;5:271. doi: 10.1186/1756-3305-5-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Galvan-Ramírez Mde L, Troyo-Sanroman R, Roman S, Bernal-Redondo R, Vázquez Castellanos JL. Prevalence of toxoplasma infection in Mexican newborns and children: A systematic review from 1954 to 2009. ISRN Pediatr. 2012;2012:501216. doi: 10.5402/2012/501216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deng H, Devleesschauwer B, Liu M, Li J, Wu Y, van der Giessen JWB, et al. Seroprevalence of Toxoplasma gondii in pregnant women and livestock in the mainland of China: A systematic review and hierarchical meta-analysis. Sci Rep. 2018;8:6218. doi: 10.1038/s41598-018-24361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malary M, Hamzehgardeshi Z, Moosazadeh M, Afshari M, Ahmadi I, Moghaddasifar I, et al. Seroprevalence of Toxoplasma gondii infection among Iranian pregnant women: A systematic review and meta-analysis. East Mediterranean Health J. 2018;24:488–96. doi: 10.26719/2018.24.5.488. [DOI] [PubMed] [Google Scholar]
- 40.Wang T, Han Y, Pan Z, Wang H, Yuan M, Lin H. Seroprevalence of Toxoplasma gondii infection in blood donors in mainland China: A systematic review and meta-analysis. Parasite. 2018;25:36. doi: 10.1051/parasite/2018037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Foroutan-Rad M, Khademvatan S, Majidiani H, Aryamand S, Rahim F, Malehi AS. Seroprevalence of Toxoplasma gondii in the Iranian pregnant women: A systematic review and meta-analysis. Acta Tropica. 2016;158:160–9. doi: 10.1016/j.actatropica.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 42.Azadi T, Darabi M, Sayehmiri F, Sayehmiri K. Investigating the prevalence of toxoplasmosis in Iranian pregnant women: A Systematic review and meta-analysis. Sci J Ilam Univ Med Sci. 2017;25:148–58. [Google Scholar]
- 43.Alzaheb RA. Seroprevalence of Toxoplasma gondii and its associated risk factors among women of reproductive age in Saudi Arabia: A systematic review and meta-analysis. Int Jf Women's Health. 2018;10:537–44. doi: 10.2147/IJWH.S173640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmadpour E, Daryani A, Sharif M, Sarvi S, Aarabi M, Mizani A, et al. Toxoplasmosis in immunocompromised patients in iran: A systematic review and meta-analysis. J Infect Dev Ctries. 2014;8:1503–10. doi: 10.3855/jidc.4796. [DOI] [PubMed] [Google Scholar]
- 45.Machala L, Kodym P, Malý M, Geleneky M, Beran O, Jilich D. Toxoplasmosis in immunocompromised patients. Epidemiol Mikrobiol Imunol. 2015;64:59–65. [PubMed] [Google Scholar]
- 46.Snydman DR, Walker M, Zunt JR. Parasitic central nervous system infections in immunocompromised hosts. Clin Infect Dis. 2005;40:1005–15. doi: 10.1086/428621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jiang C, Li Z, Chen P, Chen L. The seroprevalence of Toxoplasma gondii in Chinese population with cancer: A systematic review and meta-analysis. Medicine. 2015;94:e2274. doi: 10.1097/MD.0000000000002274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang ZD, Wang SC, Liu HH, Ma HY, Li ZY, Wei F, et al. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people: A systematic review and meta-analysis. Lancet HIV. 2017:e177–88. doi: 10.1016/S2352-3018(17)30005-X. [DOI] [PubMed] [Google Scholar]
- 49.Foroutan M. A systematic review and meta-analysis of the prevalence of toxoplasmosis in hemodialysis patients in Iran. PLoS Negl Trop Dis. 2018;40:e2018016. doi: 10.4178/epih.e2018016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Han K, Shin DW, Lee TY, Lee YH. Seroprevalence of Toxoplasma gondii infection and risk factors associated with seropositivity of pregnant women in Korea. J Parasitol. 2008;94:963–5. doi: 10.1645/GE-1435.1. [DOI] [PubMed] [Google Scholar]
- 51.Song K-J, Shin JC, Shin HJ, Nam HW. Seroprevalence of toxoplasmosis in Korean pregnant women. Korean J Parasitol. 2005;43:69. doi: 10.3347/kjp.2005.43.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh S, Pandit AJ. Incidence and prevalence of toxoplasmosis in Indian pregnant women: A prospective study. Am J Reprod Immunol. 2004;52:276–83. doi: 10.1111/j.1600-0897.2004.00222.x. [DOI] [PubMed] [Google Scholar]
- 53.Harma M, Gungen N, Demir N. Toxoplasmosis in pregnant women in Sanliurfa, Southeastern Anatolia City, Turkey. J Egypt Soc Parasitol. 2004;34:519–25. [PubMed] [Google Scholar]
- 54.Roberts T, Murrell KD, Marks S. Economic losses caused by foodborne parasitic diseases. Parasitol Today. 1994;10:419–23. doi: 10.1016/0169-4758(94)90171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foroutan-Rad M, Majidiani H, Dalvand S, Daryani A, Kooti W, Saki J, et al. Toxoplasmosis in blood donors: A systematic review and meta-analysis. Transfus Med Rev. 2016;30:116–22. doi: 10.1016/j.tmrv.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 56.Cornell JE, Liao JM, Stack CB, Mulrow CD. Annals understanding clinical research: Evaluating the meaning of a summary estimate in a meta-analysis. Ann Internal Med. 2017;167:275–7. doi: 10.7326/M17-1454. [DOI] [PubMed] [Google Scholar]
- 57.Bigby M. Understanding and evaluating systematic reviews and meta-analyses. Indian J Dermatol. 2014;59:134–9. doi: 10.4103/0019-5154.127671. [DOI] [PMC free article] [PubMed] [Google Scholar]