Abstract
Arthrofibrosis, as a result of osteoarthritis, after trauma, or after knee surgery, can have significant implications for patient function, satisfaction, and outcomes. When extensive conservative management fails to achieve satisfactory results, surgical intervention may be necessary. Arthroscopic techniques to release anterior adhesions are often viewed as easier and safer than posterior releases required for flexion contractures. We present our technique of a safe, effective, and reproducible arthroscopic complete posterior capsulotomy.
Arthrofibrosis after knee surgery, after trauma, or from osteoarthritis can have significant consequences for patients. Failure to regain full motion after knee ligament reconstruction surgery has been shown to reduce patient satisfaction scores and return-to-play rates and even increase the risk of osteoarthritis development.1,2 Extension deficits of 15° cause increased joint shear stresses and mechanical overload in both the affected knee and the contralateral limb.3 After arthroscopic knee surgery, 0.06% to 6% of patients will require some level of arthroscopic lysis of adhesions.4 Several studies have shown that arthroscopic lysis of adhesions and posterior capsular release are safe and effective.5, 6, 7, 8, 9 These techniques can improve patient satisfaction and function.6 We present a technique for medial and lateral posterior capsular release for knee flexion contracture that is safe, effective, and reproducible.
Surgical Technique
Indications
Indicated patients have a clinically significant loss of knee extension despite exhaustive conservative management. Posterior capsular release can follow failed manipulation under anesthesia and anterior lysis of adhesions or can augment these procedures.
Positioning, Motion Assessment, and Manipulation
The technique is shown in Video 1. The patient is placed supine under general anesthesia, and an examination under anesthesia is performed. A goniometer is used to document the arc of motion of the knee. Gentle manipulation under anesthesia is performed at this point. If full motion is achieved, an arthroscopic release is unnecessary. The lateral post, which will allow access to the medial knee compartment, should be able to be dropped during surgery (Fig 1).
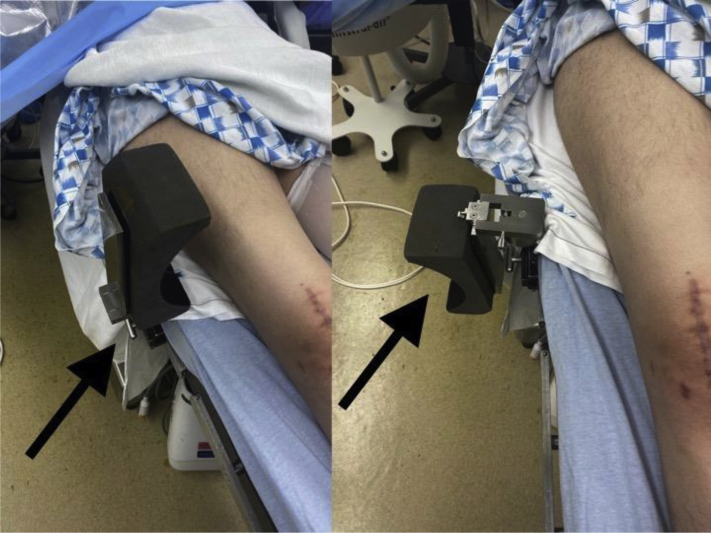
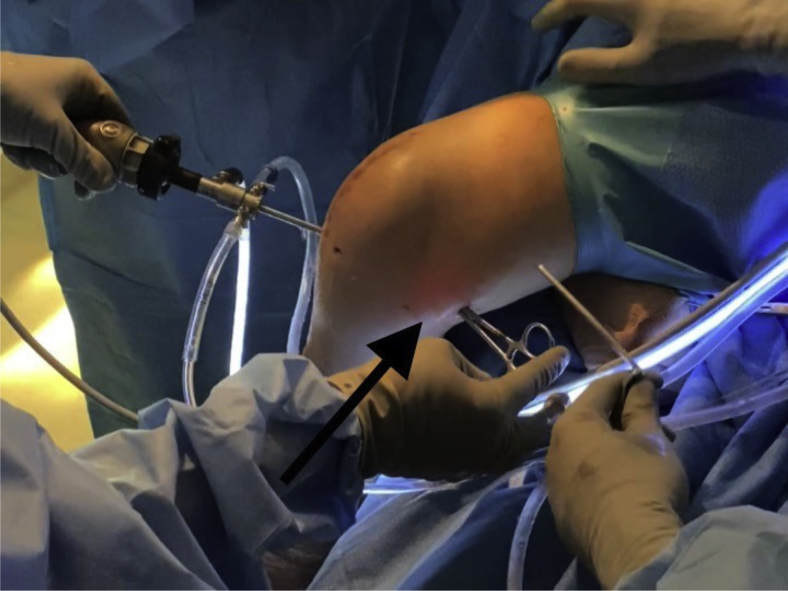
Fig 1.
Lateral post (arrows) with patient in supine position. The post is placed lateral to the surgical knee and 4 inches above the superior pole of the patella. It is used to place valgus stress on the knee, opening the medial compartment for arthroscopic access. The post is hinged, allowing it to be dropped for lateral and posteromedial arthroscopic instrumentation.
Diagnostic Arthroscopy and Anterior Debridement
Standard inferomedial and inferolateral arthroscopic portals are used. Standard anterior release and debridement are performed. Once completed, the shaver and 30° arthroscope are removed from the knee and another gentle manipulation under anesthesia is performed. If a flexion contracture still exists, attention is turned to gaining access to the back of the knee.
Posteromedial Access and Capsular Release
If the lateral post was not dropped during the anterior release after the completion of medial-compartment work, it is now dropped. The knee is allowed to hang off the edge of the bed at 90° and kept there for the remainder of the release. This allows the neurovascular structures to fall away to a safer, more posterior position.10 The leg is abducted laterally, and a bolster of surgical towels is placed under the thigh (Fig 2), which allows improved access for posteromedial portal placement and instrumentation. Arthroscopic access to the posteromedial compartment is achieved bluntly through the anterolateral portal with the trocar advanced through the intercondylar notch along the medial femoral condyle and under the posterior cruciate ligament using the technique described by Kramer et al.11 (Fig 3). Once in the posteromedial compartment, a 30° arthroscope is introduced through its sleeve and used to visualize the placement of an 18-gauge spinal needle positioned off the posterior aspect of the medial femoral condyle and just above the posterior horn of the medial meniscus (Figs 4 and 5). This represents where the posteromedial arthroscopic portal will be created, which is in the soft spot between the posterior oblique ligament and medial edge of the medial head of the gastrocnemius tendon. Too posterior placement can result in gastrocnemius tendon penetration, and too inferior placement can endanger the sartorial branch of the saphenous nerve.12 Once this position is confirmed with the spinal needle, its position and trajectory are noted; then, it is removed. A No. 15 surgical blade is used to make a small skin nick, and a straight snap is used to gently dissect through subcutaneous tissue and to penetrate the posteromedial capsule following the trajectory of the spinal needle (Fig 6). A sled or half-pipe tool is used to exchange the straight snap for a blunt switching stick (ConMed, Largo, FL) (Fig 7). A 7-mm soft-tissue dilator (Arthrex, Naples, FL) is slid over the switching stick to enlarge the capsular rent, followed by placement of a 7–mm–outer diameter twist-in cannula (Arthrex), allowing an easy exchange of instruments (Figs 8 and 9). If synovitis or adhesions obstruct a clear view of the posteromedial capsule, a torpedo shaver (Arthrex) is used to gently debride the overlying tissue (Fig 10). A 90° arthroscopic hook probe electrode (Electrode Hook 90; Arthrex) is then introduced and used to section the capsule (Fig 11). The capsule is released midway between the femoral attachment and the posteromedial meniscal attachment, starting laterally at the posterior septum and extending medially to the established portal (Figs 11 and 12). The capsular release is complete when the medial head of the gastrocnemius is visible. The shaver is then reintroduced to gently debride the edges of the capsule and prevent the ends from re-scarring to one another (Figs 13 and 14).
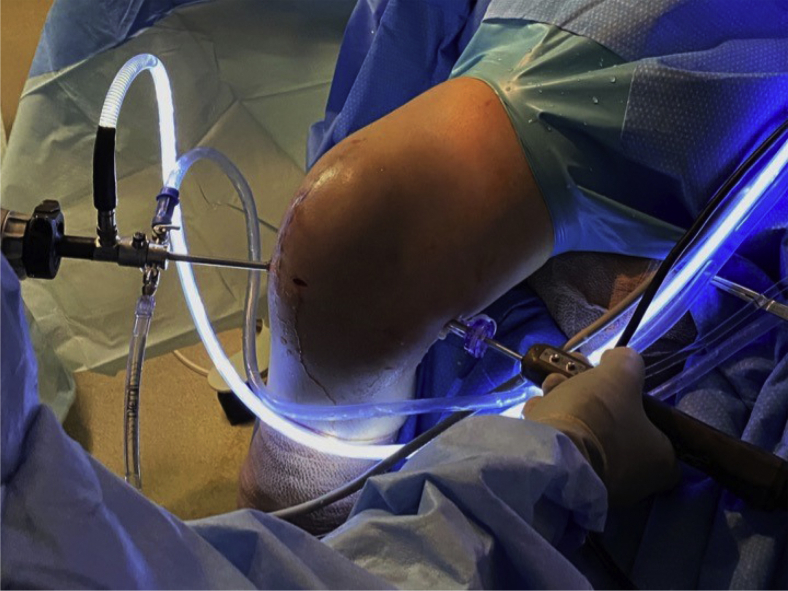
Fig 2.
Right knee with bolster placed under thigh (arrow), which improves posteromedial access for instrumentation. The tibia hangs off the bed with the knee resting in 90° of flexion.
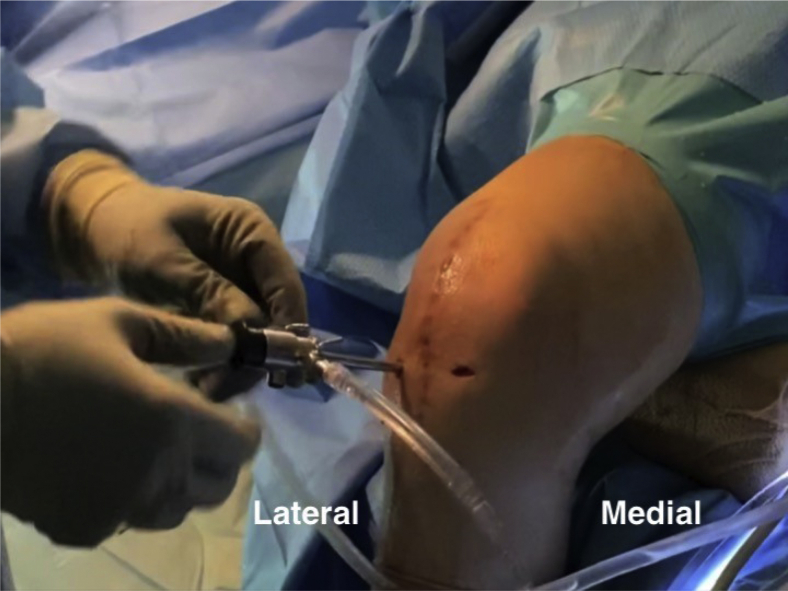
Fig 3.
Arthroscope positioning for posteromedial-compartment access. The arthroscope is directed through the notch under the posterior cruciate ligament via a standard anterolateral portal.
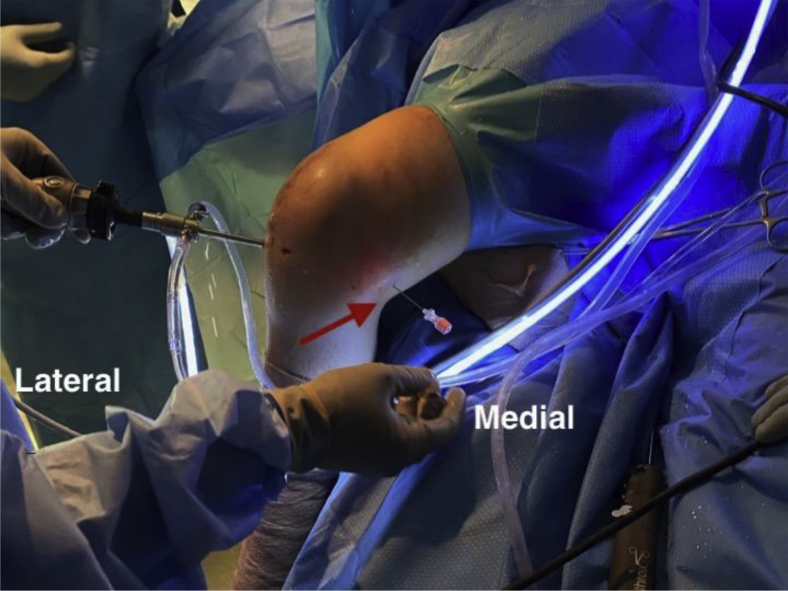
Fig 4.
Extra-articular view of spinal needle placement for posteromedial portal in soft spot between posterior oblique ligament and medial edge of medial head of gastrocnemius muscle (arrow) in right knee.
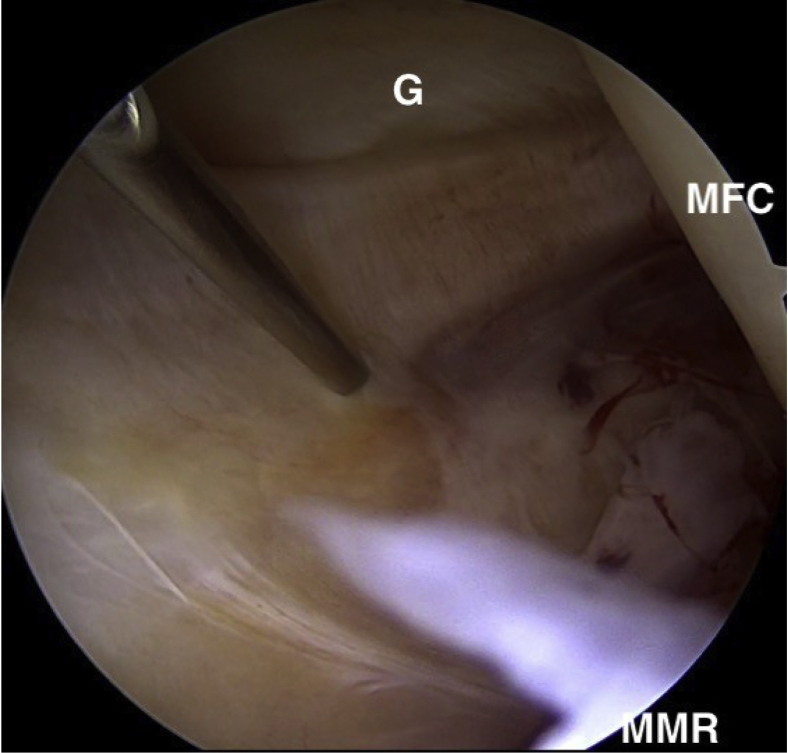
Fig 5.
Posteromedial spinal needle viewed intra-articularly, above posterior horn of medial meniscus, in right knee. (G, medial head of gastrocnemius; MFC, medial femoral condyle; MMR, medial meniscal ramp.)
Fig 6.
Extra-articular view of posteromedial portal capsulotomy being performed with straight snap in right knee. A guide for portal placement is looking for the light from the arthroscope (arrow).
Fig 7.
Introduction of half-pipe tool, allowing for exchange of straight snap for switching stick. The switching stick will allow dilation of the portal with a 7-mm dilator prior to placement of the 7-mm twist-in cannula.
Fig 8.
Extra-articular view of posteromedial cannula with shaver in place in right knee. The knee continues to be placed on a thigh bolster, improving access.
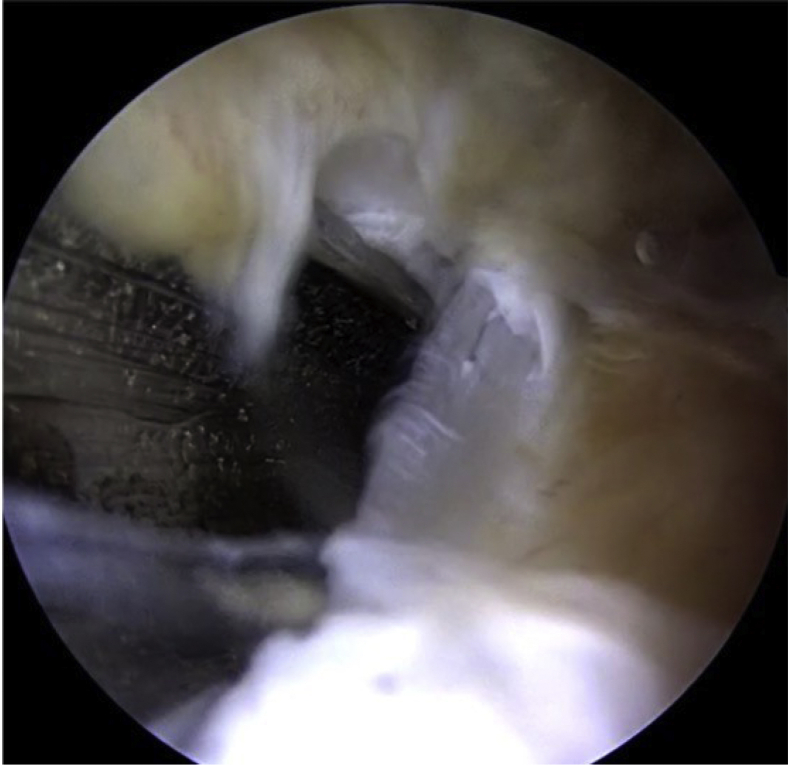
Fig 9.
Intra-articular view of 7-mm twist-in cannula (C) just after placement in right knee. (MFC, medial femoral condyle.)
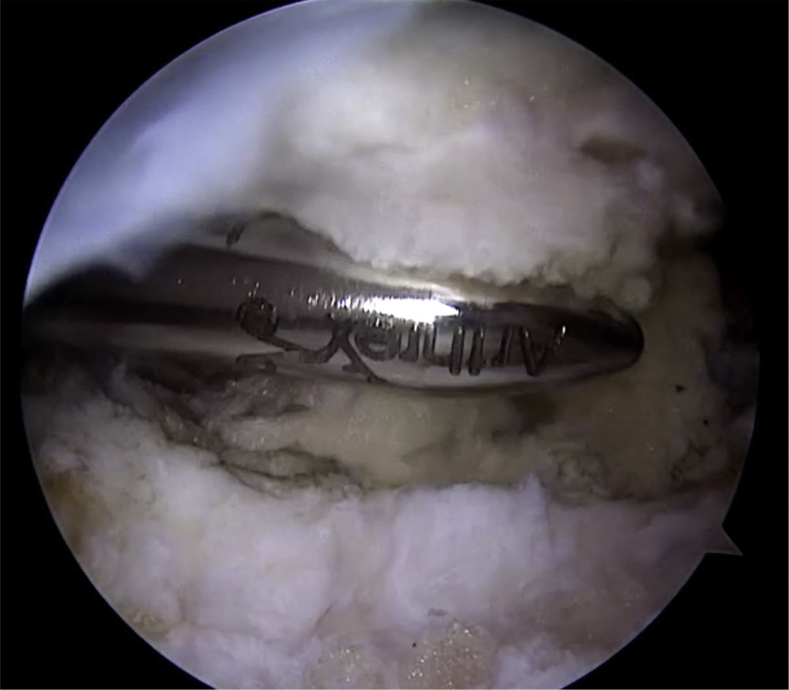
Fig 10.
Intra-articular view of torpedo shaver used to remove synovitis obstructing view of posterior capsule in right knee.
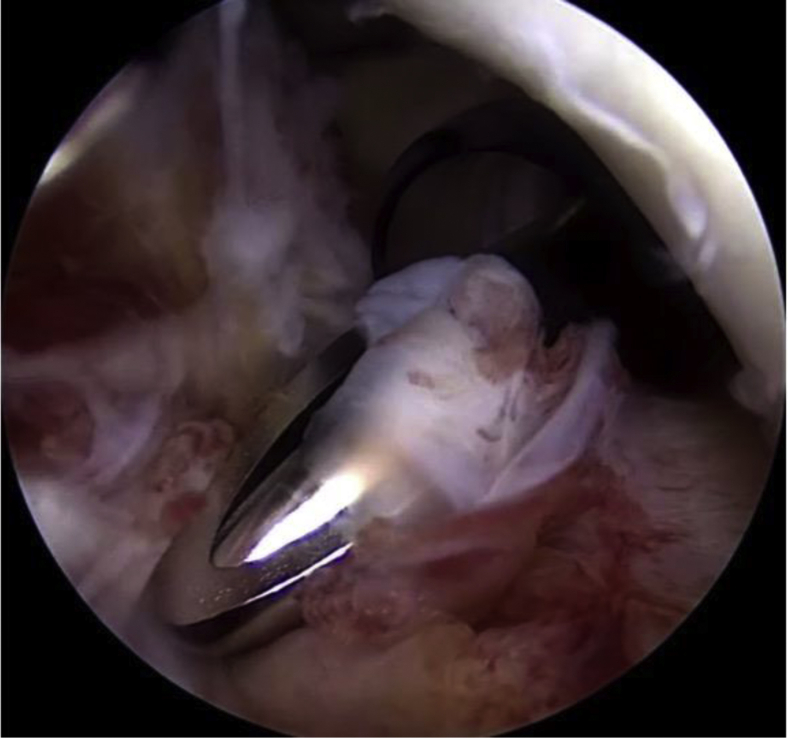
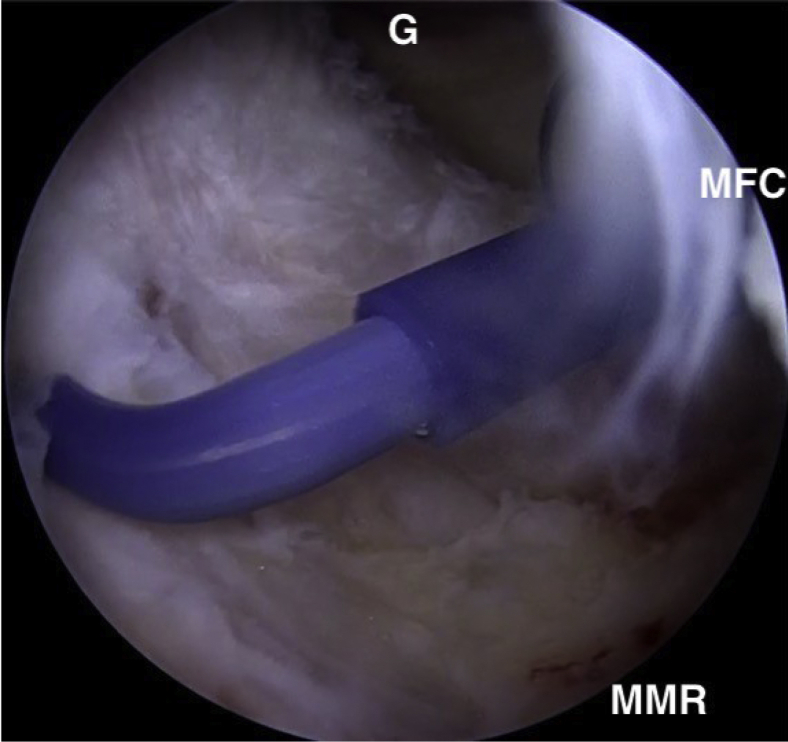
Fig 11.
Intra-articular view of 90° arthroscopic electrode beginning to release posteromedial capsule midway between femoral capsular attachment and meniscal attachment in right knee. (G, gastrocnemius tendon behind capsule; MFC, medial femoral condyle; MMR, medial meniscal ramp [just out of view].)
Fig 12.
Intra-articular view of beginning of posterior capsular release midway in right knee.
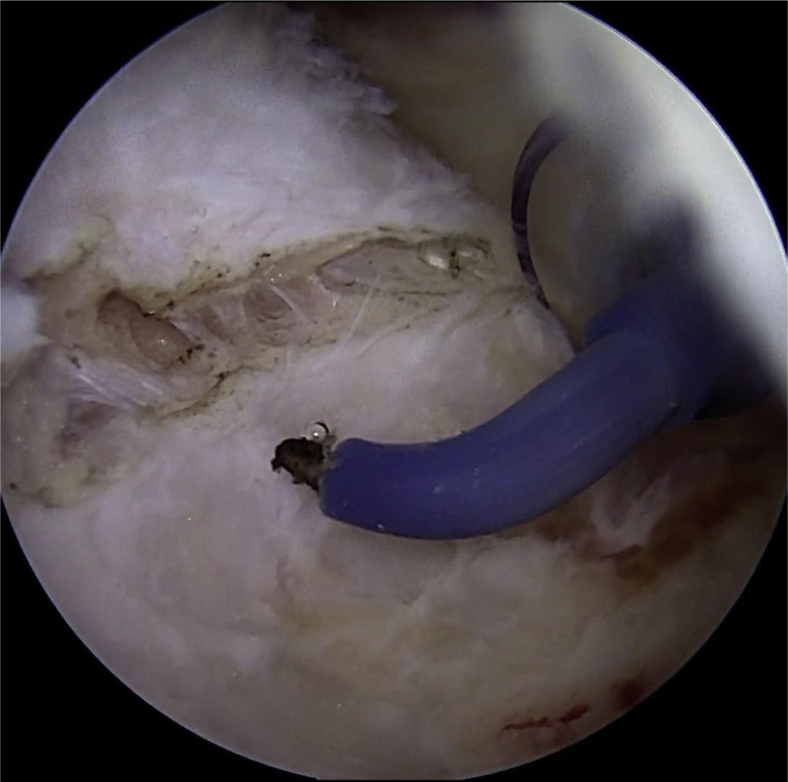
Fig 13.
Intra-articular view of torpedo shaver being used to gently debride free edges of posteromedial capsule in right knee.
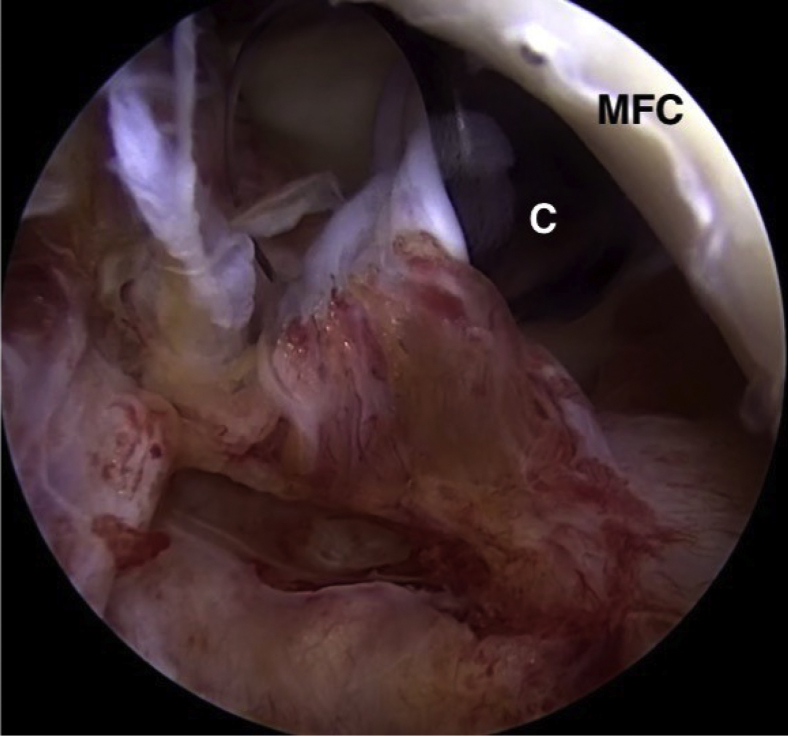
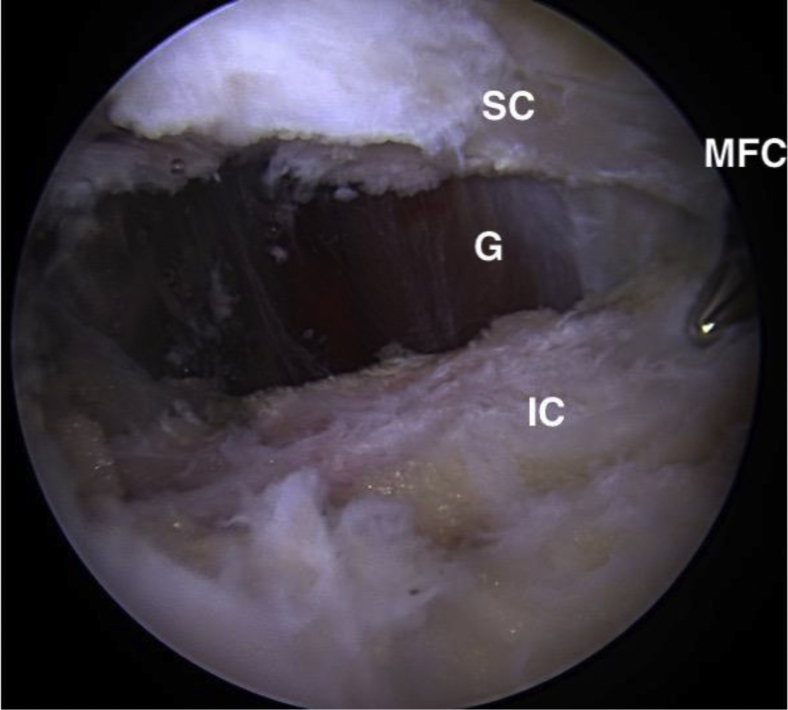
Fig 14.
View of completed posteromedial release. The medial gastrocnemius muscle and tendon (G) are visible. (IC, released inferior capsule leaflet; MFC, medial femoral condyle; SC, release superior capsule leaflet.)
Posterolateral Access and Capsular Release
The knee is maintained in 90° of flexion while hanging off the side of the bed. The posterolateral compartment viewed transcondylar through the anteromedial portal with the arthroscope between the anterior cruciate ligament and lateral femoral condyle as described by Kramer et al.11 Once the trocar is in the posterolateral compartment, the blunt obturator is removed, a 30° arthroscope is introduced, and an 18-gauge spinal needle is placed off the posterior aspect of the lateral femoral condyle (Figs 15 and 16) in the soft spot between the lateral edge of the lateral head of the gastrocnemius muscle and the fibular collateral ligament. It is important to stay anterior to the biceps femoris because the common peroneal nerve is posterior to it at this level. Once this position is confirmed with the spinal needle, its trajectory is noted and the needle is removed. Similarly to posteromedial portal establishment, a No. 15 surgical blade is used to make a skin nick and a straight snap is used to spread through subcutaneous tissues and create a capsular rent, followed by the introduction of an arthroscopic half-pipe tool (Fig 17). A blunt switching stick is introduced, and a 7-mm dilator is used to enlarge the capsular rent, followed by placement of a 7-mm twist-in cannula. Synovitis or adhesions obstructing a clear view of the posterolateral capsule are removed with a torpedo shaver. The aforementioned 90° arthroscopic hook probe electrode is introduced, and the capsule is sectioned midway between the femoral attachment and posterolateral meniscal attachment starting medially (Fig 18). The posterolateral capsule is typically thicker than the posteromedial capsule, so several passes may be required to complete the release. A shaver is used clean up the free edges of the capsule (Figs 19 and 20). At this point, the lateral gastrocnemius muscle and fat of the popliteal fossa should be visible (Fig 21). The posterior septum is left intact.
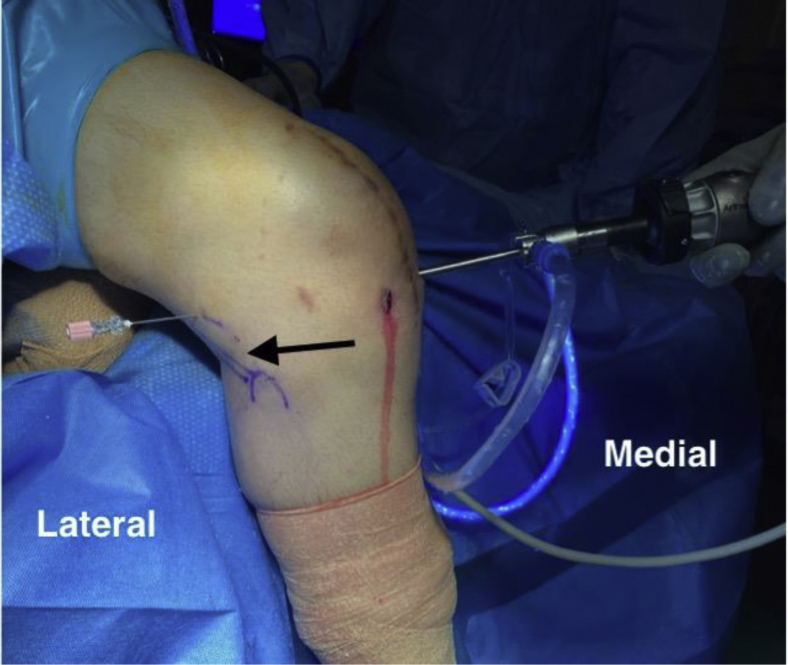
Fig 15.
Extra-articular view of spinal needle position for posterolateral portal, located in soft spot between lateral edge of lateral head of gastrocnemius muscle and fibular collateral ligament in right knee. The needle is placed anterior to the biceps femoris (arrow).
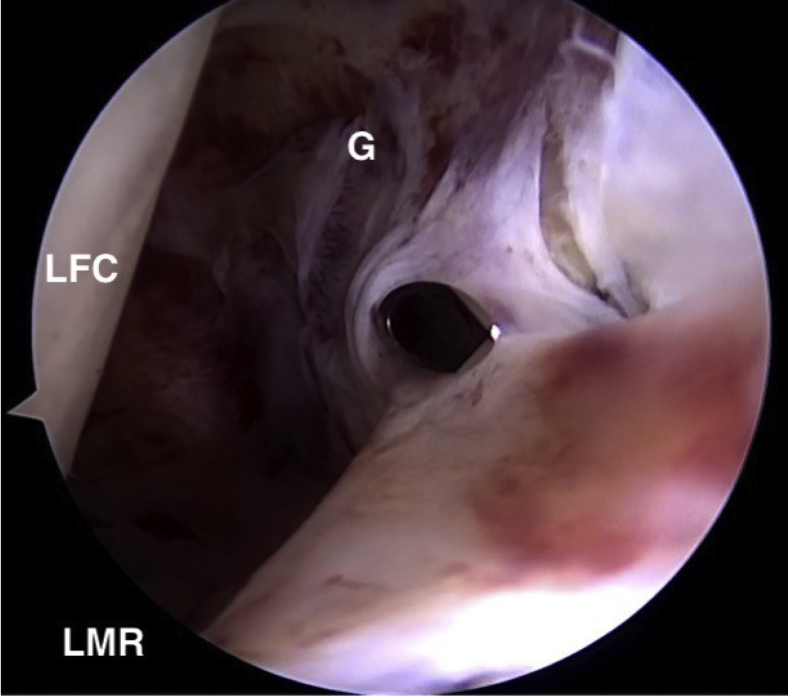
Fig 16.
Intra-articular view of spinal needle position for posterolateral portal, anterior to lateral head of gastrocnemius tendon in right knee. (G, lateral head of gastrocnemius deep to capsule; LFC, lateral femoral condyle; LMR, lateral meniscal ramp [just out of view].)
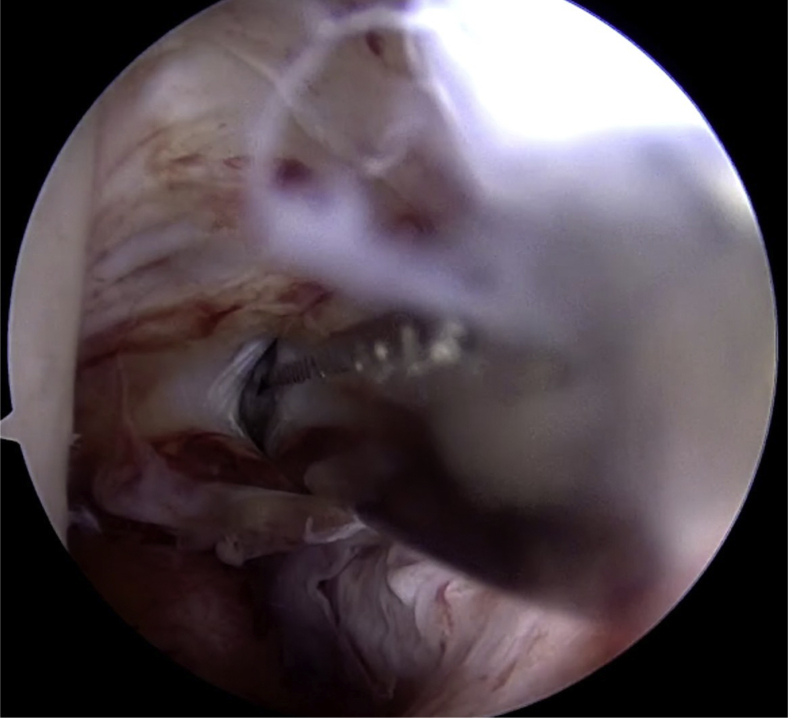
Fig 17.
Intra-articular view of straight snap making capsulotomy for posterolateral portal in right knee.
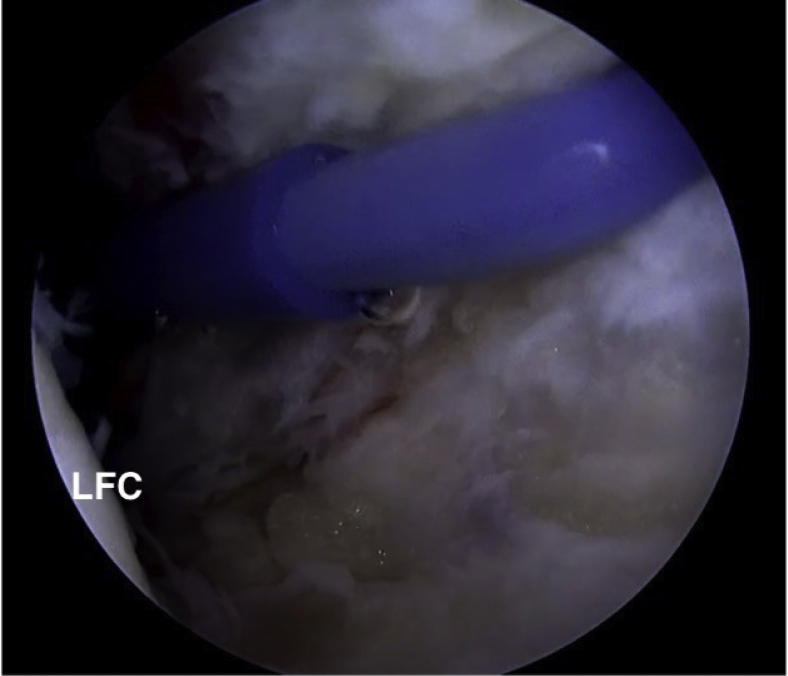
Fig 18.
Intra-articular view of 90° hook probe being used to begin posterolateral capsulotomy midway between its femoral and meniscal attachments in right knee. (LFC, lateral femoral condyle.)
Fig 19.
Intra-articular view of torpedo shaver being used to debride edges of released posterolateral capsule in right knee.
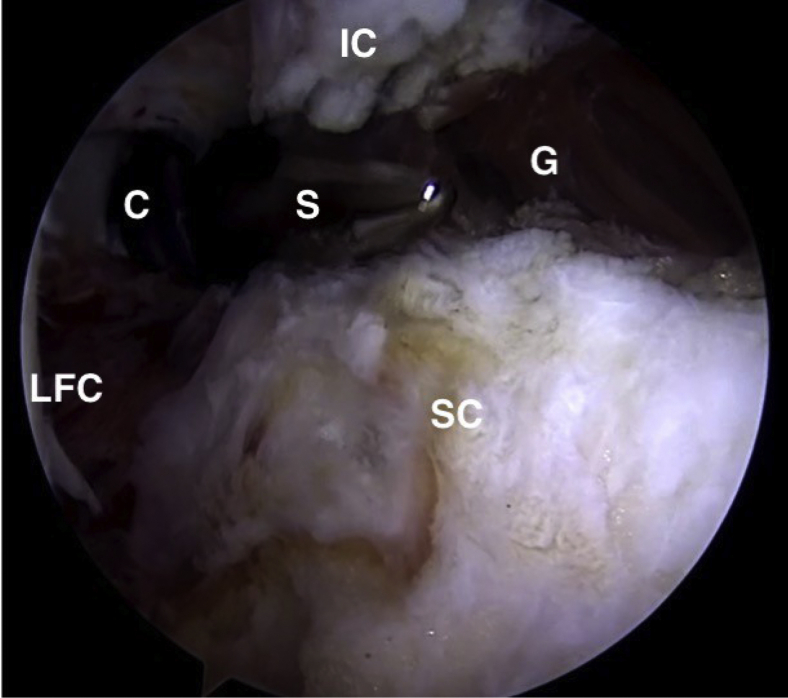
Fig 20.
Torpedo shaver (S) debriding edges of posterolateral capsule. (C, 7-mm cannula; G, gastrocnemius muscle; IC, released inferior capsular leaflet; LFC, lateral femoral condyle; SC, released superior capsular leaflet.)
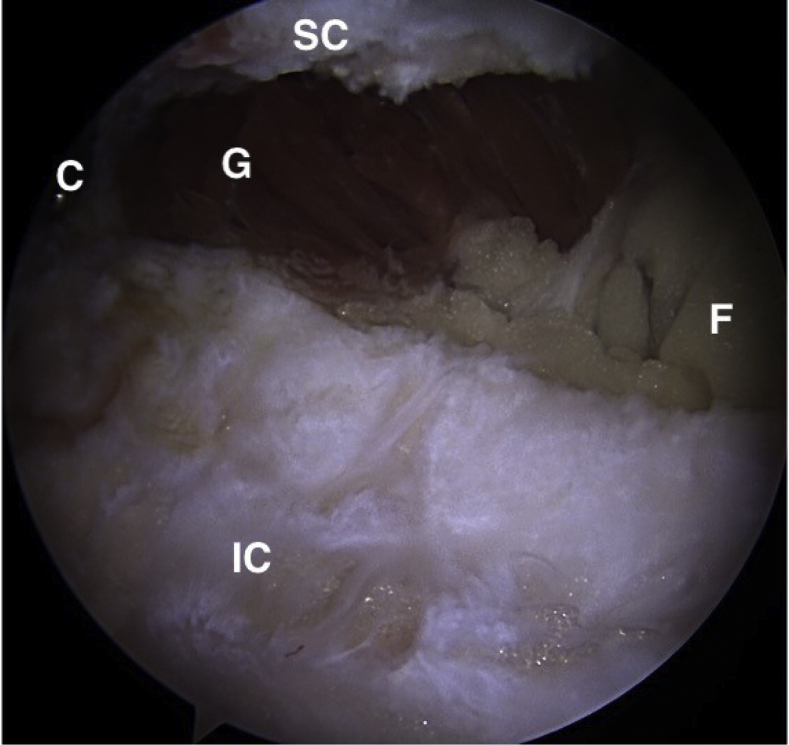
Fig 21.
Completed posterolateral release in right knee with visible gastrocnemius muscle (G) and popliteal fossa fat (F). (C, 7-mm cannula; IC, released inferior capsular leaflet; SC, released superior capsular leaflet.)
Final Manipulation and Final Range of Motion
Once the posteromedial and posterolateral releases are complete, a final manipulation under anesthesia is performed until symmetrical knee extension is obtained.
Postoperative Rehabilitation
Postoperatively, patients are instructed to perform gravitational hyperextension by floating the knee with the calf on at least 2 pillows several times per day for at least 6 weeks after surgery. Patients begin rehabilitation under the control of a physical therapist 3 times per week for 6 weeks. Ice packs can aid pain control and help during hyperextension exercises. Patients typically use crutches for 2 to 3 days after surgery.
Discussion
Patient satisfaction and outcomes can be significantly affected by knee flexion contractures after knee surgery, after trauma, or due to arthritis. When extension deficits persist despite extensive and exhausting conservative treatments, a quick, safe, and reliable way to release the posterior capsule is a necessary tool for one to have in one’s quiver. An arthroscopic release also offers the advantage of being minimally invasive, which aids in the acceleration of recovery and improved pain control over open techniques. As little as 5° to 10° of extension loss after anterior cruciate ligament reconstruction can cause gait and patellofemoral irritability and as little as 15° of extension loss can cause increased shear forces and biomechanical overload, which may have long-term arthritic consequences.3,13 Posterior capsular releases for extension deficits have been shown in the literature to be safe and effective with low complication rates.6,7,9,14 The described technique offers many advantages and few limitations (Table 1). Several reported techniques describe release of the posterior septum, but we have found satisfactory increases in knee extension without releasing this structure.14 Avoiding release of the septum further decreases the risk to the popliteal neurovascular bundle and medial genicular artery. Knowledge of the location of the peroneal nerve posterior to the biceps femoris muscle and the sartorial branch of the saphenous nerve posterior to the sartorius muscle12 minimizes the risk of damage to these structures during posterolateral and posteromedial portal placement.
Table 1.
Advantages and Limitations of Technique for Posterior Capsular Release
| Advantages |
| The technique is easy, safe, and reproducible. |
| The technique is minimally invasive with improved recovery and pain control over open techniques. |
| Adequate distances to at-risk neurovascular structures are achieved. |
| Standard arthroscopy instruments are used. |
| Limitations |
| Knowledge of the posterior knee anatomy is required to minimize neurovascular risk to the saphenous nerve and vein medially and peroneal nerve laterally. |
| An aggressive release near the midline into and past the septum may endanger the popliteal neurovascular bundle. |
In summary, this technique of directly visualized arthroscopic posteromedial and posterolateral capsular release can serve as an important tool that is safe and effective to use in patients in whom full knee extension has failed to be achieved with conservative treatments alone. Significant improvement in patient knee motion can be achieved with this procedure, and little risk is posed to patients when the performing surgeon maintains careful attention to relevant anatomy and arthroscopic principles (Table 2).
Table 2.
Pearls and Pitfalls of Technique for Posterior Capsular Release
| Pearls |
| Use of a bolster under the knee increases posteromedial access. |
| Slight valgus stress can aid in transcondylar posteromedial arthroscope placement, whereas slight varus stress can aid in posterolateral placement. |
| The procedure should be performed at 90° to increase the distance of the neurovascular bundle from the capsule. |
| If needed, use of 70° arthroscope can further improve visualization. |
| A smooth shaver should be used rather than a toothed shaver to lower the risk of overly aggressive shaving. |
| Placement of the posteromedial or posterolateral portals can be aided by visualizing the arthroscope light source through the skin (Fig 6). |
| Pitfalls |
| Knee positioning in 90° of flexion is required to access the posterior knee. |
| Osteophytes in patients with severe arthritis may limit posterior-compartment access. |
| Immediate and continued rehabilitation is important to prevent recurrence of contractures. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.B.R. is a consultant for Arthrex, outside the submitted work. The Taos Orthopaedic Institute research foundation receives industry support from Arthrex, Smith & Nephew, Breg, Medacta, and DonJoy. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique for posterior capsular release. As shown in a right knee, the release begins with anterolateral trans-notch placement of the arthroscope to view and establish a posteromedial portal. A torpedo shaver is used to debride any synovitis, and a 90° hook probe is used to section the capsule. A posterolateral portal is then established, viewing through the anteromedial portal through the notch. Synovitis is again cleared, and the capsule is released with the hook probe. The septum is left intact. After release, a manipulation under anesthesia is performed on the knee.
References
- 1.Mayr H.O., Weig T.G., Plitz W. Arthrofibrosis following ACL reconstruction—Reasons and outcome. Arch Orthop Trauma Surg. 2004;124:518–522. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne K.D., Urch S.E., Gray T., Freeman H. Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. Am J Sports Med. 2012;40:108–113. doi: 10.1177/0363546511423639. [DOI] [PubMed] [Google Scholar]
- 3.Harato K., Nagura T., Matsumoto H., Otani T., Toyama Y., Suda Y. Knee flexion contracture will lead to mechanical overload in both limbs: A simulation study using gait analysis. Knee. 2008;15:467–472. doi: 10.1016/j.knee.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Werner B.C., Cancienne J.M., Miller M.D., Gwathmey F.W. Incidence of manipulation under anesthesia or lysis of adhesions after arthroscopic knee surgery. Am J Sports Med. 2015;43:1656–1661. doi: 10.1177/0363546515578660. [DOI] [PubMed] [Google Scholar]
- 5.Malinowski K., Goralczyk A., Hermanowicz K., LaPrade R.F., Wiecek R., Domzalski M.E. Arthroscopic complete posterior capsulotomy for knee flexion contracture. Arthrosc Tech. 2018;7:e1135–e1139. doi: 10.1016/j.eats.2018.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wierer G., Runer A., Gfoeller P., Fink C., Hoser C. Extension deficit after anterior cruciate ligament reconstruction: Is arthroscopic posterior release a safe and effective procedure? Knee. 2017;24:49–54. doi: 10.1016/j.knee.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 7.Pujol N., Boisrenoult P., Beaufils P. Post-traumatic knee stiffness: Surgical techniques. Orthop Traumatol Surg Res. 2015;101:S179–S186. doi: 10.1016/j.otsr.2014.06.026. (suppl) [DOI] [PubMed] [Google Scholar]
- 8.Dean C.S., Chahla J., Makula J.D., Mitchell J.J., LaPrade R.F. Arthroscopic posteromedial capsular release. Arthrosc Tech. 2016;5:e495–e500. doi: 10.1016/j.eats.2016.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pace J.L., Wahl C.J. Arthroscopy of the posterior knee compartments: Neurovascular anatomic relationships during arthroscopic transverse capsulotomy. Arthroscopy. 2010;26:637–642. doi: 10.1016/j.arthro.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Makridis K.G., Wajsfiz A., Agrawal N., Basdekis G., Djian P. Neurovascular anatomic relationships to arthroscopic posterior and transseptal portals in different knee positions. Am J Sports Med. 2013;41:1559–1564. doi: 10.1177/0363546513492704. [DOI] [PubMed] [Google Scholar]
- 11.Kramer D.E., Bahk M.S., Cascio B.M., Cosgarea A.J. Posterior knee arthroscopy: Anatomy, technique, application. J Bone Joint Surg Am. 2006;88-A:110–121. doi: 10.2106/JBJS.F.00607. (suppl 4) [DOI] [PubMed] [Google Scholar]
- 12.McGinnis M.D., Gonzalez R., Nyland J., Caborn D.N.M. The posteromedial knee arthroscopy portal: A cadaveric study defining a safety zone for portal placement. Arthroscopy. 2011;27:1090–1095. doi: 10.1016/j.arthro.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 13.Aglietti P., Buzzi R., D’Andria S., Zaccherotti G. Patellofemoral problems after intraarticular anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1993;288:195–204. [PubMed] [Google Scholar]
- 14.Ohishi T., Takahashi M., Suzuki D., Matsuyama Y. Arthroscopic approach to the posterior compartment of the knee using a posterior transseptal portal. World J Orthop. 2015;6:505–509. doi: 10.5312/wjo.v6.i7.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for posterior capsular release. As shown in a right knee, the release begins with anterolateral trans-notch placement of the arthroscope to view and establish a posteromedial portal. A torpedo shaver is used to debride any synovitis, and a 90° hook probe is used to section the capsule. A posterolateral portal is then established, viewing through the anteromedial portal through the notch. Synovitis is again cleared, and the capsule is released with the hook probe. The septum is left intact. After release, a manipulation under anesthesia is performed on the knee.