Abstract
Objective:
The objective of this study was to assess the level of awareness and knowledge of first aid for burns among healthcare workers in Saudi Arabia.
Methods:
We conducted a cross-sectional study between September 2 and December 5, 2019, via a self-administered online questionnaire among healthcare workers at a university hospital. The questionnaire comprised 24 questions divided into two sections pertaining to demographics and first aid for burns. This study was approved by the Research Ethics Committee.
Results:
We included 1,438 respondents in this study. Females comprised 68.2% (982) of the respondents. A total of 513 respondents (35.7%) were medical students. The mean burn knowledge score of all respondents was 8.07 ± 2.03 out of 13. Interestingly, 940 individuals (65.4%) used traditional medications on the burn area. Knowledge regarding antibiotic use in burn injuries was poor—1,199 (82.3%) study participants agreed that antibiotics are beneficial in the case of burns, which is a wrong act. The mean knowledge score was significantly different across groups of different ages, sexes, nationalities, marital statuses, and job positions (P < 0.001).
Conclusion:
The level of awareness of first aid for burn patients among healthcare workers was insufficient, and the unnecessary use of traditional medicines and antibiotics in burn patients being high. Moreover, this study confirmed the need for an effective educational program among healthcare workers.
Keywords: Assessment: traditional remedies, awareness, burn first aid, healthcare workers, knowledge
Introduction
Burn injury is a major health issue worldwide with significant adverse effects in the community. It is defined as an injury to the skin or any organic tissues mainly caused by fire, electricity, radioactivity, radiation, or chemicals. According to the latest World Health Organization data (2018), approximately 265,000 deaths are reported annually from fire alone, with more deaths from electrical burns, scalds, and other forms of burns. Nonfatal burns are the most common cause of morbidity, including disfigurement, prolonged hospitalization, and disability, and often cause rejection and stigma.[1] Approximately 1.25 million and 250,000 individuals are affected by burns each year in the United States[2] and the United Kingdom, respectively.[3] On the contrary, in Australia, flame burns and scalds accounted for on average 9 deaths and almost 800 hospitalizations annually and ranked 8th and 7th as injuries causing deaths and hospitalization, respectively, in the United States.[4] After a minor burn injury, immediate first aid plays an important role in determining the outcome and level of subsequent morbidity, as well as in limiting tissue damage, including the need for surgery.[5] Applying water (10–15°C) for 20–30 min as first aid for burns is considered the most appropriate step.[6,7,8,9,10,11] According to a study conducted in Saudi Arabia, most burn injuries occur in the pediatric age group and at home. Scald injuries are the most common type of burn injuries, whereas injuries caused by flames rank second.[8,12] Therefore, primary prevention is the best method to reduce the burden of this health issue in the community, as providing first aid for burns remains an important part of the management of burns, especially as it reduces complications.[13] Burn injuries are specific category of trauma; as its management in the emergency area has some meticulous parts that must be addressed by the first healthcare providers respondents. The evaluation of awareness of healthcare workers including primary care physicians tremendously important in starting strict protocols for burn disasters. Furthermore, management of burn injuries has the most significant effect on morbidity and mortality is in the first hour since its occurrence,[14] thus, being aware of the appropriate management for such case plays a crucial role in patient's life. Therefore, of prime consequence that these healthcare providers must receive the best training and education for an effective and safe management of burn cases. Additionally, healthcare providers should be knowledgeable, as well as have the appropriate skills in managing burn emergencies. One of the first fundamentals should be taught to all the healthcare providers are the life and limb saving procedures. For example, in burns, the cornerstone procedure that can be a life and limb saver is known as escharotomy. It is considered a simple procedure, can be done without the need of anesthesia and with simple instruments, thus it can be done safely at any healthcare area. The training of healthcare workers includes handling burn injuries in a hospital setting, where necessary equipment and drugs are available. However, the awareness and knowledge required for handling an emergency such as burns without a hospital near the site of the emergency or accident may not be adequate. According to a study conducted in Saudi Arabia among medical students, the students had reasonable knowledge when it came to burn prevention and its first aid measures and also showed positive attitudes toward training.[15] To the best of our knowledge, studies assessing the awareness and knowledge of burn first aid among healthcare workers have not been conducted in Saudi Arabia yet, although several studies assessing the level of first aid knowledge regarding burns have been conducted worldwide among individuals other than healthcare workers.[5,6,7,8,9,10,11,12,13,14,15] Therefore, we aimed to identify and assess the level of awareness and knowledge of first aid of burns and the association between the overall knowledge and sociodemographic variables among healthcare worker at a university hospital.
Methods
Study design and data collection
This observational cross-sectional study was conducted via an online questionnaire from September 2 to December 5, 2019 at a university hospital. This self-administrated survey was hosted freely on the Google survey web page, and the link was sent randomly to all healthcare professionals at the hospital including medical students, medical interns, residents, specialists, consultants, and nurses via WhatsApp and other social media platforms. All participants were informed about the requirements of the study, and those who agreed to participate were enrolled. Individuals who refused to participate or failed to complete the questionnaires were excluded.
Questionnaire variables
The questionnaire was formulated on the basis of our study's objectives and available questionnaires with similar objectives.[8,13] The questionnaire comprised 24 questions divided into two sections: demographics and questions related to the burn injury and its first aid measures. The first section included age, sex, nationality, job position, specialty interest, marital status, and number of children if the respondent had any. The second section aimed to assess healthcare workers' knowledge about first aid for burns and the use any kind of traditional remedies, for example, coffee, honey, Aloe Vera, toothpaste, or oil. The overall score for awareness ranged from 1 to 13; a higher score indicated more awareness about first aid of burns.
Statistical analysis
Descriptive statistics were used to present the respondents' baseline characteristics and correct answers to questions related to knowledge on burns. The data were checked for normality using the Shapiro–Wilk test and the Kolmogorov–Smirnov test, which revealed a non-normal distribution. The mean burn knowledge score was calculated by counting the number of correct responses to each question per respondent. The associations between the mean burn knowledge score and age, marital status, and job position were observed using the Kruskal–Wallis H test. The associations between the mean burn knowledge score and sex, nationality, burn training course participation, and the experience of a burn injury to oneself or a family member were assessed using the Mann–Whitney U test. The analysis reported 95% confidence intervals using Statistical Package for Social Science (SPSS), version 23.0 (IBM, Armonk, NY, USA).
Ethical considerations
Ethical policy and institutional review board statement Ethical approval for this study was Obtained on 11/4/2019 from research ethics committee of King Abdulaziz University, Jeddah, Saudi Arabia. (Reference NO 289-19).
Results
A total of 1,438 respondents were included in this study with an overall 81% response rate, and approximately half of them, 720 (50.1%), were aged between 22 and 29 years. More than two-thirds, 982 (68.2%), of the respondents were female, and the majority, 1240 (86.2%), were Saudi Arabian. A significant number of the respondents, 974 (67.7%), experienced burn trauma to self or family, but relatively fewer respondents, 249 (17.3%), received a burn training course [Table 1].
Table 1.
Baseline characteristics of the respondents (n=1438)
| Characteristics | n | Percentage |
|---|---|---|
| Age in years | ||
| 19-21 | 372 | 25.9 |
| 22-29 | 720 | 50.1 |
| 30-39 | 210 | 14.6 |
| 40-50 | 102 | 7.1 |
| >50 | 34 | 2.4 |
| Gender | ||
| Male | 456 | 31.7 |
| Female | 982 | 68.3 |
| Nationality | ||
| Saudi | 1240 | 86.2 |
| Non-Saudi | 198 | 13.8 |
| Marital Status | ||
| Single | 1010 | 70.2 |
| Married | 401 | 27.9 |
| Widowed | 3 | 0.2 |
| Divorced | 24 | 1.7 |
| Number of children | ||
| N/A | 1118 | 77.7 |
| 1 | 91 | 6.3 |
| 2-3 | 159 | 11.1 |
| >3 | 70 | 4.9 |
| Job position | ||
| Medical student | 513 | 35.7 |
| Medical intern | 204 | 14.2 |
| Resident | 223 | 15.5 |
| Specialist | 79 | 5.5 |
| Consultant | 122 | 8.5 |
| Nurse | 297 | 20.7 |
| Specialty interest | ||
| Not decided yet General surgery | 182 183 | 12.7 12.7 |
| Internal medicine | 149 | 10.4 |
| OB/Gyn | 81 | 5.6 |
| Paediatrics | 126 | 8.8 |
| ER | 79 | 5.5 |
| Family medicine | 76 | 5.3 |
| Other | 562 | 39.1 |
| Participated in a burn training course before | ||
| Yes | 249 | 17.3 |
| No | 1189 | 82.7 |
| Experienced a burn injury before to self or family | ||
| Yes | 974 464 | 67.7 32.3 |
| No |
Of all respondents, 961 (66.8%) knew that washing the burned area with cool water was the first correct step for treating a burn trauma. However, 940 (65.4%) respondents tended to use traditional remedies on the burn area, most of the respondents 629 (43.7%) used honey as a traditional remedy. Moreover, 1,199 (82.3%) of the participants agreed that antibiotics are beneficial in the case of burns. Knowledge regarding electrical burns seemed better—more than 90% of the respondents knew it was unsafe to touch an electrocuted person still in physical contact with the electrical current and that the first action is to turn off the source of electricity [Table 2].
Table 2.
Percentage of correct answers for the burn knowledge-related questions
| Burn-related questions | Correct answer | Correct answer n | Correct answer % |
|---|---|---|---|
| Washing the burned area with cool water is the first correct step in case of burn injuries | Agree | 961 | 66.8 |
| In case of burn injury, which one out of the following traditional medications will you consider applying? | None | 498 | 34.6 |
| How does one extinguish a pot of oil that has caught fire? | Cover with cloth | 779 | 54.2 |
| Burns can lead to permanent injuries | Agree | 1327 | 92.3 |
| Burn injuries can lead to mental disorders? | Agree | 807 | 56.1 |
| In case of burn injury, covering the burned area before heading to the hospital can decrease the risk of infection | Agree | 683 | 47.5 |
| In case of burn injury, picking blisters is an incorrect action | Agree | 972 | 67.6 |
| Applying first aid medicine at home on a burned area leads to a better outcome | Agree | 1097 | 76.3 |
| In case of burn injury, apply water for: | 10-15 min | 244 157 | 17.0 10.9 |
| 15 min | 157 | 10.9 | |
| In case of burn injury, if your clothes were on fire you should roll on the ground | Agree | 1226 | 85.3 |
| In case of burn injury, it is beneficial to use antibiotics for management | Disagree | 255 | 17.7 |
| In case of electrical burn injury, I should not touch the injured person if he/she is still in contact with the electrical current | Agree | 1305 | 90.8 |
| In case of electrical burn injury, the first action is to turn off the source of electricity if possible | Agree | 1297 | 90.2 |
Respondents' predominant source of knowledge on first aid for burns was “lectures,” according to 728 individuals (50.6%). The least common source of information was “conferences,” as indicated by only 122 (8.5%) respondents [Chart 1].
Chart 1.
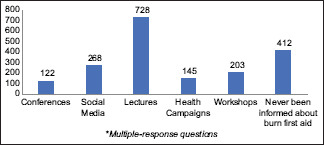
Respondents’ source of information regarding first aid for burns
Chart 2 shows the respondents' knowledge about burn centres in Jeddah, Saudi Arabia. Most of the respondents (826, 57.4%) correctly indicated that there was a burn centre in King Fahad General Hospital, Jeddah.
Chart 2.
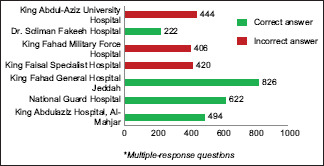
Respondents’ knowledge of burn centres in Jeddah, Saudi Arabia
The mean burn knowledge score of all respondents was 8.07 ± 2.03 out of 13. The mean burn knowledge score split by the respondents' baseline characteristics is presented in Table 3. The table also shows that the mean knowledge score was significantly different across the groups for age, sex, nationality, marital status, and job position (P < 0.001). Those who participated in the burn training course had statistically significantly higher burn knowledge scores (8.34 ± 2.20 vs. 8.02 ± 1.99) than their counterparts (P < 0.001). People who had experienced burn traumas themselves or had family members who had experienced burn traumas had significantly higher burn knowledge scores (8.17 ± 1.95 vs. 7.86 ± 2.19) (P 0.024) [Table 3].
Table 3.
Relationship between the burn knowledge score and baseline characteristics
| Characters | Mean score | P |
|---|---|---|
| Age | <001 | |
| 19-21 | 7.32±2.10 | |
| 22-29 | 8.08±1.88 | |
| 30-39 | 8.80±2.12 | |
| 40-50 | 8.94±1.79 | |
| >50 | 9.21±1.20 | |
| Gender | <001 | |
| Male | 8.46±2.01 | |
| Female | 7.89±2.02 | |
| Nationality | <001 | |
| Saudi | 7.97±2.01 | |
| Non-Saudi | 8.70±2.06 | |
| Marital status | <001 | |
| Single | 7.81±2.01 | |
| Married | 8.68±1.96 | |
| Widowed | 7.67±0.58 | |
| Divorced | 8.79±191 | |
| Job position | <001 | |
| Medical student | 7.28±2.08 | |
| Medical intern | 8.47±1.57 | |
| Resident | 8.56±1.71 | |
| Specialist | 8.82±1.89 | |
| Consultant | 9.11±1.49 | |
| Nurse | 8.19±2.20 | |
| Participated in a burn training course before | <001 | |
| Yes | 8.34±2.20 | |
| No | 8.02±1.99 | |
| Experienced a burn injury before to self or family | ||
| Yes | 8.17±1.95 | .024 |
| No | 7.86±2.19 |
Discussion
In this study we included 1,438 respondents. Females comprised 68.2% (982) of the respondents. The mean burn knowledge score of all respondents was 8.07 ± 2.03 out of 13 Interestingly, 940 individuals (65.4%) used traditional medications on the burn area. Knowledge regarding antibiotic use in burn injuries was poor—1,199 (82.3%) study participants agreed that antibiotics are beneficial in the case of burns. The mean knowledge score was significantly different across groups of different ages, sexes, nationalities, marital statuses, and job positions (P < 0.001). Different cities in Saudi Arabia report burn injuries occurring because of a variety of different causes, affecting individuals of all ages and different parts of the body.[1,2,3,4,5,6,7,8,9] Regarding the knowledge of burn prevention and first aid treatments, a variety of studies have reported a noticeable lack of awareness worldwide.[7,8,9,10] This study aimed to assess the level of awareness and perception among healthcare contributors concerning the early involvement of first aid in the case of burn injuries.
Healthcare workers' understanding and overall knowledge of first aid for burns play a crucial role in raising awareness regarding this topic in their community. This study revealed that medical personnel with different levels of experience have insufficient awareness concerning the first aid of burns overall. The mean burn knowledge score of all respondents was 8.07 ± 2.03 out of 13. This may be because of exposure to burns in general during the medical carrier even if it was not in the individual's field of expertise. The mean knowledge score of our respondents aligns with that of another study that was conducted among medical students, as the study has shown that the students had inadequate knowledge of first aid for burns and their prevention.[10] Additionally, a study with similar results conducted among Australian healthcare workers was published, as they showed burn first aid overall knowledge among healthcare workers was very poor.[11] The level of the knowledge score was significantly different across different age groups, gender groups, nationalities, marital status groups, and job positions (P < 0.001). Participants with higher-level job positions were considered more aware, and this association could potentially be explained by the experience and knowledge gained with time.
Despite the efforts of healthcare professionals to instruct the general public about the positive effects of applying water (10-15°C) for 20–30 min as preliminary control for acute burns,[7] 33.2% of the participants in our study answered “washing the burned area with cool water is the first correct step in case of burn injuries” incorrectly. Recent studies conducted in Saudi Arabia, China, Australia, and Cambodia reflected a similar situation wherein only 5.8%, 13.7%, 9%, and 13% of the study participants, respectively, had knowledge on how to apply water to the burn area.[8,12,13,14,15] With statistically significant differences in the level of understanding and education among participants, our study has shown the value of burn training courses, as those who had participated in a burn first-aid training course had a higher overall knowledge score than did their counterparts, which aligns with the results from a study conducted by Rea et al.[11] Alternatively, more than half of the respondents (65.4%) had a tendency to apply some form of conventional medicine to the burn areas, which is an incorrect technique for managing such a situation. These include substances such as toothpaste, honey, aloe vera, oil, or espresso. This kind of traditional practice can be harmful, as it can worsen pain, tenderness, and skin sloughing and increase susceptibility to infection. It has been reported in the literature that traditional remedies for burn first aid have been excessively used by people. In our study, we found that the most popular household item used for this purpose by the study population was “honey.” Less than half of the participants (43.7%) acknowledged that they applied honey as first aid treatment for their burns. This extent of this practice varies across worldwide.[15,16,17,18] The use of some herbs has created quite a controversy—aloe vera has anti-bacterial and anesthetic effects, but its effectiveness as a first aid measure for the improvement of burn outcomes conflicts with the general impression from various studies indicating that although it is not harmful it is of no benefit either.[19,20] Toothpaste was chosen by 19.1% of respondents (n = 279) as an option for burn control. The use of toothpaste in burns was also observed in other countries such as the UK (4%), Turkey (1.9%), and Cambodia (18%), where its harmful effects and possible role in exacerbation of the initial injury have been documented.[15,16,17,18] Some agents, such as honey, have beneficial effects; however, it is better for people to avoid it and use clean, water instead.[21] More than half of the respondents tended to use traditional medications on burn areas, which is not a correct approach. Overall, when it comes to the treatment of burns, in comparison with traditional remedies, the use of available scientifically verified remedies is inexpensive and simple and has no potentially harmful effects if applied appropriately. Most traditional remedies are not beneficial and make medical wound treatment difficult. This study is one of the first to assess the awareness of first aid of burns among healthcare workers. Many different interventions can be carried out to increase awareness on first aid for burns. Self-explanatory brochures and extra lectures on immediate burn treatments and the non-beneficial aspects of using traditional remedies can increase awareness regarding burn treatments and change the attitude towards traditional remedies of healthcare workers. In our study, the overall knowledge score of all respondents was 8.07 ± 2.03 out of 13. Surprisingly, the majority of the healthcare providers (82.3%) agreed on using antibiotics in management of burns. Thus, the level of awareness and knowledge of first aid for burn patients among healthcare providers was inadequate.
Limitations
Our study addressed its objective and the sample size was much larger than that in any detailed article in this field; however, some limitations need to be addressed. Our study was a single-institution, cross-sectional study, and spanned a short interval of time, as there is a possibility that the responses do not represent all healthcare workers in Saudi Arabia. We recommend future research papers that include different institutes from different regions in Saudi Arabia
Conclusion
Although healthcare workers showed a positive attitude toward the field of first aid for burns, their level of perception and knowledge of first aid for burns was insufficient. Moreover, this study confirmed the need for an effective educational program for healthcare contributors to enhance their knowledge and understanding regarding the first aid for burns, which will indirectly increase the success and provision of ideal treatment for the patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Al-Shehri M. The pattern of paediatric burn injuries in Southwestern, Saudi Arabia. West Afr J Med. 2004;23:294–9. doi: 10.4314/wajm.v23i4.28144. [DOI] [PubMed] [Google Scholar]
- 2.Gari AA, Al-Ghamdi YA, Qutbudden HS, Alandonisi MM, Mandili FA, Sultan A. Pediatric burns in Western Saudi Arabia. Saudi Med J. 2012;33:1106–10. [PubMed] [Google Scholar]
- 3.Ministry of Health Statistics. Injuries/Burns. 2018. [Last accessed on 2020 Jun 23]. Available from: http://wwwmohgovsa/Ministry/Statistics/book/Documents/2014 .
- 4.Al-Thunyan A, Al-Qattan MM, Al-Husainan H, Al-Meshal O. Contact charcoal burn associated with acute. central cord syndrome Biomed Res. 2014. p. 25. Available from: http://wwwalliedacademiesorg/articles/contact-charcoal-burn-associated-with-acute-central-cord-syndromehtml .
- 5.Othman N, Kendrick D. Epidemiology of burn injuries in the East Mediterranean Region: A systematic review. BMC Public Health. 2010;10:83. doi: 10.1186/1471-2458-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitkanen J, Al-Qattan MM. Epidemiology of domestic chemical burns in Saudi Arabia. Burns. 2001;27:376–8. doi: 10.1016/s0305-4179(00)00126-1. [DOI] [PubMed] [Google Scholar]
- 7.Raine TJ, Heggers JP, Robson MC, London MD, Johns L. Cooling the burn wound to maintain microcirculation. J Trauma. 1981;21:394–7. doi: 10.1097/00005373-198105000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Kattan AE, AlShomer F, Alhujayri AK, Addar A, Aljerian A. Current knowledge of burn injury first aid practices and applied traditional remedies: A nationwide survey. Burns Trauma. 2016;4:37. doi: 10.1186/s41038-016-0063-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alsalman AK, Algadiem EA, Alalwan MA, Farag TS. Epidemiology of infant burn in Eastern. Saudi Arabia Saudi Med J. 36:324–7. doi: 10.15537/smj.2015.3.10683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siddiqui A, Qahtani SQ, Qahtani AM, Barkout S, AlAamri AK. Knowledge, attitudes and practice of burns prevention and first aid among medical students of King Khalid University, SaudiArabia. Bangladesh J Med Sci. 2018;17:537–44. [Google Scholar]
- 11.Rea S, Kuthubutheen J, Fowler B, Wood F. Burn first aid in Western Australia--do healthcare workers have the knowledge? Burns. 2005;31:1029–34. doi: 10.1016/j.burns.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Yongqiang F, Yibing W, Dechang W, Baohua L, Mingqing W, Ran H. Epidemiology of hospitalized burn patients in Shandong Province: 2001-2005. J Burn Care Res. 2007;28:468–73. doi: 10.1097/BCR.0B013E318053D28B. [DOI] [PubMed] [Google Scholar]
- 13.Harvey L, Barr M, Poulos R, Finch C, Sherker S, Harvey J. A population-based survey of knowledge of first aid for burns in New South Wales. Med J Aust. 2011;195:465–8. doi: 10.5694/mja11.10836. [DOI] [PubMed] [Google Scholar]
- 14.Cuttle L, Kempf M, Liu PY, Kravchuk O, Kimble RM. The optimal duration and delay of first aid treatment for deep partial thickness burn injuries. Burns. 2010;36:673–9. doi: 10.1016/j.burns.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Hsiao M, Tsai B, Uk P, Jo H, Gomez M, Gollogly J, et al. What do kids know: A survey of 420 grade 5 students in Cambodia on their knowledge of burn prevention and first-aid treatment. Burns. 2007;33:347–51. doi: 10.1016/j.burns.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Khan AA, Rawlins J, Shenton AF, Sharpe DT. The Bradford burn study: The epidemiology of burns presenting to an inner city emergency department. Emerg Med J. 2007;24:564–6. doi: 10.1136/emj.2005.027730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skinner A, Peat B. Burns treatment for children and adults: A study of initial burns first aid and hospital care. N Z Med J. 2002;115:U199. [PubMed] [Google Scholar]
- 18.Karaoz B. First-aid home treatment of burns among children and some implications at Milas, Turkey. J Emerg Nurs. 2010;36:111–4. doi: 10.1016/j.jen.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 19.Cuttle L, Pearn J, McMillan JR, Kimble RM. A review of first aid treatments for burn injuries. Burns. 2009;35:768–75. doi: 10.1016/j.burns.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Hansen S, Mecham N. Pediatric anaphylaxis: Allergic reaction to egg applied to burns. J Emerg Nurs. 2006;32:274–6. doi: 10.1016/j.jen.2005.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Branche C, Oyebite K, Hyder AA, Ozanne-Smith J, Bartolomeos K, Rivara F. World Report on Child Injury Prevention. World Health Organization; 2008. [PubMed] [Google Scholar]


