Abstract
Over the past two decades, Medicare and other payers have been looking at ways to base payment for cardiovascular care on the quality and outcomes of care delivered. Public reporting of hospital performance on a series of quality measures began in 2004 with basic processes of care such as aspirin use and influenza vaccination, and it expanded in later years to include outcomes such as mortality and readmission rates. Following the passage of the Affordable Care Act in March 2010, Medicare and other payers moved forward with pay-for-performance programs, more commonly referred to as value-based purchasing (VBP) programs. These programs are largely based on an underlying fee-for-service payment infrastructure and give hospitals and clinicians bonuses or penalties based on their performance. Another new payment mechanism, called alternative payment models (APMs), aims to move towards episode-based or global payments to improve quality and efficiency. The two most relevant APMs for cardiovascular care include Accountable Care Organizations and bundled payments. Both VBP programs and APMs have challenges related to program efficacy, accuracy, and equity. In fact, despite over a decade of progress in measuring and incentivizing high-quality care delivery within cardiology, major limitations remain. Many of the programs have had little benefit in terms of clinical outcomes yet have led to marked administrative burden for participants.
However, there are several encouraging prospects to aid the successful implementation of value-based high-quality cardiovascular care, such as more sophisticated data science to improve risk adjustment and flexible electronic health records to decrease administrative burden. Furthermore, payment models designed specifically for cardiovascular care could incentivize innovative care delivery models that could improve quality and outcomes for patients. This review provides an overview of current efforts, largely at the federal level, to pay for high-quality cardiovascular care and discusses the challenges and prospects related to doing so.
Keywords: pay for performance, value-based purchasing, alternative payment models, cardiovascular care
INTRODUCTION
The last two decades saw remarkable changes in the way that quality and performance in cardiovascular care were measured and incented (Figure 1). Beginning in the early 2000s and accelerating following the passage of the Affordable Care Act (ACA) in March 2010, Medicare and other payers have increasingly moved towards value-based and alternative payment models in which payment is tied to the quality and outcomes of care. However, the focus on payment for quality and outcomes has heightened the need to ensure accurate and equitable measurement. This manuscript provides an overview of past and current efforts, largely at the federal level, to pay for high-quality cardiovascular care and discusses the challenges and prospects related to doing so.
Figure 1.
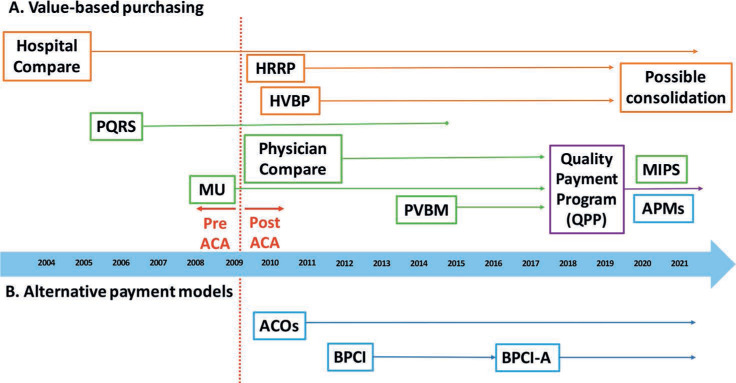
Timeline of federal efforts to improve quality of cardiovascular care. (A) Timeline for various value-based purchasing (VBP) programs divided by hospital-level (orange) and physician-level programs (green). The HRRP and HVBP were created after the ACA and will potentially be consolidated, with other federal hospital programs, into a single program in 2022. Prior physician-level programs such as PQRS, MU, and PVBM were consolidated into the QPP in 2019. The QPP has two main components, MIPS and APMs. (B) The two main APMs for cardiovascular care include ACOs and BPCI-A. ACA: Affordable Care Act; ACO: Accountable Care Organization; APM: Alternative Payment Model; BPCI: Bundled Payments for Care Improvement; BPCI-A: Bundled Payments for Care Improvement-Advanced; HRRP: Hospital Readmissions Reduction Program; HVBP: Hospital Value-Based Purchasing Program; MIPS: Merit-based Incentive Payment System; MU: Meaningful Use Program; PQRS: Physician Quality Reporting System; PVBM: Physician Value-Based Modifier Program; QPP: Quality Payment Program
VALUE-BASED PAYMENT PROGRAMS IN CARDIOVASCULAR MEDICINE
The first step in the move towards measuring and rewarding performance in cardiovascular medicine was public reporting. In 2004, Hospital Compare was created as the first national public reporting program; it was designed to incentivize providers to improve their performance through peer pressure and to allow consumers to select providers based on performance. Hospitals were incented to participate because their annual Medicare payment updates were tied to reporting data to the federal government on a series of key quality measures. Initially, these measures only included processes of care, such as aspirin being given for acute myocardial infarction; however, they expanded to include public reporting of clinical outcomes such as mortality and readmission rates for acute myocardial infarction and heart failure, added in 2008 and 2011, respectively.1
Following public reporting, Medicare and other payers moved forward with pay-for-performance programs, more commonly referred to as value-based purchasing (VBP) programs. One of the first such programs was the Hospital Readmissions Reduction Program, which penalized hospitals up to 3% of their Medicare reimbursements based on their readmission rates for heart failure, acute myocardial infarction, and pneumonia.
Hospital Value-Based Purchasing is another hospital-level program that was a component of the ACA. In this budget-neutral program, a portion of payments to hospitals are withheld and subsequently redistributed among hospitals based on their performance on a set of quality metrics in four core domains: safety, clinical care, efficiency and cost reduction, and patient/caregiver-centered experience. Cardiovascular disease features within each category, including specific measures such as heart failure mortality, acute myocardial infarction mortality, and, most recently, condition-specific cost measures for these two conditions.
A similar sequence of events, moving from public reporting to pay-for-performance, has taken place in the physician setting. The Physician Quality Reporting System was established in 2006 as a voluntary system but transitioned into a penalty program in 2011, when physicians and group practices faced negative payment adjustments for failing to report their performance data. Subsequently, a VBP program for physicians, the Physician Value-Based Modifier (PVBM), created a payment withhold that was redistributed according to how they performed on quality, outcome, and cost measures. Building on this program, the 2015 Medicare Access and CHIP Reauthorization Act created a mandatory nationwide Quality Payment Program that consists of two “tracks” for clinicians: (1) Merit-based Incentive Payment System (MIPS), or (2) alternative payment models (APMs) (Figure 2). The default program for practicing clinicians is MIPS, which has four core components that consist of quality, promoting interoperability (related to the Meaningful Use program), cost, and practice improvement activities (such as using patient portals and participating in quality improvement programs and registries). Clinicians can opt out of MIPS if they participate in a qualifying APM.
Figure 2.
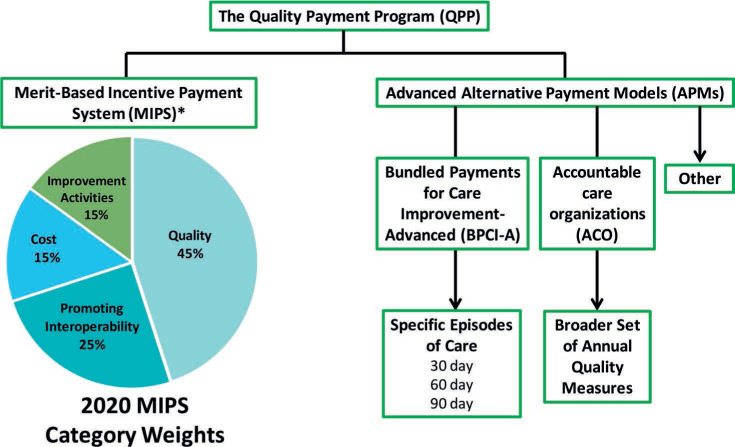
Diagram of the components within the Quality Payment Program (QPP). The QPP is composed of the Merit-Based Incentive Program (MIPS) and Alternative Payment Models (APMs). MIPS is the default program for clinicians and is composed of the following four elements (2020 weights reported): Quality 45%, Promoting Interoperability 25%, Cost 15%, Improvement Activities 15%. Clinicians can opt out of MIPs if they are enrolled in a qualifying APM; within cardiovascular care, this could mean either participating in an accountable care organization or being part of an organization that is participating in the Bundled Payments for Care Improvement-Advanced program.
ALTERNATIVE PAYMENT MODELS IN CARDIOVASCULAR MEDICINE
While VBP programs are largely based on an underlying fee-for-service payment infrastructure, APMs aim to disrupt the underlying payment mechanisms to move toward payment for quality and efficiency. The two most relevant APMs to cardiovascular care include Accountable Care Organizations (ACOs) and bundled payments. Accountable Care Organizations are groups of hospitals and clinicians that assume risk for a broader set of quality measures and for their attributed patients' total costs of care, typically on an annual basis. In Medicare's largest ACO program, the Medicare Shared Savings Program, participants are still paid on a fee-for-service basis but are held accountable for both the quality and cost of care provided to their beneficiaries each year. This program includes a number of cardiovascular quality measures, such as preventable hospitalizations for heart failure, readmission rates, and the use of certain medications for patients with ischemic heart disease or heart failure. Thus, while ACO programs depend heavily on high-quality primary care, cardiovascular specialists also play a major role in these organizations.
The other relevant APM for cardiovascular care is bundled payments, currently being tested by Medicare through the Bundled Payments for Care Improvement (BPCI) Advanced program. Bundled payment arrangements are similar to ACO arrangements except that quality and costs are evaluated over the course of an “episode,” which includes the continuum of care for a single medical event or condition such as a myocardial infarction or stroke. The episode is typically triggered by a hospitalization, and care is evaluated over a fixed, predetermined time, such as 30, 60, or 90 days in length, rather than an entire year. If Medicare payments for an episode of care are less than the target, the participant is eligible to keep a portion of the savings; however, if payments exceed the target, the participant must reimburse Medicare some of the difference.
CHALLENGES: EFFICACY
Despite transformational change over the past few decades, there are still challenges in determining a reimbursement method that leads to meaningful improvements in quality, outcomes, and costs (Figure 3). The most important challenge is efficacy because there is very little evidence that paying for performance in cardiovascular care, whether via VBP programs or APMs, has had a meaningful impact.
Figure 3.
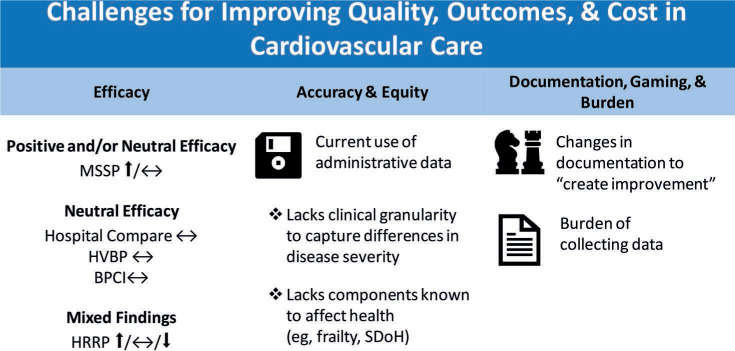
Challenges for improving quality, outcomes, and cost in cardiovascular care. The challenges facing the successful implementation of value-based, high-quality cardiovascular care include program efficacy, accuracy and equity, administrative burden, and data manipulation. BPCI: Bundled Payments for Care Improvement; HRRP: Hospital Readmissions Reduction Program; HVBP: Hospital Value-Based Purchasing Program; MSSP: Medicare Shared Savings Program; SDoH: social determinants of health
For example, the public reporting of processes and outcomes on Hospital Compare was not associated with improvements in mortality rates above and beyond secular trends,2 and evaluations of value-based payment programs have been similarly disappointing. Studies have failed to find any association between the implementation of hospital value-based purchasing and improvement in patient outcomes.3,4 The Hospital Readmissions Reduction Program (HRRP) has been associated with a significant decrease in readmission rates for Medicare beneficiaries,5 although subsequent analyses have suggested that some of the reported improvements may have been due to changes in coding of comorbidities rather than actual improvements in clinical care.6,7 Concerns have also been raised that the HRRP may have been associated with an increase in mortality for heart failure patients,8,9 although findings have been somewhat mixed.
Studies examining the effectiveness of APMs such as the Medicare Shared Savings Program have generally found that they are associated with small amounts of savings and no major improvements in quality or outcomes.10,11 Studies examining the predecessor of BPCI Advanced (formerly BPCI) have not demonstrated an association with improvements in quality, outcomes, or costs for medical conditions including heart failure or acute myocardial infarction.12
CHALLENGES: ACCURACY AND EQUITY
Another crucial challenge for using financial incentives to improve quality and outcomes in cardiovascular care is the issue of accuracy and equity. Here, the science of performance measurment is critical to consider. For many of the measures in cardiovascular quality improvement, risk adjustment is used in an attempt to level the playing field when comparing the respective performances of hospitals or practices. Most risk adjustment models use administrative claims data, which is easier and less resource intensive to implement compared to models that incorporate medical records and biometric data. However, administrative data lacks granularity on clinical comorbidities—for example, people are classified by whether or not they have heart failure rather than by their NYHA class or ejection fraction—and therefore may not capture true differences in disease severity. Most current claims-based risk adjustment models also lack information on frailty, adherence, social determinants of health, and other factors that strongly influence clinical outcomes.13–15 Consequently, models tend to be inaccurate in determining performance and can be inequitable when used to assign publicly reported performance scores or used in value-based payment programs. For example, the HRRP has penalized safety-net hospitals that care for clinically and socially high-risk populations despite data suggesting that roughly half of the worse performance of these hospitals is due to the complexity of the population they serve.16–18 The outpatient-based PVBM program also disproportionately penalized physicians and practices serving patients with high levels of social or medical risk.19,20
CHALLENGES: DOCUMENTATION, GAMING, AND BURDEN
Another concern for programs that measure and reward performance in cardiovascular medicine is that reporting entities may manipulate the data that gets reported or entered into administrative claims in order to increase the apparent risk of their patients. For example, as noted above, two studies have shown that the initial decrease seen in readmissions after the HRRP was implemented was due to changes in hospital documentation rather than underlying improvements in the quality of care.6 Similarly, a study examining changes in door-to-balloon time during public reporting for percutaneous coronary intervention quality measures showed that a significant amount of improvement over time was due to a higher proportion of cases being excluded for “diagnostic uncertainty” rather than true changes in processes of care.21
Another related challenge in value-based reimbursement is the burden of collecting and reporting data. Since many current quality measures cannot be automatically calculated from claims or even efficiently pulled from the electronic medical record, they require hand abstraction by trained personnel. Providers have to collect different measures for different payers and may even have to collect the same measures but in different formats across different payers. One study estimated that, on average, US-based physician practices spend 785 hours dealing with reporting of quality measures per physician on staff.22 The burden of collecting and reporting these measures can be particularly problematic for small hospitals and small practices, which may lack the necessary access to capital to invest in technological infrastructure and personnel; this may be one reason why consolidation continues to occur in the cardiovascular practice community.23
PROSPECTS: IMPROVING RISK ADJUSTMENT THROUGH DATA SCIENCE
Emerging methods in data science are being used to improve risk adjustment models, which may help address some of the limitations in measuring and rewarding performance in cardiovascular disease (Figure 4). When many of the current performance measures were developed, their sophistication was limited by computing power. However, better computing platforms and the ongoing explosion of progress in machine learning has led to increasingly sophisticated models that can more accurately predict clinical events (eg, mortality, acute kidney injury, bleeding risk) and therefore improve the fairness of performance measurement while also helping to better target clinical interventions.24–26
Figure 4.
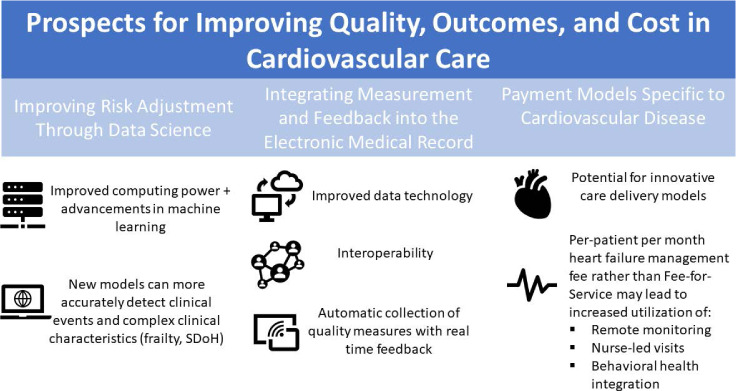
Prospects for improving quality, outcomes, and cost in cardiovascular care. Encouraging prospects for the successful implementation of value-based, high-quality cardiovascular care include the incorporation of improved data science for improved risk adjustment, decreased administrative burden, and potential innovative care delivery models. SDoH: social determinants of health
A number of recent studies have also shown that claims data can be used to detect more complex comorbidity states (eg, frailty), which holds significant promise for improving risk adjustment.27–31 The advent of codes for social determinants of health in the International Classification of Diseases-Tenth Edition (ICD-10) also may provide an opportunity to collect this information more broadly than in the past and incorporate these parameters into risk prediction.32
PROSPECTS: INTEGRATING MEASUREMENT AND FEEDBACK INTO ELECTRONIC MEDICAL RECORDS
The first electronic medical record (EMR) was introduced by IBM in the 1960s,33 but in many ways the promise of EMRs to improve quality and outcomes has still not been met.34 However, ongoing improvements in data technology and a renewed emphasis on interoperability and user interface35 could facilitate the automatic collection of quality measures with better risk adjustment as well as real-time feedback on performance.36 Faster, more relevant feedback could drive performance improvement in a way that the current time-lagged opaque metrics do not, therefore improving efficacy, accuracy, and fairness while reducing burden.
PROSPECTS: PAYMENT MODELS SPECIFIC TO CARDIOVASCULAR DISEASE
Another potential solution that could improve both efficacy and accuracy is the development of payment models that are specific to cardiovascular disease rather than “one size fits all.” In current programs such as MIPS, cardiologists, urologists, geriatricians, and other clinicians are all judged under one enormous program despite each practice having the option to submit data on any six of more than 300 distinct quality measures. Creating a payment model aimed at improving care and outcomes specifically for chronic cardiovascular disease could be an important tool in improving quality in this space. For example, a cardiology practice receiving a per-patient monthly management fee for heart failure rather than a visit-based fee-for-service might elect to implement remote patient monitoring, nurse-led visits, behavioral health integration, or other innovative care delivery models that aren't well reimbursed under the current system. Tying payment to specialty society-endorsed quality guidelines that are measured equivalently across practices could improve the accuracy of various models. Such innovation has the potential to fundamentally change how care is delivered to patients with chronic cardiovascular disease.
CONCLUSION
The ACA accelerated the attempt to deliver high-quality cardiovascular care, but many of the programs born from the ACA have had minimal to no benefit in terms of clinical outcomes while resulting in marked administrative burden. Furthermore, it remains unclear how accurate and equitable these programs have been, as they have been prone to gaming and associated with higher penalties for providers caring for high-risk populations. Despite these challenges, there are encouraging developments ahead. Improved integration of EMRs and advancements in machine learning and artificial intelligence will allow for more precise and accurate risk adjustment models while also decreasing administrative burden. In addition, novel payment models designed specifically for cardiovascular care could incentivize innovative care delivery models that could improve quality and outcomes for patients. With these prospects on the horizon, the new decade has the potential to bring us closer to an equitable, high-quality, value-based care delivery system.
KEY POINTS
Medicare and other payers are increasingly moving towards value-based purchasing programs and alternative payment models to improve quality and outcomes for patients.
Current efforts to improve care have challenges regarding program efficacy, accuracy and equity, administrative burden, and data manipulation.
There are encouraging prospects for the successful implementation of value-based, high-quality cardiovascular care, such as improvements in data science for risk adjustment, decreased administrative burden, and potential innovative care delivery models.
Footnotes
Conflict of Interest Disclosure:
Dr. Joynt Maddox does contract work for the United States Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. There are no other financial conflicts of interest to report.
REFERENCES
- 1.Wasfy JH, Borden WB, Secemsky EA, McCabe JM, Yeh RW. Public reporting in cardiovascular medicine: accountability, unintended consequences, and promise for improvement. Circulation. 2015 Apr 28;131(17):1518–27. doi: 10.1161/CIRCULATIONAHA.114.014118. [DOI] [PubMed] [Google Scholar]
- 2.Joynt KE, Orav EJ, Zheng J, Jha AK. Public Reporting of Mortality Rates for Hospitalized Medicare Patients and Trends in Mortality for Reported Conditions. Ann Intern Med. 2016 Aug 2;165(3):153–60. doi: 10.7326/M15-1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chee TT, Ryan AM, Wasfy JH, Borden WB. Current State of Value-Based Purchasing Programs. Circulation. 2016 May 31;133(22):2197–205. doi: 10.1161/CIRCULATIONAHA.115.010268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. Association between the Value-Based Purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016 May 9;353:i2214. doi: 10.1136/bmj.i2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zuckerman RB, Sheingold SH, Epstein AM. The Hospital Readmissions Reduction Program. N Engl J Med. 2016 Aug 4;375(5):494. doi: 10.1056/NEJMc1606658. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of Coded Severity With Readmission Reduction After the Hospital Readmissions Reduction Program. JAMA Intern Med. 2018 Feb 1;178(2):290–2. doi: 10.1001/jamainternmed.2017.6148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ody C, Msall L, Dafny LS, Grabowski DC, Cutler DM. Decreases In Readmissions Credited To Medicare's Program To Reduce Hospital Readmissions Have Been Overstated. Health Aff (Millwood) 2019 Jan;38(1):36–43. doi: 10.1377/hlthaff.2018.05178. [DOI] [PubMed] [Google Scholar]
- 8.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program With Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure, Acute Myocardial Infarction, and Pneumonia. JAMA. 2018 Dec 25;320(24):2542–52. doi: 10.1001/jama.2018.19232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A, Allen LA, Bhatt DL et al. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol. 2018 Jan 1;3(1):44–53. doi: 10.1001/jamacardio.2017.4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McWilliams JM, Hatfield LA, Landon BE, Hamed P, Chernew ME. Medicare Spending after 3 Years of the Medicare Shared Savings Program. N Engl J Med. 2018 Sep 20;379(12):1139–49. doi: 10.1056/NEJMsa1803388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McWilliams JM, Chernew ME, Landon BE. Medicare ACO Program Savings Not Tied To Preventable Hospitalizations Or Concentrated Among High-Risk Patients. Health Aff (Millwood) 2017 Dec;36(12):2085–93. doi: 10.1377/hlthaff.2017.0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare's Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018 Jul 19;379(3):260–9. doi: 10.1056/NEJMsa1801569. [DOI] [PubMed] [Google Scholar]
- 13.Johnston KJ, Wen H, Schootman M, Joynt Maddox KE. Association of Patient Social, Cognitive, and Functional Risk Factors with Preventable Hospitalizations: Implications for Physician Value-Based Payment. J Gen Intern Med. 2019 Aug;34(8):1645–52. doi: 10.1007/s11606-019-05009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnston KJ, Joynt Maddox KE. The Role Of Social, Cognitive, And Functional Risk Factors In Medicare Spending For Dual And Nondual Enrollees. Health Aff (Millwood) 2019 Apr;38(4):569–76. doi: 10.1377/hlthaff.2018.05032. [DOI] [PubMed] [Google Scholar]
- 15.Johnston KJ, Wen H, Hockenberry JM, Joynt Maddox KE. Association Between Patient Cognitive and Functional Status and Medicare Total Annual Cost of Care: Implications for Value-Based Payment. JAMA Intern Med. 2018 Nov 1;178(11):1489–97. doi: 10.1001/jamainternmed.2018.4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013 Jan 23;309(4):342–3. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 17.Joynt Maddox KE, Reidhead M, Hu J et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019 Apr;54(2):327–36. doi: 10.1111/1475-6773.13133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joynt Maddox KE, Reidhead M, Qi AC, Nerenz DR. Association of Stratification by Dual Enrollment Status With Financial Penalties in the Hospital Readmissions Reduction Program. JAMA Intern Med. 2019 Jun 1;179(6):769–76. doi: 10.1001/jamainternmed.2019.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen LM, Epstein AM, Orav EJ, Filice CE, Samson LW, Joynt Maddox KE. Association of Practice-Level Social and Medical Risk With Performance in the Medicare Physician Value-Based Payment Modifier Program. JAMA. 2017 Aug 1;318(5):453–61. doi: 10.1001/jama.2017.9643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts ET, Zaslavsky AM, McWilliams JM. The Value-Based Payment Modifier: Program Outcomes and Implications for Disparities. Ann Intern Med. 2018 Feb 20;168(4):255–65. doi: 10.7326/M17-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCabe JM, Kennedy KF, Eisenhauer AC et al. Reporting trends and outcomes in ST-segment-elevation myocardial infarction national hospital quality assessment programs. Circulation. 2014 Jan 14;129(2):194–202. doi: 10.1161/CIRCULATIONAHA.113.006165. [DOI] [PubMed] [Google Scholar]
- 22.Casalino LP, Gans D, Weber R et al. US Physician Practices Spend More Than $15.4 Billion Annually To Report Quality Measures. Health Aff (Millwood) 2016 Mar;35(3):401–6. doi: 10.1377/hlthaff.2015.1258. [DOI] [PubMed] [Google Scholar]
- 23.Baker LC, Pesko M, Ramsay P, Casalino LP, Shortell SM. Med Care Res Rev. 2018. Nov 22, Are Changes in Medical Group Practice Characteristics Over Time Associated With Medicare Spending and Quality of Care? 1077558718812939. [DOI] [PubMed] [Google Scholar]
- 24.Mortazavi BJ, Bucholz EM, Desai NR et al. Comparison of Machine Learning Methods With National Cardiovascular Data Registry Models for Prediction of Risk of Bleeding After Percutaneous Coronary Intervention. JAMA Netw Open. 2019 Jul 3;2(7):e196835. doi: 10.1001/jamanetworkopen.2019.6835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang C, Murugiah K, Mahajan S et al. Enhancing the prediction of acute kidney injury risk after percutaneous coronary intervention using machine learning techniques: A retrospective cohort study. PLoS Med. 2018 Nov 27;15(11):e1002703. doi: 10.1371/journal.pmed.1002703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krumholz HM, Coppi AC, Warner F et al. Comparative Effectiveness of New Approaches to Improve Mortality Risk Models From Medicare Claims Data. JAMA Netw Open. 2019 Jul 3;2(7):e197314. doi: 10.1001/jamanetworkopen.2019.7314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. How Do Frail Medicare Beneficiaries Fare Under Bundled Payments? J Am Geriatr Soc. 2019 Nov;67(11):2245–53. doi: 10.1111/jgs.16147. [DOI] [PubMed] [Google Scholar]
- 28.Johnston KJ, Wen H, Joynt Maddox KE. Inadequate Risk Adjustment Impacts Geriatricians' Performance on Medicare Cost and Quality Measures. J Am Geriatr Soc. 2020 Feb;68(2):297–304. doi: 10.1111/jgs.16297. [DOI] [PubMed] [Google Scholar]
- 29.Kim DH, Glynn RJ, Avorn J et al. Validation of a Claims-Based Frailty Index Against Physical Performance and Adverse Health Outcomes in the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2019 Jul 12;74(8):1271–6. doi: 10.1093/gerona/gly197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Segal JB, Chang HY, Du Y, Walston JD, Carlson MC, Varadhan R. Development of a Claims-based Frailty Indicator Anchored to a Well-established Frailty Phenotype. Med Care. 2017 Jul;55(7):716–22. doi: 10.1097/MLR.0000000000000729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring Frailty in Medicare Data: Development and Validation of a Claims-Based Frailty Index. J Gerontol A Biol Sci Med Sci. 2018 Jun 14;73(7):980–7. doi: 10.1093/gerona/glx229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weeks WB, Cao SY, Lester CM, Weinstein JN, Morden NE. Use of Z-Codes to Record Social Determinants of Health Among Fee-for-service Medicare Beneficiaries in 2017. J Gen Intern Med. 2020 Mar;35(3):952–5. doi: 10.1007/s11606-019-05199-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Akron's Children Hospital [Internet]. Akron, Ohio: Akron Children's Hospital; c2020. Electronic Medical Records: It's Back to the Future; 2012 Feb 20 [cited 2020 Apr 14[. Available from: https://inside.akronchildrens.org/2012/02/20/electronic-medical-records-its-back-to-the-future. [Google Scholar]
- 34.Kaiser Health News [Internet]. Schulte F, Fry E. Death By 1,000 Clicks: Where Electronic Health Records Went Wrong. Oakland, CA: Kaiser Family Foundation; c2020. 2019 Mar 18 [cited 2020 Apr 14]. Available from: https://khn.org/news/death-by-a-thousand-clicks. [Google Scholar]
- 35.American College of Cardiology [Internet]. Reducing Administrative Burden. Washington, DC: American College of Cardiology Foundation; c2020. c2019 [cited 2020 Apr 14]. Available from: https://www.acc.org/tools-and-practice-support/advocacy-at-the-acc/acc-health-care-principles/reducing-administrative-burden. [Google Scholar]
- 36.McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015 May 19;131(20):1796–803. doi: 10.1161/CIRCULATIONAHA.114.010270. [DOI] [PMC free article] [PubMed] [Google Scholar]


