Although acute care surgery practice might not be on the frontline of COVID-19 patients care, its activity has been heavily affected by the pandemic.1 During the outbreak, the surgical overall workload has decreased, and this has proven true for surgical emergencies as well. Still, acute care surgeons had to deal with surgical emergencies in COVID-19–positive, as well as suspected or negative patients, with the responsibility to ensure an effective care even in a setting overwhelmed by a number of patients primarily affected by nonsurgical respiratory disorders. In this scenario, logistics are crucial to create a safe environment for both health care professionals and acute surgical patients and to limit the spread of this highly infective disease.2 So far, Italy is the second country for the number of COVID-19–infected patients and the first in Europe experiencing the emergency outbreaks.3 The cataclysmic outbreak of COVID-19 infection and related mortality impaired the availability of hospital resources (intensive care unit beds, ventilators, blood products, health care workers) and raised the need to reorganize hospital pathways and procedures. Moreover, it exerted a deep impact on emergency and trauma surgery centers: acute care surgeons have been often shifted to COVID-19 patients care teams and had to change their standard activity, especially to reduce the risk of spreading the infection among operators and patients.4,5
In Italy, the central national government guidelines issued to respond to COVID-19 flare-up have been differently applied to hospital activities on a local basis, according to the different impact and timing of the outbreak in each region. Lazio region had 7,627 COVID-19 confirmed cases and 684 COVID-19–related deaths so far. To optimize patients load and pathways, a COVID-19–dedicated Hub-and-Spoke network has been built, resembling the regional trauma system. Our hospital is an academic/teaching hospital and an emergency and major trauma hub located in an urban area accounting for 2,000,000 inhabitants. Overall, from the beginning of the emergency, our institution took care of 689 COVID-19–positive patients of 3,200 suspected ones admitted with fever.
Despite mass casualty, simulations are routinely performed in our institution, the extraordinary COVID-19 outbreak represented a big challenge. For this reason, we would like to share our experience with the hope that it may be of help in setting up a dedicated emergency operating room (OR).
GENERAL REORGANIZATION
Early at the beginning of the outbreak, we felt that a multidisciplinary effort had to be provided to ensure an integrated hospital response and an effective communication with the regional command center. A permanent task force was activated, involving administrative and health officials as well as infectious diseases specialists and representative operators from the key hospital services: OR nurses, emergency department (ED) nurses and physicians, acute care surgeons, and leaders from the main elective operative units. The task force was organized into working groups. After receiving the key information on viral transmission modalities and protection issues, the emergency surgery working group started creating the basic protocols for health professionals' protection in the OR and patients' flow from the ED to the OR. This early phase has been demanding in terms of integration between the COVID-19 diagnostic pathways, coordinated by ED physicians, and the surgical pathways, managed by acute care surgeons.
As a result, soon after becoming a COVID-19 hub, our hospital reorganized both the surgical emergency block and the patients pathway from the emergency room to the OR (Fig. 1).
Figure 1.

Patient entry area in the emergency room, in red COVID19 pathways.
ELECTIVE PROCEDURES LOCKDOWN AND PATIENT FLOW REORGANIZATION
As with the surgical activity concerns, we canceled all elective procedures except for nonpostponable cancer surgery while preserving all surgical emergencies. All patients with fever or symptoms consistent with the suspicion of COVID-19 are admitted to specific “buffer” wards and observed until a definitive diagnosis is reached by means of computed tomography (CT) scan and/or oropharyngeal swab. If positive, they are transferred to a dedicated but mixed medical/surgical COVID-19 ward. If negative, they are moved to a standard surgical ward. All patients needing an emergency surgery procedure undergo a preoperative screening chest CT scan instead of the routine chest x-ray (Fig. 2). Three percent of the surgical candidates with nonrespiratory symptoms who had a negative chest CT scan finally had a positive nasopharyngeal swab, thus accounting for the so-called asymptomatic COVID-19 cases. For this reason, we early decided to treat surgical red code emergency and major trauma patients under maximal COVID-19 precautions (including OR) until proven negative.
Figure 2.

CT scan area, in red dedicated COVID19 CT.
SURGICAL BLOCK REORGANIZATION
The emergency surgical block has been dedicated to treat only suspected/confirmed COVID-19 patient (Fig. 3). Two operating theaters in the elective general surgery block have been shifted to host all conventional surgical emergencies. Before the arrival of the suspected/confirmed COVID-19 patient, the dedicated OR must be prewarned. The patient, mandatorily wearing a surgical mask, enters directly in the OR when all the material necessary for surgery has been prepared and when the dedicated staff is ready.
Figure 3.
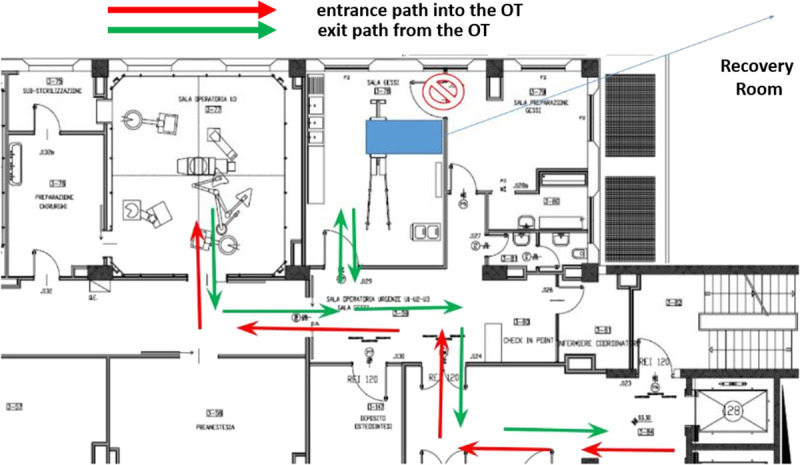
Layout of COVID-19 OR with patient entrance and exit route.
PERSONAL PROTECTION EQUIPMENT
Specific personal protection equipment (PPE) kits necessary for the entire surgical and anesthetic team (surgeons, anesthesiologist, nurses) are always available in the OR.
At the beginning of the pandemic, these kits were prepared taking into account an early shortage of PPE (especially FFP2 and FFP3 masks) that compelled us to downgrade our safety criteria: surgical mask for the surgeon and the scrub nurse, at least FFP2 (and FFP3 when available) mask for the operators at higher risk of infection due to aerosol-generating procedures, that is, the anesthesiologist and the anesthesia nurse. We did not state a minimum time after patient intubation safe enough to consider airborne spread at low risk and to allow less protected workers enter the OR, as no information were available in the literature. As soon as local devices availability changed, we upgraded the PPE kit with at least FFP2 masks for all the OR staff and FFP3 for the two operators exposed to aerosol-generating procedure. Despite this, early shortage of advanced PPEs, such as FFP2 and FFP3 masks, lasted for 2 weeks, only one operator among the OR staff has been infected by COVID-19 so far.
STRUCTURAL ADJUSTMENTS IN THE SURGICAL BLOCK
Moreover, we changed the ventilation system in the OR, opting for a negative pressure ventilation system similar to the intensive care unit (ICU) setting with the aim of containing the virus spread outside the “dirty” environment. During the surgical procedure, the OR doors must be kept closed, and the staff cannot leave the room. For this reason, we involved a staff unit to provide any material trough an “auxiliary window” without altering the setting (Fig. 1).
To limit cross-contamination between “clean” and “dirty” environments and operators, communication between the in-theater staff and the assisting staff outside the OR is provided via a walkie-talkie system previously setup for the mass casualty hospital plan and already tested in multiple simulations.
HEALTH PROFESSIONALS PROCEDURAL PROTOCOLS
At the end of the surgical procedure, undressing of the surgical staff takes place in the OR next to a dedicate exit door (different from the patient exit door). With regard to anesthesiology procedures, the patient is anesthetized and awakened within the OR and, if a postprocedure ICU recover is needed, our dedicated COVID-19 ICU is prealerted to leave the OR rapidly. On the other hand, if the patient does not require a postoperative intensive care, postsurgical observation takes place in a dedicated COVID-19 recovery room within the emergency surgery block.
OR WORKFLOW OPTIMIZATION
The entire process of COVID-19 OR usage is logistically demanding. After implementing our setup protocols, time to completion of the preliminary tasks (staff donning, protection of devices such ultrasound machines, preparation of instrument trays) before patient arrival has been optimized and limited to 15 minutes. However, OR environment decontamination after surgery is much complex and, overall, may take up to 2 hours. Air conditioning is not an issue, but deep cleaning of all surfaces and devices introduced into the OR takes at least 1 hour and 30 minutes, and supplies can only be provided after complete decontamination. Refurbishing of ventilators takes the longest time, about 4 hours as a whole. These long procedural times might impair OR availability. We overcame the problem by setting up all the 3 ORs in the emergency surgery block to be ready for COVID-19–protected surgery; thus, at least a second OR can be used while waiting for the first one to be refurbished and ready again.
Given the urge to spare resources in the COVID-19 pathway experienced during the epidemic peak, we tried to early and reliably select those emergency surgical patients not needing to be operated in a COVID-19–protected environment. When clinically feasible, surgery for chest CT-negative patients is delayed 6 hours until the result of at least the first nasopharyngeal swab is available: if negative, these patients are shifted to the standard “clean” OR; if not available, the COVID-19 pathway is activated.
RESULTS
We performed 82 emergency general surgical consultations for COVID19–positive (32) and –suspected (54) patients so far. Fifty-eight received a nonoperative management (NOM) and 24 underwent immediate general surgical procedures in the COVID-19 theater. Of these, only 3 (12,5%) were COVID-19–positive, all preoperatively documented. The remaining 21 “suspected” COVID-19 patients who underwent surgery finally resulted COVID-19–negative. This low rate of actually positive patients has prompted us to introduce some kind of “early warning scores” to better select those cases worthy of treatment under maximal COVID-19 precautions. This work is in progress.
We performed a number of different procedures: Hartmann colonic resection, small bowel resection for ischemia, appendectomy, complicated inguinal hernia reduction, subtotal colectomy for toxic megacolon.
Moreover, neurosurgical, vascular, urological, orthopedic, gynecologic, and obstetric procedures have been performed in the COVID-19 OR, including a cesarean delivery.
Finally, the COVID-19 OR and staff have addressed elective surgeries in proven COVID-19 patients.
Despite the relative complexity of the COVID-19 surgical pathway, we did not detect any significant delay in treatment. However, an early analysis of the March to April period data set documented an increase of NOM as compared with the same time interval of the previous 2 years. Given that in our policy, surgical indications have not been changed because of a COVID-19 suspicion alone (except for multidisciplinary management of respiratory failure when present), we assumed that this different treatment pattern may be due to more severe clinical conditions at arrival (e.g., septic shock) of patients who delayed access to the ED because of fear of contagion; in these cases, resuscitation and NOM were the only initial possible treatments as a bridge to surgery after restoring a satisfying functional status. On the other hand, a proportion of patients healthy enough to wait for the first COVID-19 nasopharyngeal swab had a clinical improvement during NOM that was finally confirmed as a definitive treatment.
TIPS AND TRICKS: TRAINING AND TESTING
Training of health care professionals has proven pivotal in the management of these complex patient pathways. At our institution, all health care professionals carried out a specific training on PPE use, face to face when possible, as well as online. Procedures and, consequently, training have been tailored according to the role that different professionals played in different settings during the pandemic. This allowed a significant containment of the infection rate among health care workers, which today turns out to be of 30 positive cases of 600 operators that are full time involved in the care of COVID-19 patients, with only one treated in ICU by noninvasive ventilation. Moreover, as soon as resources availability allowed it, our institution has begun testing all health care personnel, starting from the area most at risk first. This is pivotal, because, as shown in Lombardy, the most affected Italian region, one of the most frequent sources of infection is the health professionals themselves.
CONCLUSION
Our experience demonstrates how the creation and maintenance of a sustainable model for the care of surgical COVID patient needs a multidisciplinary approach and an injection of economic and human resources. Moreover, a precise and well-structured organization, with intuitive and easily reproducible paths, has to be built, maintaining flexibility to cope with different phases of the outbreak.
AUTHORSHIP
P.F. participated in the study conception and design, literature search, acquisition, interpretation and analysis of data, drafting and critically revising the article for important intellectual content; and final approval of the version to be published. G.S. participated in the drafting and critically revising the article for important intellectual content and final approval of the version to be published. M.D.G., V.F., and F.T. participated in the acquisition, interpretation, and analysis of data. V.C. participated in the drafting and critically revising the article for important intellectual content. A.L.G. participated in the drafting and critically revising the article for important intellectual content and final approval of the version to be published.
ACKNOWLEDGMENTS
We acknowledge all the Health Care Professionals involved in the management of the epidemics outbreaks at Fondazione Policlinico Universitario A. Gemelli IRCCS. In particular doctors: Andrea Cambieri, Marilena D'Alfonso, Achille Luongo (Direzione Sanitaria—Hospital Health Management), Patrizia Laurenti, Malgorzata Wachocka (Istituto di Igiene, Department of Hygiene), Filippo Berloco (Rischio Clinico—Clinical Risk Management), Maurizio Cianfanelli (Servizio Tecnico—Health Technology Assessment Unit), and Antonio Gasbarrini (Head of Department of Medical and Surgical Science). We also thank Mauro Iossa, Luca Vita, Alessio Conte for the active contribution to the setup of the ORs for COVID-19 emergency situations.
DISCLOSURE
The authors declare no funding or conflictsof interest.
Footnotes
Published online: June 23, 2020.
REFERENCES
- 1.Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elizabeth Brindle M, Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020;272:e1–e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ISS, Istituto superiore di Sanità, Italian Nation Istitute of Healt (https://www.epicentro.iss.it/coronavirus/sars-cov-2-sorveglianza-dati).
- 4.Coccolini F Perrone G Chiarugi M, et al. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020;272:e5–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]


