Abstract
COVID-19 is one of the deadliest viral infections to have hit the planet. There is urgent need to bridge the gaps in handling this pandemic by methodically synthesising available literature through a unique holistic perspective. A systematic review of articles regarding emergency and primary care during COVID-19 pandemic was carried out. PubMed, Scopus, Science Direct, Web of Science, and Google Scholar were screened for articles and qualitative data across various studies were coded and thematically analyzed. Narrative synthesis was achieved by themes identified from findings of studies. Out of n = 953 articles retrieved, we identified and critically appraised n = 7 articles of which n = 5 were narrative reviews, one was systematic review and one was scoping review from researchers across ten countries. Nine overlapping themes were identified under three broad domains – clinical understanding of the disease, social aspects of the disease, and its contextual implications during pandemic. This narrative synthesis draws up a holistic picture of recent reviews on clinical and social understanding of COVID-19 as a disease and as a pandemic. The overlap among nine themes identified in this review could mean that primary care-level screening, triaging, referral, and emergency care of COVID-19 patients in the backdrop of current clinical understanding of the pandemic are all intertwined. Coping with COVID-19 co-habitation and managing undifferentiated illnesses require a syndromic approach and deft handling at grass root levels. Inclusive health policy empowering inherent holistic specialties like family medicine and emergency medicine could be the prudent way forward during this pandemic.
Keywords: Collaborative, COVID-19, emergency care, pandemic, primary care, holistic
Introduction
COVID-19 is one of the deadliest viral infections to have hit the planet with its origin in China by late December 2019. After escalation to other regions like Europe, Americas, Eastern Mediterranean, South-East Asia, and Africa, the virus resurfaced in Western Pacific region forcing the World Health Organization (WHO) to declare it a pandemic by March 2020.[1] Till date, more than 180 countries have been affected with 11327790 positive cases and 532340 deaths. deaths as per the WHO situation reports.[2] In a recent study among doctors providing COVID-19 care, death rates revealed more than 40% being emergency and family physicians probably because they were frontline warriors during the pandemic.[3]
India reported its first case on 30 January 2020 in Kerala and now has 648315 positive cases and more than 18655 deaths.[4] In low and middle income countries (LMICs) like India, challenges in curtailing the spread of virus and provision of quality healthcare to its vast population during the pandemic with adequate protection to frontline health-care workers will be humongous. Hence, it is extremely important to identify the lags and lacunae in our understanding of the pandemic by reviewing current literature through the eyes of the most vulnerable group of health-care providers.
Rationale
There is urgent need to bridge the gaps in handling this pandemic at community, national, and international levels by methodically reviewing available literature through a unique holistic perspective. Our aim therefore is to synthesize scientific evidence on the current clinical, social, and contextual understanding of the disease and to provide a more comprehensive overview that will support government decision making on strategies.
Objectives
To identify and summarize themes in the current understanding of COVID-19 as a disease and pandemic from an emergency and primary care point of view.
To appraise and synthesize the results of this search and holistically address emergency and primary care practice and policy making during COVID-19 pandemic.
Methods
The steps outlined as per Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) 2009 checklist were followed to conduct this systematic review.
Inclusion and exclusion criteria
Scientific literature about COVID-19 is incomplete due to insufficient data from the early stages of outbreak. Also assuming paucity in qualitative data, a relatively liberal policy was adopted with inclusion of original researches, systematic reviews, meta-analyses, and narrative reviews. Only articles in English language with full-text availability were included. Articles already published and available online ahead of print as on 15 April 2020 were included. Non-scientific commentary, reports, news articles, opinion articles, letters to the editor, and studies reporting cases with incomplete information were excluded.
Search strategy
Articles related to COVID-19 were extensively searched in PubMed, Scopus, Science Direct, Web of Science, and Google Scholar and also retrieved through the bibliography lists of published reviews, where applicable. The search was carried out using established methodological and Medical Subject Headings (MeSH) terms relating to qualitative research, COVID-19, emergency care and primary care. Terms used with OR operators were: emergency care, emergency medicine, primary care, family medicine, general practice, general practitioners along with AND operator for all entry terms of COVID-19 with a filter for articles published during the last 1 year.
Articles were extracted and imported to Endnote X9 3.1 software (Clarivate Analytics) for de-duplication and referencing. Quality check of articles was performed using Critical Appraisal Skills Programme (2018) checklist.[5] A “YES” for three objects including the first two questions in checklist by the reviewers was decided a priori as inclusion cut-off for articles. A consultation between reviewers was held to reach a consensus in case of disparities. A narrative approach to synthesis was adopted in view of our broader research question from a policy making point of view.[6] Coding for concept mapping and thematic analysis were performed with the help of QDA Miner version 5.0.34 software (Provalis Research).
Results
Search built upon our methodology revealed n = 953 titles until 15 April 2020. Additional search through references and other online sources (snowballing technique) revealed n = 31 more titles. After quality check and berry picking for relevance to the objectives of our study by all reviewers, n = 7 articles[7,8,9,10,11,12,13] remained for final synthesis [Figure 1].
Figure 1.
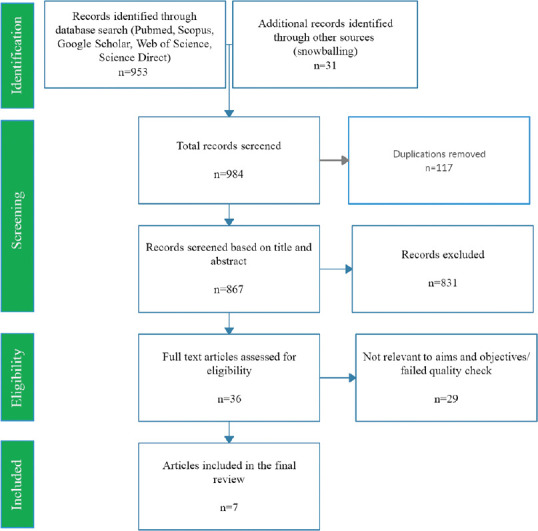
PRISMA flow Diagram. n = number of articles
Study design comparisons
Five out of the included articles were narrative reviews, one was a systematic review, and one was a scoping review. The methodological characteristics of the articles by research teams based in ten countries are summarized in Table 1.
Table 1.
Characteristics of articles reviewed in this study
| No. | Study | Year | Country | Journals/source | Methodology |
|---|---|---|---|---|---|
| 1 | Adhikari, S.P. et al.[7] | 2020 | China/USA | Infect Dis Poverty | Scoping review (Arksey and O’Malley) |
| 2 | Cascella, M. et al.[8] | 2020 | Italy | StatPearls | Review |
| 3 | Guo, Y. R. et al.[9] | 2020 | China/Singapore | Mil Med Res | Review |
| 4 | Lai, C. C. et al.[10] | 2020 | Taiwan | J Microbiol Immunol Infect | Review |
| 5 | Sohrabi, C. et al.[11] | 2020 | UK | Int J Surg | Review |
| 6 | Wu, D. et al.[12] | 2020 | China | Int J Infect Dis. | Review |
| 7 | Wynants et al.[13] | 2020 | Netherlands/Belgium/UK/Germany/Austria | BMJ | Systematic review |
Thematic synthesis
We identified nine themes across the reviewed articles – etiopathogenesis related, symptomatology related, diagnosis and treatment related, preventive aspects, community interventions, primary care point of view, emergency care point of view, and collaborative health policy point of view. These themes were further grouped under three broad domains as detailed below.
Clinical understanding of the disease
We identified n = 7 articles that described COVID-19 from a clinician's perspective. The articles discussed them under epidemiological characteristics (n = 6), etiopathogenesis (n = 6), symptomatology/clinical features (n = 6), and diagnostic or treatment aspects (n = 7).
Etiopathogenesis related aspects
Three reviews[7,8,12] mention the origin of COVID-19 virus to be from bats as suggested by Zhou., et al.[14] with unknown intermediate mammalian host.[8,12] Few reviews describe possible human-to-human transmission for COVID-19, with family members, health-care professionals and close contacts at risk.[7,8,11,12] The possibility of transmission from asymptomatic carriers have been mentioned across five reviews.[8,9,10,11,12] Reviews describe three main transmission routes for COVID-19 as: 1) droplet transmission, 2) contact transmission, and 3) aerosol transmission, with two articles[8,12] mentioning possible aerosol transmission in closed spaces. One review[7] quotes Zhang et al.[15] indicating digestive system as a potential transmission route. Another review[12] infers a possible feco-oral transmission citing Holshue et al.[16] and quotes Phelan et al.[17] in suggesting sustained human-to-human transmission citing evidence of transmission along a chain of four generations.
Symptomatology related
All reviews describe mild to severe COVID-19 symptoms with quoted frequencies consistent with the earliest available Chinese data reported by Huang et al.[18] Wang et al.,[19] and Chen et al.[20] All reviews commonly describe major symptoms as fever, cough, myalgia, or fatigue and dyspnea.[7,8,9,10,11,12,13] Five reviews[8,9,10,11,12] describe clinical manifestations of COVID-19 as variable, which includes asymptomatic carrier, pauci-symptomatic patients and pneumonia of varying degrees of severity. One review[8] described particular characteristics of the fever quoting Chinese CDC[21] for the reported classification of illness as mild, severe and critical.
Diagnostic and treatment related
Four reviews[7,8,10,12] describe virus isolation and viral nucleic acid detection as the diagnosis of COVID-19. One review[12] refers to Yu et al.[22] in stating virus isolation as the “gold standard” for diagnosis while another review[10] highlights the diagnostic dilemma as reported by Zou et al.[23] because of similar viral loads detected in asymptomatic and symptomatic patients. Various prediction models for diagnosis, anticipated admission, and prognosis of patients with COVID-19 infection were described.[7,10,13] But prediction models when used in practice was biased, unreliable and having lower performance than that is reported,[13] whereas another review[7] quotes the clinical case definition guidelines by Li et al.[24] for screening. Several prognostic factors of COVID-19 were compared in one review[10] wherein Yang et al.[25] reveal high mortality rates in patients with a baseline diagnosis of severe pneumonia attributable to a delay in diagnosis.
All reviews convey the lack of specific treatment[7,8,9,10,11,12,13] or vaccine[8,11,12] for COVID-19 at present. Couple of reviews[8,12] describe supportive treatment like oxygen therapy and non-invasive ventilation (NIV) as an effective treatment strategy for worsening inflammatory-induced lung injury. One review[9] mentions Holshue et al.[16] reporting remdesivir to successfully treat COVID-19, chloroquine and rescue therapy with convalescent plasma or immunoglobulin G as treatment options under evaluation.
Social aspects of the disease
Preventive aspects
Five articles[7,8,10,11,12] describe various preventive measures for COVID-19 like ultraviolet rays and heat inactivation,[8] hand hygiene using soap with water[7,11] or 60% alcohol based hand sanitizer,[7] lipid solvents including 75% ether, ethanol, chlorine-containing disinfectant, peroxyacetic acid and chloroform,[8] face masks,[7,11] personal protective equipments (PPE) for hospital infection prevention and control (IPC),[7,8] use of artificial intelligence (AI) for apps,[11] etc., There is mention of prophylactic or pre-emptive use of effective anti-viral agents to reduce the viral load and decrease the risk of virus spread from asymptomatic carriers in one review, with no reliable scientific backing.[10]
Community interventions
According to one review,[7] prevention and control strategies in China were reported at three levels: national level, case-related population level, and general population level. Several public health measures that may prevent or slow down the transmission of COVID-19 like quarantine, social distancing,[7] case isolation,[7,8] contact tracing, surveillance, community lockdown, hand hygiene,[11] environmental disinfection and use of face masks/PPE[7,8,11] have been described. Three reviews[7,8,11] describe interventions at hospital level (IPC measures as per WHO guidelines) to reduce the risk of exposure.
Contextual implications of the disease in a pandemic
The reviews were also thematically analysed from the context of the disease as a pandemic where a transition from clinical medicine to social medicine was evident.
Significance from primary care point of view
Diagnosis of COVID-19 based on clinical manifestations is complicated as initial mild symptoms of the disease are usually nonspecific.[8] The disease itself has various overlapping clinical stages and along with careful monitoring of the asymptomatic disease, there are other undifferentiated conditions that may require medical attention. The patients may belong to any age group, though few reviews[9,10,12] caution children, elderly, and those with co-morbidities to be at increased risk of getting infected. Apart from strategic objectives like ascertaining clinical severity, the spread of COVID-19 may be interrupted by early detection, isolation, prompt treatment, and systematic contact tracing.[11] Diagnostic and prediction models are of limited use in the context of a pandemic and not recommended for use in practice at this point.[13]
Referral should be undertaken whenever there are red flag signs like presence of septic shock, acute respiratory distress syndrome (ARDS) requiring ventilator, AKI needing renal replacement therapy (RRT), etc. One of the reviews describe oxygen for respiratory distress/hypoxemia to be initiated at 5 L/min to reach SpO2 targets of ≥90% in non-pregnant adults and children, and ≥92–95% in pregnant women.[11] In the absence of shock, intravenous fluids should be carefully initiated. Empirical treatments like systemic corticosteroids and unselective antibiotics for the treatment of viral pneumonia or ARDS are not recommended.[8] One of the reviews[8] quote Hui et al.[26] in stating that NIV can be practically used for 1-2 hours in non-severe forms of respiratory failure as these systems with good interface fitting do not create widespread dispersion of exhaled air, and their use can be considered at low risk of airborne transmission.
Significance from emergency care point of view
Patients usually approach the emergency department (ED) when symptoms of the clinical manifestations worsen, but the undifferentiated patient with symptoms may or may not be associated with COVID-19. Fever must be interpreted carefully as even in severe forms of the disease, it can be moderate or even absent.[8] One review emphasizes physicians to follow the clinical performance focusing on saturimetry values, as a decrease in oxygen saturation (<93%) rather than typical PaO2/FiO2 values for ARDS seems to indicate the crucial phase of the disease.[8] National Health Commission of China[27,28] was quoted in a review[7] stating that droplet and aerosol transmission may occur and cause infection in relatively closed environments like ED, indirectly pointing toward health-care workers using precautions like PPE while handling suspicious cases of COVID-19.
Two reviews elaborately describe[8,11] special precautions during rapid sequence intubation (RSI) among patients requiring airway control and lung protective ventilation. When clinical scenario and ventilator data suggest close differentials like pulmonary edema, excluding cardiac failure or other causes like fluid overload with bedside echocardiography helps. Rapid intravenous fluid resuscitation can be performed in shock; however, a conservative fluid management strategy is emphasized for ARDS patients without tissue hypoperfusion. In the septic shock scenario, vasopressors to maintain more than 65 mm Hg mean arterial pressure for persistent hypotension with elevated serum lactate level despite volume resuscitation and prompt RRT in patients with sepsis and AKI are described.[8,11]
Collaborative health policy
As per two reviews,[8,9] world governments and health authorities are collaborating to mitigate a shock wave that is ruthlessly testing the health system. In the USA, physicians should swiftly follow IPC measures, followed by testing for all other sources of respiratory infection with use of epidemiologic factors to assist in decision making while catering to a person under investigation (PUI).[8] Directives provided by health policy agencies often classify the disease according to the severity of the clinical pictures for more effective management. Chinese health authorities have launched psychological interventions in hospitals as medical workers bear enormous pressure and severe challenge, including a high risk of infection, inadequate protection, overwork, frustration, and exhaustion.[9]
Coverage and intertwining of themes
Coverage of themes in individual articles have been summarized in Table 2. It provides an overview of how overlapping the themes are even though we had categorized them under three separate domains.
Table 2.
Coverage of themes in included articles
| Core themes covered | No. of articles | Review articles | ||||||
|---|---|---|---|---|---|---|---|---|
| Adhikari, S.P. et al.[7] | Cascella, M. et al.[8] | Guo, Y. R. et al.[9] | Lai, C. C. et al.[10] | Sohrabi, C. et al.[11] | Wu, D. et al.[12] | Wynants et al.[13] | ||
| Clinical understanding of disease | ||||||||
| Epidemiology related | 6 | ++ | + | ++ | + | + | +++ | - |
| Etiopathogenesis related | 6 | +++ | +++ | +++ | ++ | ++ | +++ | - |
| Symptomatology related | 6 | + | +++ | +++ | +++ | ++ | +++ | - |
| Diagnostic and treatment related | 7 | + | +++ | +++ | ++ | + | +++ | ++ |
| Social aspects of disease | ||||||||
| Preventive aspects | 5 | +++ | ++ | - | + | +++ | + | - |
| Community interventions | 4 | + | ++ | - | + | +++ | - | - |
| Contextual implications of the disease in a pandemic | ||||||||
| Primary care point of view | 6 | - | +++ | + | ++ | +++ | + | ++ |
| Emergency care point of view | 4 | +++ | ++ | - | ++ | - | - | ++ |
| Health policy point of view | 5 | + | ++ | - | + | + | - | + |
- Not mentioned; + Briefly mentioned. ++ Discussed; +++ Discussed extensively
Discussion
Despite unconvincing scientific quality of available articles, we took up a systematic review including review articles in view of the gravity of current crisis. Though most reviews emphasized on clinical aspects, the concepts fitting into key themes of primary care and emergency medicine were gathered and summarized.
Main findings
In this systematic review that explored COVID-19 pandemic from an emergency or primary care point of view, we identified and critically appraised seven articles. A synthesis resulted in categorization of identified themes into three main domains - clinical understanding of the disease, social aspects of the disease, and contextual implications of the disease in a pandemic [Table 2]. Reviews describe droplet transmission, contact transmission, and aerosol transmission for COVID-19 which is a viral disease. All reviews describe the protean clinical symptoms from mild to severe and unanimously convey the lack of specific treatment or vaccines for COVID-19 at present. Diagnostic prediction models when used in practice are biased, unreliable and not recommended. Preventive measures from personal to community levels, IPC interventions at hospitals and public health measures to slow down the transmission have been described across most reviews.
Reflection on review findings
The manifold clinical manifestations with varying degrees of complexities in COVID-19 presentation require deft handling at grass root levels to offset a pandemic. COVID-19 screening is often not a simple binary classification task where expertise is required to decide when to avoid antibiotics or corticosteroids and when to refer for emergency care given the unreliable prediction models currently available. At a community level, a syndromic approach to management of fever and flu by primary care physicians in the backdrop of current pandemic seems to be the best way forward.
Screening and triage at primary care
The symptomatic patients range across age groups with multiple co-morbidities. Moreover, at individual levels, the patient has to be treated holistically with more compassion and psychosocial support, importance of which is grossly neglected in all of the reviews. It is here that the family physician is best suited in providing appropriate cost-effective treatment for possible COVID-19 cases according to the available health resources. The family physician being deeply involved with families is also the best solution to detect and monitor asymptomatic carriers in his community.
Referral
A delay in diagnosis has been described as a concern for increasing mortality rates of COVID-19. This should be read in line with lack of adequate primary care and timely referral for emergency care. Assessment of disease severity including oxygenation, respiratory rate, leukocyte/lymphocyte count, or chest imaging can be carried out at primary care level and patients need to be referred to emergency care only if found to have red flag signs, thus reducing the burden on secondary and tertiary care during a pandemic.
Triage and emergency care
ED being a closed area with multiple patients at the same time, wearing PPE and careful handling of undifferentiated suspicious cases of COVID-19 in a secluded area is utmost important. Patients arriving to ED with severe acute respiratory infection, ARDS, hypoxemia or shock may or may not be associated with COVID-19 where careful interpretation of fever, relying on saturimetry values than PaO2/FiO2 values could help. Special IPC precautions for airway and ventilatory management, use of bedside echocardiography, serum lactate level measurement in early sepsis are to be followed.
Strengths and limitations
The review applied a Methodical and rigorous search strategy to retrieve relevant articles as per research objectives. This research summarizes the holistic themes in approaching COVID-19 management from an emergency and primary care viewpoint, identifies literature gaps, and suggests future research directions on COVID-19. This review only included articles published in English. As the outbreak happened in China, many early literature in Chinese language might have been missed. There is inadequate literature from LMICs like India as the spread of the disease at the time of this review was minimal and most literature is from affluent countries of the world. But some liberty to realign the concepts reviewed to the context of LMIC has been taken in view of the of the pandemic. The word 'emergency' has also been used in various articles in the context of COVID-19 being declared as a public health 'emergency', hence a possible bias at the level of searching for articles was identified and such articles excluded. Though this review doesn't reflect the entire body of COVID-19 worldwide, it will provide some synthesised material for future references.
Implications in practice
Triaging, treatment, and referral models converging precautions and patient preferences during the pandemonium of this pandemic both in primary care and ED is challenging. Many of the developed nations are unable to contain the virus and cater to the vast array of clinical conundrums of innumerable patients that are beyond the purview of narrow specialties.
Conclusion
This narrative synthesis draws up a holistic picture of recent reviews on clinical and social understanding of COVID-19 as a disease and as a pandemic. During this early period, many published studies have explored only clinical understanding of COVID-19 and a lot more needs to be explored about patient-centric care of undifferentiated illnesses in the social context of a pandemic. The overlap among nine themes identified in this review under three domains could mean that primary care-level screening, triaging, referral, and emergency care of patients in the backdrop of current pandemic are all intertwined. Coping with COVID-19 co-habitation during the pandemic needs more inclusive long-term policies and as government agencies rely on scientific statements for translation into public policies, we recommend that the scholarly community comes up with more methodically synthesised reviews on the present public health crisis.
Manifold clinical manifestations, complexities, lack of specific therapies, and unreliable prediction models for COVID-19 require deft handling through a syndromic approach from the grass root levels to offset a pandemic. In this context of holistic specialists as forefront health-care managers of the pandemic, empowering family medicine and emergency medicine collaboration by utilizing their inherent training in these domains which other specialties might not be used to in common practice could be the prudent way forward, especially in LMICs like India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic? Acta Bio-medica: Atenei Parmensis. 2020;91:157–60. doi: 10.23750/abm.v91i1.9397. DOI: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Situation Reports. [Last accessed on 2020 Jun 03]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200602-covid-19-sitrep-168.pdf?sfvrsn=cc95e5d5_2 .
- 3.World Health Organization. India Situation Reports. [Last accessed on 2020 Jul 07]. Available from: https://wwwwhoint/docs/default-source/wrindia/situation-report/india-situation-report-23pdfsfvrsn=7c00a3f_2 .
- 4.Xu AQ, Salimi A. (2020) Physician Deaths from Corona Virus Disease (COVID-19) [Last accessed on 2020 Jul 07]. Available from: SSRN 3566141 https://wwwmedrxivorg/conten t/101101/2020040520054494v1ar ticle-metrics .
- 5.Critical Appraisal Skills Programme (2018) CASP (Qualitative checklist) [Online] [Last accessed on 2020 Apr 25]. Available from: https://casp-uknet/casp-tools-chec klists/
- 6.Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Effect. 2012;4:409–29. [Google Scholar]
- 7.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation and Treatment Coronavirus (COVID-19) StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 9.Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil Med Res. 2020;7:1–10. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.005. pii: S0163-4453 (20) 30116-X doi: 101016/jjinf 202003005 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–6. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu D, Wu T, Liu Q, Yang Z. The SARS-CoV-2 outbreak: What we know. Int J Infect Dis Int J Infect Dis. 2020;94:44–8. doi: 10.1016/j.ijid.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wynants L, Van Calster B, Bonten MMJ, Collins GS, Debray TPA, De Vos M, et al. Prediction models for diagnosis and prognosis of covid-19 infection: Systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou P, Yang X, Wang X, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. doi: 10.1038/s41586-020-2012-7. https://doi.org/10.1038/s41586-020-2012-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. The digestive system is a potential route of 2019-nCov infection: A bioinformatics analysis based on single-cell transcriptomes bioRxiv. 2020. [Last accessed on 2020 May 09]. doi: 101101/20200130927806. Available from https://wwwbiorxivorg/content/101101/20200130927806v1)
- 16.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929–36. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phelan AL, Katz R, Gostin LO. The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. JAMA. 2020 doi: 10.1001/jama.2020.1097. doi: 101001/jama 20201097 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. doi: 101001/jama 20201585 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. doi: 101001/jama 20202648 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Yu F, Du L, Ojcius DM, Pan C, Jiang S. Measures for diagnosing and treating infections by a novel coronavirus responsible for a pneumonia outbreak originating in Wuhan, China. Microbes Infect. 2020;22:74–9. doi: 10.1016/j.micinf.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–9. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of Novel Coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang Y, Lu Q, Liu M, Wang Y, Zhang A, Jalali N. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China medRxiv 2020 Feb 11. [Last accessed on 2020 May 09]. Available from: https://wwwmedrxivorg/content/101101/2020021020021675v2)
- 26.Hui DS, Chow BK, Lo T, Tsang OTY, Ko FW, Ng SS, et al. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019:53. doi: 10.1183/13993003.02339-2018. pii: 1802339 doi: 101183/1399300302339-2018 Print 2019 Apr. [DOI] [PubMed] [Google Scholar]
- 27.National Health Commission of People's Republic of China. Prevent guideline of 2019-nCoV2020. [Last accessed on 2020 Apr 25]. Available from: http://wwwnhcgovcn/xcs/yqfkdt/202001/b c661e49b5bc487dba182f5c49a c445bshtml .
- 28.National Health Commission of People's Republic of China. Pneumonia diagnosis and treatment of 2019-nCoV infection from Chinese NHC and CDC 2020. 2020. [Last accessed on 2020 Apr 15]. Available from: http://wwwnhcgovcn/xcs/zheng cwj/202001/4294563ed35b43209b31739b d0785e67/files/7a9309111267475a 99d4306962c8bf78pdf .


