Abstract
The coronavirus disease 2019 pandemic has meant that there is growing pressure on hospital resources, not least the availability of appropriate personal protective equipment (PPE), particularly face masks and respirator masks. Within the field of orthopaedic surgery, it is a common sight to see surgeons wearing ‘space suits’ (SSs) which comprise a helmet, hood and surgical gown.
In this study, the authors made modifications to two different SS systems to incorporate a high-efficiency particulate air (HEPA) filter into the fan inlet to assess their potential as re-usable PPE systems for surgeons with regard to protection from a virus spread via respiratory droplets. The testing was carried out using particle counters upstream and downstream on a mannequin wearing two different SS systems with and without modifications to the fan inlet.
The results show that using a layer of HEPA filter, cut to size and sealed to the fan inlet in the helmet, will reduce downstream particulates at the user's mouth by >99.5%; this is equivalent to a respirator mask. HEPA filter material is relatively cheap and can be used repeatedly, making this a viable alternative to disposable, and even resterilized, respirator masks in the setting of a respiratory-droplet-spread viral pandemic.
Keywords: Personal protective equipment, High-efficiency particulate air filter, COVID-19
Introduction
The emergence of the coronavirus disease 2019 (COVID-19) pandemic, affecting most of the world's population, has led to concern regarding an international shortage of personal protective equipment (PPE). The World Health Organization (WHO), in recent guidance with respect to rational use of PPE, stated that ‘The current global stockpile of PPE is insufficient, particularly for medical masks and respirators’ [1]. Current advice from a number of bodies recommends the use of FFP2 or N95 respirator masks with eye protection, as well as gloves and gowns, for specific procedures, including orthopaedic surgery [[2], [3], [4]]. More recently, guidance for all healthcare workers (HCWs) has advised that any person working within 2 m of any patient with suspected or confirmed COVID-19 should be wearing a respirator mask [[4], [5], [6]]. The use of respirator masks, such as N95 and FFP2 which provide at least 95% and 94% filtration of 0.3-μm particles, is advised as they are the best and most broadly available masks in terms of particle filtration, and offer a seal to the face. However, these masks are not custom made to fit the face of each individual, and face-fitting procedures are required which have limitations [7].
The mean diameter of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has been reported to be 78 nm [8]. The filter efficiencies of the N95 and FFP2 respirator masks relate to their ability to filter submicron particles effectively, and are standardized against uncharged particles of sodium chloride measuring 300 nm or airborne Staphylococcus aureus [7,9]. Studies have questioned the validity of using these masks to provide protection against viruses, and suggested that the performance of such masks may underestimate the penetration of nanosized virions [7]. High-efficiency particulate air (HEPA) filters are standardized against the same-sized particles for their certification, and are 99.97% efficient for filtration. A study by the National Aeronautics and Space Administration showed that HEPA filters are also efficient for smaller particles (c. 10 nm) [10].
The possibility of a global shortage of PPE, including face masks, has led to bidding wars between governments to acquire PPE for HCWs, as stated by the Irish Government [11]. With high reliance on external supplies of PPE, there is an urgent need to design ways to be more self-reliant should this particular pandemic endure or resurface, and to be prepared for future pandemics. Protocols are being developed with regards to the standardization of sterilization of face masks that show acceptable retention of filtration efficiency after five cycles [12,13]. There are limitations with regard to resterilization, namely that the face masks may suffer mechanical damage during the sterilization process, disposable masks are often not face-fit for the individual, and the fit may be damaged by the process. Face masks are not sterilized if they are grossly contaminated; in the setting of orthopaedic surgery, most masks cannot be re-used as there is often gross contamination of PPE with blood spatters and splash-back from lavage. Orthopaedic surgery generates aerosolized human tissue, including bone and blood, through the use of power tools during procedures. These aerosol-generating procedures, and the inability to resterilize common respirator masks due to contamination with blood, prompted the current authors to look at using the ‘space suits’ (SSs) used in orthopaedic surgery as an alternative to re-usable masks.
The research question in this paper was whether retrofitting a Stryker helmet with a HEPA filter at the fan inlet, draped in the usual hood and gown, would improve the SS to the point of being comparable to a N95 or equivalent mask. This was a proof-of-concept study using a mannequin to isolate the effectiveness of the retrofitted helmet with regard to its ability to filter air coming into the SS.
Methods
Study set-up
The experimental set-up of this research involved a mannequin (head and torso mounted on a stand to measure 180 cm in height) used for cardiopulmonary resuscitation training as the subject in all tests. The mannequin was cleaned with chlorohexidine scrub prior to the experiment, and all orifices other than the mouth and nose on the mannequin were sealed with Steri-Drape™ (3M, Saint Paul, MN, USA). The particle detector was placed at the mouth and sealed with leucoplast sleek tape around the detector and mouth, isolating it from the internal tubing of the mannequin, as well as taping over the nostrils of the mannequin (see Figure 1 ). The detector tubing was fed out through the bottom of the mannequin and sealed with Steri-Drape.
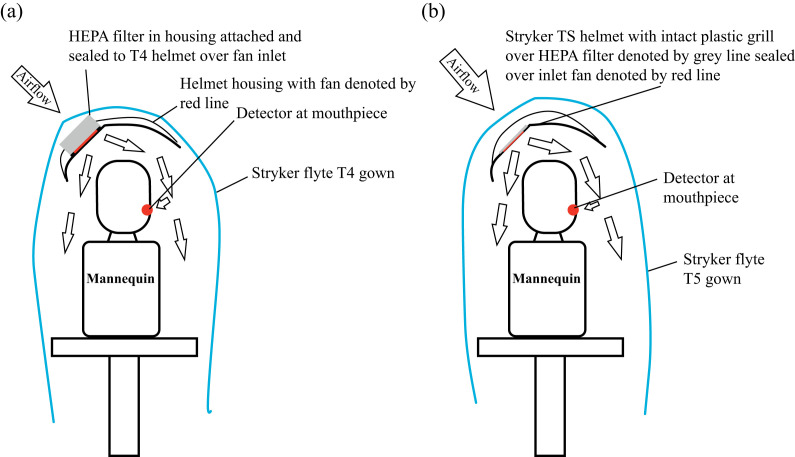
Figure 1.
Experimental set-up using a mannequin with a particulate detector sealed at the mouth of the mannequin.
Testing was performed in the orthopaedic theatre initially, but the background particle count was found to be too low to discern a reliable difference at the downstream penetration detector. Testing was subsequently performed in the adjoining anaesthetic room, and all doors and exhaust vents were closed but not sealed. An ambient recording was made to ensure that the distribution of background particulate was equal at both points for the detector in relation to the mannequin without any donned PPE, which was confirmed.
The PPE systems used in this study were Stryker Flyte T4 and T5 [14]. Both systems have a grill over the fan inlet which prevents the hood material being sucked into the inlet. The T4 helmet has a grill overlying the fan inlet that is not amenable to removal and replacement without damaging the plastic housing for this system. The grill was cut off and housing containing a HEPA filter with a rubber gasket seal was mounted over the fan inlet (see Figure 2 a).
Figure 2.
Schematic demonstrating experimental set-up for modified space suits. (a) Modified Stryker Flyte T4 helmet with housing and high-efficiency particulate air (HEPA) filter fitted at fan inlet. (b) Modified Stryker Flyte T5 helmet with HEPA filter fitted at fan inlet beneath plastic grill.
The T5 helmet has a similar grill but this can be removed and replaced without damage to the housing. Figure 2b illustrates the experimental set-up for the modified T5 system. This allowed for a HEPA filter to be placed over the fan inlet and sealed at the periphery to the helmet, with the grill replaced to prevent the hood being sucked into the fan (see Figure 3 ). The HEPA filter material was taken from the SoniQ II™ system (Vokes Air, Ludwigsburg, Germany) [15].
Figure 3.
Stryker Flyte T5 helmet with high-efficiency particulate air filter cut to size for fan inlet with plastic grill intact.
Particulate detection
Particulate testing was performed by a certified engineer who commissions ventilation systems for surgical healthcare infrastructure in this jurisdiction. The detection equipment used, Aerotrak® Handheld Particle Counter Model 9306 (TSI, Shoreview, MN, USA), is the industry standard; it generates a 2.83 L/min intake and was set to read six channels to enable reading of all particles in the size range 0.3–10 μm. The testing protocol for each measurement of particulate penetration recorded at the mouth detector involved four upstream challenge samples taken for 60 s each at either the inlet to the Stryker hood or the same point in space relative to the head for testing without wearing the hood. Four samples were taken upstream to ensure that the upstream challenge was consistent, and this required that all four readings were within 15% of the mean, which they were for all tests. The downstream detector reading was also taken over 60 s and at least three readings were taken for each experimental set-up outlined below. Ten readings were taken for the configurations using the modified hoods.
The particulate counts were collected and tabulated using Excel (Microsoft Corp., Redmond, WA, USA), and statistical analysis was performed with comparison of test configurations using Student's t-test.
The test configurations were performed as follows:
-
•
Ambient test – testing of background particulate to ensure similar readings upstream and downstream with no PPE on the mannequin. This test was required to ensure no difference in ambient distribution of particles around the mannequin, which was confirmed.
-
•
Configuration 1. A Stryker T4 helmet and hood and a standard surgical gown around the neck without the fan running.
-
•
Configuration 2. A Stryker T4 helmet and hood and a standard surgical gown around the neck with fan running at medium speed.
-
•
Configuration 3. A Stryker T4 helmet retrofitted with a mount for a HEPA filter, with a rubber gasket used to seal the mounted HEPA filter to the plastic helmet (see Figure 2), and draped with the T4 hood and standard surgical gown with the fan running at medium speed.
-
•
Configuration 4. A Stryker T5 helmet and hood and a standard surgical gown around the neck without the fan running.
-
•
Configuration 5. A Stryker T5 helmet and hood and a standard surgical gown around the neck with the fan running at medium speed.
-
•
Configuration 6. A Stryker T5 helmet with the same HEPA filter material cut to fit over the fan inlet and sealed to the helmet housing with sealant tape to prevent any filter bypass (see Figure 3), and then draped with the hood and standard surgical gown around the neck with the fan running at medium speed.
Effect of modification on ventilation
In order to investigate gas levels within the modified T5 system and the non-modified T5 system with use, the second author (JH) wore each SS with serial collection of data from a standard anaesthetic machine used in the operating theatre (GE Datix Ohmeda Asyis & GE Carescape B650, Madison, Wisconsin, USA). The experiment was performed in an operating theatre with a functional laminar airflow system. A narrow (1.2-mm diameter) PVC CO2 sample tube, connected to a multi-gas analyser (GE Carescape E-CAiO Respiratory Module, Helsinki, Finland), was placed inside the hood at the level of the participant's mouth to measure end-tidal carbon dioxide (ETCO2) and end-tidal oxygen (ETO2) continuously. This side-stream gas analyser draws 150 mL/min from the user's airway gas, where the CO2 concentration is calculated via absorption of infra-red light, according to the Beer–Lambert law, and oxygen concentration is calculated using paramagnetic analysis. No additional mask was worn. Measures for ETCO2, ETO2 and fraction of inspired oxygen (FiO2) were recorded at 5-min intervals with both the modified T5 system hood and the non-modified helmet.
Results
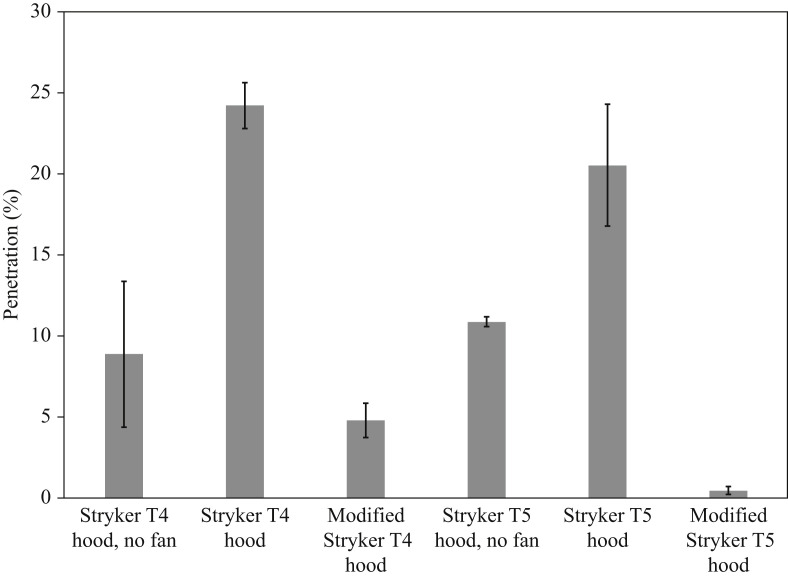
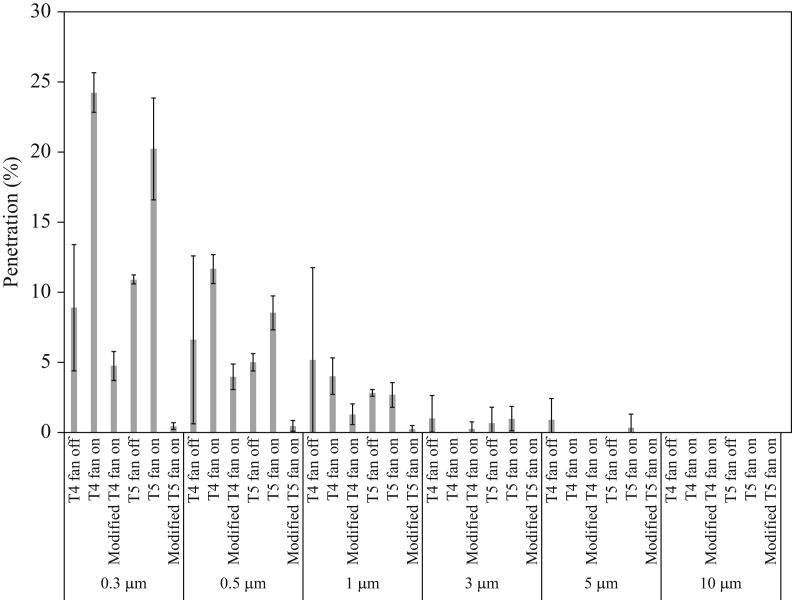
Table I shows the results found with regard to the mean percentage penetration at the downstream detector, and the associated standard deviation, for the tests. All test configurations were carried out in triplicate. For test configurations using the Stryker Flyte T5 system without a filter and the two generations of Stryker Flyte system with HEPA filter modifications, a total of 10 readings were taken. Table II presents the statistical analysis using Student's t-test and the significance of the differences observed. Figure 4 illustrates the results of overall percentage downstream penetration of all particles (range 0.3–10 μm), and Figure 5 provides a breakdown of each detection channel for the spectrum of particle sizes detected for each experimental set-up.
Table I.
Mean percentage downstream penetration of test configurations
| Configuration 1: Stryker T4 hood, no fan | Configuration 2: Stryker T4 hood | Configuration 3: modified Stryker T4 hood | Configuration 4: Stryker T5 hood, no fan | Configuration 5: Stryker T5 hood | Configuration 6: modified Stryker T5 hood | |
|---|---|---|---|---|---|---|
| Mean percentage downstream penetration | 8.89 | 24.24 | 4.79 | 10.90 | 20.54 | 0.46 |
| Standard deviation percentage downstream penetration | 4.50 | 1.41 | 1.06 | 0.30 | 3.78 | 0.24 |
Table II.
Comparison of percentage downstream penetration between test configurations
| Comparative t-tests for percentage penetration |
Test configuration with lower percentage penetration | Difference in percentage penetration | P-value |
|---|---|---|---|
| Test configurations | |||
| 1 vs 2 | 1 | 15.35% | 0.0049 |
| 2 vs 3 | 3 | 19.45% | <0.0001 |
| 2 vs 5 | 5 | 3.7% | 0.13 |
| 5 vs 6 | 6 | 20.08% | <0.0001 |
| 3 vs 6 | 6 | 4.33% | <0.0001 |
Figure 4.
Results of mean total downstream penetration (error bars represent +/− one standard deviation) for the testing configurations described.
Figure 5.
Results of mean downstream filtration by size for individual channels recorded using the Aerotrak Particle Counter (error bars represent +/− one standard deviation).
For the Stryker Flyte T4 system, one can see from these results that the SS alone provides a certain degree of protection from outside particulates, with only 8.89% (σ = 4.96%) penetration. Once the fan was turned on within the SS, downstream penetration increased to 24.24% (σ = 1.41%). With the modification of the HEPA filter at the inlet system, downstream penetration was reduced significantly to 4.79% (σ = 1.06%).
For the Stryker Flyte T5 system, the SS alone provides a similar degree of protection as the T4 system at 10.9% (σ = 0.3%); the difference was not significantly different. Similar to the T4 system above, once the fan was turned on, the downstream penetration increased to 20.54% (σ = 3.78%); again, this was not significantly different to the T4 system with the fan operating. With the modification of the HEPA filter at the inlet system, downstream penetration was reduced to 0.46% (σ = 0.24%), which was significantly better than all other test configurations and offers particulate filtration similar to FFP3 and N99 or other equivalent respirator masks. Figure 5 illustrates the downstream penetration for each experimental set-up for each of the six channels recorded by the Aerotrak Particle Counter, showing that there was <0.5% penetration of all particle sizes for the modified T5 system.
An additional experiment was run with the addition of an impenetrable cover over the hood except for the area over the inlet. This did not significantly improve efficiency, leading to the conclusion that the positive pressure experienced in the SS provides enough pressure to negate any possible infiltration of particulate through the hood material not directly over the fan inlet.
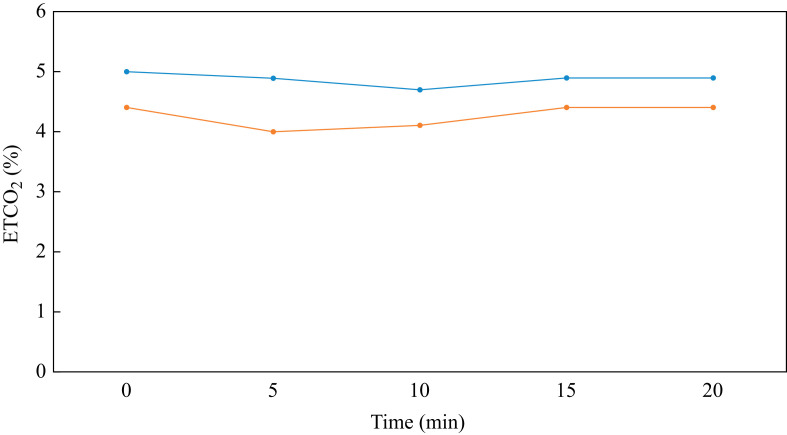
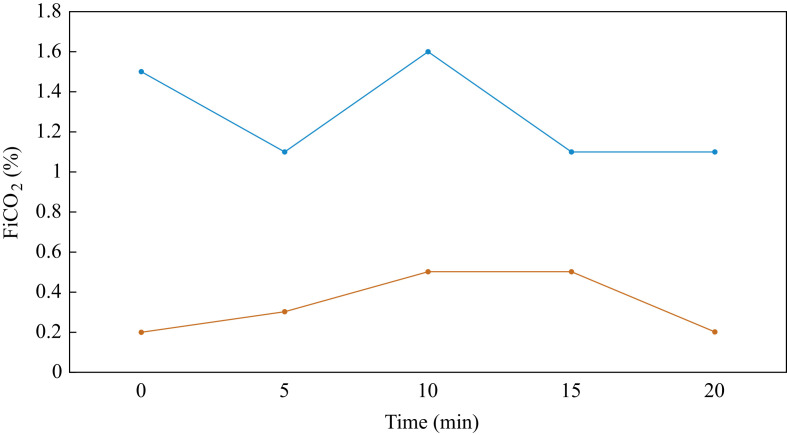
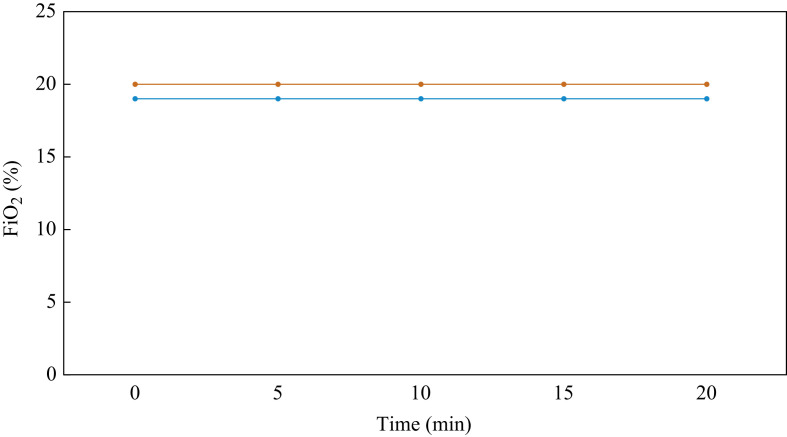
The results of gas measurement testing are outlined in Table III and illustrated in Figure 6, Figure 7, Figure 8 . ETCO2 remained steady throughout the recording. The level of ETCO2 was higher in the modified T5 system compared with the unmodified T5 system (see Figure 6). FiO2 appeared to be slightly lower for the modified T5 system compared with the non-modified T5 system. FiCO2, the inspired fraction of carbon dioxide, is normally 0. It was observed that the use of both systems resulted in an increase in FiCO2 (see Figure 7). The normal FiO2 level is 21%, and the readings demonstrated a reduction in FiO2 with use of both the modified and non-modified SSs (see Figure 8). The user did report mild discomfort when wearing the modified hoods; however, this was rated equivalent to wearing a regular FFP3 mask.
Table III.
Results of gas testing within modified and non-modified T5 systems (fan switched on)
| Time (min) | Modified T5 system |
Non-modified T5 system |
||||
|---|---|---|---|---|---|---|
| ETCO2 (%) | FiCO2 (%) | FiO2 (%) | ETCO2 (%) | FiCO2 (%) | FiO2 (%) | |
| 0 | 5 | 1.5 | 19 | 4.4 | 0.2 | 20 |
| 5 | 4.9 | 1.1 | 19 | 4 | 0.3 | 20 |
| 10 | 4.7 | 1.6 | 19 | 4.1 | 0.5 | 20 |
| 15 | 4.9 | 1.1 | 19 | 4.4 | 0.5 | 20 |
| 20 | 4.9 | 1.1 | 19 | 4.4 | 0.2 | 20 |
ETCO2, end-tidal carbon dioxide; FiCO2, fraction of inspired carbon dioxide; FiO2, fraction of inspired oxygen.
Figure 6.
Comparison of modified (blue line) and non-modified (orange line) T5 systems for variation of end-tidal carbon dioxide (ETCO2) (%) with time.
Figure 7.
Comparison of modified (blue line) and non-modified (orange line) T5 systems for variation of fraction of inspired carbon dioxide (FiCO2) (%) with time.
Figure 8.
Comparison of modified (blue line) and non-modified (orange line) T5 systems for variation of fraction of inspired oxygen (FiO2) (%) with time.
Discussion
This study found that the SSs operating without a fan offered close to 90% reduction in downstream penetration of particles; however, once the fan was turned on, downstream penetration increased to 20–25% for the T4 and T5 systems. Implementation of modifications using a HEPA filter at the fan inlet led to a significant reduction in downstream penetration; for the T5 system, the percentage downstream penetration reduced to <0.5%, which is comparable with that offered by respirator masks. The HEPA filters have a significantly longer life-span than respirator masks, even with potential resterilization of masks [12,13]. This was a pilot study of potential modification of SSs with HEPA filters, and further testing is required to confirm the recommended life-span for use, establish timing of regular quality assurance checks on the efficacy of the filters, and investigate possible further modification of the inlet to protect the HEPA filter material [16,17].
Derrick et al. previously investigated the feasibility of SSs with regards to their use for PPE [18]. They concluded that the Stryker T4 suit alone was insufficient to protect HCWs from submicron particles [18], which was confirmed by the present results for non-modified SSs. Their comparative was volunteers using either a Stryker T4 SS or a combination of an N100 filtering facepiece respirator with a surgical face mask and a full-face shield. In their methodology, the detector was placed in the breathing zone for the SS, 1 cm below the bottom edge of the transparent face piece, whilst for the facepiece respirator, the probe was passed through both the respirator and covering surgical mask 1 cm to the right of the valve. There were a number of confounders to the results observed, potentially due to in-vivo testing, as follows:
-
•
The detector in the surgical mask did not necessarily replicate the possible true particles entering the mouth, allowing for possible entrainment of surrounding air if there was even the slightest breach in face-fit [7].
-
•
Similarly, the detector for the SS was placed in the breathing area, not at the mouth, and the study design would not account for the possibility of particles from the subject's hair or skin counting towards the readings, given that the SS offers a positive pressure environment from the top of the hood downwards.
Currently, for most jurisdictions, the recommendation is for the use of respirator masks when dealing with suspected or confirmed cases of SARS-CoV-2 [4]. A respirator mask is reliant on the adequacy of the face-fit; however, studies have shown that the adequacy of a face-fit, even in controlled environments, is variable and can depend on the respiratory rate of the user as well as their position [7]. Previous work has been undertaken regarding SSs in relation to the effect of positive pressure exerted within the SS, and the pressure that this can exert all the way down to any breach, including the glove–sleeve interface [19,20]. Although these tests were performed on a static mannequin, the air provided to the user was that of a highly filtered positive pressure source with <0.5% particle penetration which was not reliant on a face-fit. Rather, the mechanical seal was protected by plastic housing in the helmet which remained static.
The reason why a mannequin was used in this study to assess the efficiency of SSs as PPE using detection methods for downstream penetration of the ambient environment was because this reduced the shedding of millions of particles from forced air being pushed over the user's head/hair/face, as well as the particles breathed out by a living person, hence changing the micro-environment within the SS that would not be accounted for upstream and therefore would lead to systematic bias that could influence the findings and pull into question the efficiency of the filtration system between the outside environment and inside the SS. The use of a mannequin was considered to be a valid method to assess the modified SS acting as a form of PPE for the user, as this reduced the confounding factor of having a person breathing and shedding particles that would inherently change the micro-environment inside the SS downstream of the HEPA filter that was responsible for protecting the user.
Another possible benefit to the use of these modified SSs in the orthopaedic setting during this pandemic and in the setting of any possible bloodborne viruses is that SSs would provide further reassurance to the operating surgeon who may be cutting bone and creating aerosolized blood and tissue material. Although the possibility of transmission of SARS-CoV-2 is not yet known, coronavirus RNA has been detected in blood donation samples and there is a theoretical risk of transmission [21,22].
A more recent study by Erickson et al. used a three-dimensional printed inlet manifold with HEPA filters, retrofitted to the helmet, to provide HEPA filtered airflow to the user [23]. This study did not provide details on the particulate filtered, but stated that it was independently verified to meet HEPA standards [23]. The system used by Erickson et al. added to the overall volume and weight of the hood, and had two plastic hoses that exited the toga posteriorly and could jeopardize sterility of a surgical field. In contrast, the set-up described for the T5 system in this study did not add any further encumberment to the user, and there was no difference in its outward appearance compared with a non-modified SS.
It appears that both modified Stryker hoods are safe to use with no appreciable interval increase in ETCO2 or FiCO2 with time. ETCO2, an approximation of arterial carbon dioxide concentration, appeared to be slightly higher with use of the modified T5 system; however, it did not continue to increase with time. The increase in FiCO2 may be due to reduced fresh gas flow as a result of the additional HEPA filter. This did not appear to impact respiration over a prolonged period, as there was no significant interval deterioration in gaseous exchange noted over the duration of the study. Similarly, the normal FiO2 level is 21%, and the readings demonstrated that there was a reduction in FiO2 with both the modified and non-modified systems. However, although FiO2 was reduced in both systems, the reductions were steady state with respect to time, suggesting that there was adequate ventilation, sufficient to keep up with the oxygen consumption of the user.
In conclusion, the aim of this study was to evaluate if SSs could be used as a reasonable alternative to face masks as PPE. This study used the well-established SSs used in routine orthopaedic surgery to potentially provide a solution to such a shortage. By fitting a SS with a HEPA filter that can be used for months at a time before needing to be assessed or changed, orthopaedic surgeons would not require face masks and this would reduce the PPE burden.
This study was a proof-of-concept study and was by no means rigorous in terms of testing and validation required for mass roll-out. However, this study has validated and provided evidence that this solution could be used safely as PPE in the setting of a respiratory-droplet-spread viral pandemic. The gown material without a HEPA filter without operation of the fan was found to provide some protection to the user, with c. 10% downstream penetration; however, the concerns of the fan raised in previous studies are valid, whereby the suction effect allows an increase in particulate detected downstream to 25%. The SS must be operated with the fan on, but the addition of a HEPA filter at the fan inlet significantly reduced the particulate count to <5% for the configuration with a HEPA filter housing mounted to the helmet. Downstream penetration was even better (<0.5%) with a HEPA filter cut to the shape of the inlet and the edges sealed to the T5 helmet. The level of particulate penetration was at the level of an FFP3 mask (>99% filtration of 0.3 um particles) or equivalent, and this is of greater filtration efficiency to the recommended N95 respirator. For the purposes of reducing reliance on the supply of face masks that are used in all areas of health care during a pandemic such as COVID-19, modification of SSs may present a viable alternative that would be palatable to orthopaedic surgeons.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.World Health Organization . WHO; Geneva: 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance, 6 April 2020. [Google Scholar]
- 2.British Orthopaedic Association . BOA; London: 2020. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. [Google Scholar]
- 3.Royal College of Surgeons in Ireland . RCSI; Dublin: 2020. Intraoperative recommendations when operating on suspected COVID infected patients. [Google Scholar]
- 4.Thomas J.P., Srinivasan A., Wickramarachchi C.S., Dhesi P.K., Hung Y.M., Kamath A.V. Evaluating the national PPE guidance for NHS healthcare workers during the COVID-19 pandemic. Clin Med. 2020;20:242–247. doi: 10.7861/clinmed.2020-0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health Service Executive . HSE Ireland; Dublin: 2020. Guidance on the use of surgical masks in the healthcare setting in the context of the COVID-19 pandemic. [Google Scholar]
- 6.Public Health England . PHE; London: 2020. When to use a surgical face mask or FFP3 respirator. [Google Scholar]
- 7.Bałazy A., Toivola M., Adhikari A., Sivasubramani S.K., Reponen T., Grinshpun S.A. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control. 2006;34:51–57. doi: 10.1016/j.ajic.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Goldsmith C.S., Tatti K.M., Ksiazek T.G., Rollin P.E., Comer J.A., Lee W.W. Ultrastructural characterization of SARS coronavirus. Emerg Infect Dis. 2004;10:320. doi: 10.3201/eid1002.030913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rengasamy A., Zhuang Z., BerryAnn R. Respiratory protection against bioaerosols: literature review and research needs. Am J Infect Control. 2004;32:345–354. doi: 10.1016/j.ajic.2004.04.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry J.L., Agui J., Vijayakimar R. NASA; Langley, VA: 2016. Submicron and nanoparticulate matter removal by HEPA-rated media filters and packed beds of granular materials. [Google Scholar]
- 11.Éireann Raidió Teilifís. RTE; Dublin: 2020. HSE seeks to accelerate PPE deliveries but warns supply remains challenging 2020.https://www.rte.ie/news/coronavirus/2020/0419/1132459-covid-19-ppe/ Available at: [last accessed November 2020] [Google Scholar]
- 12.Teesing G., van Straten B., de Man P., Horeman-Franse T. Is there an adequate alternative to commercially manufactured face masks? A comparison of various materials and forms. J Hosp Infect. 2020;106:246–253. doi: 10.1016/j.jhin.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Man P., van Straten B., van den Dobbelsteen J., van der Eijk A., Horeman T., Koeleman H. Sterilization of disposable face masks by means of standardized dry and steam sterilization processes; an alternative in the fight against mask shortages due to COVID-19. J Hosp Infect. 2020;105:356–357. doi: 10.1016/j.jhin.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stryker Corp . Kalamazoo, MI: Stryker Corp.; 2020. Flyte personal protection system.https://www.stryker.com/content/dam/stryker/orthopaedic-instruments/resources/Flyte%20Personal%20Protection%20System%20-%20COVID-19.pdf Available at: [last accessed November 2020] [Google Scholar]
- 15.VokesAir. SoniQ II . 2020. Ludwigsburg: Vokes Air.http://www.vokes.co.za/SoniQ%20II.pdf Available at: [last accessed November 2020] [Google Scholar]
- 16.Abraham G., Smith P.M.L.B., McCabe P. HEPA filter replacement experience in a biological laboratory. J Am Biol Saf Assoc. 1998;3:134–142. [Google Scholar]
- 17.Mittal H., Parks S.R., Pottage T., Walker J.T., Bennett A.M. Survival of microorganisms on HEPA filters. Appl Biosaf. 2011;16:163–166. [Google Scholar]
- 18.Derrick J.L., Gomersall C.D. Surgical helmets and SARS infection. Emerg Infect Dis. 2004;10:277. doi: 10.3201/eid1002.030764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hooper G., Rothwell A., Frampton C., Wyatt M. Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement? The ten-year results of the New Zealand Joint Registry. J Bone Joint Surg Br. 2011;93:85–90. doi: 10.1302/0301-620X.93B1.24862. [DOI] [PubMed] [Google Scholar]
- 20.Nakajima D., Tateiwa T., Masaoka T., Takahashi Y., Shishido T., Yamamoto K. Does modern space suit reduce intraoperative contamination in total joint replacement? An experimental study. Eur J Orthopaed Surg Traumatol. 2017;27:1139–1143. doi: 10.1007/s00590-016-1874-8. [DOI] [PubMed] [Google Scholar]
- 21.Chang L., Yan Y., Wang L. Coronavirus disease 2019: coronaviruses and blood safety. Transfus Med Rev. 2020;34:75–80. doi: 10.1016/j.tmrv.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Chang L.Z., Gong H., Wang L., Wang L. Severe acute respiratory syndrome coronavirus 2 RNA detected in blood donations. Emerg Infect Dis. 2020;26:1631. doi: 10.3201/eid2607.200839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erickson M.M., Richardson E.S., Hernandez N.M., Bobbert D.W., II, Gall K., Fearis P. Helmet modification to PPE with 3D printing during the COVID-19 pandemic at Duke University Medical Center: a novel technique. J Arthroplast. 2020;35:S23–S27. doi: 10.1016/j.arth.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]