Abstract
Supplemental digital content is available in the text.
SUMMARY
The COVID-19 pandemic has stressed all facets of healthcare delivery. Trauma centers serve as regional resource sites for high-acuity patients; so careful planning is required to maintain access to trauma care during an infectious pandemic. Guidance from the American College of Surgeons Committee on Trauma (ACS-COT) provides a general framework for the pandemic response, but these precepts must be contextualized to local and regional factors. The Level I trauma centers in Philadelphia collaborated to implement this guidance and to share insights throughout the early phase of the pandemic. For this report, we examined the volume, acuity, and mechanisms of presenting trauma patients and the number and acuity of COVID-19 admissions during the pandemic. We also assessed the geospatial relationship between firearm incidents and COVID-19 case density. Finally, we collated the collaborative measures taken to maintain trauma access and team safety and evaluated the effect of these measures.
Over the first 6 weeks of the pandemic, trauma contacts totaled 1,058 patients across all centers representing a 20% decrease compared with the same time last year. However, the number of penetrating trauma cases increased with a significant correlation between shooting locations and high-density COVID areas. During this time, Philadelphia trauma centers admitted a total of 1,413 confirmed COVID-19 patients, and 23% required mechanical ventilation. Divert status was activated for only 1.6% of available hours, and five of six centers remained open to all trauma transfers over the entire study period. Thus, through deliberate efforts to adapt ACS-COT guidelines and share lessons learned, the Level I trauma centers in Philadelphia maintained trauma access while simultaneously responding to the high-acuity infectious pandemic. This approach can be employed by other metropolitan areas and trauma systems to assure readiness during a prolonged crisis with large volumes of high-acuity trauma and nontrauma patients.
INTRODUCTION
On March 11, 2020 the World Health Organization declared a pandemic from the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2 or COVID-19).1 Although social distancing measures and travel restrictions likely reduced injury rates across the United States, penetrating trauma in some metropolitan centers, including Philadelphia, increased.2,3 For trauma centers already functioning near capacity, a surge of critically ill infectious patients posed two particular challenges—managing the competing demands on limited critical care space and other resources typically designated for trauma patients while simultaneously minimizing the risk of trauma team exposure to a transmissible disease. Indeed, trauma center access in one major metropolitan area was significantly compromised early in the pandemic from the surge of infectious patients.4 Concurrently, breakdowns in personal protective equipment (PPE) supply chains and rapidly changing guidance on PPE postures heightened anxiety among front-line personnel and required frequent reassessment by hospital leadership.5,6
Anticipating these challenges, the American College of Surgeons Committee on Trauma (ACS-COT) published guidelines for trauma center pandemic response.7 These were individually implemented by the Trauma Program Medical Directors (TMD) and Trauma Program Managers (TPM) of the four adult and two pediatric Level I trauma centers in Philadelphia. Based on the experience with COVID-19 in other international and domestic regions, we felt further compelled to coordinate care, maintain city-wide situational awareness, and ensure rapid sharing of evolving information.4,8,9 Thus, we initiated a weekly teleconference in which each center presented current COVID-19 and trauma patient census data, facility-level surge activities, current PPE postures, and clinical lessons learned from managing COVID-19 patients as the pandemic spread across our region (Fig. 1). The following report describes our experience during the early phase of this pandemic and outlines the measures we undertook to maintain trauma center access and trauma team safety while also caring for other critically ill patients.
Figure 1.
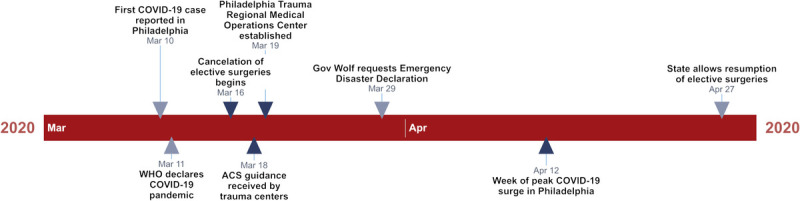
Timeline of significant COVID-19 pandemic events and response by the Philadelphia Level I trauma centers.
METHODS
A data collection tool was created with input from all sites and was distributed using the Research Electronic Data Capture (REDCap) platform hosted by the University of Pennsylvania. Institutional Review Board review was performed at each participating site, and submission of aggregated de-identified data was determined to be exempt. Trauma center activity was queried from March 9 to April 19, 2020 (COVID) and compared with the same period in 2019 (baseline). Trauma volume and acuity was assessed by activation level (highest level [alerts], all others), mechanism (penetrating, all others), and center type (adult, pediatric). Resource utilization and availability was assessed by trauma bay intubation, transfused patients and blood product utilization, and length of stay (LOS) in the emergency department (ED) for trauma patients admitted to an intensive care unit (ICU). Subgroups of animal bites and pediatric nonaccidental trauma and were also examined. To evaluate for an association between the incidence of shooting events and COVID-19 density across the city, we accessed anonymized crime data and COVID-19 infection rates by ZIP code through OpenDataPhilly (https://www.opendataphilly.org/).
Results from each center were collated and reviewed by two authors (Z.Q. and J.W.C.). Aggregate numbers were assessed with descriptive statistics and trends were evaluated in a pairwise fashion by center. Summary numbers between 2019 and 2020 were compared using χ2 or Fisher's exact test, and center-level numbers were compared over time with repeated measures using the Wilcoxon signed-rank test. Correlation between shooting locations and COVID-19 density was assessed with the Wilcoxon-Mann-Whitney test. A two-tailed difference of p < 0.05 was considered statistically significant. Data analysis was performed with R 3.5.2 (The R Foundation for Statistical Computing, https://www.r-project.org/).
RESULTS
Trauma Contacts During the COVID-19 Pandemic
Total trauma contacts across Philadelphia decreased from 1,328 at baseline to 1,058 in the COVID period (net −20.3%, Table 1). Conversely, the proportion of trauma alerts increased across the city (29.1% baseline vs. 34.5% COVID, p = 0.006) due to an increase in both the absolute number (233 vs. 251) and proportion of penetrating trauma patients (17.5% vs. 23.7%, p < 0.001, Table 1). By individual trauma center, median total trauma contacts decreased from 244 (interquartile range [IQR], 138–272) at baseline to 190 (89–238) in the COVID period (p = 0.036) (Table 1, Fig. 2) while the proportion of penetrating trauma increased from 15.4% (6.8%–23.3%) at baseline to 19.7% (11.5%–30.1%) (p = 0.031) in the COVID period (Fig. 2). When examining adult-only centers separately, the significant increase in the number and proportion of penetrating trauma persisted (Table 1) while there was no increase in the number or rate of penetrating injuries in the pediatric centers. Likewise, there was no change in the number or proportion of animal bites or pediatric nonaccidental trauma.
TABLE 1.
Aggregate Trauma Volume
| Total Volume | By Center | |||||
|---|---|---|---|---|---|---|
| Baseline | COVID | p | Baseline | COVID | p | |
| Total contacts | 1,328 | 1,058 | 244 (138–272) | 190 (89–238) | 0.036 | |
| Alerts | 387 (29.1) | 365 (34.5) | 0.006 | 42 (9–96) | 37 (10–103) | 0.674 |
| Penetrating | 233 (17.5) | 251 (23.7) | <0.001 | 37 (11–59) | 35 (12–65) | 0.419 |
| Animal bites | 10 (0.8) | 4 (0.4) | 0.357 | 1 (1–3) | 1 (0–1) | 0.362 |
| N-A trauma | — | — | — | — | — | — |
| Trauma bay intubation | 55 (4.1) | 57 (5.4) | 0.183 | 9 (3–15) | 11 (6–13) | 0.396 |
| Transfused patients | 86 (6.5) | 69 (6.5) | 1 | 15 (5–22) | 10 (4–16) | 0.584 |
| ED LOS (minutes) | — | — | — | 206 (176–241) | 190 (149–238) | 0.313 |
| Adult only | ||||||
| Total contacts | 1,111 | 939 | 269 (254–293) | 232 (205–262) | 0.125 | |
| Alerts | 383 (34.5) | 359 (38.2) | 0.086 | 83 (50–129) | 86 (44–132) | 0.625 |
| Penetrating | 225 (20.3) | 241 (25.7) | 0.004 | 57 (44–69) | 58 (38–80) | 0.625 |
| Animal bites | 6 (0.5) | 2 (0.2) | 0.302 | 1 (1–2) | 1 (0–1) | 0.371 |
| N-A trauma | — | — | — | — | — | — |
| Pediatric only | ||||||
| Total contacts | 217 | 119 | 108 (108–109) | 60 (57–62) | 0.500 | |
| Alerts | 4 (1.8) | 6 (5.0) | 0.189 | 2 (2–3) | 3 (2–4) | 1 |
| Penetrating | 8 (3.7) | 10 (8.4) | 0.113 | 4 (3–6) | 5 (4–6) | 1 |
| Animal Bites | 4 (1.8) | 2 (1.7) | 1 | 2 (1–3) | 1 (1–2) | 1 |
| N-A Trauma | 29 (13.4) | 21 (17.6) | 0.371 | 15 (12–17) | 11 (6–15) | 0.500 |
Total volume represents all trauma patients managed from 1/1 to 4/19 in the contributing centers combined. Numbers shown as n (%) or median (IQR). Adult only represents n = 4 centers; pediatric only includes n = 2 centers. ED LOS is calculated for patients admitted from the trauma bay to the ICU. N-A Trauma, nonaccidental trauma.
Figure 2.
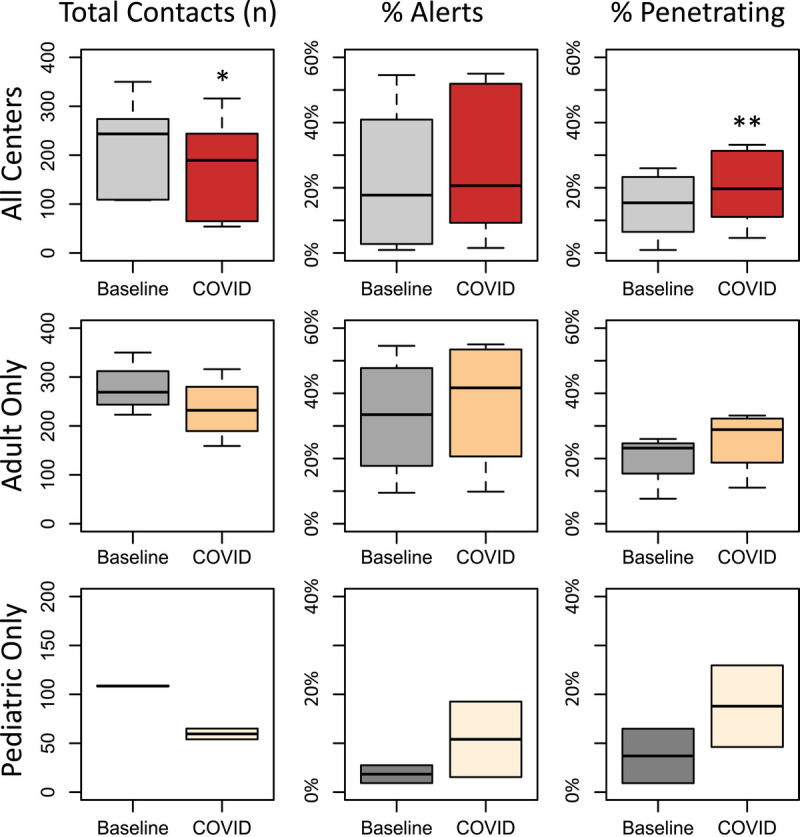
Philadelphia Level I trauma activity by center March 9, 2019 to April 19, 2019 (Baseline) vs. March 9, 2020 to April 19, 2020 (COVID). The median is shown (line) with interquartile range (IQR, shaded box); whiskers represent 1.5 times the IQR. * p = 0.036, ** p = 0.031, all others p ≥ 0.05.
Trauma bay intubations, number and proportion of transfused patients, and ED LOS did not change significantly during the COVID period compared with baseline (Table 1). However, the median number of packed red blood cells per transfused patient decreased from 3 to 2 (Supplemental Digital Content, Table 1, http://links.lww.com/TA/B730). There was no difference in number of units of fresh frozen plasma, platelets, or whole blood units transfused.
Shooting Events During the COVID-19 Pandemic
To further assess the observed increase in penetrating trauma, we compared locations of 187 individual shooting events in Philadelphia during the pandemic to the distribution of confirmed COVID-19 infections by ZIP code, adjusted for population (Fig. 3). High-density COVID ZIP codes had significantly more shootings per 10,000 individuals compared with low-density COVID ZIP codes (1.3 [0.6–1.8] vs. 0.4 [0–1.2], p = 0.022) (Fig. 3, inset).
Figure 3.
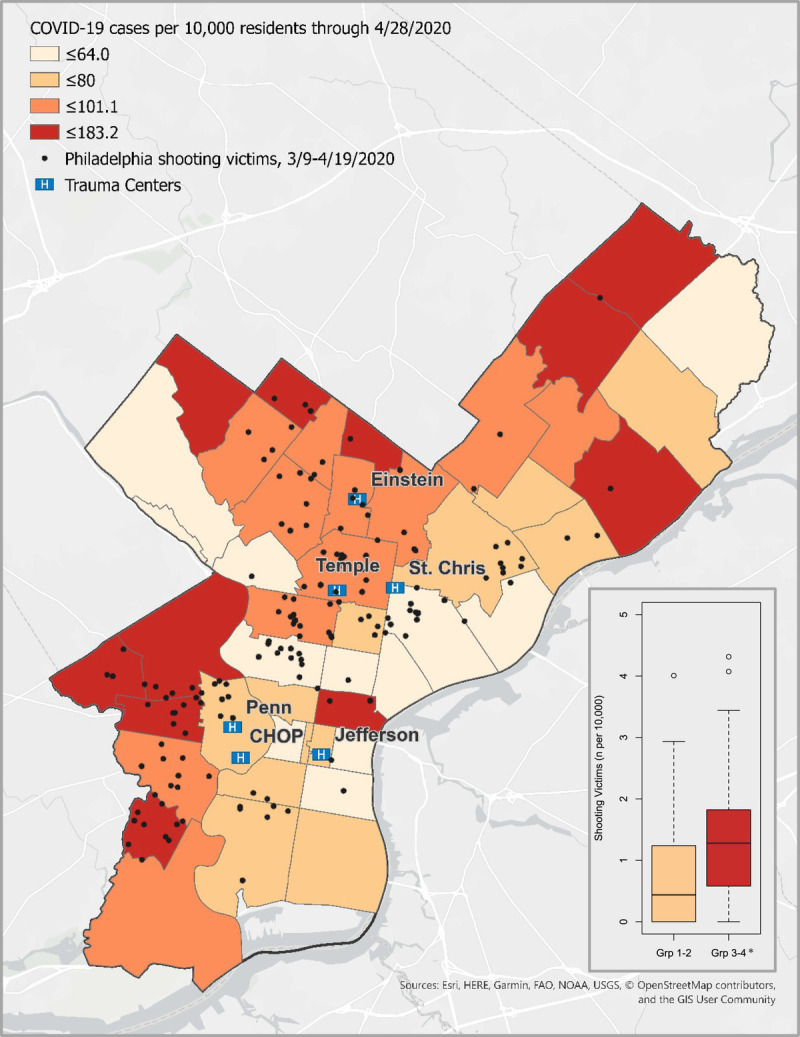
Shooting event locations (filled circles) superimposed on a heatmap of confirmed COVID-19 cases by ZIP code (density per 10,000 population). Inset shows shooting victim numbers (per 10,000 population) by the lowest and highest COVID-19 density groups (groups 1 and 2 vs. groups 3 and 4). The median is shown (line) with interquartile range (IQR, shaded box); whiskers represent 1.5 times the IQR and unfilled circles are outliers. *p = 0.022.
Trauma Center Access
During the COVID period, four of six Level I trauma centers in Philadelphia did not go on trauma divert. Total trauma divert time during the pandemic response was 95 hours across all centers (1.6% of available time). The longest divert period was due to a COVID-19 exposure in an ICU setting that depleted available trauma-qualified personnel. This same event also forced this center to temporarily close to trauma transfers. The other five trauma centers remained opened to trauma transfers of all acuity levels from referring hospitals throughout the COVID period.
Trauma Center Modifications During the Pandemic Response
During the COVID period, Philadelphia trauma centers admitted a total of 1,413 confirmed COVID-19 patients (including seven trauma patients) with 234 (22.9%) requiring mechanical ventilation (Table 2). In anticipation of this surge of critically ill COVID-19 patients in parallel with the continued high-acuity trauma volume in our city, our Level I trauma centers and trauma programs individually implemented a number of structural and operational changes to maintain trauma access and to protect our trauma team members (Table 3).
TABLE 2.
Aggregate COVID Volume
| Total Volume | By Center | |
|---|---|---|
| COVID admits | 1,413 | 306 (102–340) |
| COVID vents | 324 (22.9) | 66 (17–81) |
| Adult only | ||
| COVID admits | 1,349 | 330 (309–359) |
| COVID vents | 319 (23.6) | 79 (69–89) |
| Pediatric only | ||
| COVID admits | 64 | 32 (30–34) |
| COVID vents | 5 (7.8) | 3 (2–3) |
Total volume represents all confirmed COVID patients managed in the contributing centers combined. Numbers shown as n (%) or median (IQR).
TABLE 3.
Summary of Pandemic Response Across Philadelphia Trauma Centers
| Workforce Planning |
| Integrate trauma representative into Incident Command Structure |
| Meet weekly with regional TMDs and TPMs |
| Train nontrauma general surgeons to augment critical care services |
| Expand anesthesia role to support Emergency Department intubations |
| Streamline trauma teams to balance clinical coverage while minimizing exposure |
| Activate reserve team members as needed to support high-volume clinical activity and to backfill staff quarantining/illness |
| Integrate telemedicine into bedside rounds and specialty consults with limitation of in-person visits to essential assessments (e.g. tertiary survey) |
| Dedicated teams perform high-demand procedures (e.g. vascular access, tracheostomy) |
| Trauma Bay and Resuscitation Changes |
| Screen and/or test patients for COVID-19 during intake and trauma resuscitation |
| Add physical barriers to isolate bays |
| Designate specific bays for use by COVID-confirmed or suspected patients |
| Convert patient assessment areas to negative-pressure if possible |
| Designate specific areas for donning and doffing of PPE |
| Remove unnecessary equipment |
| Limit personnel in the trauma bay to essential personnel only |
| Perform critical procedures by most experienced care team member |
| Perform AGPs (including intubation) in the trauma bay prior to transport |
| Employ in situ simulation to reinforce workflow and procedural changes |
| Radiology Protocols |
| Limit imaging to decision-critical studies as much as possible |
| Examine for findings consistent with COVID-19 infection on chest imaging |
| Operating Room Changes |
| Transport to OR by most direct route with staff in appropriate PPE |
| Designate specific operating room(s) with negative-pressure capability for COVID-confirmed or suspected patients |
| Convert existing ORs to negative-pressure capability if possible |
| Minimize personnel traffic in the OR |
| Designate “clean” runners outside the OR to obtain needed equipment and supplies |
| Consider reconfiguring OR rooms to augment PACU/ICU capacity |
| Operating and anesthesia team members wear appropriate PPE during AGPs |
| Blood Product Utilization |
| Collaborate with national organizations (e.g., American Red Cross) to sponsor blood donation drives |
| Limit nonemergent transfusions to preserve supply |
| Limit use of rare blood types |
| Education and Training of Housestaff |
| Convert educational and working conferences to teleconference format |
| Incorporate housestaff into procedural teams to maintain and bolster technical skills |
| Record and disseminate in-situ simulation for training |
CME, continuing medical education; GME, graduate medical education.
These changes fell broadly in line with both ACS guidance and recommendations based upon experiences of other national and international centers7,9–13: ensuring trauma surgery presence in the health system incidence command system; canceling elective surgery and ambulatory clinics; altering workforce to both limit unnecessary exposure and allow maintenance of a functional trauma and critical care service; modifying trauma resuscitation bay and operating room (OR) configurations; incorporating PPE guidance; ensuring adequate and appropriate blood supply and use; and continuing the educational mission for housestaff at individual centers (incorporating both videotaped simulation and teleconferencing).14–21 Implementing these changes required a large time investment by both TMDs and TPMs. Trauma Program Medical Directors spent an average of an additional 10 hours while TPMs spent an additional 8 hours per week on these issues. In total, TMDs and TPMs invested an estimated 612 person-hours (approximately 2.5 administrative full-time equivalents) on these activities across all centers throughout the COVID period.
To further address the unprecedented threat from the pandemic, our centers quickly established a broader regional virtual working group to assist in maintaining trauma center readiness. This allowed a unique forum to maintain our situational awareness and to adapt and coordinate our response. Specific examples of this coordinated response are enumerated in the following paragraphs.
Augmenting Adult Trauma Center Capacity Through Use of Pediatric Centers
Philadelphia has two Level 1 pediatric trauma centers that typically do not accept patients over the age of 19 years. We developed a plan to transfer younger adults (age, 17–25 years) to the pediatric trauma centers as needed. This agreement created a virtual buffer for our adult centers that would facilitate continued trauma access for activations and transfers-in should capacity be reached or exceeded. Any patients transferred to pediatric centers would have potentially benefitted from a more permissive visitation strategy and additional social work resources.
Modifications to Trauma Airway Management
During these teleconferences, we specifically addressed optimal trauma airway management—a significant risk to personnel as an aerosol-generating procedure (AGP)—and the need to anticipate multiple patients requiring intubation in a short period.22–24 To ensure both first-pass intubation success and to minimize exposure, all centers designated the most experienced staff to perform these high-risk procedures. Nonessential personnel were asked to step away during intubation to minimize aerosol exposure. Furthermore, one center preferentially intubated patients in the trauma bay prior to transport to the OR in an attempt to minimize aerosolization. This represented a significant change from prior practice of deliberately delaying intubation until arriving in the OR to permit time for volume resuscitation.25
To prepare for potential intubation surges, two centers augmented ED airway teams with anesthesia back-up. This required rapid education and team training to ensure role readiness.
Adapting Ventilator Equipment
The COVID-19 pandemic resulted in a large volume of critically ill patients requiring mechanical ventilation. Both international and U.S. reports signaled the possibility of a shortage of traditional ventilators, prompting our centers to closely track ventilator inventory and to explore novel ventilator approaches.26 During our regional group meetings, we discussed practical aspects of using anesthesia and BIPAP machines as ventilators.27 Focused education allowed our trauma surgeons, not typically trained on these machines, to safely utilize them if required. Group members also related considerations for converting ORs and postanesthesia care units (PACU) to critical care space.
Personal Protective Equipment and Infection Control
The Centers for Disease Control and Prevention's recommendations for the use of PPE were discussed during the teleconference and implemented by all centers to the extent possible based on available resources (Supplemental Digital Content, Table 2, http://links.lww.com/TA/B730).17 Significant challenges in PPE implementation arose from national supply chain disruptions and frequent updates to the guidance driven by an evolving understanding of disease transmission and lessons learned through international and national reports. Aerosol-generating procedures in particular generated significant discussion among our group. While intubation represented an obvious AGP, we also felt critical resuscitative procedures (e.g., tube thoracostomy and thoracotomy) and operative techniques (e.g., laparoscopy) had significant potential of generating aerosol and hence required specific PPE guidance.28,29
The national shortage of PPE also led us to discuss mechanisms to preserve existing supplies at individual centers. Options included extended use and cycling of N95 masks and the use of ultraviolet light for N95 mask disinfection.30 These challenges notwithstanding, no trauma bay personnel or airway team members were reported to have been exposed or infected at any center.
Guideline Development
We recognized head and neck-based trauma consultation and tracheostomy as high risk exposures that warranted specific attention during our weekly teleconference. Facial and neurosurgical trauma cases posed significant risk of COVID-19 transmission.31,32 Thus, a clinical pathway for teleconsultation by the Oral/Maxillofacial Surgery, Ophthalmology, Otorhinolaryngology, and Neurosurgical services was developed by one center and relayed to the other participating sites. This approach listed indications for required in-person assessment while all other consults could be performed remotely. The attending surgeon reserved the right to request an in-person consult if this was deemed necessary.
Similarly, a pathway for tracheostomy performance was developed at one center and relayed to the other sites prior to publication.33 This pathway was developed by a multidisciplinary team of advanced airway experts who considered both the optimal timing and technique for tracheostomy insertion that balanced the benefits of tracheostomy placement with the potential for staff exposure during this AGP.
Radiology Use
We also discussed mechanisms to maintain access to radiology resources during the pandemic.34 All centers identified the need to adhere to predetermined evidence-based protocols to streamline radiology usage but did not ultimately note a significant change in use of radiology resources. Close communication between senior trauma and radiology physicians was found to be useful at one center. Another center reported limited imaging studies to patients with a high probability for injuries while also allowing only essential personnel in the radiology viewing room. Two centers reported automatic reporting of findings on chest imaging suspicious for COVID-19 infection.
Inpatient Care Activities
In addition to increased administrative responsibilities, TMDs maintained a clinically ready posture during the pandemic. All were available to cover gaps that may have developed with the surge in demand for critical-care trained physicians or from staff exposures resulting in quarantine measures. Clinical service time varied among TMDs, with two reporting increasing service time over their original scheduled hours, while others reported either no change or a decrease due to team consolidation. In some cases, TMDs also provided significant clinical coverage time for medical ICU patients (including COVID patients) in geographic areas outside of traditional ICUs such as the PACU.
Four centers reported COVID-positive trauma patients being managed on nontrauma floors. This stemmed from cohorting policies and efforts to free-up high-acuity critical care beds in trauma-designated ICUs. No unanticipated patient-level complications resulted from these practices as trauma teams and trauma-trained nurses cared for these patients in all cases. However, one center reported inadvertent exposure of multiple surgical trauma team members when an initial false-negative COVID test prompted transfer of the patient from a COVID unit to the trauma floor and removal of droplet precautions.
DISCUSSION
The COVID-19 pandemic has challenged the trauma centers in our city much like an unrelenting mass-casualty incident. During the 6 weeks following declaration of the pandemic, although overall trauma volume decreased by approximately 20%, the number and proportion of penetrating trauma increased significantly. This resulted in a continued influx of high-acuity severely injured patients in parallel with the surge of critically ill COVID-19 patients.
The high rate of interpersonal violence observed during the pandemic mirrors the experience of other metropolitan centers such as Chicago, Houston, San Antonio, and Dallas (Supplemental Digital Content, Table 3, http://links.lww.com/TA/B730) and is likely multifactorial. Possible contributing factors include increased unstructured time, a surge in gun sales, and the significant socioeconomic impact of the pandemic resulting in higher unemployment.35 Through geospatial mapping, we further found a significant relationship between the incidence of shooting events in city neighborhoods most affected by COVID-19 infections. An association between race and both COVID-19 incidence and severity has been documented36 while the geospatial relationship identified in our study suggests the social determinants of health contributing to high viral concentration likely also correlate with endemic violence. Many of the highest-density ZIP codes represent neighborhoods that have suffered from poor socioeconomic conditions in the city, and these neighborhoods feed into two of the adult centers and one pediatric center that most accounted for the increased number and proportion of penetrating trauma. Further investigation is warranted so that insights gleaned can be used to address both of these public health emergencies.
Our experience also highlights the importance of maintaining trauma center access and readiness during infectious pandemics. The dynamic early phase was filled with rapidly changing information, sometimes on an hourly basis. While single-center adaptation based on national guidance is important, we found the pandemic presented a unique opportunity to develop a close collaboration across our city's level 1 trauma centers. Cities such as New York City and Seattle saw an early patient surge and were able to provide members of our group key information (through both personal communication and published literature) that we could rapidly adapt to assure optimal care for all patients in the face of high demand for limited resources. We feel siloed adoption could have delayed our city-wide preparations and response and led to patient or staff harm. The value of this collaboration was demonstrated in the rapid and consistent dissemination of information across trauma centers and in the readiness of centers to help one another, as needed, to maximize trauma access throughout the pandemic.
As we move to a new “normal,” including the reestablishment of elective surgery, we will need to maintain this posture to manage the expected rise in trauma over the summer months alongside the ill-defined threat of COVID-19 resurgence. To this end, we will continue this frequent touchpoint. Furthermore, each represented medical system will integrate this city-wide trauma collaboration into their disaster plans via the Incident Command System representative.
We acknowledge several limitations to this report. First, we did not include data from the Level II trauma centers in our city and region. These centers play an essential role in the overall trauma response in our area; so future system-level assessments should include these centers. In addition, Hahnemann University Hospital closed in September 2019, and data from this Level I center was not available for this analysis. Finally, our data collection focused on results readily available in each center's trauma registry, publicly available shooting data, and subjective self-reporting of center-level pandemic responses. This limited focus may have inadvertently excluded significant systems-level issues that might have impacted trauma care delivery during the pandemic and social determinants of health underpinning our findings.
CONCLUSION
In the initial 6 weeks of the COVID-19 pandemic, although overall trauma volume in Philadelphia decreased, the number and proportion of penetrating trauma increased. This continued high volume and acuity of trauma patients, in addition to the large volume of critically ill COVID-19 patients, placed significant strain on our individual hospitals. But by embracing and adapting national guidance to meet our local needs and by deliberately sharing lessons learned across health systems, we maintained trauma access throughout the city during this dynamic, early period of the pandemic. Such an approach may help other centers and regions prepare for future simultaneous surges in both critically ill and critically injured patients.
AUTHORSHIP
Z.Q., M.J.K., and J.W.C. conceived this study to which all authors gave input. Z.Q. and J.W.C. designed the data collection tool. E.K. obtained geospatial data and performed the mapping. J.W.C. and Z.Q. had access to all the data. J.W.C. performed the analysis. Z.Q. and J.W.C. drafted the initial manuscript which all authors critically revised and approved.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the invaluable encouragement of many family and friends during this unique time. Your kind words and expressions of gratitude were much appreciated. We also thank members of the U.S. Army Reserve who provided both prehospital and inpatient care in the Philadelphia area as part of the national pandemic response.
Funding: The authors received no financial or in-kind support for this work.
DISCLOSURE
The authors declare no conflicts of interest related to this work.
Footnotes
Published online: June 29, 2020.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
REFERENCES
- 1.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19. Updated March 11, 2020. Accessed April 24, 2020.
- 2.Hatchimonji JS, Swendiman RA, Seamon MJ, Nance ML. Trauma does not quarantine: violence during the Covid-19 Pandemic. Ann Surg. 2020. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dean MM. Two killings in Philadelphia on Thursday raise city's total to 120 for the year—18% more than a year ago. Philadelphia Inquirer. 2020. Available at: https://www.inquirer.com/news/tahj-williams-philadelphia-police-homicide-sekou-kinebrew-gunshots-southwest-corner-store-20200424.html Accessed April 25, 2020. [Google Scholar]
- 4.Bank M, O'Neill P, Prince J, Simon R, Teperman S, Winchell R. Early report from the greater New York chapter of the American College of Surgeons Committee on Trauma on the COVID-19 crisis. 2020. Available at: https://www.facs.org/-/media/files/covid19/nyc_chapter_acs_cot_covid19_crisis.ashx. Accessed April 24, 2020.
- 5.Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382(18):e41. [DOI] [PubMed] [Google Scholar]
- 6.Livingston E, Desai A, Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons Committee on Trauma Maintaining trauma center access and care during the COVID-19 pandemic: guidance document for trauma medical directors. https://www.facs.org/covid-19/clinical-guidance/maintaining-access. Updated March 20, 2020. Accessed April 24, 2020.
- 8.Kurihara H, Bisagni P, Faccincani R, Zago M. COVID-19 outbreak in Northern Italy: viewpoint of the Milan area surgical community. J Trauma Acute Care Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 9.Stewart RM, Bulger EM, Epley E, Mitchell SH. How to set up a regional medical operations center to manage the COVID-19 pandemic. 2020. Available at: www.facs.org/covid-19/clinical-guidance/rmoc-setup. Accessed May 13, 2020.
- 10.Brindle M, Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coimbra R Edwards S Kurihara H, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020;46(3):505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ross SW, Lauer CW, Miles WS, Green JM, Christmas AB, May AK, Matthews BD. Maximizing the calm before the storm: tiered surgical response plan for novel coronavirus (COVID-19). J Am Coll Surg. 2020;230(6):1080–1091.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zarzaur BL, Stahl CC, Greenberg JA, Savage SA, Minter RM. Blueprint for restructuring a department of surgery with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. Epub 2020 Apr 14. [DOI] [PubMed] [Google Scholar]
- 14.Society of Critical Care Medicine COVID-19 ICU preparedness checklist. https://www.sccm.org/Disaster/COVID-19-ICU-Preparedness-Checklist Updated April 13, 2020. Accessed April 24, 2020.
- 15.Livingston DH, Bonne S, Morello C, Fox A. Optimizing the trauma resuscitation bay during the COVID-19 pandemic. Trauma Surg Acute Care Open. 2020;5(1):e000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020;67(6):756–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Updated April 13, 2020. Accessed April 17, 2020.
- 18.American Association of Blood Banking Statement on coronavirus and blood donation. http://www.aabb.org/advocacy/regulatorygovernment/Pages/Statement-on-Coronavirus-and-Blood-Donation.aspx updated April 6, 2020 Accessed April 24, 2020.
- 19.Shander A Goobie SM Warner MA, et al. Essential role of patient blood management in a pandemic: a call for action. Anesth Analg. 2020;131(1):74–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Almazrooq Z, Lopes M, Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in gradual medical education. J Am Coll Cardiol. Epub 2020 Apr 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buljac-Samardzic M, Doekhie KD, van Wijngaarden JDH. Interventions to improve team effectiveness within health care: a systematic review of the past decade. Hum Resour Health. 2020;18(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of anaesthetists. Anaesthesia. Epub 2020 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Au Yong PS, Chen X. Reducing droplet spread during airway manipulation: lessons from the COVID-19 pandemic in Singapore. Br J Anaesth. 2020;125(1):e176–e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mareiniss DP. The impending storm: COVID-19, pandemics and our overwhelmed emergency departments. Am J Emerg Med. 2020;38(6):1293–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dumas RP, Jafari D, Moore SA, Ruffolo L, Holena DN, Seamon MJ. Emergency department versus operating suite intubation in operative trauma patients: does location matter? World J Surg. 2020;44(3):780–787. [DOI] [PubMed] [Google Scholar]
- 26.Johns Hopkins Center for Health Security Ventilator stockpiling and availability in the U.S. http://www.centerforhealthsecurity.org/resources/COVID-19/200214-ventilatoravailability-factsheet.pdf. Updated April 1, 2020. Accessed May 22, 2020.
- 27.American Society of Anesthesiologists APSF/ASA guidance on repurposing anesthesia machines as ICU ventilators. https://asahq.org/in-the-spotlight/coronavirus-covid-19-information/purposing-anesthesia-machines-for-ventilators. Updated May 7, 2020. Accessed May 22, 2020.
- 28.Pieracci FM, Burlew CC, Spain D, Livingston DH, Bulger EM, Davis KA, Michetti C. Tube thoracostomy during the COVID-19 pandemic: guidance and recommendations from the AAST Acute Care Surgery and Critical Care Committees. Trauma Surg Acute Care Open. 2020;5(1):e000498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coccolini F, Tartaglia D, Puglisi A, Giordano C, Pistello M, Lodato M, Chiarugi M. SARS-CoV-2 is present in peritoneal fluid in COVID-19 patients. Ann Surg. Epub 2020 May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cadnum JL, Li DF, Redmond SN, John AR, Pearlmutter B, Donskey CJ. Effectiveness of ultraviolet-C light and a high-level disinfection cabinet for decontamination of N95 respirators. Pathog Immun. 2020;5(1):52–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Givi B Schiff BA Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 32.Spina A, Boari N, Gagliardi F, Bailo M, Calvanese F, Mortini P. Management of neurosurgical patients during the COVID-19 pandemic. World Neurosurg. 2020;S1878-8750(20):30870–30876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao TN, Braslow BM, Martin ND, Chalian AA, Atkins JH, Haas AR, Rassekh CH. Tracheotomy in ventilated patients with COVID-19. Ann Surg. Epub 2020 May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nasir MU Roberts J Mullen NL, et al. The role of emergency radiology in COVID-19: from preparedness to diagnosis. Can Assoc Radiol J. 2020; 846537120916419. [DOI] [PubMed] [Google Scholar]
- 35.Collins K, Yaffe-Bellany D. About 2 million guns were sold in the U.S. as virus fears spread. New York Times. 2020. Available at: http://www.nytimes.com/interactive/2020/04/01/business/coronavirus-gun-sales.html Accessed May 13, 2020. [Google Scholar]
- 36.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. [DOI] [PubMed] [Google Scholar]


