Abstract
Context:
Meditation is very useful to relieve stress via hypothalamo-pituitory axis. Meditation is considered to be useful to relieve stress and cardio-respiratory health.
Aims:
To compare the effect of meditation on autonomic function including heart rate variability (HRV) over a period of 3 months of meditation.
Settings and Design:
Longitudinal study conducted at Physiology Department, AIIMS Bhopal.
Methods and Materials:
Thirty healthy volunteers doing meditation were evaluated for autonomic function using autonomic function test battery (Ewing's battery) and HRV using Power lab (Ad instrument) and digital electrocardiograph (MARKS).
Statistical Analysis Used:
Statistical analysis was done using statistical software. Wilcoxon signed rank test was used.
Results:
Significant change was seen in Valsalva ratio and lying to standing 30:15 ratio. There was no significant change in other parameters studied with 3 months of meditation.
Conclusions:
Three months of meditation does not have any significant effect on major parameters of autonomic functions.
Keywords: Heart rate variability, meditation, yoga
Introduction
Meditation is recognized as a specific consciousness state in which deep relaxation and increased internalized attention co-exist. A working definition of meditation has been developed by Cardoso et al.[1] where a specific and defined technique is there, it involves muscle and logic relaxation. It is a self-induced state where there is the use of self-focus skill. There are various techniques of meditation, whatever may be the meditation, the basic parameters that are used are breathing, mantra, relaxation, attention and its object, spirituality and belief, and training.[2,3]
Whatever is the meditation practice, it quiets the mind. Meditation is very useful to relieve stress.[2] In a study in the persons doing Zen Meditation, an increase in slow alpha interhemispheric EEG coherence in the frontal region was seen; thus, it relaxes the mind.[4] Meditation practice is also associated with healthy lifestyle. Meditation is considered as an adjunct to guideline-directed cardiovascular risk reduction by those interested in this lifestyle modification.[5]
Government is promoting Yoga all over the world. It has started becoming very popular. Meditation is one of the integral parts of Yoga. Primary care physicians are the first point of contact to the society. Primary care physician may be a general practitioner or he may be a physician sitting up in the primary health center. We had come across some studies where yoga has been used for promoting psychological health.[6] Community people would approach primary care physician to beneficial effect of meditation. This study would definitely help know how does autonomic function changes with meditation and importantly how much duration sufficient for that.
There are various studies done in the literature whereby the beneficial effect of yoga is proved. The positive effect has been observed on cardio-respiratory and autonomic function.[7,8,9,10] These effects are shifting of autonomic balance to parasympathetic side, decrease in sympathetic activity, and sympathovagal balance improvement.[11] A further effect is significant reduction in resting pulse rate, systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure. Some authors had found significant improvement in attention. These effects have been observed in various types of meditators like Raj-yoga, Zen, Art of living meditators, and Muslim prayers.[4,7,8,8,9,10,12] However, all these studies were cross sectional. Significant effect of meditation was also observed on heart rate variability (HRV) parameters like normalized unit of power in low-frequency band (LFnu), normalized unit of power in high-frequency band (HFnu), and LF/HF ratio.[13]
We had come across two longitudinal studies where effect was seen on cardio-respiratory parameters, melatonin secretion, and psychological profile.[14,15] Improvements in these parameters were seen. However, to our best knowledge, we have not found a longitudinal study where effect on all autonomic function parameters is studied. In the present study, attempt has been taken to assess the effect of meditation on autonomic function over the duration of 3 months.
Subjects and Methods
A longitudinal study was conducted among 30 volunteers in the Department of Physiology, AIIMS, Bhopal. Thirty participants were selected from the centers related to meditation nearby territory of the institute. Before enrolling the participants for the study, detailed clinical examination was done and they were selected as per inclusion and exclusion criteria given below. It was followed by autonomic function testing including HRV. Subjects were given detailed information and were included in the study only after due consent.
The study was undertaken after due approval from the Institutional Human Ethics Committee (IHEC) of AIIMS, Bhopal and after the approval from the Research Review Board (RRB) of AIIMS, Bhopal.
Inclusion criteria and exclusion criteria were as follows:
Males: 18–45 years
Females: 18–55 years
Nonsmokers
Normotensive
Nondiabetic
New inductees to the program of training in meditation techniques at the respective centers
They should practice meditation for at least 20 min a day, minimum 5 days a week, following the schedule for the time of the study
Exclusion criteria
Experienced practitioners of any given type of meditation
Those who will not be adhering to the routine of practice
Any disease or disorder which interferes with the recording of the selected parameters
Neurological deficits
Any muscular disorders
Subjects with a history of alcohol intake, smoking, or chewing tobacco or drug abuse.
Autonomic function test
It was done using Ewing's battery of test including cold pressor test. Following tests were done. Standard procedure was followed.[16]
Immediate heart rate and blood pressure response to standing (30:15 R-R ratio)
Blood pressure response to isometric exercise (Hand Grip test)
Cold pressor test
Valsalva ratio
Heart rate variation with respiration
These parameters were assessed using Micro–RF18 digital electrocardiograph (MARKS) and digital BP instrument (Omron automatic blood pressure monitor, model no. HEM-8712).
Heart rate variability
HRV recording and assessment was done on power lab (AD InstrumentsPLtd, Castle Hill Australia). ECG was sampled at 1000 Hz for 5 min with the Power Lab acquisition system. The recording was started once the patient becomes stable in a quiet room with a comfortable temperature. Prior to recording, patients were instructed to abstain from any type of exercise, eating and drinking anything, having caffeine, 2 h prior to scheduled time for test. HRV recording was analyzed with both frequency domain and time domain analysis.
Statistical analysis
Statistical analysis was done using statistical software. Wilcoxon signed rank test was used to compare mean values of various parameters.
Result
The study was done in thirty healthy volunteers (20 males and 10 females) of age 33 years ± 4.54 (mean ± S.D). Resting heart and blood pressure is shown in Figure 1. There was no significant change in these parameters. Autonomic function test parameters and HRV parameters are shown in Tables 1-3. A significant change was seen in Valsalva ratio and 30:15 ratio; however, Valsalva ratio decreased and 30:15 ratio increased. All the volunteers were having autonomic function test within normal limit. There was no significant change in other parameters studied with 3 months of meditation.
Figure 1.
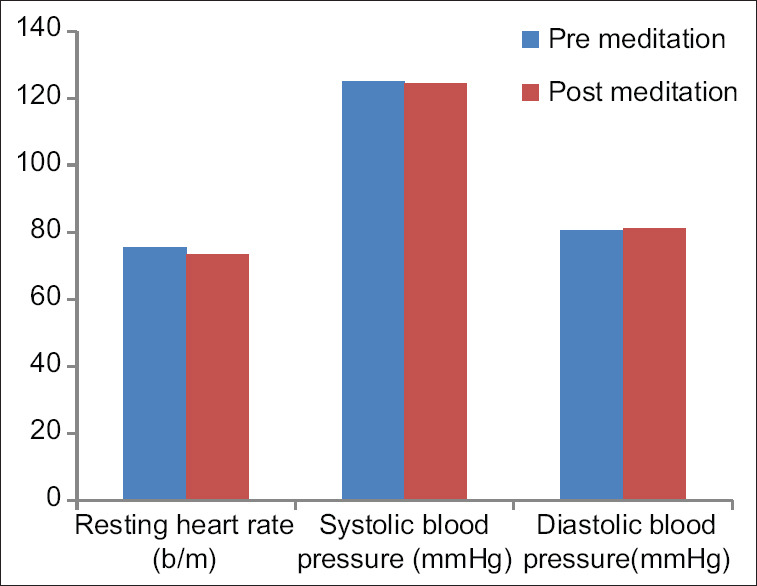
Resting heart rate and blood pressure in subjects with 3 months of meditation
Table 1.
Autonomic function test parameters in subjects with 3 months of meditation
| Parameters | Premeditation (n=30) | Postmeditation (n=30) | P |
|---|---|---|---|
| Delta HR | 14.37±6.542 | 12.97±5.458 | 0.075 |
| E:I ratio | 1.223±0.106 | 1.21±0.093 | 0.068 |
| Valsalva ratio | 1.31±0.243 | 1.44±0.308 | 0.003* |
| 30:15 ratio | 1.19±0.193 | 1.15±0.193 | 0.041* |
| Fall in systolic blood pressure in lying to standing | 7.23±1.28 | 6.81±0.91 | 0.14 |
| Increase DBP in handgrip test | 19.14±2.11 | 18.95±2.89 | 0.77 |
| Increase DBP in cold pressor test | 10.81±2.13 | 11.18±3.01 | 0.51 |
P<0.05 significant. All values are mean±S.D
Table 3.
Heart rate variability-Frequency domain parameters and Poincare analysis parameters in subjects with 3 months of meditation
| Parameters | Premeditation (n=30) | Postmeditation (n=30) | P |
|---|---|---|---|
| Total power | 2264.17±1525.72 | 2635.16±2124.75 | 0.120 |
| VLF Band Power % | 32.74±10.05 | 33.39 ±17.50 | 0.926 |
| LF Band Power (nu) | 45.54±15.26 | 46.99±14.17 | 0.65 |
| HF Band Power (nu) | 53.46±15.26 | 53.01±14.17 | 0.91 |
| LF/HF RATIO | 0.99±0.67 | 1.11±0.95 | 0.56 |
| SD1 | 87.25±61.28 | 96.30±115.47 | 0.43 |
| SD2 | 80.55±48.90 | 108.36±97.76 | 0.17 |
| SD1/SD2 | 1.08±0.33 | 0.89±0.49 | 0.08 |
P<0.05- significant. All values are mean±S.D VLF-very low frequency, LF-low frequency, HF-high frequency. SD1-dispersion of points perpendicular to the line of identity. SD2-dispersion of points along the line of identity
Table 2.
Heart rate variability-Time domain parameters in subjects with 3 months of meditation
| Parameters | Premeditation (n=30) | Postmeditation (n=30) | P |
|---|---|---|---|
| Mean RR interval (ms) | 792.29±114.98 | 817.07±66.33 | 0.165 |
| SDSD | 104.13±114.59 | 62.84±73.15 | 0.171 |
| RMSSD | 107.72±77.58 | 122.58±113.42 | 0.55 |
| pNN50 | 18.10±23.81 | 30.52±23.38 | 0.053 |
P<0.05- significant. All values are mean±S.D. SDSD- standard deviation of differences between adjacent RR interval. RMSSD- The root mean square of the mean of sum of the squares of differences between adjacent RR interval. pNN50- percentage number RR interval differences ≥ 50 ms
Discussion
Meditation is considered to be useful to relieve stress. Various cross-sectional studies had shown the positive effect of meditation on autonomic function. Hence, a longitudinal study was planned to assess the effect of 3-month meditation on autonomic function. Autonomic function was noninvasively assessed using autonomic function test battery (Ewing's battery) and HRV.
This was a longitudinal study where the effect of 3 months' meditation on autonomic function including HRV was seen. A significant change was seen in Valsalva ratio and 30:15 ratio. There was no significant change in other parameters studied with 3 months of meditation.
Valsalva ratio and 30:15 ratio are the indicators of parasympathetic function. However, one parameter showed an increase, while other showed a decrease. A shift in parasympathetic as well as sympathetic activity was seen. However, this shift was not supported by other parameters on HRV.
We had come across a longitudinal study where effect on cardiac parameters like pulse rate, systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure was studied. This may be because meditation decreases sympathetic activity, arterial tone, and peripheral resistance.[14,15] We did not get any significant change in these parameters. Minimal change in parasympathetic action may be responsible for this.
In many cross-sectional studies, a significant change was observed in many parameters of the autonomic function like standing: lying ratio, Valsalva ratio, I: E ratio, and 30:15 ratio, but in our study significant change was observed in Valsalva ratio and 30:15 ratio. Meditation was practiced for more than 5 years in these studies in contrast to 3 months in the present study.[7,17,18] In the present study, we could not get a significant effect on HRV parameters, which is in contradiction with various cross-sectional studies.[19,20] Thus, with 3 months of meditation, we could not get any major alteration in the autonomic function.
Meditation is known to have a positive effect on cardiorespiratory health.[5,21] One of the important effects of meditation is to relieve stress. Due to this, it has been used for many medical conditions. It mainly alters the autonomic function by decreasing sympathetic tone and increasing parasympathetic tone.[11,18] Better balance is seen between sympathetic and parasympathetic component.[7] This balance was maintained between sympathetic and parasympathetic component in the present study. This balance may be responsible for nonsignificant change in resting blood pressure and heart rate.
Duration and correct technique, especially breathing may also be responsible factors. During meditation, the main focus is on breathing.[2,22] Breathing is controlled by both voluntary and involuntary mechanisms. There is a complex interaction between various structures during breathing. The voluntary control of breathing can modulate autonomic nervous system mainly cardiac vagal tone which is evident on HRV and various autonomic function tests.[7,22,23] Thus, proper breathing technique during meditation would play an important role in the alteration of various autonomic functions.
Other reason is less duration. Volunteers in the present study had done meditation for 3 months. We had come across a certain study where effect during meditation on HRV is studied. HRV is significantly increased during the meditation process.[13,24] Thus, meditation has beneficial effect during meditation. However, for any physiological changes to be established, duration plays an important role. It may be because development of phenomenon known as plasticity. Any plasticity requires regular proper practice and certain duration. Three-month duration of meditation was not sufficient for development of autonomic changes. This plasticity can be explained by certain studies where functional connectivity in the various regions was studied. Increased functional connectivity was seen postcentral gyrus related network, posterior cingulate gyrus, and connections between amygdala and prefrontal cortex.[25,26,27] Experienced meditators have weaker functional connectivity for self-referential processing and emotional appraisal but they strengthened connections for moment awareness.[25] Thus, certain connections strengthen, while some connections become weak, and regular and proper practice for long duration would play important role in the development of these changes.
Importance of practice has been explained by Singer and Engert; they explained that during mental relaxation technique, focus may be on different parameters. Depending on your focus, your findings may differ. Thus, it matters what you practice.[28]
Yoga in primary care is considered to be feasible, safe. It has also shown a positive effect on mental health.[12] Primary care physicians are first point of contact with the community. Primary care physician should advice patient to do practice of meditation for long duration. Doing meditation is an art and they must advice their patient to do meditation under supervision.
Limitation of the study
Most important limitation is a sample size. The sample size was less in the present study. This is because more than 50% of subject lost during follow-up. Also, the way of doing meditation also matters. Doing meditation is art; it takes time to develop good technique of meditation. We could not control techniques of meditation.
To conclude, 3 months of meditation does not have any significant effect on major parameters of autonomic functions; however, balance is maintained between sympathetic and parasympathetic activity. We recommend more multicentric studies with large sample size and meditation supervision.
Key Points
Effect of three months of meditation on autonomic function was evaluated in the present study.
Three months of meditation could not produce any major change in autonomic function parameters.
Key message
Meditation is an art; it requires patience and it has to be done under supervision.
Declaration of patient consent
The authors certify that they have obtained all appropriate participant consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cardoso R, de Souza E, Camano L, Leite JR. Meditation in health: An operational definition. Brain Res Brain Res Protoc. 2004;14:58–60. doi: 10.1016/j.brainresprot.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Sharma H. Meditation: Process and effects. Ayu. 2015;36:233–7. doi: 10.4103/0974-8520.182756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savel RH, Munro CL. Quiet the mind: Mindfulness, meditation, and the search for inner peace. Am J Crit Care Off Publ Am Assoc Crit-Care Nurses. 2017;26:433–6. doi: 10.4037/ajcc2017914. [DOI] [PubMed] [Google Scholar]
- 4.Murata T, Takahashi T, Hamada T, Omori M, Kosaka H, Yoshida H, et al. Individual trait anxiety levels characterizing the properties of zen meditation. Neuropsychobiology. 2004;50:189–94. doi: 10.1159/000079113. [DOI] [PubMed] [Google Scholar]
- 5.Levine GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, et al. Meditation and cardiovascular risk reduction: A scientific statement from the american heart association. J Am Heart Assoc. 2017:6. doi: 10.1161/JAHA.117.002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponte SB, Lino C, Tavares B, Amaral B, Bettencourt AL, Nunes T, et al. Yoga in primary health care: A quasi-experimental study to access the effects on quality of life and psychological distress. Complement Ther Clin Pract. 2019;34:1–7. doi: 10.1016/j.ctcp.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Bharshankar JR, Mandape AD, Phatak MS, Bharshankar RN. Autonomic functions in raja-yoga meditators. Indian J Physiol Pharmacol. 2015;59:396–401. [PubMed] [Google Scholar]
- 8.Maini S, Kaur H, Maini N. Effect of Rajyoga meditation on heart rate blood pressure and ECG. J Clin Diag Res. 2011;5:1519–22. [Google Scholar]
- 9.Chung SC, Brooks MM, Rai M, Balk JL, Rai S. Effect of Sahaja yoga meditation on quality of life, anxiety, and blood pressure control. J Altern Complement Med N Y N. 2012;18:589–96. doi: 10.1089/acm.2011.0038. [DOI] [PubMed] [Google Scholar]
- 10.Sukhsohale ND, Phatak MS. Effect of short-term and long-term Brahmakumaris Raja Yoga meditation on physiological variables. Indian J Physiol Pharmacol. 2012;56:388–92. [PubMed] [Google Scholar]
- 11.Solanki A, Saiyad S. Comparative study of effect of mediation on autonomic nervous system in healthy meditators and non meditators. Natl J Integr Res Med. 2020;11:11–5. [Google Scholar]
- 12.Doufesh H, Ibrahim F, Ismail NA, Wan Ahmad WA. Effect of muslim prayer (Salat) on α electroencephalography and its relationship with autonomic nervous system activity. J Altern Complement Med. 2014;20:558–62. doi: 10.1089/acm.2013.0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arya NK, Singh K, Malik A, Mehrotra R. Effect of Heartfulness cleaning and meditation on heart rate variability. Indian Heart J. 2018;70(Suppl 3):S50–5. doi: 10.1016/j.ihj.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, et al. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med N Y N. 2004;10:261–8. doi: 10.1089/107555304323062257. [DOI] [PubMed] [Google Scholar]
- 15.Ankad RB, Herur A, Patil S, Shashikala GV, Chinagudi S. Effect of short-term pranayama and meditation on cardiovascular functions in healthy individuals. Heart Views Off J Gulf Heart Assoc. 2011;12:58–62. doi: 10.4103/1995-705X.86016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zygmunt A, Stanczyk J. Methods of evaluation of autonomic nervous system function. Arch Med Sci AMS. 2010;6:11–8. doi: 10.5114/aoms.2010.13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Telles S, Desiraju T. Autonomic changes in Brahmakumaris Raja yoga meditation. Int J Psychophysiol Off J Int Organ Psychophysiol. 1993;15:147–52. doi: 10.1016/0167-8760(93)90072-w. [DOI] [PubMed] [Google Scholar]
- 18.Kiran, Arora A, Kaur D, Thaman R. Impact of meditation on autonomic nervous system- A research study. Int J Basic Appl Med Sci. 2011;1:144–8. [Google Scholar]
- 19.Bhaskar L, Kharya C, Deepak KK, Kochupillai V. Assessment of cardiac autonomic tone following long sudarshan kriya yoga in art of living practitioners. J Altern Complement Med N Y N. 2017;23:705–12. doi: 10.1089/acm.2016.0391. [DOI] [PubMed] [Google Scholar]
- 20.Chang C-H, Lo P-C. Effects of long-term dharma-chan meditation on cardiorespiratory synchronization and heart rate variability behavior. Rejuvenation Res. 2013;16:115–23. doi: 10.1089/rej.2012.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cramer H, Sibbritt D, Park CL, Adams J, Lauche R. Is the practice of yoga or meditation associated with a healthy lifestyle? Results of a national cross-sectional survey of 28,695 Australian women. J Psychosom Res. 2017;101:104–9. doi: 10.1016/j.jpsychores.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Bushell WC, Olivio EL, Theise ND. Longevity, Regeneration, and Optimal Health: Integrating Eastern and Western Perspectives. John Wiley and Sons; 2009. p. 375. [Google Scholar]
- 23.Telles S, Nagarathna R, Nagendra HR. Autonomic changes during “OM” meditation. Indian J Physiol Pharmacol. 1995;39:418–20. [PubMed] [Google Scholar]
- 24.Nesvold A, Fagerland MW, Davanger S, Ellingsen Ø, Solberg EE, Holen A, et al. Increased heart rate variability during nondirective meditation. Eur J Prev Cardiol. 2012;19:773–80. doi: 10.1177/1741826711414625. [DOI] [PubMed] [Google Scholar]
- 25.Taylor VA, Daneault V, Grant J, Scavone G, Breton E, Roffe-Vidal S, et al. Impact of meditation training on the default mode network during a restful state. Soc Cogn Affect Neurosci. 2013;8:4–14. doi: 10.1093/scan/nsr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kral TRA, Schuyler BS, Mumford JA, Rosenkranz MA, Lutz A, Davidson RJ. Impact of short- and long-term mindfulness meditation training on amygdala reactivity to emotional stimuli. NeuroImage. 2018;181:301–13. doi: 10.1016/j.neuroimage.2018.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiao Q, Zhao X, Bi G, Wu L, Zhang H, Liu R, et al. Alterations of regional homogeneity and functional connectivity following short-term mindfulness meditation in healthy volunteers. Front Hum Neurosci. 2019;13:376. doi: 10.3389/fnhum.2019.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singer T, Engert V. It matters what you practice: Differential training effects on subjective experience, behavior, brain and body in the ReSource Project. Curr Opin Psychol. 2019;28:151–8. doi: 10.1016/j.copsyc.2018.12.005. [DOI] [PubMed] [Google Scholar]


