Abstract
Objectives:
We describe the key elements for a New York City health system to rapidly implement telecritical care consultative services to a newly created ICU during the coronavirus disease 2020 patient surge.
Design:
This was a rapid quality-improvement initiative using public health decrees, a HIPAA-compliant and device-agnostic telemedicine patform, and a group of out-of-state intensivist volunteers to enhance critical care support. Telecritical care volunteers initially provided on-demand consults but then shifted to round twice daily with housestaff in a 12-bed newly created ICU.
Setting:
A 457-bed safety net hospital in the Bronx, NY, during the pandemic.
Subjects:
The 12-bed newly created ICU was staffed by a telecritical care attending, a cardiology fellow, and internal medicine residents.
Intervention:
Prior to the intervention, the ad hoc ICU was staffed by a cardiology fellow as the attending of record, with critical care support on demand. The intervention involved twice daily rounding with an out-of-state, volunteer intensivist.
Measurements and Main Results:
Volunteers logged 352 encounters. Data from 26 unique encounters during the initial on-demand consult pilot study of tele-ICU support were recorded. The most common interventions were diagnostic test interpretation, ventilator management, and sedation change. The majority of housestaff felt the new tele-ICU service improved the quality of care of patients and decreased anxiety of taking care of complex patients. Likewise, the majority of volunteers expressed making significant alterations to care, and 100% believed critical care input was needed for these patients. The largest lessons learned centered around mandating the use of the telecritical care volunteers and integration into a structured format of rounding.
Conclusions:
The need for rapid implementation of ICUs during a major public health crisis can be challenging. Our pilot study supports the feasibility of using an out-of-state telecritical care service to support ICUs, particularly in areas where resources are limited.
Keywords: coronavirus disease 2019, critical care, information technology, intensive care units, telehealth, telemedicine
The SARS-CoV-2 pandemic caused a major public health crisis and placed a significant strain on healthcare systems worldwide. The first case of coronavirus disease 2019 (COVID-19) in New York City (NYC) was reported on March 1, 2020, and, as of August 1, the virus caused more than 200,000 cases there (1). The pandemic disproportionately affected different boroughs of NYC, with the Bronx having the highest hospitalization and death rate of 634 and 173, respectively, per 100,000 people (2).
The overwhelming influx of critically ill patients left hospitals vulnerable, particularly in resource-limited institutions. In previous epidemics, telemedicine was used for tele-expertise when resources were limited (3). Despite improving clinical and financial outcomes, telecritical care services often require extensive resources, technical support, and implementation periods (4). As illustrated by the U.S. Navy, these investments can successfully be overcome, however, by implementing low-technology telecritical care in small, understaffed hospitals (5). We describe a rapid, low-cost, and successful deployment of a tele-ICU service implemented during the COVID-19 surge in NYC.
METHODS
This single-center, observational, quality-improvement initiative was implemented at Jacobi Medical Center (Jacobi) in the Bronx, NY. Jacobi, a member of the NYC Health + Hospitals System (NYC H+H), is a 457-bed safety-net hospital in the Bronx, NY. At normal capacity, there are 12 medical ICU beds and 32 additional beds in the cardiac ICU, burn ICU, and surgical ICU for adult patients. During the peak of the surge, ICU capabilities expanded by 150% to a total of 111 beds to accommodate the surge of critically ill patients (Fig. 1). There are a total of seven medical intensivists and two fellows. At normal capacity, one intensivist and one fellow staff in the medical ICU, and an additional intensivist and fellow staff in a mobile Critical Care Consult service. One overnight in-house intensivist oversees all ICU patients. Beyond the expanded use of existing ICUs to care for critically ill COVID-19 patients, ad hoc ICUs were rapidly added throughout the hospital by modifying prior step-down spaces or creating de novo ICU spaces.
Figure 1.
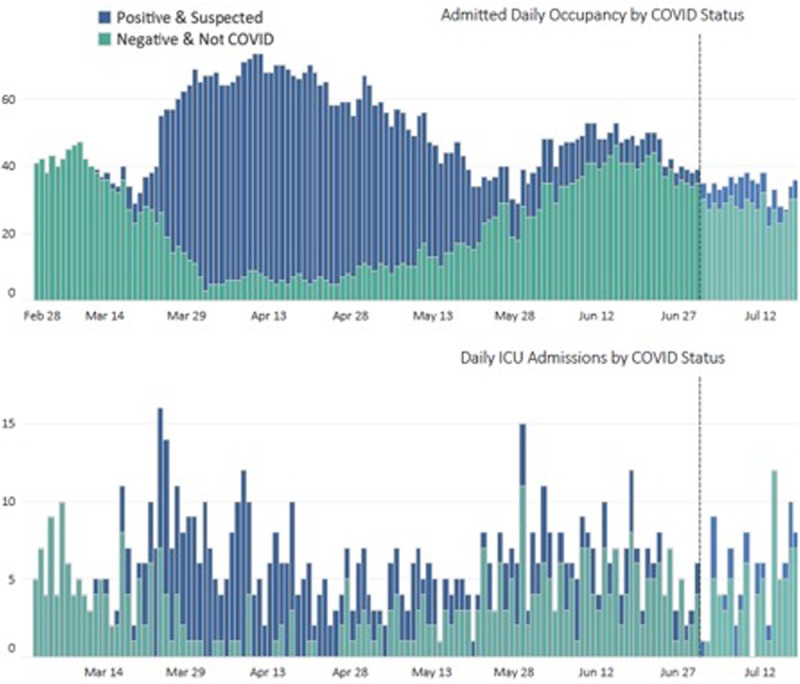
Illustration of the admitted daily occupancy and daily ICU admissions by coronavirus disease (COVID) status.
A 12-bed nontelemetry oncology floor was transformed into a COVID ICU. Because patients were triaged to this unit based on bed availability, no differences existed between the level of acuity of patients in the ad hoc ICU and the standard ICUs. The unit was staffed by medical residents supervised by a third-year cardiology fellow as the attending. Although in-house critical care fellows and attendings provided initial ICU support on a consultative basis, this coverage waned as the surge progressed and competing duties limited their availability. From the first reported case of COVID-19 at Jacobi on March 17 to April 18, 2020, 272 consults were logged, compared with 107 consults during the same period in 2019.
Because intensivist management has been associated with lower mortality and duration of mechanical ventilation (6), intensivist staffing was sought for the new ad hoc ICU. Despite extensive outreach to obtain on-the-ground critical care support from across the country, the hospital could not meet its in-person staffing needs for critical care support and, therefore, sought telecritical care support.
Due to the clinical needs of this 12-bed ICU, we piloted a tele-ICU program using a telecritical care volunteer (TCCV) physician in a consultative role. Herein, we outline the key elements needed to rapidly implement a telecritical care program. Because this effort was a quality-improvement study, Institutional Review Board approval was waived.
Declaration of a Public Health Emergency
New York State (NYS) declared a public health emergency that permitted professionals without NYS medical licenses to be able to practice physically or virtually in NYS on an emergency basis. The public health emergency also provided legal protections to any unpaid volunteer clinicians. Governor Andrew Cuomo released an Executive Order on March 23 indemnifying physicians while providing care during the COVID-19 crisis for anything short of gross negligence (7).
Recruitment of Volunteer Critical Care Specialists
The extensive search by the NYC H+H for in-person volunteers through the Society of Critical Care Medicine (SCCM) was largely successful, but it still did not meet the demand of the surge. Many potential volunteers were eager to help but could not leave their residence. Through existing prior relationships, TCCVs board-certified in medical or surgical critical care were recruited from the Baltimore Chapter of SCCM (Baltimore, MD) and Atrium Health (Charlotte, NC). Notably, both of these areas were not experiencing a large influx of COVID patients during the time of the pilot. Between April 18 and May 1, 41 volunteers were recruited.
Health System and Hospital Credentialing and Onboarding
Onboarding staff at NYC H+H provided TCCVs the emergency credentialing and rapid access to the electronic health record (EHR); in some cases, this occurred in under 72 hours. The online credentialing application was 56 questions and included demographic information, licensing information, and any prior charges (8). Recruited volunteers were sent a standard e-mail that included the link to the online credentialing form, along with instructions to select a specific field under current employer in order to streamline the TCCVs directly to the NYC H+H coordinator. Mandatory online HIPAA training was required after volunteer approval. The majority of TCCVs were familiar with the hospital’s EHR. Instead of traditional full-day EHR training, written instructions and a brief video were provided on how to access the patient’s clinical encounter, laboratory results, and imaging results, as well as how to write a note in the EHR.
One of the TCCVs (B.D.B.) served as a central coordinator to track onboarding progress and schedule shifts. He worked remotely with an on-site chief resident (S.R.) to ensure the medical team was aware of the process and knew who the assigned TCCV was for any given day.
Implementation of a Telemedicine Platform
A HIPAA-compliant platform (ICmed, LLC, Baltimore, MD) was used to provide secure video consultation from a tablet device in the ad hoc unit at Jacobi to the TCCVs remotely consulting from their personal web-enabled Android and Apple devices. The tablet device was already in use by the Department of Medicine and was analyzed by Information Technology to ensure proper security. The platform was available for download to any web-enabled device; however, we chose to have one central device for security reasons. No other equipment was purchased.
Many of the TCCVs were familiar with the chosen platform; thus, it was easily integrated into the workflow. The application allowed the housestaff to request to speak to the on-call TCCV without needing specific contact information for each TCCV, as would be required with other mainstream video services such as FaceTime or WhatsApp.
Implementing and Adjusting a Consultative and Rounding Workflow
The initial pilot study, from April 18 to April 28, involved on-demand consults from in-house providers to TCCVs, who were available for assistance during 24-hour shifts. The assigned TCCV would e-mail and text page the in-house providers before their shift to remind them of the service and encourage providers to call with any questions. Unfortunately, only 26 consults transpired during this time period. Due to the low volume of as-needed consults initiated despite a high volume of ICU patients needing expert critical care guidance, we transitioned to a more structured model of rounding in the ad hoc ICU. From April 29 to May 20, TCCVs covered 24-hour shifts, with the goal of covering at least two shifts in a row to maintain continuity. The Department of Medicine and Division of Cardiology mandated that the TCCV join formal morning and evening rounds with the medical team to establish care plans and to modify them according to clinical needs. The TCCV was also available for on-demand consults outside structured rounding times. The in-house Critical Care Consult team remained responsible for emergency requests across the hospital. Ultimately, the cardiology fellow remained the attending of record, and the TCCV acted in a consultative role. TCCVs did not having prescribing authority and did not bill for services. Recommendations were documented in the EHR in a daily progress note or event note, as each situation warranted.
RESULTS
From a total of 41 TCCVs emergency-credentialed, nine TCCV completed shifts. Encounters were logged into the online platform. The local medical teams initiated only 26 recorded consults with TCCVs during the initial pilot from April 18 to April 28. The most common interventions were diagnostic test interpretation (73.1%), ventilator change (61.5%), sedation change (53.8%), and vasoactive medication change (23.1%). However, after formal rounds with the TCCV were instituted, a total of 352 patient encounters were logged.
A postintervention survey was administered to 20 housestaff and nine TCCVs. Of the 20 house staff surveyed, 16 (80%) completed the questions. Of those 16, 62.5% strongly agreed or agreed that the tele-ICU service was a positive experience. Furthermore, 68.8% strongly agreed or agreed that having teleintensivist support improved the quality of care provided to critically ill patients and decreased anxiety of taking care of complex patients.
Of the nine TCCVs, six (66.6%) completed the survey. Of the six TCCVs completing the survey, 100% strongly agreed or agreed that the addition of critical care support was needed for these patients, and 83.3% strongly agreed or agreed that significant alterations in care plans were made. Furthermore, 83.3% integrating the teleintensivist into rounds was simple and easy.
DISCUSSION
Our pilot study from conception to implementation was completed in 3 weeks, and it highlighted our ability to rapidly deploy a TCCV-guided ad hoc ICU in a hospital that had not previously used telemedicine. The use of out-of-state intensivists proved to be essential, as we did not have enough in-state providers to meet the enormous influx of critically ill patients. Similar telecritical care programs were used in COVID-19 but were fortunate enough to use intensivists from their local network and had existing telehealth infrastructure.(9) To our knowledge, this is the first telecritical care model that has used out-of-state TCCV in an emergency setting. On a small scale, our study demonstrates that a National Emergency Tele-Critical Care Network (NETCCN) would be feasible.
The COVID-19 era highlights the need for healthcare organizations to maintain the ability to rapidly flex critical care space and deploy critical care expertise according to unpredictable surges in critically ill patients. Safety-net hospitals are particularly vulnerable to limitations of essential resources and may particularly benefit from the creation of a NETCCN to seamlessly leverage experts in areas less impacted by a particular disaster or insult (10). In the absence of a formalized telecritical care network, hospital systems or regional critical care organizations may consider maintaining a pool of potential volunteers or establishing alliances with other geographically removed hospital systems to provide mutual support according to fluctuating clinical demands.
For several reasons, telehealth has been widely recommended in lieu of in-person care during COVID-19 (11). For example, TCCVs can simultaneously be deployed to multiple hospitals rather than being limited to a single unit (12, 13). They have the added benefit of not having to use limited resources, such as personal protective equipment, and can provide medical care without risking their own exposure to a particular infectious insult.
LESSONS LEARNED
Our single-center, 12-bed unit observational study has obvious limitations when applied to other environments. The need to rapidly modify our interventions according to the evolving clinical environment at the time limited our ability to determine the direct effects of our novel intervention. However, given the dire clinical needs of the severely ill patients at Jacobi during the COVID-19 surge and the shortage of in-person critical care support, clinical circumstances demanded rapid implementation of novel solutions to deliver high-quality care.
The unpredictability of COVID-19 surges highlights the importance of the ability of hospital systems to quickly adapt care delivery to the clinical needs of the population. Implementing this initiative took approximately 3 weeks from conception. Several key factors allowed for rapid implementation. Adoption of disaster credentialing streamlined TCCV credentialing and malpractice coverage for out-of-state providers, as the usual process takes more than 3 months. Minimizing the amount of technical support required for remote care expedited the adoption of the new technology. For example, the only equipment needed was a software platform for secure video communication able to be accessed on existing tablets or smartphones, as well as remote access to the EHR. Unfortunately, consistently completing rounds inside patients’ rooms was not feasible due to challenges with sound on the tablet. Furthermore, because our EHR does not have ventilator-monitoring capability, rounds sometimes relied on noncontemporaneous data.
We also could have used any HIPAA-secure platform, as our main function of the platform was video consultation. Although the software platform was capable of both integrating clinical data from bedside equipment and interfacing with the EHR, those capabilities were not implemented due to time constraints. However, future iterations of this telecritical care model would benefit from activating those features.
The training provided to TCCV was the minimum amount necessary to be able to write a brief note, view imaging, and review laboratory results. We did not have the TCCVs bill for their encounters, as this would require more training. For a dedicated pool of providers used for future emergencies, more extensive EHR training could be provided, with specific attention to billing. Alternatively, if a NETCCN were created, providers could interface with several different EHRs, which could complicate training. Ideally, the NETCCN would have the ability for a central platform to interface with multiple EHRs (10).
Providing TCCVs a structured format is vital, especially for hospitals without existing telehealth services. Even though TCCVs were available for on-demand consults at the beginning of the pilot, the service was seldom used. Several explanations may exist for this. Any new service requires time for clinical adoption to demonstrate value. Adoption may have initially been delayed because Jacobi did not previously use any existing telehealth consultation services, and the concept was foreign to the housestaff. Furthermore, an existing in-person Critical Care Consult service was already highly used by the housestaff. Combining these factors with the use of unknown, out-of-state providers, the delays in clinical adoption were not particularly surprising. After the tele-ICU coverage was assigned to a specific medical unit and formally incorporated as a mandatory component of rounds, however, continuity of patient care and interpersonal relationships for both the TCCVs and local ICU teams was fostered, thereby accelerating tele-ICU use by the in-house ICU team. This approach enhanced adoption but may limit the TCCVs’ ability to oversee multiple units. Because a novel tele-ICU initiative such as this may be most successfully integrated into an already existing format, future exploration into integrating the telehealth services into the Critical Care Consult service, whereby certain calls are triaged by an in-house provider to telehealth providers, may facilitate greater deployment into existing workflows.
In preparation for future COVID or other disaster-related surges, NYC H+H is using information gathered from this pilot study to quickly implement tele-ICU services. Having TCCVs in a consultative role with a non-ICU clinician serving as the primary attending is ideal for flex units, as the non-ICU clinician is physically present to assist with procedures and conversations with consultants or family members.
CONCLUSIONS
Rapid implementation of critical care during a major public health crisis can be challenging, but deploying a telecritical care service to support newly formed ICUs is feasible.
Footnotes
Drs. Allison and McCurdy are advisors to the digital health company ICmed. The remaining authors have not disclosed any potential conflicts of interest.
This work was performed at Jacobi Medical Center, The Bronx, NY.
REFERENCES
- 1.NYC Health. COVID-19: Data, 2020. Available at: https://www1.nyc.gov/site/doh/covid/covid-19-data.page. Accessed August 15, 2020
- 2.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York city boroughs. JAMA 2020; 323:2192–2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohannessian R. Telemedicine: Potential applications in epidemic situations. European Research in Telemedicine 2015; 4:95–98 [Google Scholar]
- 4.Herasevich V, Subramanian S. Tele-ICU technologies. Crit Care Clin 2019; 35:427–438 [DOI] [PubMed] [Google Scholar]
- 5.Davis K, Perry-Moseanko A, Tadlock MD, et al. Successful implementation of low-cost tele-critical care solution by the U.S. navy: Initial experience and recommendations. Mil Med 2017; 182:e1702–e1707 [DOI] [PubMed] [Google Scholar]
- 6.Kapoor K, Verceles AV, Netzer G, et al. A collaborative cardiologist-intensivist management model improves cardiac intensive care unit outcomes. J Am Coll Cardiol 2017; 70:1422–1423 [DOI] [PubMed] [Google Scholar]
- 7.Cuomo A: Executive Order No. 202.10: Continuing Temporary Suspension and Modification of Laws Related to the Disaster Emergency. 2020 Available at: https://www.governor.ny.gov/news/no-20210-continuing-temporary-suspension-and-modification-laws-relating-disaster-emergency. Accessed September 21, 2020.
- 8.New York City Health + Hospitals: Disaster Volunteer Privileges Application. 2020 Available at: https://covid19.nychealthandhospitals.org/volunteer/. Accessed September 21, 2020.
- 9.Dhala A SF, Kash B, Ahmadi N, et al. Rapid implementation and innovative applications of a virtual intensive care unit during the COVID-19 pandemic: Case study. J Med Internet Res 2020; 22:e20143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott BK, Miller GT, Fonda SJ, et al. Advanced digital health technologies for COVID-19 and future emergencies. Telemed J E Health 2020; 26:1226–1233 [DOI] [PubMed] [Google Scholar]
- 11.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382:1679–1681 [DOI] [PubMed] [Google Scholar]
- 12.Subramanian S, Pamplin JC, Hravnak M, et al. Tele-critical care: An update from the Society of Critical Care Medicine Tele-ICU Committee. Crit Care Med 2020; 48:553–561 [DOI] [PubMed] [Google Scholar]
- 13.Adzhigirey LA, Ralkhelkar J, Panos RJ, et al. Building a Case for Tele-Critical Care to Improve Quality. Available at: https://www.sccm.org/Communications/Critical-Connections/Archives/2019/Building-a-Case-for-Tele-Critical-Care-to-Improve. Accessed May 20, 2020.


