Abstract
Long-term care (LTC) residents, isolated because of the COVID-19 pandemic, are at increased risk for negative mental health outcomes. The purpose of our article is to demonstrate how the interRAI LTC facility (LTCF) assessment can inform clinical care and evaluate the effect of strategies to mitigate worsening mental health outcomes during the COVID-19 pandemic. We present a supporting analysis of the effects of lockdown in homes without COVID-19 outbreaks on depression, delirium, and behavior problems in a network of 7 LTC homes in New Brunswick, Canada, where mitigative strategies were deployed to minimize poor mental health outcomes (eg, virtual visits and increased student volunteers). This network meets regularly to review performance on risk-adjusted quality of care indicators from the interRAI LTCF and share learning through a community of practice model. We included 4209 assessments from 765 LTC residents between January 2017 to June 2020 and modeled the change within and between residents for depression, delirium, and behavioral problems over time with longitudinal generalized estimating equations. Though the number of residents who had in-person visits with family decreased from 73.2% before to 17.9% during lockdown (chi square, P < .001), the number of residents experiencing delirium (4.5%-3.5%, P = .51) and behavioral problems (35.5%-30.2%, P = .19) did not change. The proportion of residents with indications of depression decreased from 19.9% before to 11.5% during lockdown (P < .002). The final multivariate models indicate that the effect of lockdown was not statistically significant on depression, delirium, or behavioral problems. Our analyses demonstrate that poor mental health outcomes associated with lockdown can be mitigated with thoughtful intervention and ongoing evaluation with clinical information systems. Policy makers can use outputs to guide resource deployment, and researchers can examine the data to identify better management strategies for when pandemic strikes again.
Keywords: Long-term care, COVID-19, interRAI, delirium, depression, behaviors
On March 11, 2020, the World Health Organization declared the outbreak of COVID-19 to be a pandemic. As we put pen to paper, the World Health Organization is reporting more than 30 million cases and more than 1,000,000 deaths in 216 countries (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). Older adults in long-term care (LTC) homes are especially vulnerable to the negative sequelae of the COVID-19 pandemic.1 In many international settings, LTC homes have been closed or “locked down” to all visitors including family and friends to maintain physical distancing measures and decrease viral transmission.2 , 3 Even in the absence of a COVID-19 outbreak within the home, LTC residents face potential negative mental health consequences of lockdown.4
LTC residents have a high prevalence and increased baseline risk of developing mental health conditions including depression, delirium, and behavioral problems. Depression is one of the most common psychiatric condition in LTC,5 with rates ranging from 11%6 to 16.9%.7 Delirium, an acute change in attention and cognition that develops rapidly over several hours or days,8 has been estimated to affect 14% of LTC residents.9 Across Canada, an estimated 26% to 66% of LTC residents exhibit behavioral problems,10 which can be disruptive, distressing, or challenging to persons in the LTC environment including other residents, staff, and family.11
Reduced social interaction associated with lockdown during the COVID-19 pandemic could further increase the risk for worsening mental health outcomes. Stress among LTC staff could lead to stress among residents, increasing the risk for delirium and behavioral problems. Isolation, lack of family contact, and lack of stimulation from social activities within the home could lead to boredom, loneliness, and depression. Indeed, in the general population, quarantine measures during COVID-19 have consistently been associated with negative psychological outcomes.12 Reports from LTC homes in Italy suggest that as many as 50% of LTC residents experienced hypokinetic delirium superimposed on dementia (eg, residents refused food and had difficulty getting out of bed).13 Calls have arisen to overcome limited physical interaction and improve social interaction via virtual strategies (eg, FaceTime, Zoom) and through creative outlets to overcome workload barriers (eg, student visitors).14 However, the implementation of such programs may be limited by access to resources (eg, tablets or smartphones), and their effect on mental health outcomes is unclear.
Robust and evidence-based clinical information systems are essential to support surveillance of mental health outcomes and evaluation of strategies to improve socialization during a public health emergency such as the COVID-19 pandemic.15 Many jurisdictions around the world have access to clinical information systems, which include the Minimum Data Set 3.0 in US LTC homes, and the interRAI long-term care facilities (LTCF) in LTC homes in more than 30 countries around the world.16 The interRAI LTCF is a standardized vehicle to record clinical observations from a structured clinical interview, observations, and document review. Assessments include domains critical to the care of frail older persons, including health instability, function, falls, dementia, delirium, depression, pain, social engagement, quality of life, communication, and caregiver stress.17 The clinical observations are then integrated by business intelligence software to produce several outputs at the point-of-care including outcome scales and clinical assessment protocols. For example, the Depression Rating Scale (DRS) can identify residents who require further evaluation for depression or regular monitoring of early symptoms.18 The data can provide essential information to frontline staff to guide daily care and human resource planning. Further, the data can describe the effect of strategies to prevent worsening conditions, such as mental health outcomes during lockdown.
The purpose of our article is to demonstrate how thoughtful use of mitigating strategies (eg, window visits and use of technology) and clinical information systems like the interRAI LTCF can inform clinical care and prevent worsening mental health outcomes (eg, depression, delirium, and behavioral problems) during the COVID-19 pandemic. Our discussion will focus on internationally adopted interRAI instruments (ie, interRAI LTCF).
Methods
Setting
Data were obtained from a network of 7 private francophone LTC homes in New Brunswick, Canada. This community of practice uses routinely collected interRAI LTCF assessment data to measure facility-level performance on a series of risk-adjusted measures of quality of care and resident-reported quality of life indicators.19 The homes in this network review reports of their performance compared with other homes in the network, and a large comparator of more than 1000 Canadian homes. The community of practice offers opportunities for interRAI data comparison and knowledge exchange (eg, strategies to overcome management, clinical, and social challenges; webinars about fostering clinical utilization of interRAI data, data quality collection, and continuing improvement). Implementation of the LTCF in New Brunswick has emphasis on the clinical (eg, scales and outcomes) and quality applications (eg, quality indicators) of the instrument. The homes in the network range in size from 30 to 85 beds, with a mean of 59.6 (standard deviation, 20.9). Data from all quarterly interRAI LTCF assessments were included from January 2017 to June 2020.
The homes included in our analyses began restricting visitors between March 12 and March 16, 2020. All group activities within the LTC homes were also halted in March 2020. Once lockdown began, recreation staff were redeployed to focus on keeping family connected with LTC residents.20 Strategies included window visits and video chats. To support these initiatives, the government of New Brunswick supplied LTC homes with 1 iPad per every 10 residents to connect with family members via video chat in April 2020.21 One of the homes also hired students to facilitate virtual calls and engage in one-on-one visits with residents. Between May 20 and June 15, 2020, the homes began in-person outdoor visits with family. Provincially, there were no COVID-19 cases in New Brunswick LTC homes between March and September 2020. Therefore, these homes provide evidence about the net impact of lockdowns where COVID-19 is not present in homes or in the surrounding communities.
Data Collection
The interRAI LTCF is a standardized assessment tool that is administered by trained registered nurses within New Brunswick LTC homes. Information to complete the assessment is collected through interaction with residents, their families, and the clinicians who work with them, and chart review if required. In New Brunswick, the interRAI LTCF is administered within 11 days of admission, and on a quarterly basis thereafter, or if there is a significant change in status. Importantly, all New Brunswick LTC homes continued to complete scheduled and change-of-status LTCF assessments throughout the lockdown period.
Table 1 provides a summary of the outcomes and covariates examined. We described social engagement with family through 2 items in the LTCF, one capturing in-person visits and the other capturing other interaction (eg, telephone or e-mail) in the last 3 days, and using the Revised Index of Social Engagement scale (Table 1).
Table 1.
Outcomes and Covariates
| Construct | Scale or Item | Description | Classification for Model |
|---|---|---|---|
| Outcomes | |||
| Depression | Depression Rating Scale (DRS)18 | Summary scale of assessor-rated depressive symptoms using 7 mood items. Scored 0 (no symptoms) to 14 (high symptom burden), where 3 represents need for follow-up for depression | Binary: Score of ≥3 or <3 |
| Delirium | Delirium Clinical AssessmentProtocol (CAP)22 | Any resident who exhibits one of the following:
|
Binary: CAP triggered yes/no |
| Behavioral problems | Aggressive Behavior Scale (ABS)23 | Severity of expressions and behaviors. Scored 0 (no behaviors) to 12 (most severe). | Binary: Score of ≥1 or 0 |
| Covariates | |||
| Age | Age | Continuous | |
| Sex | Sex | Female or male | Binary: male or female |
| Lockdown | Lockdown period | Lockdown date was specific to when each home closed | Binary: yes or no |
| Length of stay | Admission and assessment date | Number of days since admission to the home | Continuous |
| Facility X | Reference facility | Facility X was used as the reference facility because it demonstrated differences in univariate analyses | Binary: yes or no |
| Major physical disorder | Heart failure | Diagnosis of heart failure | Binary: yes/no |
| Major cognitive disorder | Alzheimer’s disease or other dementias | Diagnosis of Alzheimer’s disease or other dementias | Binary: yes/no |
| Healthy instability | Changes in Health, End-Stage disease and Symptoms (CHESS)24 | Health instability. Scored 0 (most stable) to 5 (most unstable). | Continuous |
| Functional mobility | Activities of Daily Living Hierarchy (ADL Hierarchy)25 | Hierarchical measure of functional status related to activities of daily living based on 4 key activities (personal hygiene, locomotion, toilet use, and eating) that represent early, mid, and late loss activites of daily living. Scored 0 (independent) to 6 (dependent). | Continuous |
| Cognition | Cognitive Performance Scale (CPS)26 | Global measure of cognitive status based on functional parameters rated by severity. Scored 0 (intact) to 6 (very severe impairment). | Continuous |
| Social engagement | Revised Index of Social Engagement27 | Measures positive features of LTC residents' social behavior using 6 items. 0 (no engagement) to 6 (high engagement) | Continuous |
Data Analysis
Characteristics of LTC residents at their initial interRAI assessment between January 2017 and June 2020 are presented as frequencies for categorical variables and mean and standard deviation for continuous variables. The raw, unadjusted rates of in-person visits with family members, other interaction with family members (eg, telephone,e-mail), social engagement, and mental health issues are presented before and after March 2020. Statistical significance was tested via chi-square tests, using an alpha of 0.05.
Longitudinal generalized estimating equation (GEE) were modeled for each outcome of interest, estimating changes within and between individuals from January 2017 to June 2020. Both autoregressive and exchange correlation matrices were explored. However, the autoregressive correlation matrix was deemed to be more suitable for these data because the correlation between responses is expected to decrease over time. Age, sex, and lockdown were included in all models regardless of significance. We modeled the LTC home’s effect by comparing to a reference home, called “Facility X,” which demonstrated differences in univariate analyses. Interactions that were hypothesized a priori to influence the outcomes were entered into the multivariate models, and quadratic terms were used to test for curvilinearity of the continuous covariates. The final multivariate models were constructed by adding all variables to the model and retaining those significant at P <.05.
Results
We included 4209 assessments from 765 LTC residents. On average, residents had 4.7 (standard deviation, 3.3) assessments between January 2017 and June 2020. Table 2 presents the characteristics of the included residents at their first assessment. The average age was 81.4 years (11.5), and most were female (59.5%). More than half of residents had a diagnosis of Alzheimer’s disease or another dementia (55.6%), and much fewer had a diagnosis of heart failure (6.8%).
Table 2.
Characteristics of Included Residents
| Characteristic | Mean (SD) or n (%) |
|---|---|
| Age, mean (SD) | 81.4 (11.5) |
| Female | 455 (59.5) |
| Diagnosis of Alzheimer’s disease and related dementias | 425 (55.6) |
| Diagnosis of heart failure | 52 (6.8) |
| Depression (score ≥3) | 121 (15.9) |
| Delirium (CAP triggered) | 228 (29.9) |
| Behavioral problems (ABS score ≥1) | 31 (4.1) |
ABS, Aggressive Behavior Scale; CAP, Clinical Assessment Protocol; SD, standard deviation.
Before March 2020, 73.2% of residents had in-person visits with family in the last 3 days compared with 17.9% during the lockdown period (P < .001). Although we would expect these numbers to reflect zero contact with family during the lockdown period, the homes described 3 scenarios where this item was coded as occurring: (1) compassionate visits—resident was imminently dying or palliative; (2) family member was also staff at the home; or (3) window visits were miscoded as in-person visits. The difference in the proportion of residents who had other family contact (eg, e-mail, letters) (before: 35.2%, after: 35.5%; P = .71) and whose Revised Index of Social Engagement score demonstrated high social engagement within the home (before: 56.3%, after: 53.1%; P = .67) was not different before or during lockdown. The proportion of residents with indications of depression decreased from 19.9% before lockdown to 11.5% after lockdown (P < .002). Prior to and during lockdown, the proportion of residents demonstrating any behaviors (before: 35.5%, after: 30.2%; P = .19) and with delirium (before: 4.5%, after: 3.5%; P = .51) was not different.
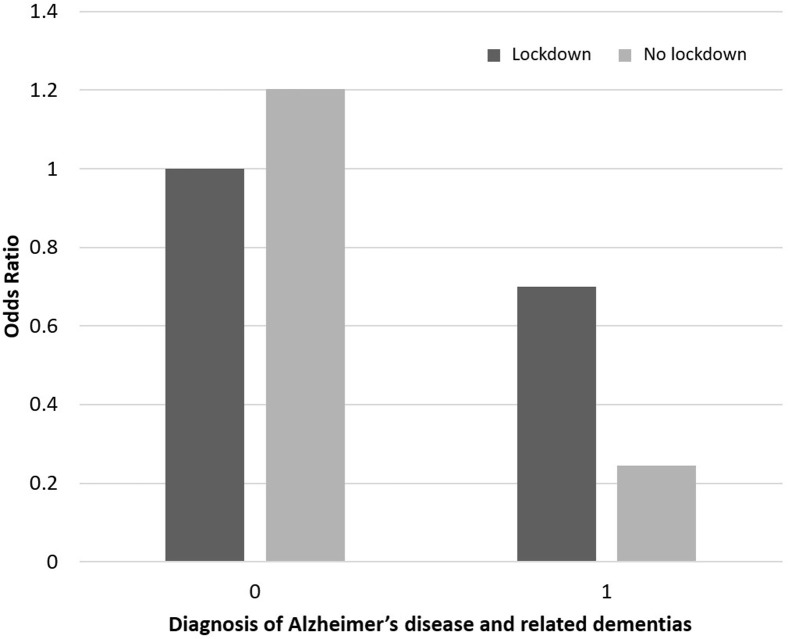
The final multivariate models (Table 3 ) indicate that lockdown did not have a statistically significant effect on rates of depression, delirium, or behavioral problems. However, there was an interaction between lockdown and dementia where residents with dementia were less likely to experience delirium during lockdown (Figure 1 ). The significance of the interaction term depended on the specified approach to correlation of error terms. This interaction was not statistically significant in the GEE with an autoregressive correlation matrix. However, it was highly significant in the model with an exchange matrix. In the final adjusted model, residents were more likely to experience depressive symptoms if they were female, had worse functional mobility, health instability, and cognitive impairment (the relationship was curvilinear), and experienced behavioral problems and less likely if they lived in Facility X, and had a diagnosis of Alzheimer’s disease or other dementias. Residents' odds of experiencing delirium were higher if they had worse cognitive impairment and lived in Facility X, and lower if they had higher levels of social engagement. Finally, residents with a diagnosis of Alzheimer’s disease or other dementias and those with cognitive impairment (the relationship was curvilinear) were more likely to have behavioral problems, whereas females, residents with high levels of social engagement, and those living in Facility X were less likely.
Table 3.
Results of Final Longitudinal Multivariate Models
| Parameter | Outcome |
||
|---|---|---|---|
| Depression, OR (95% CI) | Delirium, OR (95% CI) | Behavioral Problems, OR (95% CI) | |
| Age | 1.00 (0.98-1.01) | 1.01 (0.99-1.02) | 0.99 (0.98-1.00) |
| Sex (female) | 2.11 (1.47-3.04) | 1.35 (0.88-2.08) | 0.70 (0.52-0.92) |
| Lockdown | 0.86 (0.66-1.11) | 1.21 (0.57-2.57) | 0.88 (0.72-1.06) |
| Facility X | 0.45 (0.27-0.74) | 1.85 (1.22-2.81) | 0.58 (0.41-0.83) |
| Alzheimer’s and other dementias | 0.69 (0.48-0.99) | 0.70 (0.43-1.14) | 1.55 (1.13-2.13) |
| RISE | — | 0.74 (0.67-0.82) | 0.93 (0.89-0.98) |
| CPS | 1.55 (1.18-2.04) | 1.28 (1.13-1.45) | 2.27 (1.70-3.03) |
| CPS2 | 0.92 (0.88-0.96) | — | 0.93 (0.89-0.97) |
| CHESS | 1.17 (1.07-1.29) | — | — |
| ABS | 1.28 (1.22-1.34) | — | — |
| ADL Hierarchy | 1.11 (1.00-1.24) | — | — |
| Alzheimer’s and other dementias × lockdown∗ | — | 0.29 (0.07-1.16) | — |
ADL, activities of daily living; CHESS, Changes in End-Stage Disease, Signs and Symptoms; CI, confidence interval; CPS, Cognitive Performance Scale; OR, odds ratio; RISE, Revised Index of Social Engagement.
Dashes indicate values not included in the final model.
Interaction term.
Fig. 1.
The odds of experiencing delirium for residents with and without Alzheimer's Disease and related dementias during lockdown.
Discussion
We document an example of how clinical information systems like the interRAI LTCF can be used in a community of practice to examine changes in resident outcomes over time and evaluate strategies put in place to mitigate negative outcomes. In particular, the network of 7 private, not-for-profit LTC homes in our study who did not experience COVID-19 outbreaks but were locked down for 3 months were able to mitigate the negative effects of social isolation on depression, delirium, and behavioral problems. Using depression, delirium, and an aggressive behavior outcome embedded within the interRAI LTCF quantifies changes over time, including effects of COVID-19 policies such as lockdown, without requiring additional documentation or data collection. In addition, homes can use these routinely collected data to monitor residents’ mood over time and evaluate the effect of home-level strategies (eg, redeploying activity staff). Likewise, policy makers can use these data at a jurisdiction level to evaluate the effect of strategies (eg, providing iPads) and plan for additional resources as needed.
Our data suggest that thoughtful deployment of strategies to improve LTC residents’ social engagement may mitigate the negative consequences of lockdown, including mental health outcomes such as depression, delirium, and behavioral problems. These results contrast other emerging reports where increased depression and behavior problems have arisen throughout the pandemic,28 though these settings may have also experienced outbreaks of COVID-19 within their LTC homes, which could shift priorities of care toward infection prevention and control. Our study is unique because it allows for disaggregation of the impact of a lockdown from COVID-19 outbreaks. The observed interaction in our results where lockdown resulted in a lower risk of delirium for residents with dementia could be a result of a calmer environment with fewer people coming and going throughout the home. Given that a greater number of precipitating factors (eg, busy environment, infection, medication) increases the risk for delirium, the calmer environment induced by lockdown could result in a lower risk.29 On the other hand, the increased risk of delirium for those without dementia might indicate that stress and isolation associated with lockdowns might affect a cognitively intact population differently. The other factors (ie, sex, functional mobility, health instability, cognitive impairment, social engagement) we observed to be associated with depression, delirium, and behavioral problems are in accordance with previous literature.29, 30, 31
Implications for Practice, Policy, and Research
Widely adopted assessment systems, such as the interRAI LTCF, should be leveraged by clinicians and policy and decision makers to monitor implementation of system-level interventions and outcomes. We have demonstrated that these strategies can be used during public health crises such as the COVID-19 pandemic.
Data derived from standardized assessments can guide clinicians by tracking residents over time, targeting interventions to those who need them most, and identifying residents at high risk for negative outcomes. For example, clinicians can track changes in the Depression Rating Scale score over quarterly assessments to determine if a resident is demonstrating more depressive symptoms and target strategies to that resident (eg, increase social contact with family or friends).
Policy makers can use data arising from clinical information systems in several ways. First, scales embedded within interRAI assessments can be used to guide resource deployment during and after the pandemic. As the pandemic resolves, embedded scales will continue to identify vulnerable populations requiring ongoing support. For example, using the Depression Rating Scale, policy makers can determine areas where mental health supports may be required, and resources allocated to reflect the need. Additionally, the collected data can help policy makers to make data-informed decisions about how the sequelae of COVID-19 affect the health care system and how to reorganize or redeploy resources accordingly throughout the various phases of the pandemic. Monitoring the individuals’ needs and the staffing available will be a marathon of post-outbreak follow-up, as the crisis profoundly affects both.
However, obtaining data and using it to guide decisions requires ongoing assessments. In our example of the 7 homes in New Brunswick, assessments continued to be completed throughout lockdown, so it could be used to guide practice and evaluate changes over time. Granted, there were no COVID-19 outbreaks in the 7 homes, but home-level stress and virus-related vigilance remained high. To ensure ongoing assessment and use of routine clinical data, adequate personnel is required to complete and interpret the assessments, particularly in the LTC sector where staffing rates are often a concern.32
Standardization of clinical information systems like the interRAI LTCF and their global reach makes them eminently useful for large-scale epidemiologic research and the sharing of new information arising during this epidemic, and beyond. The interRAI LTCF is currently used in more than 30 countries. Data collected from international interRAI assessments completed before, during, and after the pandemic can be used to evaluate its effect locally, nationally, and internationally. By understanding characteristics of international populations and being able to compare to other jurisdictions, we will have information to adjust policies, respond to needs, and learn from other areas who may be having better outcomes. For example, the 7 homes included here demonstrated success in preventing increased depression, delirium, and behavioral problems in response to lockdown. Similar analyses can be conducted in other provinces and countries that use the interRAI LTCF to compare their strategies to mitigate lockdown-associated outcomes, and adjustments to practice can be made where necessary. Physical, cognitive, and psychosocial characteristics of LTC populations can be examined longitudinally to determine the effect of and local response to the pandemic. Compared internationally, these analyses will identify evidence-based strategies for minimizing the negative effects of future pandemics.
Limitations
In this study, we were most interested in the temporal effects of lockdown on mental health outcomes; we did not examine fully explanatory models for our outcomes. We were able to determine changes in our study group but did not have contemporaneous controls to ensure the effects were real. In addition, outcomes other than mental health concerns were not fully examined. Use of the interRAI LTCF has limitations as well. Poor implementation can result in decreased usability and acceptance of the assessment.33 For example, if the assessment is completed by an outside assessor and happens at arm’s length from clinical care, it can be viewed as a monitoring tool and will have limited clinical use. Likewise, if the assessment is not embedded within routine electronic medical record systems and business intelligence software features have not been optimized (eg, calculated scales are not presented in a logical location), it can lead to double documentation and assessment burden. Finally, in some instances, the interRAI LTCF may lack granularity to determine the cause of negative outcomes. For example, although it may identify a resident is demonstrating signs of delirium, it may not provide a cause for treatment to target. However, the interRAI LTCF will alert clinicians to the problem, instigating action where none may have occurred prior.
Conclusions and Implications
LTC residents, isolated because of the COVID-19 pandemic, are at increased risk for negative outcomes. Our analyses demonstrate that poor mental health outcomes associated with lockdown in LTC homes can not only be measured but mitigated with thoughtful interventions. Clinical information systems, such as the interRAI LTCF, were essential in easily measuring changes in resident status that occurred in the homes through lockdown. Policy makers can use the associated outputs to guide resource deployment, and health service researchers can examine the data to identify better management strategies for when pandemic strikes again.
Acknowledgments
We gratefully acknowledge the contributions of the LTC homes that are part of Les Visionnaires network.
A portion of this work was funded by a grant from Canadian Frailty Network.
CM, MS, GH, NW, and JH are members of interRAI, a not-for-profit international scientific organization. George Heckman receives salary support from the Schlegel Research Chair in Geriatric Medicine.
References
- 1.Fisman D.N., Bogoch I., Lapointe-Shaw L. Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Netw Open. 2020;3:e2015957. doi: 10.1001/jamanetworkopen.2020.15957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Key strategies to prepare for COVID 19 in LTCFs. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care-strategies.html Available at:
- 3.Williams D. 2020. COVID-19 Directive #3 for Long-Term Care Homes under the Long-Term Care Homes Act. Toronto, Ontario. [Google Scholar]
- 4.Simard J., Volicer L. Loneliness and isolation in long-term care and the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21:966–967. doi: 10.1016/j.jamda.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexopoulos G.S. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 6.Brown M.N., Lapane K.L., Luisi A.F. The management of depression in older nursing home residents. J Am Geriatr Soc. 2002;50:69–76. doi: 10.1046/j.1532-5415.2002.50010.x. [DOI] [PubMed] [Google Scholar]
- 7.Davison T.E., Mccabe M.P., Mellor D. The prevalence and recognition of major depression among low-level aged care residents with and without cognitive impairment. Aging Ment Health. 2007;11:82–88. doi: 10.1080/13607860600736109. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association . 5th edition. American Psychiatric Association; Washington, DC: 2014. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- 9.Ciampi A., Bai C., Dyachenko A. Longitudinal patterns of delirium severity scores in long-term care settings. Int Psychogeriatr. 2017;29:11–17. doi: 10.1017/S104161021600137X. [DOI] [PubMed] [Google Scholar]
- 10.Hirdes J.P., Mitchell L., Maxwell C.J., White N. Beyond the “iron lungs of gerontology”: Using evidence to shape the future of nursing homes in Canada. Can J Aging. 2011;30:371–390. doi: 10.1017/S0714980811000304. [DOI] [PubMed] [Google Scholar]
- 11.Alzheimer’s Society of Canada Responsive behaviours. http://alzheimer.ca/en/bc/Living-with-dementia/Caring-for-someone/Understanding-symptoms/Responsive-behaviours Available at:
- 12.Röhr S., Müller F., Jung F. Psychosocial impact of quarantine measures during serious coronavirus outbreaks: A rapid review. Psychiatr Prax. 2020;47:179–189. doi: 10.1055/a-1159-5562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trabucchi M., De Leo D. Nursing homes or besieged castles: COVID-19 in northern Italy. Lancet Psychiatry. 2020;7:387–388. doi: 10.1016/S2215-0366(20)30149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chu C.H., Donato-Woodger S., Dainton C.J. Competing crises: COVID-19 countermeasures and social isolation among older adults in long-term care. J Adv Nurs. 2020;76:2456–2459. doi: 10.1111/jan.14467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott I. Chronic disease management: a primer for physicians. Intern Med J. 2008;38:427–437. doi: 10.1111/j.1445-5994.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- 16.Hirdes J.P., Ljunggren G., Morris J.N. Reliability of the interRAI suite of assessment instruments: A 12-country study of an integrated health information system. BMC Health Serv Res. 2008;8:277. doi: 10.1186/1472-6963-8-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gray L.C., Berg K., Fries B.E. Sharing clinical information across care settings: The birth of an integrated assessment system. BMC Health Serv Res. 2009;9:71. doi: 10.1186/1472-6963-9-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koehler M., Rabinowitz T., Hirdes J. Measuring depression in nursing home residents with the MDS and GDS: An observational psychometric study. BMC Geriatr. 2005;5:1. doi: 10.1186/1471-2318-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirdes J.P., Retalic T., Muskat C. The Seniors Quality Leap Initiative (SQLI): An international collaborative to improve quality in long-term care. J Am Med Dir Assoc. 2020;21:1931–1936. doi: 10.1016/j.jamda.2020.07.024. [DOI] [PubMed] [Google Scholar]
- 20.Company C.B. Connected loved ones. https://www.cbc.ca/news/canada/new-brunswick/connected-loved-ones-coronavirus-1.5530898 Available at:
- 21.Province of New Brunswick COVID-19 in New Brunswick. https://www2.gnb.ca/content/gnb/en/news/news_release.2020.04.0222.html Available at:
- 22.Morris J.N., Berg K., Bjorkgren M. interRAI; Washington, DC: 2010. InterRAI Clinical Assessment Protocols (CAPs) for Use with Community and Long-Term Care Assessment Instruments, Version 9.1. [Google Scholar]
- 23.Perlman C.M., Hirdes J.P. The aggressive behavior scale: A new scale to measure aggression based on the minimum data set. J Am Geriatr Soc. 2008;56:2298–2303. doi: 10.1111/j.1532-5415.2008.02048.x. [DOI] [PubMed] [Google Scholar]
- 24.Hirdes J.P., Frijters D.H., Teare G.F. The MDS-CHESS scale: A new measure to predict mortality in institutionalized older people. J Am Geriatr Soc. 2003;51:96–100. doi: 10.1034/j.1601-5215.2002.51017.x. [DOI] [PubMed] [Google Scholar]
- 25.Morris J.N., Fries B.E., Morris S.A. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 26.Morris J.N., Fries B.E., Mehr D.R. MDS cognitive performance scale. J Gerontol. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 27.Gerritsen D.L., Steverink N., Frijters D.H.M. A revised Index for Social Engagement for long-term care. J Gerontol Nurs. 2008;34:40–48. doi: 10.3928/00989134-20080401-04. [DOI] [PubMed] [Google Scholar]
- 28.Van der Roest H., Prins M., van der Velden C. The impact of COVID-19 measures on well-being of older long-term care facility residents in the Netherlands. J Am Med Dir Assoc. 2020;21:1569–1570. doi: 10.1016/j.jamda.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inouye S.K. Delirium in hospitalized older patients: Recognition and risk factors. J Geriatr Psychiatry Neurol. 1998;11:118–125. doi: 10.1177/089198879801100302. [DOI] [PubMed] [Google Scholar]
- 30.Chau R., Kissane D.W., Davison T.E. Risk factors for depression in long-term care: A systematic review. Clin Gerontol. 2019;42:224–237. doi: 10.1080/07317115.2018.1490371. [DOI] [PubMed] [Google Scholar]
- 31.Stutte K., Hahn S., Fierz K., Zúñiga F. Factors associated with aggressive behavior between residents and staff in nursing homes. Geriatr Nurs (Minneap) 2017;38:398–405. doi: 10.1016/j.gerinurse.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Castle N.G., Hyer K., Harris J.A., Engberg J. Nurse aide retention in nursing homes. Gerontologist. 2020;60:885–895. doi: 10.1093/geront/gnz168. [DOI] [PubMed] [Google Scholar]
- 33.Turcotte L.A., Tran J., Moralejo J. Evaluation of a staff training programme to reimplement a comprehensive health assessment. BMJ Open Qual. 2018;7 doi: 10.1136/bmjoq-2018-000353. [DOI] [PMC free article] [PubMed] [Google Scholar]