Abstract
Acute lunate and perilunate dislocations are not commonly observed injuries. In particular, palmar-divergent dislocation is a very rare injury with only a few cases reported in the literature. In this report, we describe the case of a 37-year-old patient with palmar-divergent dislocation of the scaphoid and lunate and discuss the mechanism of this type of injury. We also report a potential treatment for this pattern of palmar-divergent dislocation. The scapholunate and scaphocapitate joints were stabilized with K-wires and a modified pin-in-plaster fixation for 5 weeks after successful closed reduction. At the 1-year follow-up, magnetic resonance imaging showed no evidence of avascular necrosis of the scaphoid or lunate. However, radiographs showed mild dorsal intercalated segment instability deformity. The patient experienced no intermittent wrist pain or limitation in motion, with only 15% loss in grip strength. The Mayo wrist score was 90/100, and the patient resumed work as a craftsman. The carpal height ratio at the 4-year follow-up was 1.51 and 1.52 for the left and right wrists, respectively. In conclusion, we recommend this treatment method due to its benefits of being relatively simple, easy to perform, and having a relatively short operation time. Essentially, a good outcome was achieved using this method, including full range of motion and freedom from pain.
Keywords: Palmar-divergent dislocation, Scaphoid and lunate, Pin-in-plaster, Carpal instability, Perilunate dislocation
Carpal dislocation injuries are relatively rare. They occur most commonly in young males who sustain high-energy trauma injuries, such as injuries from a motor vehicle accident, fall from a height, or in contact sports. Acute lunate and perilunate dislocations are uncommon. In particular, palmar-divergent dislocation is a very rare injury, with only a few cases having been reported (Table 1) (1–6).
Table 1.
Treatment methods reported previously for palmar-divergent dislocation
| Author/year | Surgical procedure | Duration of immobilization | Range of motion | Sequelae/pain |
|---|---|---|---|---|
| Gordon/1972 | Open reduction | Cast/4 weeks | Ext 15° Flex 25° |
DISI Minimum pain |
| Küpfer/1986 | Open reduction K-wire pinning(S-L) |
Cast/4 months K-pins/4 months |
Ext 25° Flex 0° |
DISI & AN Free of pain |
| Baulot et al./1997 | Open reduction Anterior capsule suture |
Cast/6 weeks | Almost full | DISI Free of pain |
| Kang et al./2003 | Open reduction K-wire pinning(S-L/S-C) |
Cast/6 weeks K-pins/6 weeks |
Almost full | None Intermittent pain |
| Komura et al./2011 | Closed reduction Anterior capsule suture Interosseous ligament repair K-wire pinning(S-L/L-T) |
Splint/7 weeks K-pins/7 weeks |
Ext 50° Flex 40° |
None NR |
| Idrissi and Galiua/2011 | Closed reduction K-wire pinning(S-L/L-T) |
Cast/4 weeks K-pins/6 weeks |
Ext 40° Flex 60° |
DISI Free of pain |
K-wire: Kirschner wire; S: scaphoid; L: lunate; T: triquetrum; C: capitate; DISI: dorsal intercalated segment instability; Ext: extension, Flex: flexion; AN: Avascular necrosis; NR: not recorded
To the best of our knowledge, this is the second reported case of a palmar-divergent dislocation of the scaphoid and lunate treated using closed reduction and percutaneous pinning. Herein, we discuss the mechanism of this type of injury and report how the pattern of palmar-divergent dislocation affects treatment.
Case Presentation
A 37-year-old man who fell from a height of 6 m onto his left hand and chin was brought to the hospital emergency center. The left wrist of the patient, who was left-handed, was swollen with marked volar tenderness, while the neurovascular status of the hand was normal. Radiographs of the injured wrist revealed complete palmar-divergent dislocation of the scaphoid and lunate (Figure 1). Additionally, the patient had a head injury and a fractured mandible. Two hours after sustaining the injury, an unsuccessful attempt at closed reduction was performed under thiamylal sodium anesthesia in the emergency room. The patient was scheduled for closed or possible open reduction under general anesthesia in the operating room.
Figure 1. a, b.
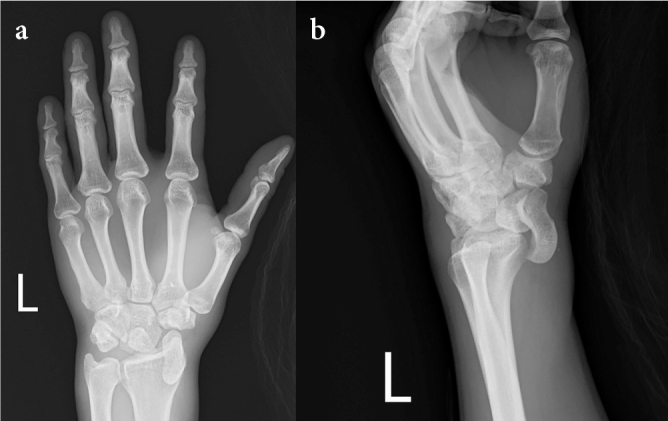
Anteroposterior radiograph at initial diagnosis showing palmar-divergent dislocation of the scaphoid and lunate (a). Lateral radiograph clearly shows that the scaphoid and lunate were dislocated volarly (b)
Under general anesthesia, the arm was stabilized with the elbow flexed at 90°. Manual axial traction with a 5-kg weight was applied on the hand (Figure 2). The lunate was first pushed with both thumbs distally into its fossa, following which a reduction of the scaphoid was performed. Fluoroscopy showed normal alignment of the radius, lunate, and capitate. The scapholunate (SL) and scaphocapitate joints were fixed using two 1.5-mm K-wires inserted from the scaphoid to the lunate and from the radial styloid to the capitate. Two additional 1.8-mm pins were placed in the radius and in the second metacarpal. Following this, all the pins were incorporated into an immobilizing resin cast (Figure 3).
Figure 2.
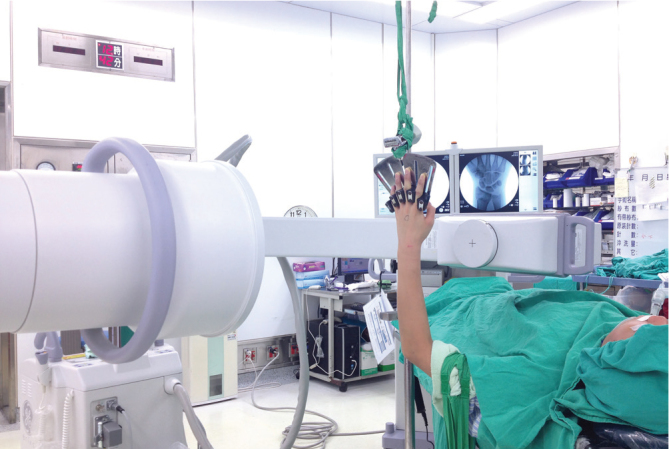
Photograph shows the patient’s wrist suspended in finger traps with 5-kg traction under fluoroscopic assessment in preparing for the closed reduction
Figure 3. a, b.
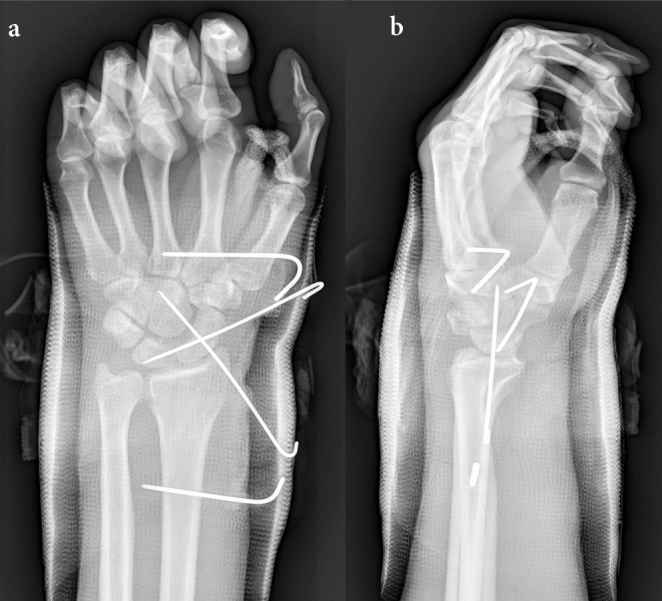
Postoperative anteroposterior radiograph shows the scapholunate and scaphocapitate joints fixed with two Kirschner wires. A modified pin-in-plaster technique was used to maintain sufficient immobilization (a). Lateral radiograph shows that the scaphoid and lunate were reduced anatomically (b)
The patient was carefully monitored after surgery. X-rays were obtained 2 weeks after surgery. X-rays were also obtained at the 5-week follow-up when the K-wires and cast were removed (Figure 4). Subsequently, the patient started 1 month of intensive rehabilitation. At the 1-year follow-up, the patient reported that he had returned to normal life and work without experiencing wrist pain. The range of motion (ROM) of both wrists was almost the same, but the grip strength was approximately 85% on the injured side compared with that on the uninjured side (Figure 5). The modified Mayo wrist score was 90/100 points (pain, 25 points; satisfaction, 25 points; ROM, 25 points; grip strength, 15 points), which is considered excellent. Magnetic resonance imaging showed no evidence of avascular necrosis of the scaphoid or lunate. However, dorsal intercalated segment instability (DISI) deformity was observed on radiographs. The capitolunate angle was 32°, and the SL angle was 84° (Figure 6). This condition remained unchanged at the 4-year follow-up. The carpal height ratio (measured using the Nattrass method) at the 4-year follow-up was 1.51 and 1.52 for the left and right wrists, respectively.
Figure 4. a, b.

Anteroposterior view (a). Lateral view (b). Radiographs show that the normal relationships of carpal bones have been well maintained after removal of the pins and castthat the scaphoid and lunate were reduced anatomically (b)
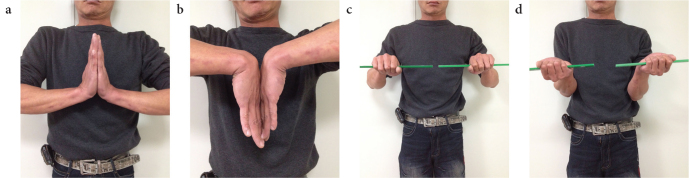
Figure 5. a–d.
Photographs show range of motion of wrist at the 1-year follow-up. There is almost full forearm extension, flexion, pronation, and supination
Figure 6. a–d.
Anteroposterior view (a). Lateral view (b). Radiographs show scapholunate joint space widening and a DISI deformity. MRI shows no avascular necrosis of any carpal bone (c)
DISI: dorsal intercalated segment instability
Discussion
This case report describes a male patient with palmar-divergent dislocation of the scaphoid and lunate who was treated using closed reduction and percutaneous pinning.
The mechanisms of scaphoid and lunate displacements, as a unit and palmar-divergent dislocation, most likely differ due to a diversified sequence of forces applied to the wrist joint at the time of injury. The forces could be associated with the differences in tearing of the major ligaments. In displacement with union, two major ligaments that require repair are the radioscaphocapitate (RSC) ligament and the lunotriquetral (LT) ligament. In palmar-divergent dislocation, three major ligaments that require repair are RSC, LT, and SL.
The optimal treatment course for these types of injuries has been discussed and indicated; however, the opinions are contrasting because of an insufficient number of reported cases. Previously, closed or open reductions with or without K-wire fixation were performed in most cases. Consequently, open reduction with K-wire pinning and interosseous ligament repair for perilunate dislocation had been recommended to prevent carpal instability (7, 8). Although ligament repair can prevent carpal instability, in some cases it leads to stiffness of the wrist joint. We speculate that stiffness may occur in cases with several injured ligaments and compromise the effectiveness of ligament repair. Various treatment methods for acute lunate and perilunate dislocations have been reviewed by Budoff (9).
The main aim of treatment is to achieve carpal stability. Therefore, the treatment targets the torn ligaments and aims to restore carpal stability. To avoid DISI in palmar-divergent dislocation, it is essential to repair and heal SL and RSC. The first, second, and third priority in surgical restoration is given to SL, RSC, and LT, respectively. Accordingly, closed reduction with two pins was used to perform fixation. The first pin was used to fix the scaphoid-lunate together, and the second pin was used to fix the radial styloid-scaphoid-capitate, thereby preventing carpal displacement during the ligament healing stage. In cases with palmar dislocation of the scaphoid and lunate as a unit, it is not usually required to fix the scaphoid and lunate because the SL ligament has not been torn. However, it might be necessary to fix the lunate and triquetrum ligament to prevent possible volar intercalated segment instability.
We used a modified pin-in-plaster technique to reinforce immobilization after reduction. The pin-in-plaster technique was effectively used previously to maintain reduction during bone healing in patients with distal radius fracture (10, 11). Moreover, Domeshek et al. used proximal row carpectomy and a volar plaster forearm splint to immobilize the wrist in patients with complete dislocation of the lunate and scaphoid (12). In the present case, the pin-in-plaster technique strengthens the fixation and provides reliable conditions to maintain accurate reduction through proper immobilization. Re-dislocation did not occur until the pins and cast were removed from the operated hand.
In the present case, the grip strength was approximately 85% on the injured side compared with that on the uninjured side. Furthermore, the patient had DISI deformity. The decrease in grip strength may be associated with DISI in patients with no interosseous ligament repair. A similar case was reported by Idrissi and Galiua (6). The patient was treated with closed reduction followed by percutaneous pinning and had DISI deformity at the 1-year follow-up.
In cases with palmar-divergent dislocation of the scaphoid and lunate, Baulot et al. and Komura et al. recommended repairing the interosseous ligaments by combined the palmar and dorsal approaches (3, 5). To prevent carpal instability, it was indicated to repair the volar and dorsal ligaments associated with stabilization of the entire carpus using SL, lunate-triquetrum, and capitate-lunate K-wire fixation. However, the results obtained during this method were not analyzed and compared with the results observed during surgery with closed reduction and percutaneous pinning. Notably, because of the unique blood supply in the wrist, there is a potential risk of avascular necrosis of the scaphoid or lunate in complicated perilunate dislocation with open reduction, especially in cases in which treatment was delayed (2, 13). In addition, ligament repair in perilunate dislocation may lead to joint stiffness with a decrease in ROM (5, 7). Therefore, closed reduction with percutaneous pinning is a better alternative in the treatment of this type of injury.
Conclusion
This case of palmar-divergent dislocation is similar to the six other reported cases of this type of injury. The cases differ mainly in the treatment method and outcomes. Our treatment method is relatively simple and easy to perform. Additionally, it does not require a long operation time. Importantly, a good outcome can be achieved using this method, including full ROM and freedom from pain. The only shortcoming of this treatment method is a slight reduction in grip strength.
To obtain even better treatment outcomes, we recommend that the pins and cast be removed after 8 weeks (instead of after 5 weeks, as was done in our case). This is to ensure that the tear in the SL ligament has been properly repaired to minimize the possibility of future SL dissociation, which can lead to DISI, resulting in joint pain and reduced grip strength.
HIGHLIGHTS.
Open reduction with K-wire pinning and interosseous ligament repair for perilunate dislocation had been recommended to prevent carpal instability in cases with delayed diagnosis.
We report a case with palmer divergent dislocation of scaphoid and lunate, treated with closed reduction followed by percutaneous pinning and pin-in-plaster technique.
Our treatment approach achieved good outcome and is relatively simple to perform. There was no evidence of avascular necrosis and scaphoid or lunate, no limitation in motion or intermittent wrist pain at follow up.
For even better treatment outcomes, we recommend that the pins and cast be removed after 8 weeks to ensure that the tear in the SL ligament has been properly repaired.
Footnotes
Informed Consent: Written informed consent was obtained from the patient who participated in this study.
Author Contributions: Concept - S.W.K., C.L.W.; Design - S.W.K., C.L.W.; Data Collection and/or Processing - S.W.K., I-C.C.; Analysis and/or Interpretation - S.W.K., I-C.C.; Literature Search - S.W.K., I-C.C.; Writing Manuscript - S.W.K., C.L.W.; Critical Review - C.L.W.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declare that this study has received no financial support.
References
- 1.Gordon SL. Scaphoid and lunate dislocation. Report of a case in a patient with peripheral neuropathy. J Bone Joint Surg Am. 1972;54:1769–72. doi: 10.2106/00004623-197254080-00019. [DOI] [PubMed] [Google Scholar]
- 2.Kupfer K. Palmar dislocation of scaphoid and lunate as a unit: case report with special reference to carpal instability and treatment. J Hand Surg Am. 1986;11:130–4. doi: 10.1016/S0363-5023(86)80120-4. [DOI] [PubMed] [Google Scholar]
- 3.Baulot E, Perez A, Hallonet D, Grammont PM. Scaphoid and lunate palmar divergent dislocation. Apropos of a case. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:265–9. [PubMed] [Google Scholar]
- 4.Kang HJ, Shim DJ, Hahn SB, Kang ES. Palmar divergent dislocation of scaphoid and lunate. Yonsei Med J. 2003;44:1091–3. doi: 10.3349/ymj.2003.44.6.1091. [DOI] [PubMed] [Google Scholar]
- 5.Komura S, Yokoi T, Suzuki Y. Palmar-divergent dislocation of the scaphoid and the lunate. J Orthop Traumatol. 2011;12:65–8. doi: 10.1007/s10195-011-0131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Idrissi KK, Galiua F. Palmar dislocation of scaphoid and lunate. Clin Pract. 2011;1:e87. doi: 10.4081/cp.2011.e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gomez Fernandez JM, Mendez López JM, Grau Galtés P, Caracuel Redondo F. Palmar scaphoid dislocation associated with dorsal perilunate dislocation. A case report and review of the literature. Rev Esp Cir Ortop Traumatol. 2013;57:140–4. doi: 10.1016/j.recote.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 8.D’arienzo M, Galvano N, Butera M, Siragusa F. Dissociated dislocation of the lunate and carpal bones: Case report. Austin J Musculoskelet Disord. 2015;2:1017. [Google Scholar]
- 9.Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am. 2008;33:1424–32. doi: 10.1016/j.jhsa.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 10.Chen CE, Juhn RJ, Ko JY. Treatment of distal radius fractures with percutaneous pinning and pin-in-plaster. Hand (N Y) 2008;3:245–250. doi: 10.1007/s11552-008-9093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirghasemi SA, Rashidinia S, Sadeghi MS, Talebizadeh M, Rahimi N. A prospective study of a modified pin-in-plaster technique for treatment of fractures of the distal radius. Bone Joint Res. 2015;4:176–80. doi: 10.1302/2046-3758.411.2000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Domeshek LF, Harenberg PS, Rineer CA, Hadeed JG, Marcus JR, Erdmann D. Total scapholunate dislocation with complete scaphoid extrusion: case report. J Hand Surg Am. 2010;35:69–71. doi: 10.1016/j.jhsa.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Coll GA. Palmar dislocation of the scaphoid and lunate. J Hand Surg Am. 1987;12:476–80. doi: 10.1016/S0363-5023(87)80028-X. [DOI] [PubMed] [Google Scholar]