Abstract
Context:
World'spopulation is ageing and increase in geriatric population demands improved oral health care. Previous epidemiologic studies in general population of India and particularly in Kerala (state with maximum proportion of elderly) provided very little information about oral mucosal lesions in elderly.
Aims:
To find out the prevalence, pattern and distribution of oral mucosal lesions in geriatric patients and to explore their association with different study variables.
Settings and Design:
A descriptive, hospital-based, cross sectional study was conducted for a period of 9 months in the out-patient clinic, Department of Oral Medicine and Radiology, Government Dental College, Kozhikode (tertiary healthcare centre in Kerala, India).
Methods and Materials:
Participants aged 60 and above were selected by consecutive sampling. Data were collected through clinical examination and by using a structured proforma.
Statistical Analysis Used:
Descriptive statistics with tests of significance of associations were done.
Results:
The geriatric population (N=750, 66.89 ± 6.07, M: F=1.4:1), was recruited by screening 43,180, and 447 (67.29 ± 6.15, M: F=2:1) were identified having oral mucosal lesions withprevalence of 59.6% (95% CI=56.05–63.05). Most common lesion group was red and white (73.2%), followed by pigmented (15.5%). Oral mucosal lesions were significantly associated with age over 65, male gender, presence of habit and denture usage (P < 0.05).
Conclusions:
The prevalence of oral mucosal lesions in geriatric people is high. Hence setting up of geriatric dental clinics, with appropriate preventive and palliative intervention strategies is mandatory.
Keywords: Prevalence, oral mucosal lesions, geriatric population, geriatric dentistry
Introduction
Oral health is a reflection of general health, and any disease affecting oral health condition will influence general health and quality of life of an individual. This is particularly important in vulnerable age groups, like pediatric and geriatric population. World is facing a dramatic shift in its population characteristics, especially in the proportion of geriatric people. In total 13% of world's population was aged 60 or more in 2017 and it is increasing at a rate of about 3% per year.[1] In India, 8% of the population was aged 60 years or more and among Indian states, Kerala had the highest percentage of geriatric people (12.6%).[2]
World Health Organization defined aging as “The lifelong process of growing older at cellular, organ or whole- body level throughout the life span”.[3] The regressive changes related to old age make them susceptible to many chronic diseases, physical, and mental disabilities which restrict daily activities and reduction in self care. Age-related changes predispose oral cavity to various lesions, periodontal diseases, infections, caries and salivary gland diseases.
Geriatric healthcare is not a well developed speciality in Indian subcontinent and people often report at primary health centres for all their health problems. Also previous epidemiologic studies showed high prevalence of oral mucosal lesions in geriatric population and relevant studies are fewer in India in general and Kerala in particular. The objectives of this study were to find out the prevalence, pattern and distribution of oral mucosal lesions in geriatric patients and to explore their association with relevant study variables which may be very useful for enlightening primary care physician.
Methods
A descriptive, hospital-based, cross sectional study was conducted for a period of 9 months (March–November 2016) in the out-patient clinic, Department of Oral Medicine and Radiology, Government Dental College, Kozhikode, which is a tertiary health care centre in Kerala, India. Geriatric population was defined as those aged 60 years and above.[4] The participants were recruited for the study by consecutive sampling. All were clinically examined by the principal investigator, for the purpose of identifying oral mucosal lesions. A specially designed, structured proforma was used for obtaining relevant patient information. The study was approved by Institutional Research and Ethics Committee, Dental College, Kozhikode and informed consent was obtained from each participating patient. Patients with terminal illness or requiring emergency management and who were not willing to participate were excluded from the study.
A pilot study was conducted for 30 patients: initial examination by the principal investigator followed by a specialist examination. There was good inter-observer agreement in clinical findings (>0.5).
Patient's details regarding age, gender, socio demographic factors, chief complaint, systemic diseases, deleterious oral habits, and denture use status were obtained. Gender data was grouped as male and female. Systemic disease status, the presence of deleterious habits and denture usage were recorded as dichotomous variables and details regarding each were documented.
All subjects were clinically examined under standard conditions, with proper illumination, using mouth mirrors, retractors, and dental explorers. The examination for oral mucosal lesions was systematic, following WHO guide for examination of oral mucosa.[5] Recording of mucosal lesions were done under the following classes-red and white lesions, pigmented lesions, ulcerative lesions, oral cancer, and benign tumors.[6] The lesions were diagnosed based on standard recommendations and criteria.[5,7,8,9] For formulating a systematic approach in collection and reporting the common oral diseases and conditions, we followed International Classification of Diseases: Application to Dentistry and Stomatology (ICD-DA).[10] Histopathologic examination was done in relevant cases with potential risk for malignancy.
Data entry was done using SPSS version 18 for Windows. Clinically relevant variables were categorized and verified for analysis. The outcome measurements was treated as binary (1=Oral mucosal lesions present, 2=No oral lesion). The presence of individual oral mucosal lesions was also treated as binary outcome variables. Univariate Analysis: The descriptive statistics of relevant socio-demographic variables were carried out. Continuous variable (age) were categorized as 5 year age group interval. Bivariate Analysis: Crosstabs were done for relevant variables from different domains against clinical diagnosis of oral lesions. The variables include age, gender, habits (smoking, chewing, and alcoholism), systemic diseases and denture use status in the study group. Detailed description was given for variables significant (P < 0.05) in Chi-Square tests.
Results
In this study 43,180 patients were screened and 750 (1.74%) patients were identified in the geriatric population, aged above 60. Prevalence of oral mucosal lesions was 59.6% (95% CI=56.05–63.05), with 447 patients having oral lesions. Mean age of geriatric population (N=750) was 66.89±6.07, with age range 60–100 (median=65, mode=60). Mean age of the population with oral mucosal lesions (n=447) was 67.29 ± 6.15, ranging from 60 to 100 years.
Male to female ratio of the geriatric population was 1.4:1 and in patients with oral mucosal lesions it was 2:1 [Figure 1a and b]. More than half of them were having deleterious oral habits (399/750) and most prevalent habit in the study group was smoking. 74% were affected with systemic diseases and commonest systemic disease was hypertension (50.5%). There were 136 denture users in the study population. Prevalence of oral lesions in those with systemic diseases was 58.92%, 71.3% in denture wearers and 69.7% in habitués. Characteristics of population with oral mucosal lesions (n=447), are described in Table 1.
Figure 1.
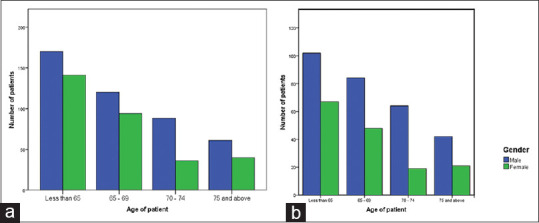
(a) Gender and age group distribution of Geriatric patients (N=750) and (b) Gender and age group distribution in patients with mucosal lesions (n=447)
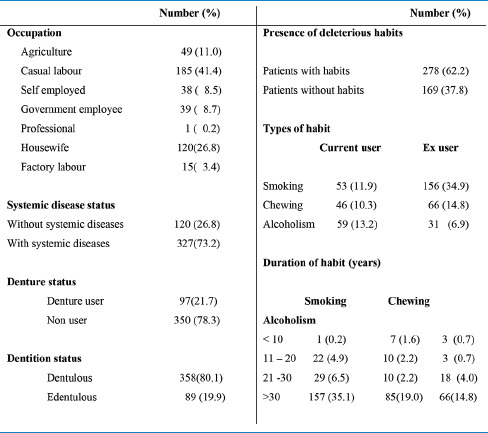
Table 1.
Description of study population with oral mucosal lesions (n=447)
Oral mucosal lesions were classified into five groups–Red and white lesions (73.2%), pigmented lesions (15.5%), ulcerative lesions (6%), oral cancers (3.3%), and benign tumors (2%) [Table 2].
Table 2.
Distribution of various oral mucosal lesion
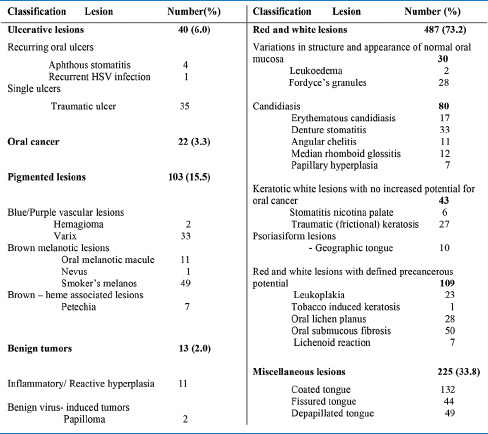
Considering individual lesions, the most prevalent lesion identified in this study population was coated tongue (19.8%), followed by oral submucous fibrosis (7.5%), smoker's melanosis (7.4%), depapillation of tongue (7.4%), fissured tongue (6.6%).
Age group distribution of individual oral mucosal lesions has been shown in Heatmap [Figure 2]. Among the four age group categories,[11] oral mucosal lesions were higher in males less than 65 years (102/169) and least in both genders over 75 years. There were 109 lesions with defined precancerous potential. The most common site of oral lesion was dorsum of tongue (42%) in this study. Majority of patients (38%) presented with single lesion and maximum number of mucosal lesions in any one subject was 4 (0.9%). Prevalence of oral mucosal lesions in patients with deleterious oral habits was 69.7% (95% CI=64.99–73.98). Among 447 patients presented with lesion, 278(62.2%) were having oral deleterious habits–226 (81%) males and 52 (19%) females. The most common habit was smoking, seen in 209 patients. 72% of smokers, 74% of chewers and 78% of alcoholics were having oral mucosal lesions in this study group. There was a definite predilection for malignant and potentially malignant lesions in patients with habits. All the patients with oral submucous fibrosis, 78% of patients with leukoplakia and 95% of oral cancer patients were having habit history.
Figure 2.
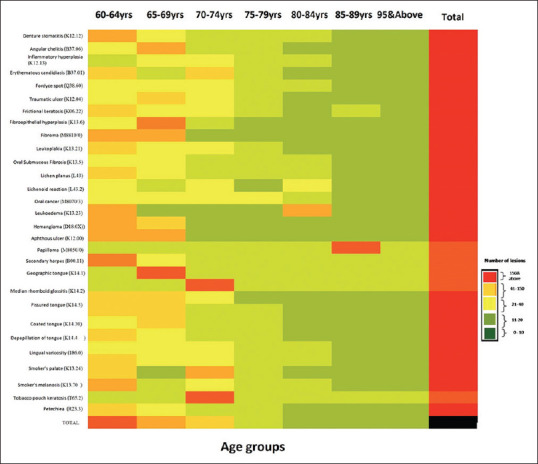
Heat map–Age group distribution of individual oral mucosal lesion (with ICD-DA coding) (n=665)
Prevalence of oral mucosal lesions in patients with systemic diseases was 58.92% (95% CI=54.78–62.94). 324/439 males and 231/311 females were having any one systemic disease. The most common disease was hypertension (35.6%), followed by diabetes mellitus (27.5%), cardiac disease (17%), and cancer (7.8%). Among the patients with mucosal lesions 69% were under chronic medication for various systemic diseases and majority were under treatment for 1–5 years (39%).
Prevalence of oral mucosal lesions in patients using dentures was 71.3% (95% CI=63.22–78.26). In total 21.7% of patients presented with mucosal lesions were using dentures and commonest lesion among them was denture stomatitis (33/136).
On Chi-square analysis, presence of oral mucosal lesions was having statistically significant association with variables like male gender, above 65 years of age, presence of deleterious oral habits and denture use [Table 3].
Table 3.
Association of oral mucosal lesions with relevant study variables
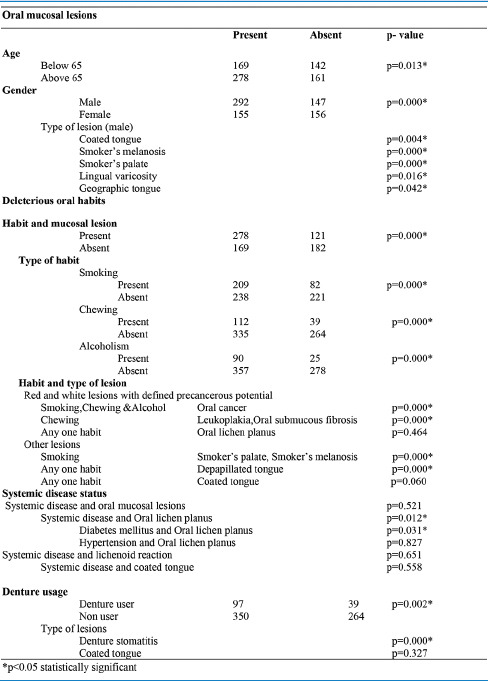
Patients without oral mucosal lesions were 303 in number, 147 males and 156 females. 161/303 was above 65 years. Patients with systemic diseases were high in this group (227/303), compared to population with lesion (327/447). Habits were more in patients with oral lesions than (3/5th) without lesion (2/5th). Denture users were less in study group without lesion (39/303) than group with lesions (97/447).
Discussion
Current demographic analysis shows that elderly group is increasing worldwide, which is also reflected in the Indian population trend. World Health Organization (WHO) points out two key factors which are causing population aging-high life expectancy and reduced fertility rates. Other contributing factors include better economic standards, advances in health care facilities and change in leading cause of death from infectious and parasitic diseases to non-communicable and chronic ones.[12]
In India oral health education is literally nil, and population seek healthcare mainly at primary level. Most physicians are not aware of oral disease-burden, which often lead to underestimation and mismanagement of disease. Knowing the prevalence and distribution of oral mucosal pathologies will be useful in this regard.
Oral lesions are predominant in older age group,[13] but pattern of distribution was different in different population. Literature analysis showed a wide variation in the prevalence of oral mucosal lesions in geriatric patients, ranging from 2.47%[14] to 98%.[15] This difference is due to difference in country of residence, nature of the study population, clinical definition of the lesion, types of lesions included in the study etc. There is no universally accepted classification system for oral mucosal diseases, which also leads to discrepancy in study results.
A high prevalence of mucosal lesions was observed in the present study (59.6%), a result comparable with that observed by Mujica et al.[16] But literature was reporting high prevalence[13,17,18] and low prevalence[19,20] in various other studies. High prevalence of coated tongue in this study could be due to low oral hygiene maintenance in geriatric people or as side effects of medications.[21]
Of the five age groups, 60–65 age category was having more lesions. Males were having significantly more number of mucosal lesions compared to females. Similar result with high prevalence in males (P = 0.028)[19] and contradictory study results[18] were noticed in the literature. Coated tongue, smoker's melanosis, smoker's palate, lingual varicosity, and geographic tongue had statistically significant association with male gender. No lesions were found to be associated with female gender.
Most prevalent systemic disease was hypertension (35.6%), followed by diabetes and cardiac diseases. Similar[17] and different[19] patterns were previously reported. Hypertension was commonly affecting females (P < 0.001), whereas diabetes was seen equally in both genders. Statistically significant association was observed between presence of oral lichen planus and diabetes mellitus (P value=0.031). But such an association was not evident between lichen planus and hypertension. Systemic disease status and oral mucosal lesions were found to be significantly associated, in Turkish study.[20]
Among habitués, 3/4th was having oral mucosal lesions, with significant association between male gender and mucosal lesions with habits. Similar observation was noticed in several other studies.[22,23] An Indian study showed statistically significant association between leukoplakia and male gender.[24] The most prevalent premalignant lesion was oral submucous fibrosis, an observation similar to that of an Indian study.[13,25] This is due to increased quid chewing habit in Indian subcontinent.
There were 22 cases of oral cancer in this study, most common site of occurrence was buccal mucosa and most of the cases were proven histologically as moderately differentiated squamous cell carcinomas. An Indian study showed similar result with 2% oral malignancy, all of them were histologically proven to be squamous cell carcinomas.[13]
Most of the denture users were having oral mucosal lesions. Denture stomatitis was the commonest denture related lesion and the use of denture and presence of lesion has got a significant association, which is similar to various other studies.[13,17,19,26]
Strengths and limitations of the study
The present study with a large sample size will be an approximate measure of the true disease burden, pattern and distribution of various oral mucosal lesions in geriatric population of Kerala, where data in this domain are few. This can be replicated in different study setting. Prediction models can also be attempted using logistic regression analysis using the study sample. Treatment needs of geriatric patients can be identified from this study for further policy making in management and prevention of oral mucosal lesions.
This is a hospital-based study done in a tertiary health care setting in Kerala. Hence, population attended may not represent the disease burden in the community. In this study, diagnosis of the lesions was done based on clinical criteria, by trained oral medicine specialist. Biopsy was done for indicated cases only. Follow-up of patients was not done in this study, being a cross sectional design.
Implications of the study
The current demographic pattern shows an increase of geriatric population compared to other age groups, and this trend will continue in future. This demands special focus on geriatric general and oral health care, which warrant further research studies in this area.
Very few facilities exist for managing chronic mucosal lesions of geriatric population in the current health system. Initiating Hospital-based Registry for Chronic Oral Mucosal Lesion will enable us to have a realistic hospital-based estimation of these lesions in the population and for the easy follow-up of the patients, who needs long duration of treatment. This study will help to formulate preventive public health strategies and palliative care needs for elderly Indian population.
Conclusion
Present study gives an accurate estimate regarding prevalence, pattern and distribution of various oral mucosal lesions in geriatric population. Prevalence of oral mucosal lesions and disease are high in geriatric population and the risk increases with advancing age, presence of habits and use of dentures. Potentially malignant lesions accounted for 17% of total lesions which is significantly related to habits. These results highlight the importance of early diagnosis of oral lesions by screening examination and timely interventions. It is high time for implementing programmes for the improvement of general and oral health of this vulnerable group.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables 2017 Working Paper No ESA/P/WP/248 [Google Scholar]
- 2.Census of India Website: Office of the Registrar General and Census Commissioner, India [Internet] [Google Scholar]
- 3.WHO Centre for Health Development (Kobe, Japan) A glossary of terms for community health care and services for older persons. Kobe, Japan: WHO Centre for Health Development; 2004. [Google Scholar]
- 4.Das PK. Crime against elderly: A critical analysis. Help Age India-Res Dev J. 2009;15:21–33. [Google Scholar]
- 5.Kramer IR, Pindborg JJ, Bezroukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol. 1980;8:1–26. doi: 10.1111/j.1600-0528.1980.tb01249.x. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg M, Glick M, Ship AJ. Burket's Oral Medicine. 11th ed. USA: BC Decker INC; 2008. [Google Scholar]
- 7.Kramer IR, Lucas RB, Pindborg JJ, Sobin LH. Definition of leukoplakia and related lesions: An aid to studies on oral precancer. Oral Surg Oral Med Oral Pathol. 1978;46:518–39. [PubMed] [Google Scholar]
- 8.Axéll T, Pindborg JJ, Smith CJ, Waal I van der. Oral white lesions with special reference to precancerous and tobacco-related lesions: conclusions of an international symposium held in Uppsala, Sweden, May 18–21 1994. J Oral Pathol Med. 1996;25:49–54. doi: 10.1111/j.1600-0714.1996.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 9.Warnakulasuriya S, Johnson NW, Van Der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa: Potentially malignant disorders. J Oral Pathol Med. 2007;36:575–80. doi: 10.1111/j.1600-0714.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Application of the International Classification of Diseases to Dentistry and Stomatology: ICD-DA. 3rd ed. Geneva: World Health Organization; 1995. [Google Scholar]
- 11.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age standardization of rates: A new WHO standard. Geneva: World Health Organization; 2001. p. 9. [Google Scholar]
- 12.World Health Organization. World Report on Ageing and Health. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 13.Patil S, Doni B, Maheshwari S. Prevalence and distribution of oral mucosal lesions in a geriatric Indian population. Can Geriatr J. 2015;18:11–4. doi: 10.5770/cgj.18.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peter JC, T S R, Mohiyuddin SMA, Kuppuswamy SK. Oral mucosal lesions in geriatric population- South Indian hospital based study. IP Indian J ClinExpDermatol. 2018;4:10–5. [Google Scholar]
- 15.Mozafari PM, Dalirsani Z, Delavarian Z, Amirchaghmaghi M, Shakeri MT, Esfandyari A, et al. Prevalence of oral mucosal lesions in institutionalized elderly people in Mashhad, Northeast Iran. Gerodontology. 2012;29:e930–4. doi: 10.1111/j.1741-2358.2011.00588.x. [DOI] [PubMed] [Google Scholar]
- 16.Mujica V, Rivera H, Carrero M. Prevalence of oral soft tissue lesions in an elderly venezuelan population. Med Oral Patol Oral CirugiaBucal. 2008;13:270–4. [PubMed] [Google Scholar]
- 17.MohanadJameel N. Oral diseases and disorders among sample of elderly patients in Basrah province. Misan J Academic Stud. 2013;12:21–8. [Google Scholar]
- 18.Jainkittivong A, Aneksuk V, Langlais RP. Oral mucosal conditions in elderly dental patients. Oral Dis. 2002;8:218–23. doi: 10.1034/j.1601-0825.2002.01789.x. [DOI] [PubMed] [Google Scholar]
- 19.Dundar N, IlhanKal B. Oral mucosal conditions and risk factors among elderly in a Turkish school of dentistry. Gerontology. 2007;53:165–72. doi: 10.1159/000098415. [DOI] [PubMed] [Google Scholar]
- 20.Bozdemir E, Yilmaz HH, Orhan H. Oral mucosal lesions and risk factors in elderly dental patients. JDent ResDent ClinDent Prospects. 2019;13:24–30. doi: 10.15171/joddd.2019.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurniawan A, Wimardhani YS, Rahmayanti F. Oral health and salivary profiles of geriatric outpatients in CiptoMangunkusumo general hospital. J Dent Indones. 2010;17:53–7. [Google Scholar]
- 22.de Lima Saintrain MV, Holanda TG, Bezerra TM, de Almeida PC. Prevalence of soft tissue oral lesion in elderly and its relations with deleterious habits. Gerodontology. 2012;29:130–4. doi: 10.1111/j.1741-2358.2011.00618.x. [DOI] [PubMed] [Google Scholar]
- 23.Demko CA, Sawyer D, Slivka M, Smith D, Wotman S. Prevalence of oral lesions in the dental ofice. Gen Dent. 2009;57:504–9. [PubMed] [Google Scholar]
- 24.Kumar S, Narayanan V, Ananda S, Kavitha A, Krupashankar R. Prevalence and risk indicators of oral mucosal lesions in adult population visiting primary health centers and community health centers in Kodagu district. J Family Med Prim Care. 2019;8:2337–42. doi: 10.4103/jfmpc.jfmpc_344_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rohini S, Sherlin HJ, Jayaraj G. Prevalence of oral mucosal lesions among elderly population in Chennai: A survey. J Oral Med Oral Surg. 2020;26:10–15. [Google Scholar]
- 26.Cueto A, Martínez R, Niklander S, Deichler J, Barraza A, Esguep A. Prevalence of oral mucosal lesions in an elderly population in the city of Valparaiso, Chile. Gerodontology. 2013;30:201–6. doi: 10.1111/j.1741-2358.2012.00663.x. [DOI] [PubMed] [Google Scholar]


