To the Editor:
The coronavirus disease 2019 (COVID-19) pandemic has had tremendous impact on health-care systems by requiring diversion of resources to focus on the immediate needs of critically ill patients while postponing “nonessential” services, including lung cancer screening (LCS) low-dose CT scanning (LDCT).1 , 2 Although annual LCS is recommended for high-risk individuals,3 the risk of COVID-19 exposure for both patients and health-care workers may outweigh the benefits amidst the pandemic.1 As a result, multiple organizations recommended delaying LCS.1 , 4, 5, 6 Postponement of baseline and follow-up examinations, especially for high-risk patients with Lung-RADS (LR; American College of Radiology) categories 3 (1%-2% probability of malignancy) and 4 (5%-15% probability of malignancy), may result in delayed diagnosis and treatment of lung cancer.7 The purpose of our study was to assess how LCS LDCT volume was impacted by the COVID-19 pandemic.
Materials and Methods
Study Setting and Data Collection
This is a single-institution, retrospective review that is compliant with the Health Insurance Portability and Accountability Act and approved with exemption by our Institutional Review Board. At our institution, patients are referred to LCS by affiliated providers after shared decision-making conversations, and LCS examinations that require follow-up evaluation are tracked by our LCS manager/navigator. Data on all LCS LDCT and non-LCS chest CT scans in our system between January 1, 2020, and July 25, 2020, were extracted from the electronic medical record. During the 2020 COVID-19 surge in Massachusetts (March and April 2020), initial and annual examinations were postponed until August or September in compliance with hospital policy. Six-month (LR3) and 3-month (LR 4A, B, X) follow-up examinations were not postponed. All patients who were past due for the follow up were identified to accomplish compliance with follow-up examinations, and our LCS program manager and navigator contacted patients and physician offices by letters (Fig 1 ), phone calls, and the electronic medical record patient portal. Our LCS program manager also contacted providers and patients to reassure them of safety measures instituted across our hospital sites. Shared decision-making conversations for any new baseline examinations during the post-COVID peak were conducted as part of telehealth provider visits.
Figure 1.
A, A sample letter sent by our program manager to patients who missed their follow-up lung cancer screening low-dose CT scan. B, A sample message sent to referring providers or their offices to notify them of patients who missed their lung cancer screening low-dose CT study.
Analysis
Three time periods were analyzed: (1) “pre-COVID peak”: January 1 through February 29, 2020 (weeks 1 through 8), prior to LCS scheduling changes in March; (2) “COVID peak”: March 1 through May 2, 2020 (weeks 9 through 17), during which annual and initial LCS examinations were postponed due to COVID-19 surge in Massachusetts; and (3) “post-COVID peak”: May 3 through July 25, 2020 (weeks 10 through 29), after resumption of normal LCS scheduling.
Results
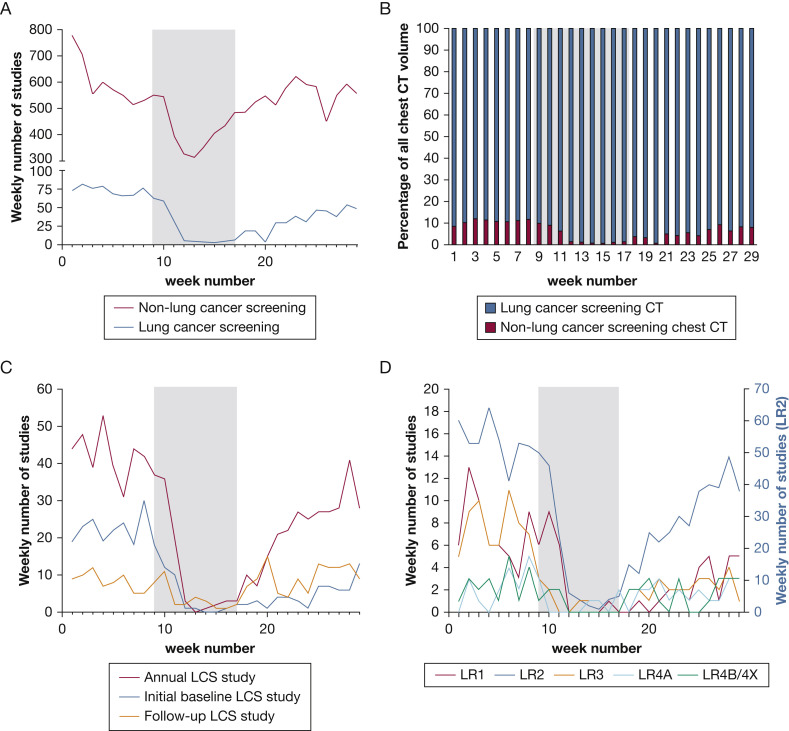
Average weekly non-LCS chest CT volume decreased by 29% from the pre-COVID peak period to the COVID peak period and recovered to 92% of pre-COVID peak levels during the post-COVID peak period (Fig 2 A). The average weekly LCS LDCT volume decreased by 74% from the pre-COVID peak period to the COVID peak period, followed by gradual recovery, reaching 68% of average pre-COVID peak LCS weekly volume by the end of July (week 29) (Fig 2A). An average 10.8% of the weekly overall chest CT volume were LCS studies during the pre-COVID-peak period compared with 3.6% during the COVID peak period, which recovered to 8.1% by the end of July (week 29) (Fig 2B).
Figure 2.
A-D, Lung cancer screening CT scan volume trend from January 1 through July 25, 2020. A, Overall lung cancer screening low-dose CT scan volume and non-lung cancer screening chest CT scan volume trend. B, Relative proportion of lung cancer screening low-dose CT volume to non-lung cancer screening chest CT scan volume. C, Trend in annual, initial baseline, and follow-up lung cancer screening low-dose CT scan volumes. D, Trend in lung cancer screening low-dose CT scan volume based on lung imaging data and reporting system category. The shaded time period in each panel indicates the “COVID peak” period, with preceding “pre-COVID peak” period and following “post-COVID peak” period. LCS = lung cancer screening; LR = Lung-RADS.
During the COVID peak period, annual LCS LDCT volume and baseline LCS LDCT study volume decreased by approximately 72% and 78%, respectively, from the pre-COVID peak period, whereas follow-up LCS LDCT volume decreased by approximately 50% (Fig 1C). Both annual and initial baseline LCS LDCT study volumes remained decreased during the post-COVID peak period, whereas follow-up LCS LDCT volume returned to similar levels as the pre-COVID peak period (Fig 2C). LCS volume of all LR categories decreased during the COVID-peak period, followed by recovery of all LR categories during the post-COVID peak period, with complete recovery of LR 4A and LR 4B/4X categories by week 29. (Fig 2D).
Discussion
Institutional LCS LDCT volume disproportionally and significantly decreased during the COVID-19 pandemic compared with non-LCS chest CT volume, followed by complete recovery of follow-up LCS volume and more gradual recovery of annual and baseline LCS LDCT volume. LCS volume decreased by a greater proportion than non-LCS chest CT scans, which reflects the outpatient nature of LCS and exigencies of inpatient imaging.8 As daily COVID-19 cases declined in Massachusetts and our hospital resumed routine scheduling of LCS in May, LCS CT volume began to recover. The delay in LCS volume recovery may reflect postponement of imaging appointments by patients and providers due to ongoing concerns about the pandemic and the slow recovery of routine visits by primary care providers. The backlog of LCS cases may further impact clinical and imaging operations in the future.
During the COVID-peak period, our departmental policy was to keep scheduled LCS LDCT studies for LR grades 3 and 4A follow-up examinations, as well as follow-up examinations that were 3 or 6 months past due. However, we noticed an initial decrease in volume across all LR category studies, including LR grades 3 and 4. The initial decline in LCS LDCT volume across all LR categories was mitigated through efforts of our department and our navigator, including letters, email messages, phone calls, and electronic reminders to both patients and referring providers. These efforts led to robust and complete recovery of LR category 4 studies and 3- and 6-month follow-up LCS volume, with ongoing recovery of annual follow up and baseline LCS volumes by the end of the study period. This highlights the active role that LCS programs must take to ensure continuity of follow up of high-risk patients to decrease the possibility of delayed diagnosis or treatment of lung cancer. Additional proactive outreach and recovery efforts may be needed for more vulnerable communities because the COVID-19 pandemic has disproportionately affected minority and marginalized communities.9 , 10
In conclusion, we report initial sharp decreases in institutional LCS LDCT volume during the COVID-19 pandemic, followed by an encouraging recovery of volume, especially for higher risk category follow-up examinations. A more gradual recovery of LCS LDCT volume compared with non-LCS chest CT volume highlights the importance of planning for the challenges of LCS programs during this ongoing global pandemic.
Acknowledgments
Other contributions: We thank MaryAnn Tateosian, MM, for her efforts as our LCS program manager and navigator that contributed to the recovery of our LCS LDCT volume.
Footnotes
M. D. Succi and B. P. Little contributed equally to this work.
FINANCIAL/NONFINANCIAL DISCLOSURES: The authors have reported to CHEST the following: B. P. L. is a textbook author and associate editor for Elsevier and receives royalties for his prior work not related to this manuscript. M. D. S. reports personal fees and nonfinancial support from 2 Minute Medicine, Inc, and royalties from Frequency Therapeutics for work not related to this manuscript. E. J. F. reports grant funding from the American College of Radiology Innovation Fund and the National Cancer Institute Research Diversity Supplement for work not related to this manuscript. J. O. S. receives royalties as an author from Elsevier. A. Sharma has received research support from Hummingbird Diagnostics Inc for unrelated work and is a textbook sub-editor for Elsevier. A. Som is a board member, chief medical officer, and shareholder of CareSignal, a digital health company that helps health-care systems with remote deviceless patient monitoring for chronic disease management, and is a board member of Sling Health, a medical student innovation incubator. This relationship is not related in any way to the subject of this article, lung cancer screening, or radiology. None declared (M. L., T. Y., M. P., T. C. M., S. S., A. M. P.).
References
- 1.Mazzone P.J., Gould M.K., Arenberg D.A., et al. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST expert panel report. Chest. 2020;158(1):406-415 doi: 10.1016/j.chest.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lang M., Yeung T., Mendoza D.P., et al. Imaging volume trends and recovery during the COVID-19 pandemic: a comparative analysis between a large urban academic hospital and its affiliated imaging centers. Acad Radiol. 2020;27(10):1353-1362 doi: 10.1016/j.acra.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer V.A., Force US Preventive Services Task Force Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 4.Information for Healthcare Professionals about Coronavirus (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Findex.html
- 5.ACR COVID-19 Clinical Resources for Radiologists. American College of Radiology. https://www.acr.org/Clinical-Resources/COVID-19-Radiology-Resources
- 6.Cancer Screening During the COVID-19 Pandemic. American Cancer Society. https://www.cancer.org/healthy/find-cancer-early/cancer-screening-guidelines/cancer-screening-during-covid-19-pandemic.html
- 7.Lung CT Screening Reporting and Data System (Lung-RADS) https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads
- 8.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020;296(3):E141-E144 doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joseph N.P., Reid N.J., Som A., et al. Racial/ethnic disparities in disease severity on admission chest radiographs among patients admitted with confirmed COVID-19: a retrospective cohort study. Radiology. 2020;297(3):E303–E312. doi: 10.1148/radiol.2020202602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]