Case identification, isolation, and contact tracing are fundamental strategies used to control the spread of coronavirus disease 2019 (COVID-19). This has led to widespread testing that interrupted the supply chain for testing materials around the world. A prospective study was conducted to compare inexpensive and easily sourced 3-dimensionally (3D)-printed polylactic acid and polyester nasopharyngeal swabs to commercially manufactured swabs for the detection of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2).
KEYWORDS: COVID-19, nasopharyngeal, swab
ABSTRACT
Case identification, isolation, and contact tracing are fundamental strategies used to control the spread of coronavirus disease 2019 (COVID-19). This has led to widespread testing that interrupted the supply chain for testing materials around the world. A prospective study was conducted to compare inexpensive and easily sourced 3-dimensionally (3D)-printed polylactic acid and polyester nasopharyngeal swabs to commercially manufactured swabs for the detection of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2). During the study period, 287 laboratory-confirmed hospitalized COVID-19 patients, at multiple stages of their illness, were enrolled. The median age for the study population was 47.6 years (interquartile range [IQR], 34.4 to 56.6 years), and two-thirds (67.6%) of the subjects were male. The median duration of hospitalization, at the time of sampling, was 13 days (IQR, 10 to 16 days). Overall concordance between the prototype and control swabs was 80.8% (Cohen’s kappa coefficient, 0.61). Most discrepant results were due to prototype-positive control-negative results. When considering all positive results to be true positives, the prototype swab had a higher sensitivity (90.6% versus 80.8%; 95% confidence interval [CI], 85.7% to 94.0% and 74.7% to 85.7%, respectively; P < 0.015). The cost to produce the prototype swab was estimated to be $0.05 per swab. Polylactic acid 3D-printed polyester-tipped swabs were shown to be effective for nasopharyngeal sample collection. We believe that this design can easily be adopted in countries where commercial swabs are not readily available and can play a vital role in public health efforts for disease control in low-income countries.
INTRODUCTION
Since the severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) was identified as a novel agent causing coronavirus disease 2019 (COVID-19), early patient identification, isolation, and contact tracing strategies have become pivotal for mitigating transmission (https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19) (1). These measures enforced the need for widespread diagnostic testing as a prerequisite for the success of public health interventions to contain the COVID-19 pandemic. The increased demand for testing materials, combined with a shortage in their supply chain, has led to innovations in finding alternative testing methods (2–5). Consequently, additive manufacturing processes, such as 3-dimensional (3D) printing have been widely adopted during the COVID-19 pandemic to produce essential medical devices, including ventilator valves, personal protective equipment, and even nasopharyngeal swabs (6, 7).
The use of stereolithography (SLA) printers for the production of resin nasopharyngeal swabs was previously validated (7). At our center, we experienced difficulties sourcing SLA printers and the necessary surgical grade resin required to manufacture these swabs. As a result, we aimed to develop a 3D-printed swab using the less expensive and more widely available polymer polylactic acid (PLA). Another advantage of PLA is that it is nontoxic and biodegradable, as it is derived from natural sources, such as corn and tapioca. However, the suitability of PLA to viral specimens for PCR-based diagnostics has not been established (8).
The fused deposition modeling (FDM) printers required to manufacture PLA nasopharyngeal swabs are less expensive and easier to procure than the SLA printers. However, they have certain limitations (9). Due to their inherent properties, the lattice design used to create the SLA printer’s high-resolution tip was challenging to replicate. Instead, we sought to develop a method to apply a synthetic absorbent material easily and consistently to the swab’s tip. Polyester was chosen, as it was inexpensive and easy to source. Polyester has also been shown to be nontoxic to viral viability in transport media and is commonly used by several commercial swab manufacturers (10).
The first aim of our study was to develop a 3D-printed swab using PLA and polyester as raw materials. Next, we sought to validate the efficacy and biocompatibility of these swabs for collecting and maintaining the viral genetic material for real-time PCR (RT-PCR) of samples obtained from COVID-19 patients, compared with commercially available swabs.
MATERIALS AND METHODS
Swab design considerations.
To ensure that the nasopharyngeal (NP) swabs were manufactured to clinically acceptable standards, a thorough review of the literature, with the assistance of a medical librarian, was conducted to elucidate the attributes required to design the ideal swab. The following databases were included in the search: PubMed, EMBASE, Cochrane Database of Systematic Reviews, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, and Scopus and Google Patents. To complement the literature search, the opinion of a panel of experts, including a microbiologist from industry, clinical infectious disease and infection control clinicians, and engineers with expertise in 3D printing technologies, was solicited to provide a consensus on the ideal manufacturing properties of the NP swab. Based on the literature review and the opinions from the expert panel, a list of attributes, to be considered when the prototypes for the NP swab were made, was created (Table 1).
TABLE 1.
Prototype desirable properties based on literature review and expert panel consensus
| Property category | Desirable properties |
|---|---|
| Biocompatibility and biosafety | Biosafety and lack of toxic materials |
| Biocompatibility of the materials with regard to viral viability (preferably synthetic materials and fiber) | |
| Dimensions | Ideal length for a swab (14–16 cm, based on the total length of described nasal cavity sampling in the literature) |
| The ideal diameter of the swab (around 1.5–4.0 mm, enough to gain access to the nasopharynx with minimal trauma to surrounding tissues) | |
| Creation of a “breaking point” proximally in the swab’s rods to ensure that it fits into the transportation tube after sampling | |
| Material properties | Ideal rigidity for the swab rod to ensure that enough pressure is exerted to collect a sufficient sample volume |
| Ideal flexibility to ensure that the swab rod can withstand testing pressures and does not break during testing | |
| The ability to safely sterilize the materials used to manufacture the swabs, while maintaining their integrity | |
| The ability of the synthetic materials used in the sampling head of the swab to obtain a clinical sample that is sufficient for accurate testing |
Fused deposition modeling (FDM) 3D printers (Prusa I3 MK2S and Dremel 3D45) were used in the production of the nasopharyngeal swabs. Printing time was approximately 3 hours for each batch of 60 swabs for each printer. To achieve the goal of manufacturing a swab with the desired material properties, the PLA swabs were tested for a balance between flexibility and rigidity by undergoing a 180-degree bend test to ensure that they maintained their tensile strength when they were maneuvered through the nasal cavity.
PLA has a glass transition temperature, at which the material loses its rigidity and softens, of 60°C. For that reason, low-temperature hydrogen peroxide plasma sterilization using evaporated hydrogen peroxide (at 45°C) was utilized to sterilize and package the swabs. Sterilization was performed at the Central Sterilization Service Department (CSSD) of the Ministry of Health.
To ensure that the sterilization procedures used were adequate, 10 randomly selected swabs were directly applied to a blood agar plate (BAP) and a chocolate agar plate, and then the plates incubated at 35°C ± 2°C in oxygen and carbon dioxide environments, respectively. The plates were checked for bacterial growth after 48 h.
The viral transport medium (VTM) was prepared according to the standard operating procedure (SOP) published by the Centers for Disease Control and Prevention (CDC) (11). All VTM production was performed at Jaber Al-Ahmad, Al-Sabah Hospital Laboratory, Kuwait. VTM reagent preparation and mixing were conducted in class II biosafety cabinets, and sterility testing was performed following the SOP. Three tubes were randomly selected from the beginning, middle, and end of each batch to confirm sterility. Using a sterile micropipette, 100 μl of the prepared VTM was inoculated onto BAP and incubated at 35°C ± 2°C for 48 hours.
To test for the possibility of false-positive results, 10 prototype swabs which were void of clinical sample were placed in VTM for at least 1 hour before sending them to the lab as anonymous specimens.
Pilot testing in normal subjects.
Twenty non-COVID-19 volunteers of either gender and above the age of 21 were recruited to participate in the pilot study. After informed consent was obtained, a nasopharyngeal specimen was collected by experienced physicians, using the prototype swab. The user experience and whether any undesirable events, such as significant nasopharyngeal trauma, occurred were noted. Volunteers were asked to rate whether their experience of being swabbed by the prototype on the following scale was not tolerable, uncomfortable but tolerable, or comfortable. Next, the samples were processed according to the protocol outlined in the Clinical and Laboratory Standards Institute (CLSI) standard M40-A2 (12) to verify that the number of respiratory ciliated epithelial cells present in the collected samples was compliant with CLSI recommendations for collection sufficiency.
This study, including the pilot testing, was approved by the Research Ethics Committee of the Ministry of Health of Kuwait (reference no. 2020/1415).
Clinical testing in COVID-19 patients.
We performed a prospective cohort study, with a head-to-head comparison of the prototype swab to the best available commercial swab for nasopharyngeal specimen collection. This study was conducted at a 1,190-bed tertiary center in Jaber Al-Ahmad Hospital, which is the main COVID-19 center in Kuwait. Adult PCR-confirmed COVID-19 patients with various disease severity who were admitted at Jaber Al-Ahmad Hospital between 27 April 2020 and 19 May 2020 were enrolled in the study.
Clinical testing was done to evaluate the performance of the prototype swabs and the locally produced VTM kit compared with the commercially available kits (FLOQSwab sample collection kit [ref: A305CS01] by COPAN Diagnostics Murrieta, USA; CITOSWAB [ref: 2122-009] and viral transport medium (ref: 2118-0019) by Citotest Scientific Jiangsu, People’s Republic of China) (11). After informed consent was obtained, patients who were scheduled for nasopharyngeal swabbing, as determined by the treating team, were tested using the control swab and, shortly after, were swabbed again by the same health care worker in the alternate nostril using the prototype swab and locally produced VTM kit. Swabs were collected by an experienced physician, following standard collection procedures (13). The prototype swab was only rotated clockwise after reaching the pharynx. Patient samples were then immediately transported to the virology laboratory to be processed within 1 h.
Specimens collected by control or prototype swabs were sent to a single virology laboratory and were tested simultaneously in the same extraction and real-time PCR (RT-PCR) run (MagNa Pure and LightCycler 480; Roche, Basel, Switzerland). RT-PCR was performed using the Tib MolBiol LightMix kit (Roche, Basel, Switzerland), detecting both E and RNA-dependent RNA polymerase (RdRP) genes. A result was considered positive if both E and RdRP genes were positive, equivocal if only the E gene was positive, and negative if both were negative. To calculate categorical agreement between the two swabs, equivocal results were considered positive.
Statistical analysis.
Demographic data were analyzed using descriptive statistics. RT-PCR data were reported as either positive or negative. Categorical values were compared using the McNemar test. Result agreement was assessed using Cohen’s kappa coefficient. Linear regression was used to evaluate paired cycle threshold (CT) values from both swabs. Statistical analysis was performed using IBM SPSS version 25 for Windows.
RESULTS
Swab development.
The prototype swabs were 150 mm long and had a tapered breakpoint, 90 mm from the tip of the swab, to facilitate accommodating the swab into the VTM tube after use. At the tip of the shaft, 6 tiny “barbs” were included in order to help the polyester fiber adhere to the swab, without requiring the use of adhesive substrates. The swab was then rotated clockwise until the polyester was fully rolled. In order to ensure uniformity in the diameter (4 mm) of the polyester that is applied to the swab tips, a swab applicator was designed and subsequently 3D printed for use (see Video S1 in the supplemental material). After the first 50 swabs using the FDM printers were made, the dimensions were rechecked to ensure uniformity. All the swab dimensions that were measured remained consistent.
The 10 initial prototypes that were created were all successful in passing the 180-degrees bend test. Also, none of the 10 randomly selected swabs that were selected for sterility testing grew any bacteria after a 48-hour incubation period. There was no difference detected by the high-precision scale, in the weights of the swabs before and after sterilization.
Pilot testing for safety and sample collection sufficiency.
Of 20 patients recruited for pilot testing, 1 volunteer found their experience of being swabbed as being intolerable (5%), the vast majority found it to be uncomfortable but tolerable (16/20, 80%), and 3 out of 20 (15%) found it comfortable. None of the subjects in the pilot study experienced major adverse events, and none of the swabs malfunctioned during testing (e.g., loss of integrity of the swab tips or shafts during sampling). Nineteen out of 20 samples (95%) that were tested for sample collection sufficiency were compliant with CLSI recommendations (12). The same volunteer with the failed swab was tested again using a different prototype kit, which passed the cell count threshold. The reason behind the initial failed test is unclear.
Clinical testing for efficacy.
During the study period, 287 paired prototype and control nasopharyngeal swab samples were collected from admitted adult patients. The median age of the study population was 47.6 years (interquartile range [IQR], 34.4 to 56.6 years), and two-thirds (67.6%) of the subjects were male. The median duration of hospitalization at the time of sampling was 13 days (IQR, 10 to 16 days).
Overall, concordant results were observed in 232 cases (80.8%) (Fig. 1), which resulted in substantial agreement (Cohen’s kappa, 0.61) between the prototype swab and control swabs. Positive agreement was 88.4% and negative agreement was 71.7%. Among discordant results, 60% of samples were positive for a single PCR target (E gene). Interestingly, most discrepant results (67.3%) occurred as prototype-positive/control-negative results. Discordant results had a slightly higher E gene cycle threshold (CT) (median, 34; IQR, 33 to 35) than concordant results (median, 33; IQR, 31 to 34). When considering all positive results to be true positives, the prototype kit had higher sensitivity that the control kit (90.6% versus 80.8%; 95% CI, 85.7% to 94.0% and 74.7% to 85.7%, respectively; P < 0.015).
FIG 1.
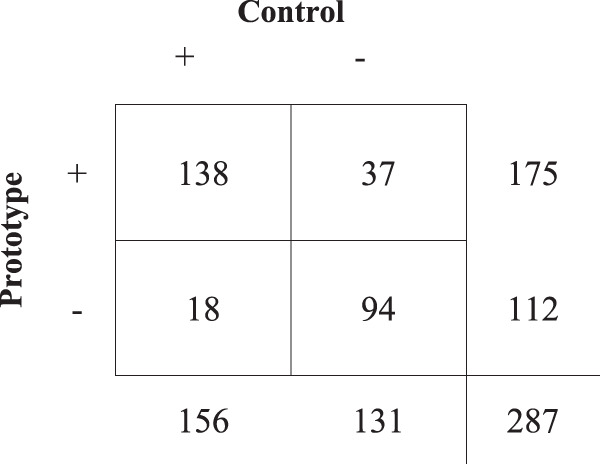
Categorical concordance against control swabs.
In a subset analysis, comparing the prototype swabs to flocked swabs (n = 110), result concordance was slightly lower (79.1%; Cohen’s kappa, 0.58). The prototype swab had a slightly higher sensitivity (86.3% versus 82.2%; 95% CI, 76.6% to 92.4% and 71.9% to 89.3%, respectively; P = 0.167), when all positive results were considered true positives (Fig. 2).
FIG 2.
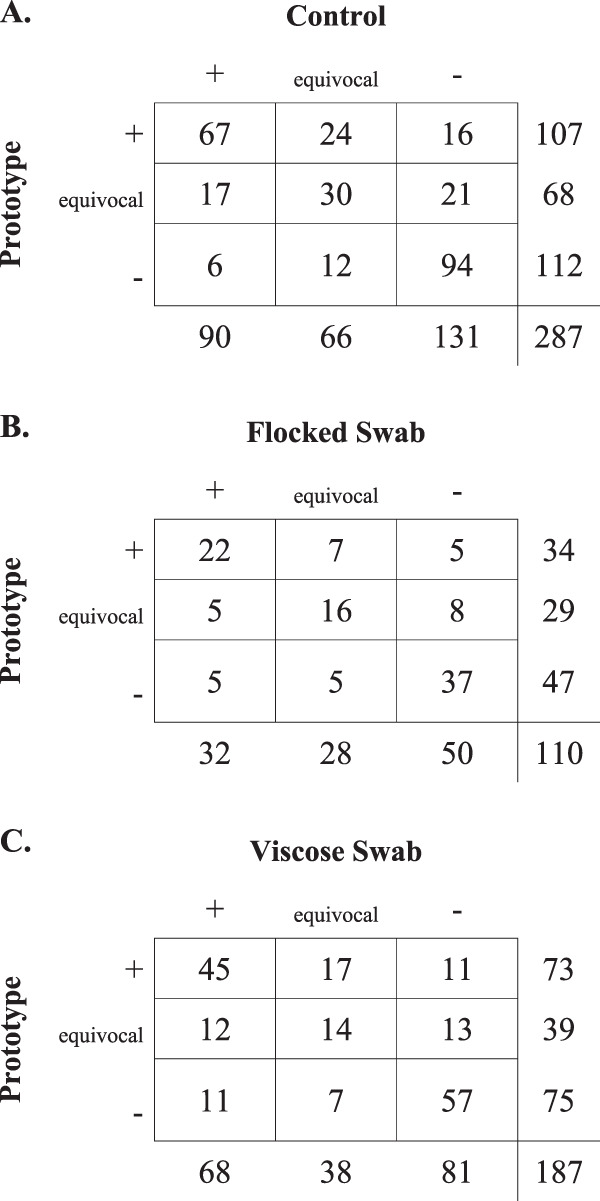
Detailed categorical concordance of prototype swab against control swab (A), flocked swab (B), and viscose swab (C).
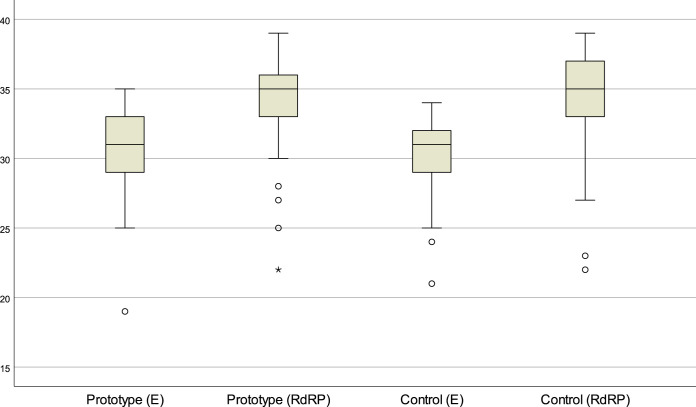
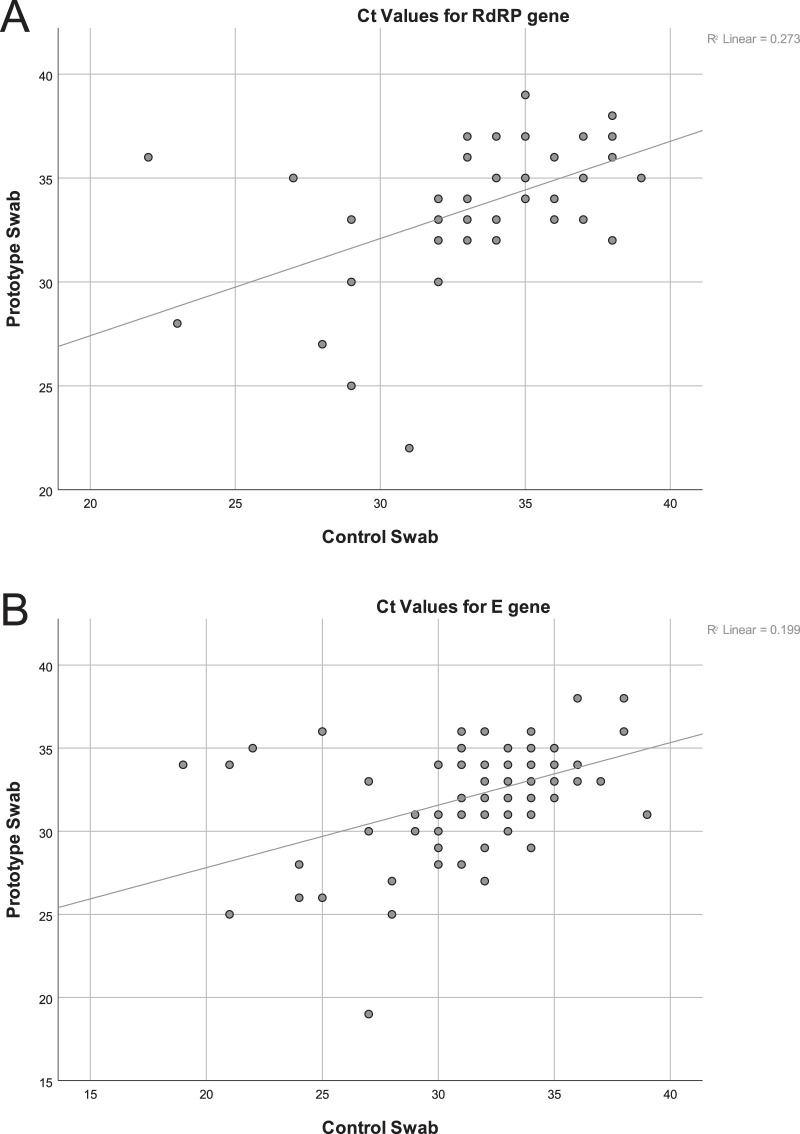
Of 331 individual swabs with positive results, CT values were recorded by the virology laboratory for 272 (82.2%) swabs. Median CT values for the E and RdRP genes were similar. Both prototype and control swabs had a median CT value for the E gene of 33 (IQR, 31 to 34 and 31 to 35, respectively) (Fig. 3). Similarly, the median CT value for the RdRP gene was 35 for both swabs (IQR, 33 to 37 and 33 to 38 for the prototype and control swabs, respectively). Figure 4 shows CT values of specimens collected using the prototype swab relative to those collected by the control swab, with a linear regression fit superimposed on the scatterplot.
FIG 3.
Distribution of cycle threshold (CT) values of specimens collected using the prototype and control swab.
FIG 4.
Cycle threshold (CT) values from nasopharyngeal samples collected using the prototype swab relative to those collected using the control swab. (A) Using values related to the RNA-dependent RNA polymerase (RdRP) gene (n = 36). (B) Using values related to the E gene (n = 57). Please note that threshold values for negative results were not included in the scatterplot. Only CT values that were available from the lab and concordant are represented in the figures.
During the study period, no patient-related adverse events concerning the use of the prototype kit was reported. None of the 10 swabs that were void of clinical samples and were sent as anonymous specimens tested positive for the E or the RdRP genes.
DISCUSSION
Over the last few months, expanding access for SARS-CoV-2 testing coupled with limited production capacity, along with an interrupted supply chain, led to a shortage in basic diagnostic tools around the world. Over the course of the pandemic, securing a constant supply of flocked nasopharyngeal swabs was difficult at our center, as well as in other centers in our country. Here, we present a simple, inexpensive, and easy-to-produce swab that can be used to obtain nasopharyngeal specimens for diagnosing COVID-19. In our sample, we found that, when considering any positive result as a true positive, the prototype swab was superior in viral detection sensitivity compared with the best available control swabs.
Due to the expected shortages in swabs and viral transport media, we explored immediately available resources to produce reliable nasopharyngeal collection kits. The swab shafts were made of PLA, a safe, readily available, and durable material. The physical and chemical properties of PLA, as well as its biocompatibility, have been well described (14, 15). These features, along with the ease of adoption of 3D printings methods, makes PLA a good option for manufacturing a readily available swab shaft. However, the effect of PLA on viral recovery and PCR was never evaluated previously. On the other hand, polyester-tipped swabs are commonly used in standard virologic sample collecting systems (16). Currently, flocked swabs are the gold standard for collecting nasopharyngeal samples, due to their design, which has maximized the surface area and release properties of the swab tips. Although flocked nylon swabs been extensively evaluated against rayon swabs, the evidence for their performance compared with polyester swabs in a clinical setting is lacking (17, 18).
Several other studies have evaluated different materials and 3D printing methods to resolve shortages in the supply of swab. Callahan et al. developed four 3D-printed swabs using four different materials and designs, which were all comparable to the flocked swabs, with high agreement (7). However, some of the materials used in the study are proprietary and require relatively expensive 3D printers. On the other hand, fused deposition modeling (FDM) printers are less expensive, can be open-sourced, and use less expensive raw materials (PLA) (15). In our study, the sensitivities of the prototype and the flocked swabs were comparable (86.3% versus 82.2%, P = 0.167). However, the prototype detected more positive specimens (13 versus 10) when considering an equivocal result to be positive (Fig. 2). Access to alternate molecular testing methods to confirm the positivity of discrepant result was not available to us when this study was performed. However, none of the 10 randomly selected prototype swabs that were void of clinical specimens tested positive.
Freire-Paspuel et al. evaluated the used of cotton-tipped swabs that were immediately available for use in the clinical setting. They found that cotton-tipped swabs were comparable to rayon-tipped swabs for obtaining the nasopharyngeal specimens needed to detect SARS-CoV-2 in 44 adults (19). However, polyester swabs were shown to have a larger absorption capacity and extraction efficiency than cotton or rayon for recovering human DNA from salivary samples (10).
The production of the prototype swabs was extremely inexpensive compared with all commercially available kits. The price to acquire one of the printers used in our study was around $750, and the cost of PLA was between $20 and $25 per kg. Each swab weighed on average 0.63 g, which was equal to $0.01 of PLA per swab. Polyester was acquired from a local vendor at a price of $4 per kg. Each swab is tipped with around 0.01 g of polyester. This results in a material price per swab to be less than $0.05. FDM printers can print up to 60 swab shafts every 3 hours. The process of applying polyester to the prototype swabs, via the 3D-printed applicator, was performed at a rate of approximately 100 swabs per hour.
This study is limited by the use of two different control swabs, due to the shortages of flocked swabs that we experienced at our center. However, paired samples in which flocked swabs were used as controls were recorded, allowing us to perform a subgroup analysis. Also, study subjects were all previously confirmed COVID-19 cases with a relatively long median duration of 13 days of hospitalization prior to evaluation. Consequently, the patient specimens had high CT values on average, as well as a higher than expected number of equivocal results. This is in keeping with observations by Sutjipto et al. that nasopharyngeal swab clinical sensitivity decreased from 95.3% (95% CI, 83% to 99.1%) to 70% (95% CI, 50.4% to 84.6%) after day 7 of illness (20). The findings of the current study may therefore be less broadly applicable to patients earlier in disease presentation and with higher viral loads. In addition, due to the time constrains and the increased workload in the clinical virology laboratory at our center, some CT values were missing and further testing to resolve discrepant results was not possible. Finally, most subjects in the pilot evaluation reported that the protype swab was uncomfortable or intolerable. However, comfort was not formally assessed or compared in patients enrolled in the study.
To our knowledge, this is the second manuscript that has evaluated a 3D-printed nasopharyngeal swab. However, it is the first to provide a swab design that could be produced using relatively inexpensive printers and raw materials. We believe that this design can easily be adopted by countries where commercial swabs are not readily available and can play a vital role in addressing diagnostic test shortages in countries with fewer resources. Currently, mass production of the prototype swab is being considered at a national level in our country until commercial flocked swabs are available again, as a consequence of this study’s findings. The swab design blueprint and production standard operating procedures (SOPs) are available online (https://projectjaber.com/).
Supplementary Material
ACKNOWLEDGMENTS
We thank the following volunteers who contributed their time and effort into 3D printing the NP swabs, prepared the viral transport media, and helped during the clinical testing: Nada Al-Youha, Suzane Al Bustan, Farah Al-Mutairi, Yousif Alqabandi, Yousef Alkandry, Ahmad Alsharhan, Ali Al-Shatti, Ameerah Alazemi, Abdullah Alawwam, Hala Hamdan, Rehab Alajmi, Fatima Alsulaili, Shahad Al-Roumi, Noor Alquraini, Fatma Hijazi, Nada Elsaid, Kawthar Murad, Mohamed Fadel, Thunian AlFaresi, and Zaid AlFarhan. The FDM printers and PLA were provided by two of the coauthors (S. Alzabin and Y.A.-M.).
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
J.P. has received consulting/honoraria fees from AbbVie, Cepheid, and Seegene; and research grant funding outside the current work from AbbVie, BD Diagnostics, Sanofi Pasteur, and MedImmune.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Heymann DL, Shindo N, WHO Scientific and Technical Advisory Group for Infectious Hazards. 2020. COVID-19: what is next for public health? Lancet 395:542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hogan CA, Sahoo MK, Pinsky BA. 2020. Sample pooling as a strategy to detect community transmission of SARS-CoV-2. JAMA 323:1967. doi: 10.1001/jama.2020.5445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lohse S, Pfuhl T, Berkó-Göttel B, Rissland J, Geißler T, Gärtner B, Becker SL, Schneitler S, Smola S. 2020. Pooling of samples for testing for SARS-CoV-2 in asymptomatic people. Lancet Infectious Diseases doi: 10.1016/S1473-3099(20)30362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azzi L, Carcano G, Gianfagna F, Grossi P, Gasperina DD, Genoni A, Fasano M, Sessa F, Tettamanti L, Carinci F, Maurino V, Rossi A, Tagliabue A, Baj A. 2020. Saliva is a reliable tool to detect SARS-CoV-2. J Infect 81:e45–e50. doi: 10.1016/j.jinf.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng MP, Papenburg J, Desjardins M, Kanjilal S, Quach C, Libman M, Dittrich S, Yansouni CP. 2020. Diagnostic testing for severe acute respiratory syndrome-related coronavirus 2: a narrative review. Ann Intern Med 172:726–734. doi: 10.7326/M20-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ishack S, Lipner SR. 2020. Applications of 3D printing technology to address COVID-19-related supply shortages. Am J Med 133:771–773. doi: 10.1016/j.amjmed.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Callahan CJ, Lee R, Zulauf KE, Tamburello L, Smith KP, Previtera J, Cheng A, Green A, Azim AA, Yano A, Doraiswami N, Kirby JE, Arnaout RA. 2020. Open development and clinical validation of multiple 3D-printed nasopharyngeal collection swabs: rapid resolution of a critical COVID-19 testing bottleneck. J Clin Microbiol 58:e00876-20. doi: 10.1128/JCM.00876-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zuniga JM, Cortes A. 2020. The role of additive manufacturing and antimicrobial polymers in the COVID-19 pandemic. Expert Rev Med Devices 17:477–481. doi: 10.1080/17434440.2020.1756771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chia HN, Wu BM. 2015. Recent advances in 3D printing of biomaterials. J Biol Eng 9:4. doi: 10.1186/s13036-015-0001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruijns BB, Tiggelaar RM, Gardeniers H. 2018. The extraction and recovery efficiency of pure DNA for different types of swabs. J Forensic Sci 63:1492–1499. doi: 10.1111/1556-4029.13837. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. 2020. Preparation of viral transport medium (SOP#: DSR-052–03). Centers for Disease Control and Prevention, Atlanta, GA: https://www.cdc.gov/coronavirus/2019-ncov/downloads/Viral-Transport-Medium.pdf. [Google Scholar]
- 12.Clinical and Laboratory Standards Institute. 2014. Quality control of microbiological transport systems; approved standard. CLSI document M40-A2. Second edition ed, vol 34 Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 13.Marty FM, Chen K, Verrill KA. 2020. How to obtain a nasopharyngeal swab specimen. N Engl J Med 382:e76. doi: 10.1056/NEJMvcm2010260. [DOI] [PubMed] [Google Scholar]
- 14.Gupta B, Revagade N, Hilborn J. 2007. Poly(lactic acid) fiber: an overview. Prog Polym Sci 32:455–482. doi: 10.1016/j.progpolymsci.2007.01.005. [DOI] [Google Scholar]
- 15.Singhvi MS, Zinjarde SS, Gokhale DV. 2019. Polylactic acid: synthesis and biomedical applications. J Appl Microbiol 127:1612–1626. doi: 10.1111/jam.14290. [DOI] [PubMed] [Google Scholar]
- 16.Khare R, Grys TE. 2016. Specimen requirements selection, collection, transport, and processing, clinical virology manual, fifth edition American Society of Microbiology, Washington, DC. [Google Scholar]
- 17.Hernes SS, Quarsten H, Hagen E, Lyngroth AL, Pripp AH, Bjorvatn B, Bakke PS. 2011. Swabbing for respiratory viral infections in older patients: a comparison of rayon and nylon flocked swabs. Eur J Clin Microbiol Infect Dis 30:159–165. doi: 10.1007/s10096-010-1064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daley P, Castriciano S, Chernesky M, Smieja M. 2006. Comparison of flocked and rayon swabs for collection of respiratory epithelial cells from uninfected volunteers and symptomatic patients. J Clin Microbiol 44:2265–2267. doi: 10.1128/JCM.02055-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freire-Paspuel B, Vega P, Velez A, Castillo P, Gomez-Santos I, Cruz M, Garcia-Bereguiain MA. 2020. Cotton tipped plastic swabs for SARS-CoV-2 RT-qPCR diagnosis to prevent supplies shortage. medRxiv 10.1101/2020.04.28.20079947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutjipto S, Lee PH, Tay JY, Mendis SM, Abdad MY, Marimuthu K, Ng OT, Lin C, Chan M, Soon M, Lin RTP, Leo Y-s, De PP, Barkham T, Vasoo S, National Centre for Infectious Diseases COVID-19 Outbreak Research Team. 2020. The effect of sample site, illness duration and the presence of pneumonia on the detection of SARS-CoV-2 by real-time reverse-transcription PCR. Open Forum Infect Dis doi: 10.1093/ofid/ofaa335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.