Abstract
Background
Vocalization is often used to assess pain, sometimes combined with other behaviours such as facial expressions. Contrary to facial expressions, however, for vocalization, there is little evidence available on the association with pain. The aim of this systematic review was to critically analyse the association between vocalization and pain, to explore if vocalizations can be used as a “stand‐alone” indicator for pain.
Methods
The search was performed according to the Prisma Guidelines for systematic reviews and meta‐analysis. The following terms were used: “Pain Measurement,” “Vocalization” and “Verbalization.” The study population included verbal and non‐verbal individuals, including older people and children. The search was performed in three different databases: PubMed, Embase and CINAHL. A total of 35 studies were selected for detailed investigation. Quality assessments were made using two grading systems: Grading of Recommendations Assessment Development and Evaluation system and the Newcastle‐Ottawa scale.
Results
An association between vocalization and pain was found in most studies, particularly when different types of vocalizations were included in the investigation. Different types of vocalization, but also different types of pain, shape this association. The association is observed within all groups of individuals, although age, amongst others, may have an influence on preferred type of vocalization.
Conclusions
There is an association between vocalization and pain. However, vocalization as a “stand‐alone” indicator for pain indicates only a limited aspect of this multifactorial phenomenon. Using vocalization as an indicator for pain may be more reliable if other pain indicators are also taken into account.
Significance
Vocalizations are frequently used in pain scales, although not yet thoroughly investigated as a “single indicator” for pain, like, e.g. facial expression. This review confirms the role of vocalizations in pain scales, and stresses that vocalizations might be more reliable if used in combination with other pain indicators.
1. INTRODUCTION
Pain assessment in the 21st century is still in its infancy (Lautenbacher, 2014). Pain is defined by the International Association of Pain (IASP) as “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (IASP, 1979).” It is a personal and subjective experience (Davis, 2011). Therefore, self‐report, either spontaneous or after being asked about pain with questionnaires and/or rating scales (Oosterman & Brazil, 2015), is considered the gold standard (Gregory, 2015; Stahnisch, 2015) for pain assessment. Those who are unable to verbally communicate their pain, such as older people with cognitive impairment caused by dementia and people with stroke or brain injuries, but also younger children, are completely dependent on others to be attentive to nonverbal signs of pain (Craig, 2009). These include facial expressions (e.g. grimace, frown, opened mouth), altered activity patterns (Corbett et al., 2014), body movements (e.g. rigid, tense body posture; restricted movement) and vocalizations (e.g. screaming, groaning, sighing). Of all nonverbal signs of pain, facial expression has been thoroughly investigated and recent reviews confirm an association between facial expression and pain (Kunz, Meixner, & Lautenbacher, 2018; Lautenbacher & Kunz, 2017). To our knowledge, there are no reviews on the possible association between vocalization and pain.
Vocalization is the utterance of sounds, noises and words using the vocal apparatus. Vocalization incorporates all verbalizations, such as mentioning pain or using offensive words (but not in the self‐conscious and intentional form as in self‐reporting pain), and non‐verbal vocalizations such as moaning, crying and groaning (Corbett et al., 2014). Sometimes, changes in respiration are also included in the definition of vocalization, e.g. sighing (Waters, Riordan, Keefe, & Lefebvre, 2008). According to the American Geriatric Society (AGS), vocalizations can be categorized as: verbal utterances, nonverbal utterances and breathing. The AGS points vocalization out as a common pain behaviour, including the following items: sighing, moaning, groaning, grunting, chanting, calling out, noisy breathing, asking for help and being verbally abusive (Corbett et al., 2014). However, the AGS does not categorize crying as a vocalization, but as a mental status change (Corbett et al., 2014).
Although vocalization is often mentioned in studies investigating pain, most studies do not directly investigate the association between vocalizations and pain. Other lines of research focus on creating, comparing or validating different types of pain scales (Fuchs‐Lacelle et al., 2003; Newman et al., 2005; Snoek, Timmers, Albertyn, & van Dijk, 2015; Strong, Ashton, & Chant, 1991; van Herk, van Dijk, Baar, Tibboel, & de Wit, 2007; Weiner, Peterson, Logue, & Keefe, 1998; Weiner, Pieper, McConnell, Martinez, & Keefe, 1996; Wood et al., 2004), operating under the assumption that vocalizations are a valid indicator for pain (Basler et al., 2006; Cook, Roddey, Bamer, Amtmann, & Keefe, 2013; Hesselgard, Larsson, Romner, Strömblad, & Reinstrup, 2007; Schuler et al., 2007). In these studies, vocalization is often given the same status as pain indicators that have been extensively studied, such as facial expression. Facial expression has been widely accepted as a pain indicator and available studies even allow reviews specified for types of facial expression as indicators for pain (Kunz et al., 2018). Such studies are not yet available for vocalization, but nonetheless, vocalization is used to prove the presence of pain. Clarity about the association between vocalization and pain would provide analgesic medication trials and developers of pain scales insight into the validity of the use of vocalization.
Hence, the objective of this systematic review was to investigate if vocalizations are a valid indicator for pain in different groups of subjects, including children, older persons and people who are cognitively impaired.
2. METHODS
2.1. Literature search
A review protocol was developed based on the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) statement (www.prisma‐statement.org).
A comprehensive search was performed in the bibliographic databases PubMed, Embase.com and Ebsco/CINAHL Library, in collaboration with a medical librarian. Databases were searched from inception up to January 29, 2019. The following terms were used (including synonyms and closely related words) as index terms or free‐text words:
“Pain Measurement” AND (“Vocalization” OR “Verbalization”). The search was performed without date, language or publication status restriction. Duplicate studies were excluded. The full search strategies for all databases can be found in the Supplementary Information.
2.2. Study selection
Two reviewers (LH and RW) independently screened the titles and abstracts. Exclusion criteria were defined as no vocalization, no pain involved, reviews, comparison of pain scales with no possibility of extracting data on vocalization, no separate measure of vocalization and no animal studies. To avoid circular reasoning, studies based on a presumed causal relationship between pain and vocalization were also excluded. Experiments, observational studies and randomized controlled trials investigating the relationship between vocalization and pain were all included. If the association between vocalization and pain was not the primary goal of the study, but data were available to investigate the association, the study was also included. Children, older people and ill and healthy humans were investigated. All types of vocalization were included. Some authors classified crying as a vocalization. Therefore, crying was also included. Following title and abstract screening, the full‐text studies were assessed. After removing duplicates, 568 studies were selected. Additionally, one study was added after hand‐searching the literature lists of relevant studies. See Figure 1 for a flowchart.
Figure 1.
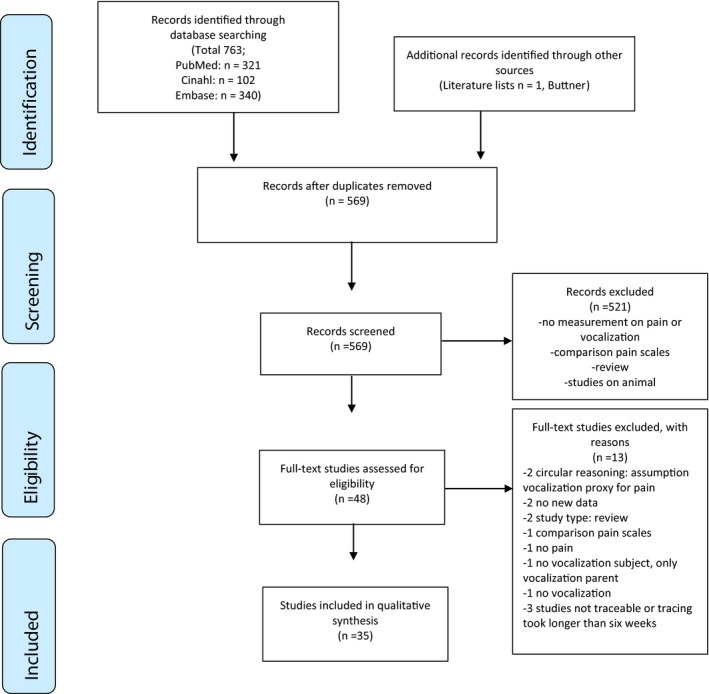
Flowchart of the included and excluded studies, according to PRISMA 2009
To give a better overview of the selected studies, a distinction was made between studies that directly investigated vocalization in participants and studies that retrieved their information through focus groups and questionnaires for experienced caregivers. This second group of studies is addressed separately under the heading “Expert opinions.”
2.3. Quality assessment
After screening and assessment of full‐text studies, all selected studies were rated according to the Grading of Recommendations Assessment Development and Evaluation quality evaluation system (GRADE) (Atkins et al., 2004). In brief, a study is rated high if it is a randomized controlled trial, low in case of an observational study and very low for all other types of study. This qualification is then further refined by assessing other aspects including the presence of inconsistencies and risk of bias, in which case the study is “downgraded.” The presence of a strong association, evidence of a dose–response gradient or control of confounders that would have reduced the effect is then assessed and if indicated, the study is upgraded. The outcome is one of four categories: “High,” “Moderate,” “Low” and “Very low.” Most of the included studies, however, were cohort studies. To rate these studies with more nuance, an additional quality assessment tool was used, viz., the Newcastle‐Ottawa Scale (NOS), which is appropriate for non‐randomized studies (Wells et al., 2013). According to the NOS, a study is awarded stars (range 0–9) by assessing three different components. A maximum of four stars can be awarded concerning the selection of the cohort. A fifth star is given for the comparability of this cohort, based on the study design or analysis, any additional control group accounts for a sixth star. Three more stars are awarded in the component “outcome,” with questions concerning assessment and follow‐up (Wells et al., 2013).
3. RESULTS
3.1. Search results
The literature search yielded 321 studies through PubMed, 340 through Embase and 102 throughCINAHL. One additional study was added by the authors after the manual search. After initial screening, 521 studies were excluded and another 13 were excluded based on the full text. A total of 35 studies met the inclusion criteria. Figure 1 represents the flow of the selection process.
3.2. Characteristics of selected studies
The 35 included studies describing the role of vocalization as an indicator for pain were published between 1982 and 2017. All of these studies were observational. After evaluating the quality of included studies with GRADE, nine studies were rated “Moderate,” 24 studies were rated “Low,” and two “Very low.” Additionally, all cohort studies (22/35) were also rated according to the NOS scale. The number of stars appointed after application of the NOS ranged from three to six. The results of these assessments are presented in the Supplementary Information (tables A and B). Tables C and D of the Supplementary Information provide an extended version of the study characteristics.
Of all 35 studies, 22 studies gathered the results by directly observing the subjects. These studies are classified per group: children (10/22), adults (9/22) and older persons (3/22). In these studies, different pain behaviours were included, varying from just crying or sighing to a variety of behaviours, including vocalization. The results are summarized in Table 1.
Table 1.
Included studies with information specific to the association between pain and vocalization, Grade and NOS scores: Direct observation
| Study | Sample size | Vocalizations | Conclusion vocalization | Conclusion relevant to review | GRADE score a | Newcastle‐Ottowa Scale (NOS) score, number of stars b |
|---|---|---|---|---|---|---|
| Büttner and Finke (2000) | 584 newborns/young children | crying, verbalization | crying amongst other was an important indicator for pain, verbalization was not a reliable pain indicator | positive association crying and acute pain | 3. low | 3 |
| Dale (1989) | 30 infants | crying | DTP injections led in all cases to crying | positive association crying and acute pain | 3. low | 3 |
| Dubois et al. (2008) | 47 children | vocalization | there was significantly more vocalization postoperative than preoperative | positive association vocalization and acute pain | 2. moderate | 5 |
| Elander et al. (1993) | 12 infants | vocalization | vocalization occurred, though maybe (not only) related to pain, although pain scales indicated insufficient pain relief | positive association vocalization and acute pain | 4. very low | 5 |
| Esfahlan et al. (2017) | 100 burn patients, age 15−60years | vocalization, crying, moaning, groaning, verbalization, vocalization stops c | Moaning, crying and vocalization stops associated significantly with self‐reported pain; an association between self‐reported pain and groaning and verbalization is not mentioned | positive association vocalization and pain | 2. moderate | 5 |
| Keefe and Block (1982) | 27 patients with low back pain | sighing | sighing amongst other was an important indicator for pain | positive association sighing and chronic pain | 2. moderate | 6 |
| Maitre et al. (2017) | 54 infants | crying | crying in newborns is not a specific marker for pain | no association crying and acute pain | 3. low | 6 |
| Manfredi et al. (2003) | 9 older persons | vocalization | combination facial expression and vocalization are associated with pain | positive association vocalization with facial expression and acute pain | 3. low | 5 |
| Nazari et al. (2018) | 35 patients of the intensive care unit | sighing, moaning | Pain behaviours included sighing and moaning | positive association vocalization and pain | 2. moderate | 6 |
| Oueriagli Nabih et al. (2016) | 40 children | vocalization | the majority of the autistic children vocalized after the painful stimulus | positive association vocalization and acute pain | 3. low | 3 |
| Puntillo et al. (2004) | 5,957 adults | verbalization, moaning, screaming, whimpering, crying | verbalizations and moaning increased significantly during procedural pain; an effect of procedural pain on screaming, whimpering and crying is not mentioned | positive association vocalization and acute pain | 2. moderate | 5 |
| Robbins et al. (2011) | 13 female adults | sighing | no significant relation between sighing and pain | no association sighing and chronic pain | 2. moderate | 6 |
| Rossato and Angelo (1999) | 41 children | vocalization, crying, sobbing, breathing, screaming, groaning | crying and screaming are important indicators for pain, groaning and sobbing were associated with pain in 10%–20% of the children, breathing showed no association with pain | positive association vocalization and pain | 3. low | 6 |
| Roulin and Ramelet (2015) | 116 patients with brain injury | Groaning & moaning, screaming & howling, crying, sighing | None of the vocalizations were significantly associated with pain | no association vocalization and pain | 3. low | 6 |
| Shega et al. (2008) | 77 older persons | sighing | sighing is not an important indicator for pain | no association sighing and pain | 3. low | 6 |
| Stanford et al. (2005) | 58 children | verbalization | only half of the children used verbalization to express pain | no association verbalization and pain | 2. moderate | 5 |
| Takai et al. (2014) | 252 older persons | vocalization | vocalization associated significantly with self‐reported pain | positive association vocalization and pain | 2. moderate | 5 |
| Topolovec‐Vranic et al. (2014) | 32 patients with brain injury | vocalization | vocalization associated with self‐reported pain | positive association vocalization and acute pain | 3. low | 6 |
| van den Berg et al. (2005) | 43 women selected for caesarean delivery | vocalization | vocalization scores differed significantly between the lidocaine and the control group | positive association vocalization and pain | 2. moderate | 4 |
| van der Putten and Vlaskamp (2011) | 32 children and adults | Moaning & groaning, crying/gasping & sobbing, penetrating sounds of restlessness | adults express pain mostly by moaning and groaning. Children use penetrating sounds of restlessness for pain expression. Crying/gasping & sobbing were rarely observed and not associated with pain. | positive association moaning/groaning and pain in adults, penetrating sounds and pain in children | 3. low | 4 |
| Warnock (2003) | 4 newborn males | vocalization, crying | crying with high‐pitched screeches was an indicator for pain | positive association specific type of crying and pain | 3. low | 5 |
| Waters et al. (2008) | 92 rheumatoid arthritis patients | sighing | sighing is not an important indicator for pain | no association sighing and chronic pain | 4. very low | 4 |
Abbreviations: human: human study; GRADE: Grading of Recommendations Assessment Development and Evaluation quality evaluation system; NOS: Newcastle‐Ottawa Scale.
A study can be awarded with one or two stars depending on the answer of each question, e.g. question S1 about the representativeness of the cohort investigated: One star if the cohort was representative or somewhat representative, no stars in case of a selected group.
Vocalization stops are also included in these articles as a pain behaviour in the category “vocalization.”
A study is classified depending on the design (RCT, observational, etc.) and can ascend or descend depending on report of bias, calculation of power, strength of evidence or in case of a dose–response gradient.
In Table 2, the information of the other 13 studies is summarized. These studies obtained their results through questionnaires and focus groups of experienced caregivers. They will be discussed separately under the heading “Expert opinions.”
Table 2.
Included studies with information specific to the association between pain and vocalization, Grade score: Expert opinion
| Study | Sample size | Vocalizations | Conclusion vocalization | Conclusion relevant to review | GRADE a |
|---|---|---|---|---|---|
| Abbey and Abbey (2009) | 598 residential care facilities | vocalization | vocalization was found important by most caretakers for assessing pain | positive association vocalization and pain | 3. low |
| Cohen‐Mansfield and Creedon (2002) | 72 nursing staff members | vocalization | repetitive vocalizations are an important behavioural parameter for pain | positive association vocalization and pain | 3. low |
| Decker (2009) | 16 nurses | vocalization, sighing, moaning, crying, yelling | Sighing, moaning, crying and yelling were identified as a behavioural indicators for pain | positive association vocalization and pain | 3. low |
| Gélinas et al. (2018) | 77 clinicians, adult neuroscience | moaning, verbal complaints | moaning and verbal complaints were identified as important pain behaviour by clinicians | positive association vocalization and pain | 3. low |
| Igier et al. (2014) | 79 nurses | verbalizations ‐ complains of pain | patient verbalizations had a significant effect on the judged pain level | positive association verbalization and judged level of pain | 3. low |
| Kovach et al. (2000) | 30 nurses | vocalization | moaning, crying and specific/nonspecific verbal behaviour were rated important behavioural indicators for pain | positive association vocalization and pain | 3. low |
| Pereira et al. (2011) | 19 caretakers of patients with cognitive impairment | vocalization, moaning, groaning, crying, yelling | moaning, groaning and crying are pain behaviours, yelling is not | positive association vocalization and pain | 3. low |
| Rose et al. (2011) | 140 nurses | vocalization | vocalization was found important by most nurses for assessing pain | positive association vocalization and pain | 3. low |
| Solodiuk (2013) | parents of 50 nonverbal children | vocalization, whimpering, growl, crying, screaming, howling, yelling, vocalization stops b | vocalization was identified as a behavioural indicator for pain, different types of vocalization were not specified in the result section | positive association vocalization and pain | 3. low |
| Swiggum et al. (2010) | 13 physical therapists | vocalization | vocalization was identified as a behavioural indicator for pain | positive association vocalization and pain | 3. low |
| Symons et al. (2013) | caregivers of 44 patients | vocalization | vocalization was identified as a behavioural indicator for pain | positive association vocalization and pain | 3. low |
| van Iersel et al. (2006) | 185 care providers | vocalization | vocalization was found important by most nurses for assessing pain | positive association vocalization and pain | 3. low |
| Zwakhalen et al. (2004) | 135 nurses | vocalization | vocalization was found important by most nurses for assessing pain | positive association vocalization and pain | 3. low |
Abbreviations: eo: expert opinion; GRADE: Grading of Recommendations Assessment Development and Evaluation quality evaluation system.
A study is classified depending on the design (RCT, observational, etc.) and can ascend or descend depending on report of bias, calculation of power, strength of evidence or in case of a dose–response gradient.
Vocalization stops are also included in these articles as a pain behaviour in the category “vocalization.”
3.3. Type of vocalization
Of all 22 direct‐observational studies, seven studies examined vocalization in general (7/22) and ten investigated one or two types of vocalization (10/22), e.g. only sighing or crying and verbalization. More than three different types of vocalization were investigated in only five studies (5/22) (Esfahlan, Safiri, Lotfi, Zamanzadeh, & Babapoor, 2017; Puntillo et al., 2004; Rossato & Angelo, 1999; Roulin & Ramelet, 2015; van der Putten & Vlaskamp, 2011). These vocalizations were crying, sighing, moaning, groaning, verbalizations, whimpering, growling, screaming, howling, yelling, gasping, sobbing, penetrating sounds of restlessness, breathing, verbal protest and vocalization stops.
An association between pain and vocalization was found in 16 out of 22 studies. Four out of five studies on crying found an association with pain (Büttner & Finke, 2000; Dale, 1989; Maitre et al., 2017; Rossato & Angelo, 1999; Warnock, 2003). A total of six studies did not find an association between vocalization and pain, three of which investigated sighing and pain (Robbins, Mehl, Holleran, & Kasle, 2011; Shega et al., 2008; Waters et al., 2008) and one investigated verbalization and pain (Stanford, Chambers, Craig, McGrath, & Cassidy, 2005). Most studies (3/4) that investigated more than three different vocalizations found an association between these vocalizations and pain (Esfahlan et al., 2017; Puntillo et al., 2004; Rossato & Angelo, 1999; van der Putten & Vlaskamp, 2011). Overall, the studies that included more than three vocalizations scored relatively highly on quality assessment (GRADE either 2. Moderate or 3. Low and NOS 4 to 6 stars) and four out of five concluded an association between vocalization and pain (Esfahlan et al., 2017; Puntillo et al., 2004; Rossato & Angelo, 1999; Roulin & Ramelet, 2015; van der Putten & Vlaskamp, 2011).
3.4. Type of pain
Some studies specified in type of pain investigated, i.e. acute or chronic. All studies on chronic pain investigated a possible association with sighing, and two out of three did not find an association (Keefe & Block, 1982; Robbins et al., 2011; Waters et al., 2008). In the studies investigating acute pain, however, the results were very different. Seven out of eight studies found an association between acute pain and vocalization (Büttner & Finke, 2000; Dale, 1989; Dubois, Bringuier, Capdevilla, & Pry, 2008; Elander, Hellstrom, & Qvarnstrom, 1993; Maitre et al., 2017; Manfredi, Breuer, Meier, & Libow, 2003; Oueriagli Nabih et al., 2016; Puntillo et al., 2004). One of these studies could only correlate vocalization and pain when accompanied by facial expression (Manfredi et al., 2003). Type of pain seems to play a role in the association with vocalization, and acute pain, rather than chronic pain, appears to have an association. Quality scores on the GRADE and NOS scales ranged from low to high, both in studies that did and did not find an association.
3.5. Paediatric studies
Ten studies included children. They reported on postoperative pain (3/10), pain due to a painful stimulus like vaccine injection (6/10) or during a planned care moment (1/10). In this latter case, pain was presumed to be present (van der Putten & Vlaskamp, 2011). The study investigated people with profound intellectual and multiple disabilities. The researchers included adults as well as children. The authors found different vocalizations to correlate with pain in adults and children, with children making more often penetrating sounds of restlessness and adults using moaning and groaning more often to express their pain (van der Putten & Vlaskamp, 2011).
Eight out of these ten studies found an association between pain and vocalization. The studies that did not find an association, investigated only verbalization or only crying. The study on verbalization found that 48.3% of all children (age range 4–6 years) used verbalizations to express pain, while the remaining 51.7% did not. Younger children used verbalizations more often. The authors suggested that this could be attributed to social factors. Older children might be more influenced by the observers not to show their pain (Stanford et al., 2005). In postoperative children, crying was amongst other behavioural parameters for pain, such as facial expression and motor restlessness, important for infants as well as for toddlers (Büttner & Finke, 2000). In almost all paediatric studies (8/10), vocalization was associated with pain, while in others facial expression and motor restlessness are also labelled as important behavioural parameters for pain. These eight studies scored average on both quality assessments. The two studies that found no association between vocalization and pain scored average on the GRADE scale and high on the NOS scale. On the NOS scale, they were awarded five and six stars; however, they only investigated one type of vocalization, i.e. verbalization and crying, respectively (Maitre et al., 2017; Stanford et al., 2005).
3.6. Adult studies
The group of nine studies on adults included patients with cognitive impairment and brain injury (Roulin & Ramelet, 2015; Topolovec‐Vranic et al., 2014), although further subjects were also investigated, varying from patients in the intensive care unit (Nazari et al., 2018) to needle insertion in pregnant women (van den Berg, Sadek, Swanson, & Ghatge, 2005).
The largest group of participants in one sample consisted of 5,957 cognitive healthy and communicative adults (Puntillo et al., 2004). These adults underwent one of the following six medical procedures in a hospital setting: turning, central venous catheter insertion, wound drains removal, wound care, tracheal suctioning and femoral sheath removal. All medical procedures were given an average pain score in a previous study and turning was appointed the highest procedural pain score (Puntillo et al., 2004). Amongst the seven most frequently observed behaviours were moaning and verbal complaints; both of them were exhibited more by patients with increased procedural pain (Puntillo et al., 2004).
Six out of nine studies on adults found an association between vocalization and pain. Again, quality scores on the GRADE and NOS scales ranged from low to high, both in studies that did and in studies that did not find an association. Overall, the majority of studies found an association between vocalization and pain.
3.7. Studies on older people
Three included studies investigated older people only; the median age in all studies was above 75 years. Two studies found an association between vocalization and pain, albeit one of them only if combined with facial expressions (Manfredi et al., 2003; Takai, Yamamoto‐Mitani, Ko, & Heilemann, 2014). In this case, dressing changes were videotaped in nine older patients with severe dementia suffering from painful decubitus ulcers. Independent viewers rated the videotapes for different pain behaviours. Facial expressions and vocalizations showed an association with the painful event with sensitivity, specificity, positive and negative predictive values all between 0.70 and 0.90. The intensity of the pain was not specified in this study (Manfredi et al., 2003). All three studies scored relatively high on the NOS scale, with five or six stars. The study that did not find an association between vocalization and pain scored best with six stars, but only included sighing (Shega et al., 2008). One study scored moderately on the GRADE scale, which is above average compared to the other studies, and found an association between vocalization and pain (Takai et al., 2014).
3.8. Expert opinions
Expert opinions (either physicians or nurses) were gauged through focus groups and questionnaires for experienced caregivers in thirteen studies. The outcomes are summarized in Table 2. The type of pain was not specified. The studies interviewed experts on human pain behaviour, most of them on pain behaviour in older people (6/13) or children (3/13). According to the employees of residential care facilities, the most useful pain indicators in older people are facial expression, body language and vocalization. Respondents also ranked different types of vocalizations used in different pain scales. Most highly rated and therefore more important were “calling out,” moaning, groaning and crying. “No vocalization” was rated the least useful (Abbey & Abbey, 2009). There was a consensus amongst all expert opinion studies that vocalization was an important behavioural indicator for pain. Other frequently used behavioural indicators for pain were facial expression, restless body movement and tense muscles.
Four of these studies investigated more than one vocalization, all thirteen studies scored average on the GRADE scale, and all thirteen studies found an association between vocalization and pain (Abbey & Abbey, 2009; Cohen‐Mansfield & Creedon, 2002; Decker, 2009; Gélinas et al., 2018; Igier, Sorum, & Mullet, 2014; Kovach, Griffie, Muchka, Noonan, & Weissman, 2000; Pereira, Morete, Bueno, & Santo, 2011; Rose et al., 2011; Solodiuk, 2013; Swiggum, Hamilton, Gleeson, Roddey, & Mitchell, 2010; Symons, Byiers, Tervo, & Beisang, 2013; van Iersel, Timmerman, & Mullie, 2006; Zwakhalen, van Dongen, Hamers, & Abu‐Saad, 2004).
3.9. Quality assessment
When comparing the grades awarded to the included studies by the two quality assessment systems, GRADE and NOS, it was found that some studies received a low GRADE score but a high NOS score. This difference can be attributed to the more specific type of questions of the NOS system in case of cohort studies. For example, one study was classified as very low by GRADE and still received 5 stars by NOS, because of describing structured observations and follow‐up (Elander et al., 1993). Overall, there is little difference between the quality of studies that did and the ones that did not find an association between pain and vocalization. Therefore, no consistent conclusions can be drawn, from the GRADE or the NOS quality assessment.
4. DISCUSSION
The aim of this systematic review was to critically analyse the presumed association between vocalization and pain, to see if vocalizations can be used as a “stand‐alone” indicator for pain. An association between vocalization and pain is suggested by most of the included studies (29/35).
Divergent outcomes in studies concerning the association between vocalization and pain could be attributed to a variety of differences in measurements. In most studies, only one or a few types of vocalizations were investigated. Of studies that did not find an association, five out of six included only one type of vocalization in their investigation, e.g. only sighing or only verbalization (Maitre et al., 2017; Robbins et al., 2011; Shega et al., 2008; Stanford et al., 2005; Waters et al., 2008). Possibly, not only the quantity of different vocalizations contributes to the association with pain, but also the type of vocalization. Research has shown that some phonetic characteristics are more associated with pain than others. In particular, increased pitch and loudness of vocalization were found to be associated with pain (Lautenbacher, Salinas‐Ranneberg, Niebuhr, & Kunz, 2017).
According to the American Geriatrics Society (AGS) Panel, crying is not a vocalization, but a mental status change (AGS Panel on Persistent Pain in Older Persons, 2002). Nevertheless, crying was categorized as a vocal behaviour in some of the included studies. In four out of five included studies where crying was the only vocalization investigated, an association between crying and pain was found (Büttner & Finke, 2000; Dale, 1989; Maitre et al., 2017; Rossato & Angelo, 1999; Warnock, 2003). One of those studies was in neonates. In this study, the association was found only for crying in an exhausted and weak manner (Warnock, 2003). The studies on crying included in this review mainly investigated children, some of them very young, in whom crying is the only way available to express themselves. In this case, crying might not be very specific to pain (Kurth et al., 2014; Warnock, 2003) but more related to distress. Calling out or facial features such as an eye squeeze, a nasolabial furrow or open‐mouth may be clearer pain indicators (Bustos, Jaaniste, Salmon, & Champion, 2008; Warnock, 2003). Two out of three studies that investigated crying in adults did not find any association with pain (Puntillo et al., 2004; Roulin & Ramelet, 2015). Thus, crying seems to be a pain indicator in children, but this association is less specific in adults.
The associations with pain vary by type of vocalization. Moaning and pain are associated in most studies. For verbalization or screaming an association with pain is found in just under half of the cases, whereas sighing or groaning and pain are not associated in most cases. Overall, too little evidence was found to distinguish which of these types of vocalization have a lesser or stronger association with pain. The same applies to the type of pain. Although most of the studies on chronic pain did not find an association with vocalization, the evidence is too weak to assume that only acute pain is associated with vocalization. In all three studies on chronic pain, the only vocalization included in the investigation was sighing, so this cannot be extrapolated to vocalization in general. It might be that different types of vocalization or different volumes of vocalization are associated with different types of pain, i.e. acute or chronic, and maybe even with intensity of pain. In a study on women in labour, medical staff were able to distinguish between the first and second stages of childbirth by listening to recordings of vocalizations (Baker & Kenner, 1993).
Two studies included in this review investigated not only a variety of different vocalizations, but also a decrease in vocalization; of those, the observational study found that this decrease could indicate the presence of pain (Solodiuk, 2013). This is also seen in children experiencing posttraumatic stress symptoms: up until a month after a burn, they displayed fewer smiles and vocalizations (Stoddard et al., 2006).
The literature shows that, amongst others, temperament, coping behaviour and developmental level play a role in pain behaviour (Broome, Bates, Lillis, & McGahee, 1990; Wallace, 1989). This was also found in one of the included paediatric studies, where the authors concluded that older children are more aware of rules of social display concerning the report of pain (Stanford et al., 2005).
Children with profound intellectual and multiple disabilities more often make penetrating sounds of restlessness, while adults with such disabilities use moaning and groaning more often in response to presumed painful stimuli (van der Putten & Vlaskamp, 2011). The children and adults included in this study were observed during a planned care moment (mostly incontinence garment change). It can be questioned if this event is truly painful, or rather more uncomfortable or embarrassing. In the included study on newborns, diaper change was classified as a non‐noxious event and associated with distress, not with pain (Warnock, 2003). In a study on infants (<3 years old), a clear difference was seen in behaviours related to pain and distress: pain as a result of a painful infectious disease, most frequently in HIV patients, led to more tension in the extremities, while assumed distress led to crying, moaning and alertness (Snoek et al., 2015).
Differences between participants in coping strategies are not included in this research, but might also influence pain behaviour. In the literature, a study on high catastrophizers found a difference in length of communicative pain behaviour (Sullivan, Adams, & Sullivan, 2004). Catastrophizers are individuals with an exaggerated negative mental vision during an actual or anticipated painful experience. When in the company of an observer, this behaviour was observed during a longer period than when left alone. This difference was not seen in low catastrophizers (Sullivan et al., 2004). This suggests that personality, but also the social environment, can influence communicative pain behaviour (Heathcote et al., 2015; Sullivan et al., 2004). Hence, vocalization is not exclusive to pain, but considering that distress and social interaction play a role, we can conclude there is an association between vocalization and pain.
Little high‐quality evidence is available on the association between vocalization and pain. Even less evidence is available when it comes to pain measurement tools for those who cannot self‐report their pain, as self‐report is the gold standard in the measurement of pain (Gregory, 2015; Stahnisch, 2015). Some of the available literature on vocalization is based on the assumption that vocalization and pain correlate, leaving other factors that can influence vocalizations out of the theoretical model.
The use of GRADE as a quality assessment system in this review allowed us to rate all studies through the same system. However, it brought little nuance to the included cohort studies. Therefore, the NOS scale was used for these studies. Using the NOS, differences between cohort studies were clarified, although the included studies did not exceed six out of nine stars. Frequently, this lower quality was attributed to the study design. Future research could be improved in stronger cohort studies with control groups, structured observations and follow‐up. It would also be interesting to test different types of vocalization as indicators for pain. Studies that incorporated three vocalizations or more all found an association between vocalization and pain. Therefore, it would be interesting to investigate if some vocalizations might have a stronger association with pain than others. The types of vocalization that showed unclear results in this review are screaming, groaning, verbalization and sighing. Authors of the included studies contradicted each other on the association with pain in these specific vocalizations. Hence, investigating them separately would give insight into which vocalizations contribute more to an association with pain. In addition, investigating vocalizations for different types of pain, especially chronic pain, could also prove interesting, as there is not much available evidence.
In this review, the relationship between pain and vocalization was approached from a dichotomous perspective, i.e. an association or no association. All associations were positive, none were negative, as can be found in Tables 1 and 2. However, associations are continuous parameters, reflecting the strength of an association. At this stage, it is not possible to provide continuous information about the strength of a relationship, due to difficulties in comparing study designs and populations.
5. CONCLUSION
The results of this systematic review demonstrate that even though there is an association between vocalization and pain, it should be interpreted with caution. As with many pain indicators, vocalization is neither unique nor specific to pain. Moreover, pain can also be associated with less vocalization.
The association between vocalization and pain may also be influenced by other factors, such as social environment, personality type or age. Also, vocalization may be the result of other factors, such as fear or stress.
Multidimensional approaches are always better, not only in the case of vocalization. Using vocalization as a single pain indicator is too limited an approach to the multifactorial phenomenon “pain”; therefore, it is of utmost importance that other pain behaviours, such as facial expression and body movement, are also considered.
CONFLICTS OF INTEREST
The authors declare no financial or other conflicts of interest.
AUTHOR CONTRIBUTIONS
LH, RW and FL conceived and designed the study. RdV was involved in performing the search. LH and RW selected the studies. LH drafted the manuscript. All authors were involved in revising and approving the manuscript.
Supporting information
Supplementary Material
Helmer LML, Weijenberg RAF, de Vries R, et al. Crying out in pain—A systematic review into the validity of vocalization as an indicator for pain. Eur J Pain. 2020;24:1703–1715. 10.1002/ejp.1623
REFERENCES
- Abbey, J. , & Abbey, B. (2009). Pain management for residents with severe dementia in Australian residential care facilities: Policies, practices and pain scales. Journal of Pain and Symptom Management, 1, 379–389. [Google Scholar]
- AGS Panel on Persistent Pain in Older Persons (2002). The management of persistent pain in older persons. Journal of the American Geriatrics Society, 50, S205–S224. [DOI] [PubMed] [Google Scholar]
- Atkins, D. , Best, D. , Briss, P. A. , Eccles, M. , Falck‐Ytter, Y. , Flottorp, S. , … … GRADE Working Group . (2004). Grading quality of evidence and strength of recommendations. BMJ, 328, 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker, A. , & Kenner, A. N. (1993). Communication of pain: Vocalization as an indicator of the stage of labour. Australian and New Zealand Journal of Obstetrics and Gynaecology, 33, 384–385. 10.1111/j.1479-828X.1993.tb02115.x [DOI] [PubMed] [Google Scholar]
- Basler, H. D. , Hüger, D. , Kunz, R. , Luckmann, J. , Lukas, A. , Nikolaus, T. , & Schuler, M. S. (2006). Assessment of pain in advanced dementia. Construct validity of the German PAINAD. Schmerz, 20, 519–526. [DOI] [PubMed] [Google Scholar]
- Broome, M. E. , Bates, T. A. , Lillis, P. P. , & McGahee, T. W. (1990). Children's medical fears, coping behaviors, and pain perceptions during a lumbar puncture. Oncology Nursing Forum, 17, 361–367. [PubMed] [Google Scholar]
- Bustos, T. , Jaaniste, T. , Salmon, K. , & Champion, G. D. (2008). Evaluation of a brief parent intervention teaching coping‐promoting behavior for the infant immunization context: A randomized controlled trial. Behavior Modification, 32, 450–467. 10.1177/0145445507309031 [DOI] [PubMed] [Google Scholar]
- Büttner, W. , & Finke, W. (2000). Analysis of behavioural and physiological parameters for the assessment of postoperative analgesic demand in newborns, infants and young children: A comprehensive report on seven consecutive studies. Paediatric Anaesthesia, 10, 303–318. 10.1046/j.1460-9592.2000.00530.x [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , & Creedon, M. (2002). Nursing staff members' perceptions of pain indicators in persons with severe dementia. Clinical Journal of Pain, 18, 64–73. 10.1097/00002508-200201000-00010 [DOI] [PubMed] [Google Scholar]
- Cook, K. F. , Roddey, T. S. , Bamer, A. M. , Amtmann, D. , & Keefe, F. J. (2013). Validity of an observation method for assessing pain behavior in individuals with multiple sclerosis. Journal of Pain and Symptom Management, 46, 413–421. 10.1016/j.jpainsymman.2012.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett, A. , Achterberg, W. , Husebo, B. , Lobbezoo, F. , de Vet, H. , Kunz, M. , … Lautenbacher, S. (2014). An international road map to improve pain assessment in people with impaired cognition: The development of the Pain Assessment in Impaired Cognition (PAIC) meta‐tool. BMC Neurology, 14, 229 10.1186/s12883-014-0229-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig, K. D. (2009). The social communication model of pain. Canadian Psychology/Psychologie Canadienne, 50, 22–32. 10.1037/a0014772 [DOI] [Google Scholar]
- Dale, J. C. (1989). A multidimensional study of infants' behaviors associated with assumed painful stimuli: Phase II. Journal of Pediatric Health Care, 3, 34–38. 10.1016/0891-5245(89)90047-3 [DOI] [PubMed] [Google Scholar]
- Davis, K. D. (2011). Neuroimaging of pain: What does it tell us? Current Opinion in Supportive and Palliative Care, 5, 116–121. 10.1097/SPC.0b013e3283458f96 [DOI] [PubMed] [Google Scholar]
- Decker, S. (2009). Behavioral indicators of postoperative pain in older adults with delirium. Clinical Nursing Research, 18, 336–347. 10.1177/1054773809341734 [DOI] [PubMed] [Google Scholar]
- Dubois, A. , Bringuier, S. , Capdevilla, X. , & Pry, R. (2008). Vocal and verbal expression of postoperative pain in preschoolers. Pain Management Nursing, 9, 160–165. 10.1016/j.pmn.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Elander, G. , Hellstrom, G. , & Qvarnstrom, B. (1993). Care of infants after major surgery: Observation of behavior and analgesic administration. Pediatric Nursing, 19, 221–229. [PubMed] [Google Scholar]
- Esfahlan, A. J. , Safiri, S. , Lotfi, M. , Zamanzadeh, V. , & Babapoor, J. (2017). Association between behavioral responses and burn pain intensity. Trauma Monthly, 22(3). 10.5812/traumamon.39442 [DOI] [Google Scholar]
- Fuchs‐Lacelle, S. , Hadjistavropoulos, T. , Sharpe, D. , Williams, J. , Martin, R. , & LaChapelle, D. (2003). Comparing two observational systems in the assessment of knee pain. Pain Research and Management, 8, 205–211. 10.1155/2003/434267 [DOI] [PubMed] [Google Scholar]
- Gélinas, C. , Puntillo, K. A. , Boitor, M. , Bérubé, M. , Topolovec‐Vranic, J. , Ramelet, A. S. , … Streiner, D. L. (2018). Content validation of behaviours and autonomic responses for the assessment of pain in critically ill adults with a brain injury. Australian Critical Care, 31, 145–151. 10.1016/j.aucc.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Gregory, J. (2015). The complexity of pain assessment in older people. Nursing Older People, 27, 16–21. 10.7748/nop.27.8.16.e738 [DOI] [PubMed] [Google Scholar]
- Heathcote, L. C. , Vervoort, T. , Eccleston, C. , Fox, E. , Jacobs, K. , Van Ryckeghem, D. M. L. , & Lau, J. Y. F. (2015). The relationship between adolescentsʼ pain catastrophizing and attention bias to pain faces is moderated by attention control. Pain, 156, 1334–1341. 10.1097/j.pain.0000000000000174 [DOI] [PubMed] [Google Scholar]
- Hesselgard, K. , Larsson, S. , Romner, B. , Strömblad, L.‐G. , & Reinstrup, P. (2007). Validity and reliability of the Behavioural Observational Pain Scale for postoperative pain measurement in children 1–7 years of age. Pediatric Critical Care Medicine, 8, 102–108. 10.1097/01.PCC.0000257098.32268.AA [DOI] [PubMed] [Google Scholar]
- IASP (1979). IASP pain terms. Pain, 6, 247–252.460931 [Google Scholar]
- Igier, V. , Sorum, P. C. , & Mullet, E. (2014). Judging patients' pain from external cues. Journal of Health Psychology, 19, 570–573. 10.1177/1359105313475899 [DOI] [PubMed] [Google Scholar]
- Keefe, F. J. , & Block, A. R. (1982). Development of an observation method for assessing pain behavior in chronic low back pain patients. Behavior Therapy, 13, 363–375. 10.1016/S0005-7894(82)80001-4 [DOI] [Google Scholar]
- Kovach, C. , Griffie, J. , Muchka, S. , Noonan, P. , & Weissman, D. (2000). Nurses' perceptions of pain assessment and treatment in the cognitively impaired elderly: It's not a guessing game. Clinical Nurse Specialist, 14, 215–220. 10.1097/00002800-200009000-00011 [DOI] [PubMed] [Google Scholar]
- Kunz, M. , Meixner, D. , & Lautenbacher, S. (2018). Facial muscle movements encoding pain – A systematic review. Pain, 160(3), 535–549. [DOI] [PubMed] [Google Scholar]
- Kurth, E. , Kennedy, H. P. , Zemp Stutz, E. , Kesselring, A. , Fornaro, I. , & Spichiger, E. (2014). Responding to a crying infant – You do not learn it overnight: A phenomenological study. Midwifery, 30, 742–749. 10.1016/j.midw.2013.06.017 [DOI] [PubMed] [Google Scholar]
- Lautenbacher, S. (2014). Pain assessment in special patient groups such as those with dementia: At the finishing line or just starting from scratch? Pain, 155, 1419–1420. 10.1016/j.pain.2014.05.001 [DOI] [PubMed] [Google Scholar]
- Lautenbacher, S. , & Kunz, M. (2017). Facial pain expression in dementia: A review of the experimental and clinical evidence. Current Alzheimer Research, 14, 501–505. 10.2174/1567205013666160603010455 [DOI] [PubMed] [Google Scholar]
- Lautenbacher, S. , Salinas‐Ranneberg, M. , Niebuhr, O. , & Kunz, M. (2017). Phonetic characteristics of vocalizations during pain. Pain Reports, 2, e597 10.1097/PR9.0000000000000597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maitre, N. L. , Stark, A. R. , McCoy Menser, C. C. , Chorna, O. D. , France, D. J. , Key, A. F. , … Bruehl, S. (2017). Cry presence and amplitude do not reflect cortical processing of painful stimuli in newborns with distinct responses to touch or cold. Archives of Disease in Childhood. Fetal and Neonatal Edition, 102, F428–F433. 10.1136/archdischild-2016-312279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi, P. L. , Breuer, B. , Meier, D. E. , & Libow, L. (2003). Pain assessment in elderly patients with severe dementia. Journal of Pain and Symptom Management, 25, 48–52. 10.1016/S0885-3924(02)00530-4 [DOI] [PubMed] [Google Scholar]
- Nazari, R. , Pahlevan Sharif, S. , Allen, K. A. , Sharif Nia, H. , Yee, B.‐L. , & Yaghoobzadeh, A. (2018). Behavioral pain indicators in patients with traumatic brain injury admitted to an intensive care unit. Journal of Caring Sciences, 7, 197–203. 10.15171/jcs.2018.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman, C. J. , Lolekha, R. , Limkittikul, K. , Luangxay, K. , Chotpitayasunondh, T. , & Chanthavanich, P. (2005). A comparison of pain scales in Thai children. Archives of Disease in Childhood, 90, 269–270. 10.1136/adc.2003.044404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterman, J. , & Brazil, I. A. (2015). Tools that should be considered in pain assessment: Cognitive factors, emotion and personality In Pickering G. & Gibson S. (Eds.), Pain, emotion and cognition (pp. 83–100). Cham: Springer. [Google Scholar]
- Oueriagli Nabih, F. , Benali, A. , Kachouchi, A. , Adali, I. , Manoudi, F. , & Asri, F. (2016). Pain perception in children with autism (prospective study of 40 cases). Neuropsychiatr Enfance Adolesc, 64, 52–57. [Google Scholar]
- Pereira, C. , Morete, M. , Bueno, M. , & Santo, D. E. (2011). Knowledge of caretakers about pain of long‐stay patients with cognitive impairment. European Journal of Pain Supplements, 5, 78. [Google Scholar]
- Puntillo, K. A. , Morris, A. B. , Thompson, C. L. , Stanik‐Hutt, J. , White, C. A. , & Wild, L. R. (2004). Pain behaviors observed during six common procedures: Results from Thunder Project II. Critical Care Medicine, 32, 421–427. 10.1097/01.CCM.0000108875.35298.D2 [DOI] [PubMed] [Google Scholar]
- Robbins, M. L. , Mehl, M. R. , Holleran, S. E. , & Kasle, S. (2011). Naturalistically observed sighing and depression in rheumatoid arthritis patients: A preliminary study. Health Psychology, 30, 129–133. 10.1037/a0021558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, L. , Haslam, L. , Dale, C. , Knechtel, L. , Fraser, M. , Pinto, R. , … Watt‐Watson, J. (2011). Survey of assessment and management of pain for critically ill adults. Intensive & Critical Care Nursing, 27, 121–128. 10.1016/j.iccn.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Rossato, L. , & Angelo, M. (1999). Using tools for pain perception assessment in hospitalized pre‐school children submitted to painful procedure. Revista Da Escola De Enfermagem Da USP, 33, 236–249. [DOI] [PubMed] [Google Scholar]
- Roulin, M.‐J. , & Ramelet, A.‐S. (2015). Generating and selecting pain indicators for brain‐injured critical care patients. Pain Management Nursing, 16(3), 221–232. 10.1016/j.pmn.2014.06.003 [DOI] [PubMed] [Google Scholar]
- Schuler, M. S. , Becker, S. , Kaspar, R. , Nikolaus, T. , Kruse, A. , & Basler, H. D. (2007). Psychometric properties of the German “Pain Assessment in Advanced Dementia Scale” (PAINAD‐G) in nursing home residents. Journal of the American Medical Directors Association, 8, 388–395. 10.1016/j.jamda.2007.03.002 [DOI] [PubMed] [Google Scholar]
- Shega, J. W. , Rudy, T. , Keefe, F. J. , Perri, L. C. , Mengin, O. T. , & Weiner, D. K. (2008). Validity of pain behaviors in persons with mild to moderate cognitive impairment. Journal of the American Geriatrics Society, 56, 1631–1637. 10.1111/j.1532-5415.2008.01831.x [DOI] [PubMed] [Google Scholar]
- Snoek, K. G. , Timmers, M. , Albertyn, R. , & van Dijk, M. (2015). Pain indicators for persisting pain in hospitalized infants in a South African setting: An explorative study. Journal of Pain & Palliative Care Pharmacotherapy, 29, 125–132. 10.3109/15360288.2015.1035830 [DOI] [PubMed] [Google Scholar]
- Solodiuk, J. C. (2013). Parent described pain responses in nonverbal children with intellectual disability. International Journal of Nursing Studies, 50, 1033–1044. 10.1016/j.ijnurstu.2012.11.015 [DOI] [PubMed] [Google Scholar]
- Stahnisch, F. W. (2015). Objectifying pain in the modern neurosciences: A historical account of the visualization technologies used in the development of an algesiogenic pathology, 1850 to 2000. Brain Sciences, 5, 521–545. 10.3390/brainsci5040521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford, E. A. , Chambers, C. T. , Craig, K. D. , McGrath, P. J. , & Cassidy, K.‐L. (2005). “Ow!”: Spontaneous verbal pain expression among young children during immunization. Clinical Journal of Pain, 21, 499–502. 10.1097/01.ajp.0000146164.38400.91 [DOI] [PubMed] [Google Scholar]
- Stoddard, F. J. , Ronfeldt, H. , Kagan, J. , Drake, J. E. , Snidman, N. , Murphy, J. M. , … Sheridan, R. L. (2006). Young burned children: The course of acute stress and physiological and behavioral responses. American Journal of Psychiatry, 163, 1084–1090. 10.1176/ajp.2006.163.6.1084 [DOI] [PubMed] [Google Scholar]
- Strong, J. , Ashton, R. , & Chant, D. (1991). Pain intensity measurement in chronic low back pain. Clinical Journal of Pain, 7, 209–218. 10.1097/00002508-199109000-00007 [DOI] [PubMed] [Google Scholar]
- Sullivan, M. J. L. , Adams, H. , & Sullivan, M. E. (2004). Communicative dimensions of pain catastrophizing: Social cueing effects on pain behaviour and coping. Pain, 107, 220–226. 10.1016/j.pain.2003.11.003 [DOI] [PubMed] [Google Scholar]
- Swiggum, M. , Hamilton, M. L. , Gleeson, P. , Roddey, T. , & Mitchell, K. (2010). Pain assessment and management in children with neurologic impairment: A survey of pediatric physical therapists. Pediatric Physical Therapy, 22, 330–335. 10.1097/PEP.0b013e3181ea8d7d [DOI] [PubMed] [Google Scholar]
- Symons, F. J. , Byiers, B. , Tervo, R. C. , & Beisang, A. (2013). Parent‐reported pain in Rett syndrome. Clinical Journal of Pain, 29, 744–746. 10.1097/AJP.0b013e318274b6bd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takai, Y. , Yamamoto‐Mitani, N. , Ko, A. , & Heilemann, M. V. (2014). Differences in pain measures by mini‐mental state examination scores of residents in aged care facilities: Examining the usability of the Abbey pain scale‐Japanese version. Pain Management Nursing, 15, 236–245. 10.1016/j.pmn.2012.09.004 [DOI] [PubMed] [Google Scholar]
- Topolovec‐Vranic, J. , Gelinas, C. , Innis, J. , Li, Y. , McFarlan, A. , & Canzian, S. (2014). Pain‐related behaviors among critically ill adults with and without brain injury. Pain Research and Management, 19, e94. [Google Scholar]
- van den Berg, A. A. , Sadek, M. , Swanson, S. , & Ghatge, S. (2005). Epidural injection of lidocaine reduces the response to dural puncture accompanying spinal needle insertion when performing combined spinal‐epidural anesthesia. Anesthesia and Analgesia, 101, 882–885. 10.1213/01.ANE.0000159159.98754.46 [DOI] [PubMed] [Google Scholar]
- van der Putten, A. , & Vlaskamp, C. (2011). Pain assessment in people with profound intellectual and multiple disabilities; a pilot study into the use of the Pain Behaviour Checklist in everyday practice. Research in Developmental Disabilities, 32(5), 1677–1684. 10.1016/j.ridd.2011.02.020 [DOI] [PubMed] [Google Scholar]
- van Herk, R. , van Dijk, M. , Baar, F. P. M. , Tibboel, D. , & de Wit, R. (2007). Observation scales for pain assessment in older adults with cognitive impairments or communication difficulties. Nursing Research, 56(1), 34–43. 10.1097/00006199-200701000-00005 [DOI] [PubMed] [Google Scholar]
- van Iersel, T. , Timmerman, D. , & Mullie, A. (2006). Introduction of a pain scale for palliative care patients with cognitive impairment. International Journal of Palliative Nursing, 12, 54–59. 10.12968/ijpn.2006.12.2.20531 [DOI] [PubMed] [Google Scholar]
- Wallace, M. R. (1989). Temperament: a variable in children's pain management. Pediatric Nursing, 15, 118–121. [PubMed] [Google Scholar]
- Warnock, F. (2003). An ethogram of neonatal distress behavior in response to acute pain (newborn male circumcision). Infant Behavior and Development, 26, 398–420. 10.1016/S0163-6383(03)00038-9 [DOI] [PubMed] [Google Scholar]
- Waters, S. , Riordan, P. , Keefe, F. , & Lefebvre, J. (2008). Pain behavior in rheumatoid arthritis patients: Identification of pain behavior subgroups. Journal of Pain and Symptom Management, 36, 69–78. 10.1016/j.jpainsymman.2007.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner, D. K. , Peterson, B. L. , Logue, P. , & Keefe, F. J. (1998). Predictors of pain self‐report in nursing home residents. Aging Clinical and Experimental Research, 10, 411–420. 10.1007/BF03339888 [DOI] [PubMed] [Google Scholar]
- Weiner, D. , Pieper, C. , McConnell, E. , Martinez, S. , & Keefe, F. (1996). Pain measurement in elders with chronic low back pain: Traditional and alternative approaches. Pain, 67, 461–467. 10.1016/0304-3959(96)03150-8 [DOI] [PubMed] [Google Scholar]
- Wells, G. , Shea, B. , O'Connell, D. , Peterson, J. , Welch, V. , Losos, M. , & Tugwell, P. (2013). The Newcastle‐Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. Retrieved from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Wood, C. , von Baeyer, C. L. , Bourrillon, A. , Dejos‐Conant, V. , Clyti, N. , & Abitbol, V. (2004). Self‐assessment of immediate post‐vaccination pain after two different MMR vaccines administered as a second dose in 4‐ to 6‐year‐old children. Vaccine, 23, 127–131. 10.1016/j.vaccine.2004.08.029 [DOI] [PubMed] [Google Scholar]
- Zwakhalen, S. M. G. , van Dongen, K. A. J. , Hamers, J. P. H. , & Abu‐Saad, H. H. (2004). Pain assessment in intellectually disabled people: Non‐verbal indicators. Journal of Advanced Nursing, 45, 236–245. 10.1046/j.1365-2648.2003.02884.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


