Abstract
Introduction:
Fasting is observed as a religious custom in various forms across the globe. Among them, the Ramadan fasting is very common and widely practiced. People with diabetes observe fasting with or without obtaining medical advice. Uncontrolled diabetes appears to be a risk factor for COVID-19 infection and its poorer outcomes. Fasting during Ramadan is challenging in people with diabetes. This year, the background of COVID-19 made it difficult for both the patients and health care workers to effectively manage diabetes and its complications during Ramadan. Because of a lack of sufficient evidence, clinicians were perplexed in handling this difficult situation.
Materials and Methods:
We accessed PubMed, Google Scholar, various guidelines and other evidence-based articles to review the available current literature which deals with diabetes, Ramadan, and COVID-19.
Results:
The importance of pre-Ramadan assessment, adequate nutrition, and hydration, choosing the right therapy has been emphasized. This review tries to address the common practical challenges and relevant possible solutions for the same. Due consideration has been given to various socio-cultural practices that can influence the management of diabetes patients in the setting of Ramadan and COVID-19 pandemic.
Conclusions:
Diabetes is associated with increased severity and susceptibility to COVID-19. People with diabetes should go through systemic and structure-based management during fasting. Family physicians who deliver personalized care play a vital role in managing diabetes during this crisis period. Telemedicine is emerging as an effective mode of managing various needs of individuals.
Keywords: COVID-19, diabetes, fasting, India, primary care physician, Ramadan
Introduction
Religious fasting is a form of intermittent [time-restricted] fasting.[1] Fasting during Ramadan is one of the five pillars of Islam.[2] Coronavirus disease [COVID-19] caused by Severe Acute Respiratory Syndrome Coronavirus 2 [SARS-CoV-2] is a global public health issue. Diabetes tops the disease-wise COVID-19 fatality rate (DFR) with 39.4% in our country.[3] This COVID-19 pandemic poses different challenges for both patients and health care professionals [HCPs] during Ramadan. This review focusses on the possible solutions in managing diabetes during Ramadan in the background of COVID-19 for both primary and specialist-care physicians.
Background
COVID-19 is transmitted mainly by droplets and fomites.[4] India is the largest hub of COVID-19 in South Asia.[5] The fasting observed in various religions can be either periodic or during special occasions.[6] Approximately two billion Muslims observe the obligatory fasting from dawn to sunset during the holy month of Ramadan.[2] Fasting can last for 11–20 hours a day depending on the latitude.[7] The Epidemiology of Diabetes and Ramadan [EPIDIAR] study and the CREED study showed that 78–94% of Muslim diabetes subjects fasted for at least 15 days.[8,9] Individuals who are ill, travelling, pregnant, or at high-risk for complications are exempted from fasting. Despite religious exemptions being available, a significant number of them continue to fast.[10]
A recent prospective study on individuals with diabetes reported that nearly 67% of them did not receive proper guidance and follow-up prior to and during the fasting period.[7] The clinicians find it challenging to provide a holistic care to individuals in special situations due to the lack of knowledge on beliefs, practices, and religious customs.[11] Hence, the physicians must be aware about various aspects of fasting and diabetes management.
Rationale Behind this Review
In 2019, nearly 463 million adults had diabetes globally, and the figure is expected to rise to 700 million by 2045.[12] The entire country went into a complete lockdown on March 24, 2020. Millions of people are forced to remain indoors.[13] Diabetes with high chances of hypo and hyperglycemia, which can be fatal is considered a risk for people fasting during Ramadan.[14] Family Physicians are the first point of contact for most of the acute illnesses including COVID-19. Clinical decision making becomes complicated in such difficult situations. As there are very few articles on this subject, this is likely to be the first guidance for primary care physicians to manage diabetes in Ramadan during the COVID-19 pandemic considering the socio-cultural issues relevant to the present scenario.
Methodology
We identified the references through searches in PubMed and Google Scholar for articles published in English from May 2000 to June 2020 using keywords such as “coronavirus,” “COVID-19,” “Diabetes,” “Ramadan,” and “Family physician.” Guidelines for the management of Diabetes in Ramadan published by the American Diabetes Association [ADA], International Diabetes Federation [IDF], International Group for Diabetes and Ramadan [IGDR], and South Asian Consensus Statement were reviewed. We also looked into the guidelines for the management of COVID-19 issued by the World Health Organization [WHO], US Centers for Disease Control and Prevention, the Ministry of Health and Family Welfare, Government of India, and Indian Council of Medical Research [ICMR]. We also reviewed relevant references cited in the retrieved articles and personal files of the authors. The final reference list was compiled based on the relevance of the information provided.
Ramadan and Diabetes
Impact of fasting on the daily routine
Fasting during Ramadan induces a sudden change in meal times, sleep, and wakefulness patterns. The day starts early for most Muslims before dawn to have the morning meal [Suhoor]. The food consumed after the period of fasting is usually calorie-dense contributing to hyperglycemia.[11] During Ramadan, there is a paradoxical risk of excessive eating after hours of fasting. Hence, high-calorie intake with decreased physical activity may sometimes, lead to weight gain.[15]
Some might return to sleep afterward and wake up later to begin the day. Following Iftar [evening meal], many stay awake until midnight, or later. This usually leads to a reduction in rapid eye movement [REM] sleep and total sleep duration which causes an increase in glucose intolerance.[16] The change in the circadian rhythm can negate the benefits of intermittent fasting.[1] The individuals who do not receive medical advice before fasting tend to continue their routine medications and end up with recurrent hypoglycemic events. The physical activity during the day time is lesser compared to the night. There is also a prevailing misconception that monitoring the blood glucose would void the fast.[11]
Complications due to fasting
In those with Type 1 Diabetes Mellitus [T1DM], fasting leads to excessive glycogen breakdown and increased gluconeogenesis along with increased ketogenesis. Type 2 Diabetes Mellitus [T2DM] patients also have similar risk especially if poorly controlled. Thus, the risk of hypoglycemia, hyperglycemia, diabetic ketoacidosis [DKA], dehydration, and thrombosis are heightened during this period in all patients with long-standing diabetes.[17] However, hypoglycemic episodes are more common and fatal compared to hyperglycemic complications.[7]
There is evidence that the majority [90%] of the individuals observing the fast do not discontinue the fast in the background of hypoglycemia.[7] The EPIDIAR study, a landmark trial reported an increase in the incidence of severe hypoglycemia during Ramadan in people with T1DM and T2DM compared with non-Ramadan periods.[8] In T1DM, fasting seems to inhibit glucagon secretion in response to hypoglycemia, leading to subsequent hypoglycemic episodes.[17] Those with autonomic neuropathy are at a higher risk and respond inadequately to hypoglycemic episodes.[18]
Although fasting causes drastic changes in sleep patterns and dietary habits, which can lead to complications, there are a plethora of benefits [Table 1].[15,19] There are no major adverse effects of Ramadan fasting on the systemic functions provided the advice given by the physician is followed.[15]
Table 1.
| Metabolic Benefits | Other Systemic Benefits |
|---|---|
| Reduction in plasma glucose | Increases average life expectancy and promotes psychological well-being |
| Increase in insulin sensitivity | Improves physical composition and function |
| Reduction in Low Density Lipoprotein-C, total cholesterol, and triglyceride level | Enhances cognitive functions - spatial, associative and working memory |
| Increase in High Density Lipoprotein-C level | Reduction in Atherosclerosis risk |
| Regulation of sleep pattern and ageing | |
| Reduction in blood pressure | Protects against cancer, diabetes, obesity |
| Reduction in total body weight | Delay or reverse stroke, Alzheimers disease, and Parkinsons disease |
| Reduction in waist circumference | Alleviates symptoms of asthma, multiple sclerosis, and arthritis. |
| Reduction of inflammatory marker |
LDL-C: Low Density Lipoprotein-C, HDL-C: High Density Lipoprotein-C
Ramadan-Specific Diabetes Management
It is essential to individualize every patient and provide comprehensive and continuous diabetes education.[20] Pre-Ramadan assessment ideally done two months before the start of Ramadan for risk stratification[21,22,23] [Table 2], medication dose modification along with regular blood glucose monitoring has reduced the rate of hospitalization during Ramadan.[24] A pre-Ramadan assessment [Figure 1] comprising of risk stratification and quantification, identification of the type of diabetes, risk of hypoglycemia, presence of any complications or comorbidities, current medications, previous Ramadan fasting experience, and personal background is essential for all patients especially those considered to be at high-risk for complications.[21]
Table 2.
Risk stratification for people with Diabetes wishing to fast during Ramadan in the background of COVID -19 Pandemic[21,22,23]
| Category | Situation |
|---|---|
| Very High | Poorly controlled patients (HbA1c >8.5%) (Average blood glucose >300 mg/dL) |
| Risk | Type 1 Diabetes mellitus |
| History of Hypoglycemic unawareness, severe or recurrent hypoglycemia, Diabetic ketoacidosis or hyperosmolar hyperglycemic coma in the last 3 months | |
| Acute illness | |
| Pre- existing DM in pregnancy or Gestational DM on insulin | |
| Immunocompromised patients [HIV, Cancer, PTB, Transplant recipients, on immunosuppressants] | |
| Associated co-morbidities like heart failure, recent myocardial infarction, hepatic failure, severe respiratory illness, CKD Stage 4 and 5] | |
| Elderly who are ill | |
| COVID-19 positive patients, or with history of contact or travel with COVID-19 positive patients. | |
| High risk | Moderately controlled patients (HbA1c 7.5-8.5%) (Average blood glucose 150-300 mg/dL) |
| Renal insufficiency- CKD stage 3 | |
| Pregnant and lactating women- controlled by diet only or metformin | |
| Living alone on multiple insulin injections | |
| Autonomic neuropathy, moderate to severe micro and microvascular complications | |
| Members living in same premises of COVID-19 positive patient | |
| Moderate risk | Patients with good glycemic control (HbA1c 7-7.5%) |
| On insulin, oral anti-diabetes agents, GLP-1 receptor agonists | |
| People living in COVID-19 hotspot areas | |
| Low risk | Well controlled patients (HbA1c <7%) |
| On lifestyle modification only or monotherapy and healthy |
GLP-1: Glucagon-Like-Peptide, CKD: Chronic kidney disease, DM : Diabetes mellitus, HIV : Human Immunodeficiency virus, PTB : Pulmonary tuberculosis. Adapted from: ADA 2020, IDF 2016, IGDR 2015, IDF-DAR Practical Guidelines, South Asian Consensus Guidelines, ICMR guidelines, South Asian Health Foundation Update
Figure 1.
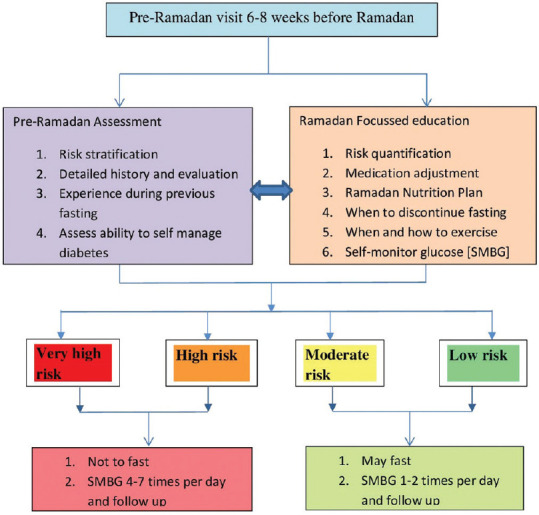
Approach to a patient with Diabetes wishing to fast during Ramadan
The Ramadan Education and Awareness in Diabetes [READ] study showed that a structured education caused significant reduction in hypoglycemic events in people with Type 2 Diabetes.[25] Diabetes and Ramadan International Alliance have developed a web-based tool to help HCP's to provide patient-centered medical nutrition therapy during Ramadan.[21] In general, people with T1DM with a history of recurrent hypoglycemia, hypoglycemia unawareness, uncontrolled diabetes, non-compliance to treatment, difficulty in monitoring and managing blood glucose levels, and brittle diabetes should strictly avoid fasting. Those who still insist on fasting must do it under close medical supervision.[26]
Self-monitoring of blood glucose [SMBG] is required in all those who fast. The various recommended timings to check blood glucose levels are before Suhoor, 2 hours after Suhoor, at noon, mid-afternoon, before Iftar, 2 hours after Iftar, and at any time the person feels unwell or has symptoms of hypoglycemia or hyperglycemia.[21] All patients should be sensitized regarding the dangers of very low and very high blood sugars, and be advised to break the fast if blood glucose is lesser than 70 mg/dL or is greater than 300 mg/dL.[23] As family physicians, the fact that SMBG during the day does not violate the fast should be communicated to the patient.
Optimal Ramadan Nutrition Plan
The goal should be to improve the glycemic control, help people with overweight or obesity to make use of the opportunity, and lose excess weight during Ramadan. Also, we should assist them in choosing a proper diet plan according to their lifestyle and exercise plan during Ramadan. We must provide education to help patients identify the warning symptoms of hypoglycemia, dehydration, and other complications.[21] An Optimal Ramadan Nutrition Plan includes a balanced diet with adequate hydration [Table 3].
Table 3.
Dietary recommendations for patients with diabetes during Ramadan fasting[21]
| • Calorie requirement is 1800-2200 kcal/day for men and 1500-2000 kcal/day for women |
| • Divide daily calories=Suhoor (30-40%) + Iftar (40-50%) + Snacks (10-20%) once or twice between meals if necessary |
| • Balanced diet with 45-50% carbohydrate, 20-30% protein, <35% fat (preferably mono- and polyunsaturated), fibre 20-35 gram per day |
| • Adequate protein and fat ensures satiety and reduced postprandial hyperglycemia |
| • Include low glycemic index, high fibre foods that release energy slowly before and after fasting |
| • Include adequate fruit, vegetables and salads |
| • Minimise foods that are high in saturated fats like samosas, pakoras |
| • Avoid sugary desserts |
| • Keep hydrated whenever possible by drinking water and other non-sweetened beverages |
| • Avoid caffeinated and sweetened drinks |
| • Avoid large calorie dense meal, and take smaller meals divided into two or three |
Physical Activity during Ramadan
In general, exercise improves glycemic control and lipid profile thereby lowering the cardiovascular risk. Exercise during the postprandial period in Ramadan reduces the oxidative stress and carbonyl stress, decreases mean amplitude of glucose excursion [MAGE], mean postprandial glucose excursion [MPPGE], and average plasma glucose.[27] Prayer by itself [Namaaz] involves repeated movements like bending, kneeling, bowing, and rising. One to two hours after Iftar is the daily night [Isha] prayer, followed by the special Ramadan prayer called Tarawih, which lasts for almost an hour can control post-meal hyperglycemia.
It is important to avoid hypovolemia, hypoglycemia, and hyperglycemia and personalize the exercise according to the daily schedule during Ramadan. No exercise should be performed in the hours before Iftar due to the risk of hypoglycemia. It is advisable to do moderate-intensity exercise modifiable to the altered pattern of eating, sleeping, and working. Strengthening and stretching exercises can be performed as per the recommendations [Table 4].[28,29] Those with a tendency for unpredictable hypoglycemic episodes or with retinopathy, nephropathy, or neuropathy should be advised regarding the glucose monitoring and limiting the exercise accordingly.[29]
Table 4.
| Situations | Recommendations |
|---|---|
| Those on lifestyle modification | Modifying frequency and intensity of physical activity. |
| Type 2 Diabetes on oral medications or insulin | Avoid exercise before Iftar. |
| Type 1 Diabetes | Personalised decision, Avoid intense exercise. |
| Preferable mode of exercise | Maintain normal daily routine, walking, stationary cycling. Perform Tarawih prayers. |
| Exercise timing (depending on work pattern during Ramadan) | Preferably 2 hours after Iftar, after night (Isha) and after midnight (Tahajud) prayers. |
|
General recommendations 1. Glucose monitoring needed before, during and after exercise in very high and high-risk individuals.
2. Ensure adequate hydration before and after exercise. | |
COVID-19 and Diabetes
Susceptibility and vulnerability of diabetes to COVID-19
Most people with COVID-19 have comorbidities, of which, diabetes, cardiovascular disease, and hypertension are the most prevalent.[30] Few mechanisms have been proposed that could play a role in COVID-19 infection by enhancing the susceptibility of patients with diabetes, but the conclusive association could not be established due to paucity in literature.[31,32] Imbalance in Angiotensin-Converting Enzyme [ACE2] expression by COVID-19 in diabetes can lead to hyper-inflammation, cell damage, and respiratory failure.[33] COVID-19 may also cause beta-cell damage leading to insulin deficiency.[34] Dysfunctional pro-inflammatory cytokine response could be another possible cause of severe COVID-19 in diabetes.[35]
Recent evidence shows that there is a bidirectional relationship between COVID-19 and diabetes.[36] Chronic hyperglycemic and inflammatory states are associated with immunosuppression and hence, diabetes patients may be at high risk of contracting COVID-19 and associated complications.[13] Compared to those with well-controlled glycemic status, poor glycemic control in patients with COVID-19 and pre-existing type 2 diabetes was shown to be associated with multi-organ damage, increased need for medical interventions, and higher mortality. In contrast, those with glycemic variability between 70 and 180 mg/dL had a significant reduction in complications.[37] However, those with prediabetes and metabolic dysfunction associated fatty liver disease [MAFLD] are also at high risk for COVID-19 and its complications.[38] Special attention should be given to patients with fatty liver disease and obesity as they may have a marked inflammatory response including the cytokine storm.[39]
A recent meta-analysis demonstrated that diabetic patients with COVID-19 have a higher risk for Intensive care unit admission [Odds ratio (OR) 2.79] during the infection. Moreover, DM increased the risk of mortality [OR 3.21] during the infection.[40] Glycosylated hemoglobin [HbA1c] estimation during hospitalization provides an opportunity to differentiate patients with stress hyperglycemia from those with previously undiagnosed diabetes, and to optimize their treatment regimen.[41] Inpatient hyperglycemia is an independent marker of poor outcomes during the hospital stay in patients irrespective of previous glycemic status.[42] The CORONADO [Coronavirus SARS-CoV-2 and Diabetes Outcomes] study revealed that a longstanding good glycemic control did not favor the COVID-19 affected patients with diabetes.[43] International Society for Pediatric and Adolescent Diabetes summary of recommendations regarding COVID-19 in children with diabetes stated that children with diabetes in general, are less affected than adults[44] possibly due to a unique ACE2 plasma profile.[45] But there have been multiple reports of patients presenting to emergency services with severe DKA.[46]
Management of diabetes patients unaffected by COVID-19
Recent studies have raised concerns regarding the risks of new-onset diabetes, weight gain, and metabolic alterations in apparently healthy individuals due to the lifestyle changes which develop during home confinement or lockdown.[47] Lifestyle modification, proper patient-education, and regular follow-up improves the glycemic status and quality of life in individuals with diabetes.[48] Physical activity of a minimum of 150 minutes per week should be advised to compensate for the loss of activity due to the absence of work during the lockdown period. There are also many patient-related social concerns amidst the present lockdown which needs to be addressed [Table 5].[4,49,50]
Table 5.
| Challenges | Solutions |
|---|---|
| Disruption of pharmaceutical supply | Secure stable stock of medication |
| Loss of access to healthcare | Virtual consultation, Volunteer help |
| Lonely, technologically challenged | Telephonic consultation |
| Fear of glycemic variation | Regular self-monitoring blood glucose |
| Offering Zakaat | Pre-packaged food and safe distancing |
| Faith-based teachings and practices | Religious leaders on digital platform |
| Conducting religious gatherings | WHO risk assessment tool |
| Ensuring safe precautions | Advocacy by religious organizations in liaison with local health authorities |
| Holding Prayers after approval | Social distancing at entry and exit points |
| Smaller, shorter and periodic prayers | |
| Face mask and handwashing facility | |
| Personal prayer rugs | |
| Usage of alcohol-based hand rub | Not forbidden as topical medication |
In general, the ADA recommends a target HbA1c of less than 7%, pre-prandial plasma glucose levels of 80–130 mg/dL and postprandial peak glucose levels less than 180 mg/dl except in certain young individuals where lower targets are recommended if achievable without causing hypoglycemia and higher targets in elderly individuals with or without comorbidities which may predispose to hypoglycemia.[51] A more frequent SMBG will help in early recognition of any deviation from glycemic targets. In patients not affected by COVID-19, the usual medications may be continued under regular monitoring.
Management of Diabetes patients affected by COVID-19
Various glucose-lowering therapies may require dose modification during times of COVID-19 and fasting [Tables 6, 7].[28,34,44,52,53,54] As a strategy to limit the risk of repeated exposures, a non-critically ill patient may be provided a glucose meter and SMBG taught to communicate values over the phone. Alternative strategies to protect HCP's include, use of a single daily dose of basal insulin, insulin pump, or continuous subcutaneous insulin infusion which can be managed remotely with Bluetooth.[52] The decision regarding target glycemic goals, drug selection, and route of insulin administration may differ among different subsets of patients [Table 8].[28,34,52] For T1DM individuals, nearly 4–6 times daily SMBG is essential. If the value is above 250 mg/dL for more than two times, urine ketones need to be checked. In case the urine ketone is positive, the patient requires to be hospitalized and managed as DKA according to the hospital or standard protocols.[28] Based on currently available evidence and recommendations, patients should continue with their antihypertensive regimens including ACE Inhibitor [ACEI], Angiotensin Receptor Blocker [ARB], and statins.[55]
Table 6.
| Glucose-lowering Therapy | Recommendation during Ramadan Fasting | Recommendation during COVID-19 |
|---|---|---|
| Metformin | No dose modification required for OD and BD dose. For TID dosing, one dose after suhoor and remaining two doses together after Iftar. | Stop Metformin.in COVID-19 positive with severe symptoms, poor oral intake, risk of dehydration and AKI |
| First line glucose lowering therapy | ||
| Low risk of hypoglycemia | ||
| Insulin | Avoid Glibenclamide due to high risk of hypoglycemia | Dose reduction may be needed depending on blood sugar levels |
| Secretagogues | Glimepiride, Gliclazide can be used | |
| OD dose: take at Iftar | ||
| BD dose: Iftar dose remains the same, Suhoor dose should be halved | ||
| Repaglinide: take before meals | ||
| DPP-4 inhibitors and AGI | No dose modification required | No dose modification |
| Low risk of hypoglycaemia | ||
| SGLT-2 inhibitors | No dose modification required usually | COVID -19 with severe symptoms -stop the drug. COVID -19 with no/mild symptoms -Dose modification to be considered. |
| Low risk of hypoglycaemia | ||
| Fix stable dose 4 weeks before Ramadan | ||
| Thiazolidinediones | No dose modification required | No dose modification |
| Low risk of hypoglycaemia | ||
| Hydroxychloroquine (insufficient data) | Low risk of hypoglycemia but dose of concomitant drug needs to be reduced | Hypoglycemia risk (along with few drugs) |
OD: Once daily, BD: Twice daily, TID: Thrice daily, AKI: Acute kidney injury, DPP4: Dipeptidyl peptidase 4, AGI: Alpha Glucosidase inhibitors, SGLT-2: Sodium Glucose co-transporter-2. Adapted from: ADA 2020, IDF 2016, IGDR 2015, IDF-DAR Practical Guidelines, South Asian Consensus Guidelines.
Table 7.
Summary of therapeutic titration for injectable therapies[28,34,44,52]
| Glucose-lowering therapy | Recommendation during Ramadan Fasting | Recommendation during COVID-19 |
|---|---|---|
| GLP-1RA | • No dose modification required | • Dose reduction needed when poor oral intake, GI problems, dehydration, AKI, active COVID -19 |
| • Low risk of hypoglycaemia | ||
| Insulin | • High risk of hypoglycemia | • Dose reduction may be needed, depending on blood sugar levels |
| Basal insulin: Preferred initial formulation. | ||
| OD dose: Reduce dose by 15- 30 % and take at iftar. | • Check blood glucose regularly | |
| BD dose: Normal morning dose at Iftar | • Check ketones in Type 1 | |
| And half the evening dose at Suhoor. | Diabetes regularly | |
| Short, Rapid-acting insulin, Pre-mixed insulin: | • Follow “sick day rules” | |
| OD dose- Take at iftar. | ||
| BD dose- Normal morning dose at Iftar and reduce night dose by 25-50 % and take it at Suhoor. | ||
| TID dose- Omit afternoon dose, adjust Iftar and Suhoor doses according to BG every 3 days | ||
| Insulin Pump: Basal rate reduce dose by 20-40% in the last 3-4 hours of fasting and increase dose by 0-30% after Iftar. Bolus rate is based on carbohydrate counting and insulin sensitivity factor. |
GI: Gastrointestinal, AKI: Acute kidney injury, OD: Once daily, BD: Twice daily, TID: Thrice daily, GLP-1RA : Glucagon-like-peptide-1 receptor agonist, BG: Blood glucose Adapted from: ADA 2020, IDF 2016, IGDR 2015, IDF-DAR Practical Guidelines, South Asian Consensus Guidelines.
Table 8.
| Situation | Treatment Plan |
|---|---|
| Critically ill, hospitalized | Intravenous insulin infusion [preferably] or subcutaneous basal-bolus |
| Non- critically ill, hospitalized | Insulin subcutaneous [preferably basal-bolus regimen] |
| With dehydration or | Should Stop - Diuretics, ACEI, ARB, |
| Acute Kidney Injury | Metformin, SGLT2i. Consider Stopping if required - Sulphonylureas, GLP1RA |
| Out patientse | May need dose/medication adjustment |
| COVID-19 positive | |
| Out patients without | Continue usual medications - no dose adjustment needed |
| COVID-19 | |
| On Statins | Continue medication [Cardiovascular benefit-short and long term] |
| On Anti-Hypertensives | Continue medication [Insufficient evidence to stop the drug] |
| Therapeutic Aims | |
| Random plasma glucose 72-180 mg/dL (in-patients) and 72-144 mg/dL (out-patients) | |
| Premeal CBG 80-130 mg/dL | |
| 2-hour post meal CBG <180 mg/dL | |
| HbA1c: < 7% | |
| CGM/FGM | |
| TIR (70-180 mg/dL): >70% (> 50% in frail and elderly) | |
| Hypoglycemia (<70 mg/dL): <4% (< 1% in frail and elderly) | |
| General suggestions | |
| Adequate hydration and regular blood glucose monitoring to be ensured for all. | |
| Medical Nutrition therapy to be modified according to caloric demands during acute illness. | |
| Diabetic self-foot examination and care, watch for any other complications | |
CGM: Continuous glucose monitoring, FGM: Flash glucose monitoring, TIR: Time in range
COVID-19-specific concerns in diabetes
Few concerns regarding the COVID-19 pandemic include the need for chemoprophylaxis, immunization against vaccine-preventable respiratory infections, the safety of Sodium-glucose co-transporter 2 inhibitors [SGLT-2i], and the need to change ACEI and ARB drugs.
The ICMR suggests chemoprophylaxis with hydroxychloroquine for people having a high-risk contact with COVID-19 positive patients.[56] But most of the other agencies do not recommend the same. The risk of hypoglycemia should be considered in patients with diabetes who are taking hydroxychloroquine prophylaxis. Hence, frequent monitoring and dose adjustment in medications may be required.[53,54] The usual immunization recommended for all diabetes patients should be continued and reinforced. This can prevent a high-risk hospital admission during this pandemic period and may also avoid co-infection and worsened outcomes in the case of a COVID-19 infection.
SGLT-2 inhibitors have the potential to cause dehydration, hypotension, hyponatremia, euglycemic ketoacidosis, and genital infections, particularly during fasting in summer. This can be avoided by identifying the right subset of patients before starting them on SGLT-2i, educating them regarding signs and symptoms of possible complications, and advising on adequate hydration and nutrition along with personal hygiene. Dose adjustment may be required in the background of COVID-19 and renal impairment.[57,58]
Family Physicians are frontline HCPs during this pandemic catering to a wide range of problems [Table 9].[59,60] They need to reinforce the patient regarding sick day guidelines (especially for T1DM) which may help to avoid an episode of DKA, severe hyperglycemia, or hypoglycemia. During this pandemic with distressed social systems, they should consider dispensing medications for extended periods and coordinate the online drug delivery system. The decision to advise fasting cannot be made based on the age of an individual alone. Recently, in Iran, it was suggested that healthy individuals less than 65 years of age can fast with adequate safety precautions.[61] And special populations like children, pregnant, and lactating women should be advised not to fast.[23]
Table 9.
| • Provide cost-effective, comprehensive, continuous and holistic medical care |
| • Available and accessible to people during crisis |
| • Promote health awareness and impart good sociocultural practices |
| • Focus on primary prevention and control of risk factors for Diabetes |
| • Prevent and manage complications associated with diabetes |
| • Handle diabetes related emergencies |
| • Resolve more and refer less - reduce unnecessary burden at tertiary centres |
| • Involve in training the paramedics |
| • Assist local health authorities in policy formulation |
Teleconsultation
Telephones and mobile phones are probably the preferred modes of communication for the technologically challenged patients. Face to face interaction through digital platforms can provide better satisfaction. In today's scenario, this way of consultation can be very useful and may become the default mode for future consultations.[13] Many studies have shown that telemedicine can improve HbA1c levels and other parameters related to Diabetes.[10] Tele-consultation and telemonitoring by the health care practitioner in confirmation with the laws should come in handy in managing diabetes during pandemics.
Potential areas for research
This includes safety aspect of glucose-lowering therapies during COVID-19 and fasting, the effect of COVID-19 on the quality of life in people during Ramadan, Spectrum of complications during the duo Ramadan and COVID-19 pandemic, Knowledge Attitude, and Practices of Muslims during COVID-19 and Ramadan, Association between hyperglycemia and COVID-19, Use and safety of Hydroxychloroquine in people with Diabetes affected by COVID-19, and Efficacy of digital platforms as a mode to patient consultation.
Conclusion
People with diabetes should go through a systemic and structure-based Ramadan management plan. Fasting is also observed for long hours in various other religions and communities. There is an urgent need to identify the high-risk population during the COVID-19 outbreak to reduce the disease burden. This pandemic during Ramadan is one of the most unprecedented challenges to the health and wellness of the people. The ultimate decision regarding fasting during COVID-19 should be taken by each individual as per recommendation by their treating physician. Teleconsultation is essential in dealing with the vulnerable during this crisis.
Family physicians who deliver personalized care play a vital role in the management of Diabetes. This novel review may be considered as guidance for various HCPs at primary and specialist care levels. We have put forth from experience as well as expertise. Nevertheless, there is a need for large evidence-based guidelines to provide better clarity surrounding the practice of Ramadan, Diabetes, and COVID-19. Translating the guidelines into clinical situations and practicing precision and personalized clinical medicine is the need of the hour.
Key points
Fasting should be recommended after risk stratification.
Dose modification of medications must be addressed.
Regular blood glucose monitoring is essential.
The prescription must contain an appropriately modified and individualized general advice.
Sociocultural history is important in diabetes management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ranjbar G. Ramadan fasting and diabetes Care. J Nutr Fasting Health. 2019;7:68–9. [Google Scholar]
- 2.Khan M, Al-Lehebi R. Respiratory disease and Ramadan. Lancet Respir Med. 2020;8:449–50. doi: 10.1016/S2213-2600(20)30112-0. [DOI] [PubMed] [Google Scholar]
- 3.Dey JK, Dey SK. SARS-CoV-2 pandemic, COVID-19 case fatality rates and deaths per million population in India. J Bioinform Computat Syst Biolo. 2020;2:110. [Google Scholar]
- 4.World Health Organization [Internet] Safe Ramadan practices in the context of the COVID-19: Interim guidance, 15 April 2020. World Health Organization; Available from https://appswhoint/iris/handle/10665/331767 . Cited 10 May 2020. [Google Scholar]
- 5.Murugesan B, Karuppannan S, Mengistie AT, Ranganathan M, Gopalakrishnan G. Distribution and trend analysis of COVID-19 in India: Geospatial approach. J Geogr Stud. 2020;4:1–9. [Google Scholar]
- 6.Golbidi S, Daiber A, Korac B, Li H, Essop MF, Laher I. Health benefits of fasting and caloric restriction. Curr Diab Rep. 2017;17:123. doi: 10.1007/s11892-017-0951-7. [DOI] [PubMed] [Google Scholar]
- 7.Noon MJ, Khawaja HA, Ishtiaq O, Khawaja Q, Minhas S, Niazi AK, et al. Fasting with diabetes: A prospective observational study. BMJ Global Health. 2016;1:e000009. doi: 10.1136/bmjgh-2015-000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salti I, Benard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: Results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–11. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 9.Babineaux SM, Toaima D, Boye KS, Zagar A, Tahbaz A, Jabbar A, et al. Multi-country retrospective observational study of the management and outcomes of patients with type 2 diabetes during Ramadan in 2010 (CREED) Diabet Med. 2015;32:819–28. doi: 10.1111/dme.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JY, Wong CP, San San Tan C, Nasir NH, Lee SW. Telemonitoring in fasting individuals with type 2 diabetes mellitus during Ramadan: A prospective, randomised controlled study. Sci Rep. 2017;7:1–9. doi: 10.1038/s41598-017-10564-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myers P, Dardas LA. Ramadan fasting and diabetes management among Muslims in the United States: An exploratory study. J Muslim Minor Aff. 2017;37:233–44. [Google Scholar]
- 12.International Diabetes Federation [Internet] IDF Diabetes Atlas. 9th edition. 2019. Last cited 10 May 2020. Available from: https://wwwdiabetesatlasorg/ [PubMed]
- 13.Stoian AP, Banerjee Y, Rizvi AA, Rizzo M. Diabetes and the COVID-19 pandemic: How insights from recent experience might guide future management. Metab Syndr Relat Disord. 2020;18:173–5. doi: 10.1089/met.2020.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rashid F, Abdelgadir E. A systematic review on efficacy and safety of the current hypoglycemic agents in patients with diabetes during Ramadan fasting. Diabetes Metab Syndr. 2019;13:1413–29. doi: 10.1016/j.dsx.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed MH, Husain NE, Elmadhoun WM, Noor SK, Khalil AA, Almobarak AO. Diabetes and Ramadan: A concise and practical update. J Family Med Prim Care. 2017;6:11. doi: 10.4103/2249-4863.214964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bahammam A, Alrajeh M, Albabtain M, Bahammam S, Sharif M. Circadian pattern of sleep, energy expenditure, and body temperature of young healthy men during the intermittent fasting of Ramadan. Appetite. 2010;54:426–9. doi: 10.1016/j.appet.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for management of diabetes during Ramadan: Update 2010. Diabetes Care. 2010;33:1895–902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bottini P, Boschetti E, Pampanelli S, Ciofetta M, Del Sindaco P, Scionti L, et al. Contribution of autonomic neuropathy to reduced plasma adrenaline responses to hypoglycemia in IDDM: Evidence for a nonselective defect. Diabetes. 1997;46:814–23. doi: 10.2337/diab.46.5.814. [DOI] [PubMed] [Google Scholar]
- 19.Pakkir Maideen NM, Jumale A, Alatrash JI, Abdul Sukkur AA. Health benefits of islamic intermittent fasting. J Nutr Fasting Health. 2017;5:162–71. [Google Scholar]
- 20.Ahmed WN, Kannampilly JJ. Mysterious hyperglycemia—Are we prescribers or healers? Int J Diabetes. 2019;1:39–40. [Google Scholar]
- 21.Hassanein M, Al-Arouj M, Hamdy O, Bebakar WM, Jabbar A, Al-Madani A, et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract. 2017;126:303–16. doi: 10.1016/j.diabres.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Hanif S, Ali SN, Hassanein M, Khunti K, Hanif W. Managing people with diabetes fasting for ramadan during the COVID-19 pandemic: A South Asian health foundation update. Diabetic Med. 2020;37:1094–102. doi: 10.1111/dme.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadikot S, Jothydev K, Zargar AH, Ahmad J, Arvind SR, Saboo B. Clinical practice points for diabetes management during Ramadan fast. Diabetes Metab Syndr. 2017;11:S811–9. doi: 10.1016/j.dsx.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Rashid F, Abdelgadir E, Bashier A. A systematic review on the safety of Ramadan fasting in high-risk patients with Diabetes. Diabetes Res Clin Pract. 2020;164:108161. doi: 10.1016/j.diabres.2020.108161. [DOI] [PubMed] [Google Scholar]
- 25.Ahmedani MY, Haque MS, Basit A, Fawwad A, Alvi SF. Ramadan prospective diabetes study: The role of drug dosage and timing alteration, active glucose monitoring and patient education. Diabet Med. 2012;29:709–15. doi: 10.1111/j.1464-5491.2011.03563.x. [DOI] [PubMed] [Google Scholar]
- 26.Mohsin F, Azad K, Zabeen B, Tayyeb S, Baki A, Nahar N. Should type 1 diabetics fast in Ramadan. J Pak Med Assoc. 2015;65:S26–9. [PubMed] [Google Scholar]
- 27.Zakaria A, Sabry I, El Shehaby A. Ramadan-like fasting reduces carbonyl stress and improves glycemic control in insulin treated type 2 diabetes mellitus patients. Life Sci J. 2013;2:10:384–90. [Google Scholar]
- 28.Arun CS, John M, Praveen V P, Gangadhar P, George J, Jayaprakash P, et al. Physician guidance – Management of Diabetes during COVID – 19 pandemic May 2020. doi: 1013140/RG222295649289. [Google Scholar]
- 29.Shaikh A. Physical Activity in Ramadan Ramadan &. Diabetes Care. 2018. pp. 82–6. https://doiorg/105005/jp/books/13049_10 .
- 30.Chen Y, Gong X, Wang L, Guo J. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: A systematic review and meta-analysis. medRxiv. 2020 published online March 30. doi: 101101/2020032520043133. [Google Scholar]
- 31.Hoffmann M, Kleine-Weber H, Schroeder S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–80e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21–e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pal R, Bhansali A. COVID-19, diabetes mellitus and ACE2: The conundrum. Diabetes Res Clin Pract. 2020;162:108132. doi: 10.1016/j.diabres.2020.108132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8:546–50. doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – A systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14:395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rubino F, Amiel SA, Zimmet P, Alberti G, Bornstein S, Eckel RH, et al. New-onset diabetes in Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMc2018688. doi: 101056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–77e3. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharma P, Kumar A. Metabolic dysfunction associated fatty liver disease increases risk of severe Covid-19. Diabetes Metab Syndr. 2020;14:825–7. doi: 10.1016/j.dsx.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andersen CJ, Murphy KE, Fernandez ML. Impact of obesity and metabolic syndrome on immunity. Adv Nutr. 2016;7:66–75. doi: 10.3945/an.115.010207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol. 2020;127:104354. doi: 10.1016/j.jcv.2020.104354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mazurek JA, Hailpern SM, Goring T, Nordin C. Prevalence of hemoglobin A1c greater than 65% and 70% among hospitalized patients without known diagnosis of diabetes at an urban inner city hospital. J Clin Endocrinol Metab. 2010;95:1344–8. doi: 10.1210/jc.2009-1151. [DOI] [PubMed] [Google Scholar]
- 42.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: An independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2020;87:978–82. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- 43.Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study? Diabetologia. 2020:1–16. doi: 10.1007/s00125-020-05180-x. doi: 10.1007/s00125-020-05180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hanif W, Patel V, Ali S, Karamat A, Saeed M, Hassanein M, et al. The South Asian Health Foundation (UK) guidelines for managing diabetes during Ramadan. Diabetes Res Clin Pract. 2020;164:108145. doi: 10.1016/j.diabres.2020.108145. [DOI] [PubMed] [Google Scholar]
- 45.Ciaglia E, Vecchione C, Puca AA. COVID-19 infection and circulating ACE2 levels: Protective role in women and children. Front Pediatr. 2020;8:206. doi: 10.3389/fped.2020.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.International Society for Pediatric and Adolescent Diabetes [Internet] Coronavirus infection (COVID-19)-International Society for Pediatric and Adolescent Diabetes. Available from: https://wwwispadorg/page/Corona virusinfectionCOVID-19-IIISPADSummary . Cited 10 May 2020.
- 47.Ghosal S, Arora B, Dutta K, Ghosh A, Sinha B, Misra A. Increase in the risk of type 2 diabetes during lockdown for the COVID19 pandemic in India: A cohort analysis. Diabetes Metab Syndr. 2020;14:949–52. doi: 10.1016/j.dsx.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahmed WN, Manjunath S, Shobha P. Lifestyle interventions to improve diabetes management. Int J Diabetes. 2019;1:3–6. [Google Scholar]
- 49.World Health Organisation [Internet] Practical considerations and recommendations for religious leaders and faith-based communities in the context of COVID-19. Available from: https://wwwwhoint/publications-detail/practical-considerations-and-recommendations -for-religious-leaders-and-faith- based- communities -in-the-context-of-covid-19 . Cited 10 May 2020.
- 50.Ahmed QA, Memish ZA. The cancellation of mass gatherings (MGs) Decision making in the time of COVID-19. Travel Med Infect Disease. 2020 doi: 10.1016/j.tmaid.2020.101631. doi: 101016/jtmaid 2020101631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American Diabetes Association. Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66–76. doi: 10.2337/dc20-S006. [DOI] [PubMed] [Google Scholar]
- 52.Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020 doi: 10.1016/j.dsx.2020.04.004. doi: 101016/jdsx 202004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pareek A, Chandurkar N, Thomas N, Viswanathan V, Deshpande A, Gupta OP, et al. Efficacy and safety of hydroxychloroquine in the treatment of type 2 diabetes mellitus: A double blind, randomized comparison with pioglitazone. Curr Med Res Opin. 2014;30:1257–66. doi: 10.1185/03007995.2014.909393. [DOI] [PubMed] [Google Scholar]
- 54.Singh AK, Singh A, Shaikh A, Singh R, Misra A. Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: A systematic search and a narrative review with a special reference to India and other developing countries. Diabetes Metab Syndr. 2020;14:241–6. doi: 10.1016/j.dsx.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.European Society of Cardiology [Internet] ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic ESC. Last cited 25 June 2020. Available from: https://wwwescardioorg/Education /COVID-19-and-Cardiology/ESC-COVID-19-Guidance .
- 56.National task force for COVID-19. Advisory on the use of hydroxy-chloroquine as prophylaxis for SARS COV 2 infection. Last cited 7 May 2020. Available from: https://wwwmohfwgovin/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxis forSARSCoV2infectionpdf .
- 57.Pal R, Bhadada SK. Should anti-diabetic medications be reconsidered amid COVID-19 pandemic? Diabetes Res Clin Pract. 2020;163:108146. doi: 10.1016/j.diabres.2020.108146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scott ES, Jenkins A, Fulcher GR. Challenges of diabetes management during the COVID-19 pandemic. Med J Aust. 2020 doi: 10.5694/mja2.50665. doi: 105694/mja250665. [DOI] [PubMed] [Google Scholar]
- 59.Katon W, Von Korff M, Lin E, Simon G. Rethinking practitioner roles in chronic illness: The specialist, primary care physician, and the practice nurse. Gen Hosp Psychiatry. 2001;23:138–44. doi: 10.1016/s0163-8343(01)00136-0. [DOI] [PubMed] [Google Scholar]
- 60.Brown JB, Harris SB, Webster-Bogaert S, Wetmore S, Faulds C, Stewart M. The role of patient, physician and systemic factors in the management of type 2 diabetes mellitus. Fam Pract. 2002;19:344–9. doi: 10.1093/fampra/19.4.344. [DOI] [PubMed] [Google Scholar]
- 61.Tootee A, Larijani B. Ramadan fasting during Covid-19 pandemic. J Diabetes Metab Disord. 2020;19:1–4. doi: 10.1007/s40200-020-00534-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


