Abstract
Meniscal radial root tears can disrupt the load-bearing function of the meniscus and worsen instability in anterior cruciate ligament–deficient knees. Paracentral radial tears adjacent to the root (types 1, 2, and 4) repaired with a transtibial pullout suture technique can lead to over-medialization of the meniscal root and a high-tension nonanatomic repair. We propose 2 all-inside techniques for anatomic repair of medial and lateral meniscal radial root tears with (1) an all-inside meniscal repair device and (2) an antegrade suture passer. We present the technical requirements and tips for these techniques. For lateral meniscal radial root repair with an all-inside meniscal repair device, ideal viewing is from an anterolateral portal with device entry from an anteromedial portal to reduce the risk of vascular injury. We recommend at least 2 stitches across the tear, with the depth setting limited to 18 to 20 mm for a central stitch and 16 mm or less for a peripherally placed stitch. For root repair with an antegrade suture passer, viewing should be from an anteromedial portal with the passer entering from an anterolateral portal. At least 2 stitches should be placed across the tear, with 1 central and 1 peripheral or 1 superior and 1 inferior.
Radial root tears in the meniscus disrupt its load-bearing function in the knee and increase compartment pressure by more than 25%.1 Meniscal repair can potentially restore compartment peak contact pressures to nearly normal. Lateral meniscal posterior root tears have been reported to reduce the stability of anterior cruciate ligament–deficient knees during rotational loading because they function as a secondary stabilizer of the knee under pivot-shift loading.2 In addition, pivot-shift grades in patients with lateral meniscal posterior root tears have been found to be significantly greater on preoperative physical examination than those in controls with no root tears.3 This finding suggests the influence of lateral meniscal root injury on rotational stability of the knee. Transtibial pullout suture repair of posterior meniscal root tears has been reported to yield improvements in function, pain, and activity level postoperatively.4
Not all lateral meniscal root tears are the same. In the meniscal root tear classification system of LaPrade et al.,5 types 1, 2, and 4 are paracentral radial tears adjacent to the root and types 3 and 5 are root avulsions. Paracentral radial tears repaired with a transtibial pullout suture technique can lead to over-medialization of the lateral meniscal root and, consequently, a high-tension repair. We propose 2 techniques to repair paracentral meniscal radial root tears that allow for residual meniscal root tissue (fixed to the anatomic root) to be incorporated into the repair, preventing over-medialization and high tension.
Indications for Surgery
The described anatomic repair techniques can be used for both medial and lateral radial root tears. However, traumatic radial lateral root tears are more commonly associated with anterior cruciate ligament injuries. Patients with multiple medical comorbidities or severe chondral changes (Outerbridge grade 3 or 4) in the ipsilateral compartment are excluded from repair. In patients with significant malalignment, corrective osteotomy should be considered before meniscal repair.
Surgical Technique
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table with a thigh tourniquet. After induction of general anesthesia, the foot of the table is removed, allowing the knee to be flexed at 90° and freely manipulated. The knee is examined for ligamentous stability and range of motion.
Diagnostic Arthroscopy
Standard anterolateral and anteromedial portals are made next to the patellar tendon. The knee joint is inspected with a 30° arthroscope. The root tear is probed and assessed for tear type. Root avulsions (types 3 and 5) can be repaired with a transtibial pullout suture technique. However, paracentral radial tears adjacent to the root (type 1, 2, and 4) with a significant stump are amenable to side-to-side repair techniques. We propose 2 side-to-side techniques for repair of radial meniscal root tears with a significant meniscal root stump, first with a FAST-FIX 360 all-inside meniscal repair device (Smith & Nephew, Andover, MA) and second with a Scorpion antegrade suture passer (Arthrex, Naples, FL). The first technique can be performed with any all-inside meniscal repair device. Similarly, the second technique can be performed with any available antegrade suture passer that can achieve access under the femoral condyles. The arthroscopic surgical techniques are explained in Video 1.
All-inside Meniscal Repair Device Technique
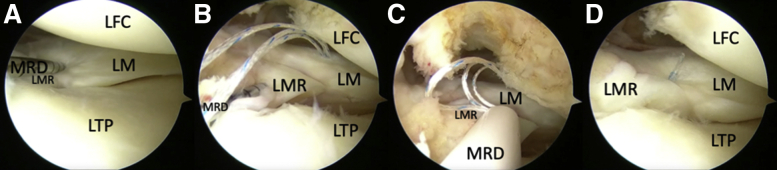
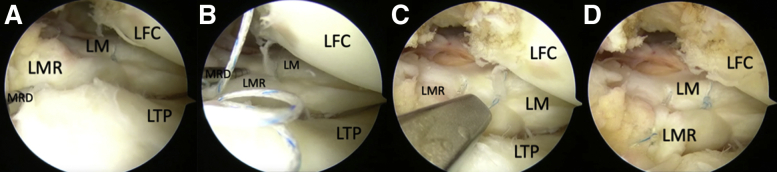
For lateral meniscal radial root repair with an all-inside meniscal repair device, the knee is placed in a figure-of-4 position. Ideal viewing of the lateral meniscus should be from an anterolateral portal with FAST-FIX 360 all-inside meniscal repair device entry guided by a slotted cannula (Fig 1) via an anteromedial portal to reduce the risk of vascular injury.6 There may sometimes be a requirement for the meniscal repair device to be introduced from the anterolateral portal for optimal stitch placement. This brings the tip of the repair device closest to the posterior vascular structures; therefore, the surgeon must be cognizant of the depth setting in relation to stitch placement to reduce the risk of vascular injury (Table 1). The depth limiter for the device is set at 18 to 20 mm when the entry point for the first side-to-side stitch in the meniscal root is in the central part of the meniscus. For a peripheral entry point in the red-red zone, we set the depth limiter to 16 mm or less. We recommend placement of at least 2 stitches across the tear (Fig 2).
Fig 1.
Arthroscopic image in a left knee from the anterolateral viewing portal, showing deployment of the all-inside meniscal repair device (MRD) from the anteromedial working portal into the lateral (A) and medial (B) parts of the paracentral lateral meniscal radial root. The suture repair is tensioned (C) and trimmed (D). (LFC, lateral femoral condyle; LM, lateral meniscus; LMR, lateral meniscal root; LTP, lateral tibial plateau.)
Table 1.
Tips on Using All-inside Meniscal Device
| Tip | |
|---|---|
| Portal | Lateral meniscal root repair: view from anterolateral portal and insert device from anteromedial portal (lower risk of vascular injury) In cases with small root remnant, device may be introduced from anterolateral portal (view from anteromedial portal) |
| Depth setting | Central stitch: 18- or 20-mm depth setting Peripheral stitch: ≤16 mm |
| Stitch configuration | ≥2 stitches across tear |
Fig 2.
Arthroscopic image in a left knee from the anterolateral viewing portal, showing deployment of a second all-inside meniscal repair device (MRD) from the anteromedial working portal into the lateral (A) and medial (B) parts of the paracentral lateral meniscal radial root. The suture repair is tensioned (C) and trimmed (D). (LFC, lateral femoral condyle; LM, lateral meniscus; LMR, lateral meniscal root; LTP, lateral tibial plateau.)
For medial meniscal radial root tear repair, viewing and device entry can be achieved from either aforementioned portal with the knee in 20° of flexion with a valgus force applied. A percutaneous medial collateral ligament release may help to improve visibility and access to the posterior horn of the medial meniscus.7 The surgeon should be comfortable with switching between the anteromedial and anterolateral portals for viewing and introduction of the all-inside meniscal repair device.
Antegrade Suture Passer Technique
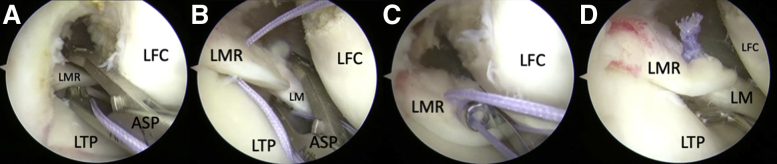
For lateral meniscal radial root repair, the knee is placed in a figure-of-4 position. Viewing should be from the anteromedial portal with the Scorpion antegrade suture passer entering from the anterolateral portal (Fig 3). Adequate access must be obtained under the femoral condyle to pass the sutures safely. The antegrade suture passer is loaded with an No. 2 Orthocord suture (Mitek, Raynham, MA) and passed through both sides of the radial tear. The knot is tied arthroscopically to bring the edges of the radial tear together. This technique can also be combined with an all-inside meniscal repair device technique for the second stitch. At least 2 stitches should be placed across the tear, with 1 central and 1 peripheral or 1 superior and 1 inferior (Table 2). This decision is subject to access to the meniscus, tissue quality, and distance between the first and second sutures. A cannula can be used for suture and soft-tissue management during knot tying. An absorbable suture is recommended because it reduces the risk of knot interference in the knee joint. It is important to use an antegrade suture passer that is designed for use in the knee and can gain access to the lateral meniscus under the lateral femoral condyle. For medial meniscal radial root tear repair, ideal viewing is from the anterolateral portal with antegrade suture passer entry from the anteromedial portal, with the knee in 20° of flexion and a valgus force applied.
Fig 3.
Arthroscopic image in a left knee from the anteromedial viewing portal, showing an No. 2 Orthocord suture passed with an antegrade suture passer (ASP) through the medial (A) and lateral (B) parts of the paracentral lateral meniscal radial root tear via the anterolateral working portal. Arthroscopic knots are tied (C) and cut with a short tail (D). (LFC, lateral femoral condyle; LM, lateral meniscus; LMR, lateral meniscal root; LTP, lateral tibial plateau.)
Table 2.
Tips on Using Antegrade Suture Passer
| Tip | |
|---|---|
| Portal | Lateral meniscal root repair: view from anteromedial portal and insert passer from anterolateral portal Medial meniscal root repair: view from anterolateral portal and insert passer from anteromedial portal |
| Stitch configuration | ≥2 stitches across tear: 1 central and 1 peripheral or 1 superior and 1 inferior |
| Suture management | Use of cannula can be considered |
Postoperative Protocol
After radial meniscal root tear repair, patients are placed in a knee brace with range of motion of 0° to 90° to limit deep knee flexion that can compromise the repair. They are also kept on protected weight bearing (≤50% weight on the operated leg) for 6 weeks.
Discussion
We describe all-inside meniscal repair device and antegrade suture passer techniques for meniscal radial root tear repair and present the technical requirements and tips for these techniques. Meniscal root tears should be repaired to restore meniscal hoop stresses. Posterior radial root tears that extend to the capsule and posterior horn attachments of the lateral meniscus are frequently amenable to repair. Anderson et al.8 found that 22 of 24 radial and posterior horn lateral meniscal tear repairs functioned successfully over a mean follow-up period of 58.6 months.
There are 2 main types of meniscal root tears. Paracentral radial tears adjacent to the meniscal root are more common than true root avulsions when associated with anterior cruciate ligament injuries. Meniscal root avulsions are repaired by passing sutures through the posterior root, drilling a transtibial tunnel, and securing the pullout sutures to a button on the tibial cortex. LaPrade et al.4 reported good results with transtibial meniscal root repair using pullout sutures, with patients having significantly improved postoperative outcome scores. Paracentral radial meniscal root tears (types 1, 2, and 4) ideally should not be repaired with transtibial pullout sutures. Such repairs would be potentially under high tension, with the meniscal posterior horn and body being overly medialized. There can be excessive tibiofemoral contact pressure after placement of pullout sutures, resulting in excessive tension and lack of normal physiological excursion.9
Our 2 side-to-side repair techniques for radial root tears allow for restoration of the natural meniscus position, anatomy, and tension. In meniscal repair, absorbable sutures have shown comparable healing rates to nonabsorbable sutures.10 We use a No. 2 Orthocord partially absorbable suture, which is in contrast to the absorbable No. 0 polydioxanone (PDS; Ethicon, Somerville, NJ) suture hook (Linvatec, Largo, FL) technique used by Ahn et al.11 This suture provides good handling and knot stability. The PDS component in Orthocord allows the knot profile to continue to diminish several months after surgery and has less bacterial adherence. We recommend placement of 2 stitches across the tear for optimal fixation.12 In our experience, when the repair was inspected, it was stable in all cases even when hyperflexion maneuvers were used.
For ease of repair, we highlight some technical considerations for each all-inside repair technique (Table 3). These considerations include surgeon comfort with using the meniscal repair device at various depth settings depending on where it is introduced in the meniscus, the ability to tie arthroscopic knots, and comfort in working with both the anteromedial and anterolateral portals for viewing and device introduction. We outline the risks, limitations, and advantages of our technique in Table 4.
Table 3.
Technical Requirements of Each Technique
| All-inside meniscal repair device |
| Comfort with using meniscal device |
| Awareness of depth setting at different regions—central and peripheral—and appropriate trajectory |
| Ability to work with different portals |
| Antegrade suture passer |
| Comfort with using suture passer for mattress configuration across radial tear |
| Ability to tie arthroscopic knots |
| Suture management |
Table 4.
Risks, Limitations, and Advantages
| Risks and limitations |
| Entails risk to popliteal vessels in lateral meniscal posterior root repair with all-inside repair device—requires care with choice of working portal and depth-limiter setting |
| Requires ability to tie knots arthroscopically |
| Advantages |
| Allows for more anatomic repair of meniscal root tears—restores tension and physiological excursion |
| Avoids additional incisions and/or bone tunnels that are required in transtibial pullout suture root repair |
Identification of meniscal radial root tears and awareness of repair techniques are becoming more common. We believe paracentral radial root tears with a significant stump are more anatomically repaired with side-to-side sutures with either an all-inside repair device or an antegrade suture passer.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.L.Y.H. receives travel grants for conferences from Smith & Nephew and J&J Mitek; receives speaker and consultant fees from Smith & Nephew and J&J Mitek; and receives a travel grant from Zimmer Biomet, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Two side-to-side techniques for repair radial meniscal root tears with a significant meniscal root stump are explained, first with an all-inside meniscal repair device and then with an antegrade suture passer. For lateral meniscal root repair with an all-inside meniscal repair device, the left knee is placed in a figure-of-4 position and viewed from the anterolateral portal. The repair device is introduced from the anteromedial portal guided by a slotted cannula. The depth limiter for the device is set at 20 mm for a central entry point and 16 mm for a peripheral entry point in the red-red zone. The 2 side-to-side stitches repair the radial root tear with restoration of the natural meniscus anatomy and tension. The second technique uses an antegrade suture passer. For lateral meniscal root repair, the knee in placed a figure-of-4 position and viewed from the anteromedial portal. The antegrade suture passer is loaded with an No. 2 Orthocord suture and introduced from the anterolateral portal. The suture is passed on both sides of the radial root tear and tied arthroscopically to bring the edges of the radial tear together.
References
- 1.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 2.Shybut T.B., Vega C.E., Haddad J. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament–deficient knee. Am J Sports Med. 2015;43:905–911. doi: 10.1177/0363546514563910. [DOI] [PubMed] [Google Scholar]
- 3.Minami T., Muneta T., Sekiya I. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. 2018;26:1174–1184. doi: 10.1007/s00167-017-4569-8. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 6.Mao D.W., Upadhyay U., Thalanki S., Lee D.Y.H. All-inside lateral meniscal repair via anterolateral portal increases risk of vascular injury: A cadaveric study. Arthroscopy. 2020;36:225–232. doi: 10.1016/j.arthro.2019.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Todor A., Caterev S., Nistor D.V. Outside-in deep medial collateral ligament release during arthroscopic medial meniscus surgery. Arthrosc Tech. 2016;5:e781–e785. doi: 10.1016/j.eats.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson L., Watts M., Shapter O. Repair of radial tears and posterior horn detachments of the lateral meniscus: Minimum 2-year follow-up. Arthroscopy. 2010;26:1625–1632. doi: 10.1016/j.arthro.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Seo J.-H., Li G., Shetty G.M. Effect of repair of radial tears at the root of the posterior horn of the medial meniscus with the pullout suture technique: A biomechanical study using porcine knees. Arthroscopy. 2009;25:1281–1287. doi: 10.1016/j.arthro.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Yoon K.H., Park J.-Y., Kwon Y.B., Lee Y.J., Kim E.J., Kim S.-G. Inside-out repair of the meniscus in concomitant anterior cruciate ligament reconstruction: Absorbable versus nonabsorbable sutures. Arthroscopy. 2020;36:1074–1082. doi: 10.1016/j.arthro.2019.08.045. [DOI] [PubMed] [Google Scholar]
- 11.Ahn J.H., Lee Y.S., Yoo J.C., Chang M.J., Park S.J., Pae Y.R. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:67–75. doi: 10.1016/j.arthro.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Jiang E.X., Everhart J.S., Abouljoud M. Biomechanical properties of posterior meniscal root repairs: A systematic review. Arthroscopy. 2019;35:2189–2206.e2. doi: 10.1016/j.arthro.2019.01.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two side-to-side techniques for repair radial meniscal root tears with a significant meniscal root stump are explained, first with an all-inside meniscal repair device and then with an antegrade suture passer. For lateral meniscal root repair with an all-inside meniscal repair device, the left knee is placed in a figure-of-4 position and viewed from the anterolateral portal. The repair device is introduced from the anteromedial portal guided by a slotted cannula. The depth limiter for the device is set at 20 mm for a central entry point and 16 mm for a peripheral entry point in the red-red zone. The 2 side-to-side stitches repair the radial root tear with restoration of the natural meniscus anatomy and tension. The second technique uses an antegrade suture passer. For lateral meniscal root repair, the knee in placed a figure-of-4 position and viewed from the anteromedial portal. The antegrade suture passer is loaded with an No. 2 Orthocord suture and introduced from the anterolateral portal. The suture is passed on both sides of the radial root tear and tied arthroscopically to bring the edges of the radial tear together.