Dear editor,
Since the first cases of SARS-CoV2 (COVID-19) outbreak was declared by local authorities in Wuhan, Hubei province, People’s Republic of China in December 2019, we are gathering more information about the virus and the disease. On March 11th WHO Director General Tedros Adhanom Ghebreyesus declared outbreak a “pandemic” that eventually infected 3.726.299 persons and unfortunately killed 257.405 lives in 215 countries (1). The very same day, Health Minister of Republic of Turkey Dr. Fahrettin Koca has announced the first COVID-19 case in Turkey (Figure 1) (2). The pandemic poses unprecedented threat to global public health, social and economic stability that the World needs to recover. How and when we will resume normal life is a matter of curiosity that will depend on the definition of the new “normal”, yet the answer is not clear. Therefore, orthopaedics and traumatology surgeons and other surgical disciplines must realize that we are not only a part of the pandemic team but also carry the responsibility to set safety standards for our patients and ourselves. Under these circumstances authors tried to compile information on the management of the elective, urgent and time sensitive cases related Orthopaedics and Traumatology.
Figure 1.
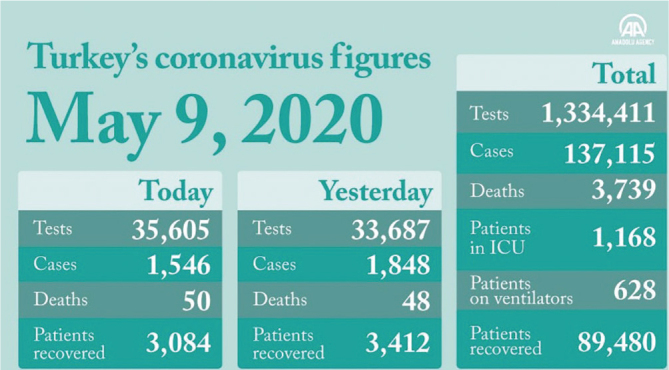
Number of cases and breakdown on May 9th (2)
American College of Surgeons advises that hospitals should establish their pandemic plans and delay elective surgeries until pandemic declines. These guidelines will allow us rational use of ward and ICU beds and ventilators. Delaying non-urgent/elective surgeries not only will reduce the health care workers’ risk of becoming infected, but also alleviate burden on anesthesiology, ICU staff and nursing staff (2), The pandemic is managed by Ministry of Health in accordance to the advices of Scientific Board in Turkey. The guidelines, which are updated based on published new literature, are prepared to prevent the spread of the virus and to protect the medical staff (3). Under these circumstances, all published guidelines recommend the treatment of trauma patients. The prevention methods will protect not only the surgical team but also the other uninfected patients.
It will be easy to divide the routine orthopaedics and traumatology patients under groups to describe the prevention methodology. It is strongly advisable that surgeons should follow the daily released statistics and guidelines by either The Ministry of Health or other reliable sources such as WHO, USA-CDC, Imperial College, London, UK-NHS etc. Should there be a suspicion, COVID-19 fast test (Ig G/Ig M rapid test) may be asked wherever available, otherwise scanning may be performed in 5-day period by RT-PCR molecular test.
Outpatient cases: Asymptomatic patients are very important at the spread of the virus. Routine controls of previously operated patients should be postponed by contacting patients (4). Waiting area in outpatient clinics should be organized in a way to ensure sufficient social distancing. All patients entering the waiting area must wear surgical/three layer facemasks. Facemasks should be provided to patients arriving without a mask. Hand sanitizers should be at disposal in a visible location. Body temperature screening is advisable when possible. Doctors’ personal protective equipment (PPE) should include a disposable hood, surgical mask preferably with a shield, disposable gown and non-sterile examination gloves and shoe covers (Figure 2). In case shields are not available, goggles should be worn at all times (5–7). Disposable examination bed sheaths should be used. After the examination, gloves and sheaths must be disposed in the medical waste bin.
Figure 2.
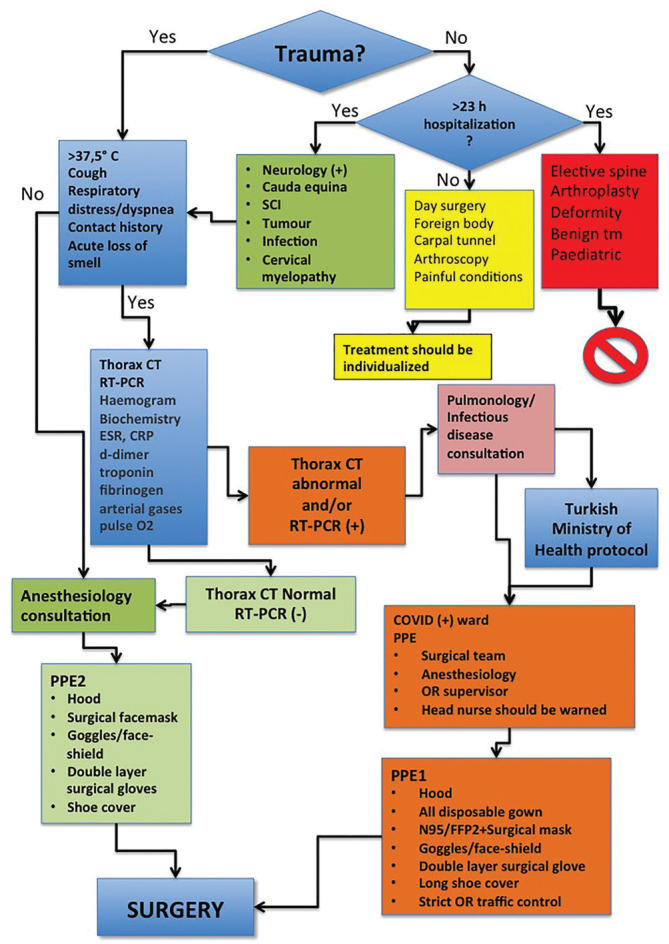
Pre-operative flow-chart for patients undergoing orthopaedic surgery
Telemedicine may be of help for follow-up patients in institutions that have established infrastructure (4, 8).
Emergency cases: Casualties should be admitted to examination rooms that are prepared specifically to evaluate and treat COVID-19 positive or suspected cases. Medical equipment like injectors, sponges, plaster of paris cast, elastic bandages, etc. must be prepared for the patient in a tray and brought into the examination room. All equipment that is not imminently needed must be kept in storage rooms near by to reduce the risk of contamination. Even if there is an open fracture or multiple trauma in the ER, the priority of the surgical team must be self-protection, examination and intervention should only start after appropriate PPE is donned (5, 6, 9). Designated doffing areas must be established with readily visible visual guideline hung on the wall.
Evaluation of the patients who need surgical procedures
Authors prefer to evaluate patients in 5 different groups. Surgical procedures must be short and definitive to reduce the risk of virus exposure and multiple OR returns.
Day surgery: (patients requiring <23 hours hospital stay) All patients must be evaluated for having fever, cough, nasopharyngeal symptoms, myalgia, loss of smell and diarrhea. Patients having these symptoms must be consulted to Infectious Diseases, and Pulmonology clinics. It is well known that most of the COVID-19 patients are asymptomatic, routine PPE must be donned. Arthroscopic procedures, nerve entrapments, and implant removals are included in this group. The surgical exposures had better be as small as possible. The hospitalization must be as short as possible. Arthroscopic procedures cause aerosol particles during using of shavers, burrs and RF equipment, so arthroscopy may be performed with limited indications. Besides, we must emphasize that this group of surgeries must be delayed to preserve beds for COVID-19 patients and conservative treatment methods may be tried to relieve the symptoms (5, 7, 10). During normalization period of the pandemic the definitive treatment of these patients may be managed in COVID free hospitals.
Elective surgeries: (patients requiring>23 hours hospital stay) Osteoarthritis, paediatric deformities, spinal deformities and the surgical procedures, which require more than 23-hour hospitalization, must be delayed. Conservative treatments like intraarticular steroid injections for gonarthrosis may be performed with care to relief the symptoms. NHS guideline for the use of corticosteroids advocate steroids when they are the only option to use (11).Use of telemedicine is recommended for follow-up of such patients wherever possible (4, 5, 7, 8, 10, 12).
Urgent surgical procedures: Treatment of these patients must be performed as soon as possible. In COVID-19 positive patients, we advise readers to refer Turkish Republic, Ministry of Health guideline released on 14 April 2020 (Figure 2).
Hip fractures, pelvis and acetabulum fractures, paediatric fractures, long bone fractures, peri and intraarticular fractures, osteoporotic/pathologic fractures, open fractures and septic arthritis are in this group. Most of our geriatric patients will have comorbidities like diabetes mellitus, hypertension and chronic obstructive pulmonary diseases. Clinical studies revealed that patients with comorbidities have increased risk of morbidity and mortality. Minimal invasive surgical procedures with short surgery time may be preferred for these patients and surgeries with high risk of morbidities must be avoided. Need of blood transfusion, wound complications and systemic complications may be decreased by these measures. Continuous use of electrocautery, high torque drilling, saw and reamerisation must be avoided if possible (7, 13–16).
Oncologic patients: Management of oncologic cases must be performed under proper PPE protection as described in figure 2. Adjuvant or neoadjuvant therapies should continue for the oncology cases that do not require urgent surgeries. If there is a radiosensitive tumour, radiotherapy can help us to delay the surgery for three or four months. However, musculoskeletal oncology pathologies are time sensitive and may be life threatening, therefore case based decision is advisable (7, 15, 17).
Spinal procedures: Patients with spinal pathologies will be evaluated in two groups. Group 1 includes patients with urgent spinal pathologies and group 2 includes deformities, spinal stenosis, and discopathies without neurologic deficits (12).
Group 1 patients: Cauda-equina syndromes, spinal traumas, primary or metastatic spinal tumours, discopathies with neurologic deficits are in this group. The surgical treatment must be performed according to the steps in figure 2 with PPE protection. Minimal invasive procedures in prone position may be preferred in the suitable circumstances. Spinal surgery has high risk of bleeding in intraoperative and postoperative period. Therefore, ultimate measures should be taken to minimize bleeding like using tranexamic acid, limited surgical exposure, and using electrocautery. While using electrocautery, continuous aspiration will help to reduce the aerosol particles. Corticosteroids like Betamethasone, which will not make suppression on the hypothalamic pathway, must be preferred when in need (12, 18).
Group 2 patients: Conservative measures will resume first line in this group. Telemedicine may be referred when in need (7, 8, 12, 18, 19).
Steroid uses in Covid-19 pandemic:
Don’t stop current steroids but taper their dose if possible and clinically safe to do so.
Think before starting steroids in the current pandemic.
Use the lowest possible dose of oral steroids.
Only give steroid injections if patient has significant disease activity and there are no alternatives.
Only use for inflammatory joints where there is active synovitis±effusion intra-articular injections.
Generally, avoid for spinal pain and instead recommend simple analgesia, activity modification and exercise. Consider referral for epidural or nerve root block for severe radicular pain (20).
Coagulopathy is frequently seen in COVID-19. Postoperative use of anticoagulants should be ordered as usual. Prothrombin time, aPTT, D-Dimer, fibrinogen and thrombocyte count should be monitored. Detailed anticoagulant protocol can is described in Ministry of Health guideline (4).
In conclusion, definitive treatment should be performed in urgent cases during this SARS-CoV2 pandemic. Besides, appropriate conservative treatments in selected elective cases spare the beds of our institutions, medical equipment and efforts of the medical team. Conservative treatment of fractures should be prioritized whenever possible. Our basic goal must be to reduce the nosocomial COVID-19 infections while keeping our patients and us safe. We may have to treat a COVID-19 (+) patient and be part of the pandemic team, under such conditions multidisciplinary care will be of the utmost importance.
Health Minister Koca declared 7428 healthcare personnel to be COVID-19 (+) on April 29th. Thus it is paramount that we healthcare work-power should protect ourselves to continue treating our patients. Latest literature states that even under high standard prevention measures doctors, nurses may be infected in common meeting areas, lounges and toilets due to the virus carrying aerosols (21).
One of the most important issues remaining is the education of orthopaedics and traumatology residents, every measure should be taken to reassure the continuation of education (22).
Management of Orthopedics and Traumatology Patients During SARS-Cov-2 Pandemic is shown at Table 1 (6, 17, 23–30).
Table 1.
| Preoperative period | Perioperative surgery staff and perioperative surgery nurses | Scrub nurse and OR technician | Anaesthesiology specialist and technician | OR technician | |
|
| |||||
| COVID-19 (+,?) | COVID-19 (−) | Prepares for surgery,
|
They should follow the Turkish Health Ministry COVID -19 guidelines for OR and anesthesiology | Provide the equipment which will be used during surgery | |
|
| |||||
| Isolated ward/PACU/ICU | Orthopedic ward | ||||
|
| |||||
| PPE1 | PPE2 | ||||
|
| |||||
| Intraoperative period | Surgeon takes precautions to shorten the time of surgery.
|
||||
| Postoperative period |
|
||||
| Clinical follow-up and rehabilitation period |
|
||||
PPE: personal protective equipment. Referred to flowchart for PPE1 and PPE2; PACU: post-anesthesia care unit; ICU: intensive care unit; OR: operating room; DVT: deep vein thrombosis; LMWH: low-molecular-weight heparin
It is now the time to plan normalization procedures. Management of the cases may begin from minor/day surgery procedures and then major procedures, which require long hospital stay. The control of the SARS-CoV2 pandemic in a short time will help us to reach our normal life as usual.
References
- 1.WHO. WHO situation report 2020. May 08, 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.COVID-19: Recommendations for Management of Elective Surgical Procedures. American College of Surgeons; Mar 13, 2020. [Google Scholar]
- 3.Covid-19 (Sars-CoV-2 Enfeksiyonu) Rehberi. TC Sağlık Bakanlığı Halk Sağlığı Genel Müdürlüğü. 2020 Apr 14; [Google Scholar]
- 4.Villani A, Scalvenzi M, Fabbrocini G. Teledermatology: a useful tool to fight COVID-19. J Dermatolog Treat. 2020;31:325. doi: 10.1080/09546634.2020.1750557. doi: 10.1080/09546634.2020.1750557. [DOI] [PubMed] [Google Scholar]
- 5.Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic. National Health Service; Mar 16, 2020. [Google Scholar]
- 6.Kamer E, Çolak T. What to do when a patient infected with COVID-19 needs an operation: A pre-surgery, peri-surgery and post-surgery guide. Turk J Colorectal Dis. 2020;30:1–8. doi: 10.4274/tjcd.galenos.2020.2020-3-7. [DOI] [Google Scholar]
- 7.Chang Liang Z, Wang W, Murphy D, Po Hui JH. Novel coronavirus and orthopaedic surgery: Early experiences from Singapore. J Bone Joint Surg Am. 2020;102:745–9. doi: 10.2106/JBJS.20.00236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:487–92. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Correia M, Ramos RF, Von Bahten LC. The surgeons and the COVID-19 pandemic. Rev Col Bras Cir. 2020;47:e20202536. doi: 10.1590/0100-6991e-20202536. doi: 10.1590/0100-6991e-20202536. eCollection 2020. [DOI] [PubMed] [Google Scholar]
- 10.Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP. COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative period. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003925. doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS. Clinical guide for the management of patientswith musculoskeletal and rheumatic conditionson corticosteroids during the coronaviruspandemic. 2020 [Google Scholar]
- 12.Clinical guide for the management of patients requiring spinal surgery during the Coronavirus pandemic. National Health Service; Mar 20, 2020. Publications approval reference: 001559. [Google Scholar]
- 13.Tay YC, Ng SY, Soh CR. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020 Mar 13; doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tellez Duarte A. COVID 19 in Orthopedics. Available from: https://www.researchgate.net/publication/340049928_COVID_19_in_Orthopedics. [DOI]
- 15.Karaca AS, Özmen MM, Uçar AD, Yastı AÇ, Demirer S On Behalf of the Initiative of the Board of Directors of the Turkish Surgical Society. General surgery operating room practice in patients with COVID-19. Turk J Surg. 2020;36(1) doi: 10.5578/turkjsurg.202001. doi: 10.5578/turkjsurg.202001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeh HC, Turner RS, Jones RK, Muggenburg BA, Lundgren DL, Smith JP. Characterization of aerosols produced during surgical procedures in hospitals. Aerosol Sci Technol. 1995;22:151–61. doi: 10.1080/02786829408959736. [DOI] [Google Scholar]
- 17.Bartlett DL, Howe JR, Chang G, et al. Management of cancer surgery cases during the COVID-19 pandemic: Considerations. Ann Surg Oncol. 2020;27:1717–20. doi: 10.1245/s10434-020-08461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zou J, Yu H, Song D, Niu J, Yang H. Advice on standardized diagnosis and treatment for spinal diseases during the coronavirus disease 2019 pandemic. Asian Spine J. 2020;14:258–63. doi: 10.31616/asj.2020.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong J, Goh QY, Tan Z, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020;67:732–45. doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Services NHC. Clinical guide for the management of patients with musculoskeletal and rheumatic conditions on corticosteroids during the corona virus pandemic. 2020 Mar 25; Publications approval reference: 001559. Version 1. [Google Scholar]
- 21.Liu Y, Ning Z, Chen Y, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020 doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz A, Wilson J, Boden S, Moore T, Bradbury T, Fletcher N. Managing resident workforce and education during the COVID-19 pandemic: Evolving strategies and lessons learned. JBJS Open Access. 2020;5 doi: 10.2106/JBJS.OA.20.00045. doi: 10.2106/JBJS.OA.20.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020;67:756–8. doi: 10.1007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Editor-in-Chief P. Yu L. Handbook of COVID-19 Prevention and Treatment. 2020 [Google Scholar]
- 25.Liang T, editor. Handbook of COVID-19 Prevention and Treatment. The First Affiliated Hospital, Zhejiang University School of Medicine; 2020. Available from: https://cm-us-standard.s3.amazonaws.com/documents/Zhejiang-University-Handbook-of-COVID-19-Prevention-and-Treatment.pdf. [Google Scholar]
- 26.Chow TT, Kwan A, Lin Z, Bai W. Conversion of operating theatre from positive to negative pressure environment. J Hosp Infect. 2006;64:371–8. doi: 10.1016/j.jhin.2006.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park J, Yoo SY, Ko JH, et al. Infection prevention measures for surgical procedures during a Middle East respiratory syndrome outbreak in a tertiary care hospital in South Korea. Sci Rep. 2020;10:325. doi: 10.1038/s41598-019-57216-x. doi: 10.1038/s41598-019-57216-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li HW, Wu CY, Tepper F, Lee JH, Lee CN. Removal and retention of viral aerosols by a novel alumina nanofiber filter. J Aerosol Sci. 2009;40:65–71. doi: 10.1016/j.jaerosci.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pandemi Döneminde Ameliyathanelerde Alınacak Enfeksiyon Kontrol Önlemleri. TC Sağlık Bakanlığı Halk Sağlığı Genel Müdürlüğü. 2020 Apr 26; [Google Scholar]
- 30.COVID-19 Pandemi Döneminde Ameliyathanelerde Alınacak Enfeksiyon Kontrol Önlemleri. TC Sağlık Bakanlığı Halk Sağlığı Genel Müdürlüğü. 2020 Apr 27; [Google Scholar]


