Abstract
Introduction
Prostate cancer is treated with increasingly sophisticated radiation techniques. The aim of the study is to compare acute toxicity in patients managed with different therapeutic modalities.
Material and methods
A total of 60 patients irradiated between 2012 and 2016 were analyzed: A. conformal 3D – 11, B. intensity-modulated radiation therapy (IMRT) 20, C. image-guided radiation therapy (IGRT) – 19 and D. volumetric modulated arc therapy (VMAT) – 10. Patients' age ranged from 46 to 85 years (median 70.5), prostate-specific antigen values at the time of diagnosis were in the range of 3.54–154 ng/ml (median 15.9). Acute toxicity from the genitourinary (GU) and gastrointestinal (GI) tracts according to the European Organization for Research and Treatment of Cancer (EORTC) /Radiation Therapy Oncology Group (RTOG) grading system were assessed.
Results
All irradiation techniques were well tolerated and neither 3 nor 4 degrees acute toxicity was observed. Importantly, IGRT and IMRT did not lead to Grade 2 GI acute toxicity. There was no relationship between the severity of GU acute toxicity depending on the irradiation technique used (p = 0.8), but a trend towards a significant relationship was noted for GI acute toxicity (p = 0.05).
Conclusions
All assessed irradiation methods do not lead to severe acute adverse effects. Importantly, patients treated with IGRT and IMRT had only minor GI toxicity.
Keywords: prostate cancer, radiotherapy, acute toxicity
INTRODUCTION
In prostate cancer management, increasingly sophisticated radiation techniques are being used. Recent years brought many advancements in external beam radiotherapy. Since the constructing of the megavoltage linear accelerator and the creation of the Cobalt-60 unit, we have observed a continuous improvement of irradiation technology, and as a consequence different techniques have been developed.
After the invention of computed tomography (CT), new possibilities of imaging of internal structures emerged. That enabled the first prostate radiation treatment planning and creation of 3-dimensional conformal radiotherapy. Conformal 3D radiation therapy enables the creation of a 3-dimensional picture of the tumor in order to target the tumor accurately and give it the highest possible dose of radiation while sparing normal tissue as much as possible [1]. Visualization of soft tissues surrounding the prostate, especially bladder and rectum, enables the limitation of irradiation of these organs. The invention of conformal 3D radiotherapy was an impulse to create more precise methods.
Intensity-modulated radiation therapy (IMRT) was the next improvement of radiotherapy technique. Both IMRT and image-guided radiation therapy (IGRT) allow high radiation doses to be focused on the tumor while minimizing the dose to surrounding healthy tissue. Additional planning and safety checks are necessary due to their complexity. Computer systems, which are based on radiological imaging, optimize irradiation of the prostate [2]. IGRT consists of implantation of electromagnetic seeds into a prostate. Real-time movements of this organ are processed and radiation beams are modulated during treatment. This allows to further reduce the surrounding tissue margin to three millimeters, with a subsequent potential to decrease in bladder and rectum toxicity. The further desire of decreasing adverse reactions focused on hypofractionation. Lowering of total doses of irradiation was possible due to invention of stereotactic body radiation therapy (SBRT). It combines image guidance with real-time tracking and using technique of volume-modulated arc (VMAT). In contrast to previously described step-and-shoot methods of radiotherapy, VMAT uses rotating gantry. As a result, the time of procedure is shorter. Furthermore, VMAT accurately shapes the radiation dose to the tumor [3].
The choice of the optimal treatment option for patients with prostate cancer aims at increasing effectiveness and lowering toxicity. The genitourinary (GU) and the digestive gastrointestinal (GI) tracts are particularly susceptible to damage during irradiation of a prostate because of their proximity [4]. The aim of the study is to assess short-term, acute radiation toxicity in prostate cancer patients irradiated using different techniques.
MATERIAL AND METHODS
Sixty patients irradiated between 2012 and 2016 in the University Hospital in Zielona Góra were analyzed. Patients underwent treatment with four different techniques of external beam radiotherapy ie.: A. conformal 3D – 11 patients, B. IMRT – 20, C. IGRT – 19 and D. VMAT – 10 respectively. Patients' age ranged from 46–85 years (median 70.5), prostate-specific antigen (PSA) concentration at the time of diagnosis were in the range of 3.54–154 ng/ml (median 15.9).
Tumor characteristics in our group revealed: T1c (n = 19), T2a (n = 1), T2b (2), T2c (n = 29), T3a (n = 3), T3b (n = 6), grade Gleason 5 (n = 4), Gleason 6 (n = 18), Gleason 7(3+4) (n = 15), Gleason 7(4+3) (n = 5), Gleason 8 (n =15), Gleason 9 (n = 3). Genitourinary (GU) and gastrointestinal (GI) acute toxicity (within 3-month follow-up) according to the EORTC /RTOG scale were evaluated. The scale from one to four was assigned to each patient. The study was approved by the hospital. Furthermore, all participants gave written consent to the Centre of Monitoring of Cancer Treatment. The parametric (ANOVA) and non-parametric methods (Pearson's chi-square) were used to assess the relationship between acute toxicity and irradiation method. The volume of the bladder and rectum covered by the 70Gy dose was also analyzed depending on the treatment technique used.
RESULTS
In our group of patients, all of the applied techniques of external beam radiotherapy were well tolerated. There was no acute Grade 3 and 4 toxicity reported in any presented method. Importantly, IMRT and IGRT did not lead to any Grade 2 acute toxicity of gastrointestinal system.
The adverse reaction of genitourinary system reached Grade 2 in 7 patients (11.67%), Grade 1 in 26 patients (43.33%) and Grade 0 in 27 patients (45%). Acute toxicity of gastrointestinal system presented Grade 2 in 4 patients (6.67%), Grade 1 in 24 patients (40%) and Grade 0 in 32 patients (53.33%).
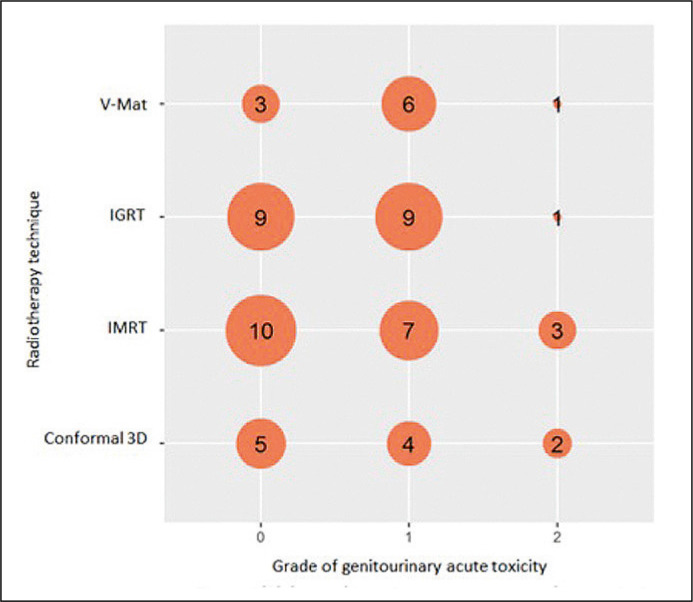
Figure 1 presents number of patients who suffered from certain grade of acute toxicity of genitourinary system. Each technique and corresponding grade is represented as a circle with a size depending on the number of patients that were described with this adverse reaction. We used Pearson's chi-square with a p-value of 0.8. Therefore, we did not find a statistical relation between genitourinary acute toxicity grade and the radiotherapy technique used.
Figure 1.
Grade of genitourinary acute toxicity depending on radiotherapy technique.
Pearson's chi-square; p-value = 0.8
V-Mat – volume-modulated arc therapy; IGRT – image-guided radiation therapy; IMRT – intensity-modulated radiation therapy; 3D-conformal – 3-dimensional conformal radiotherapy
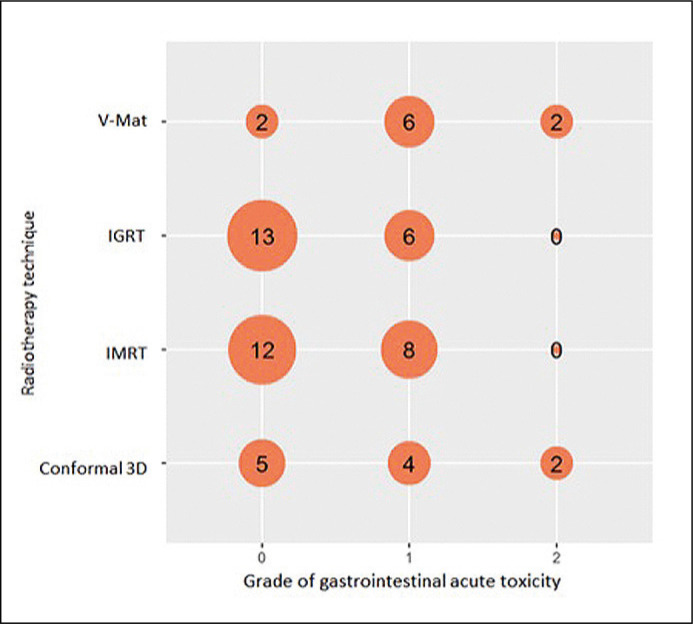
Figure 2 presents corresponding results in gastrointestinal system. P-value of Pearson's chi-square was 0.05. There was a trend towards a statistical relation between gastrointestinal acute toxicity grade and radiotherapy technique. IGRT and IMRT appeared to have a better toxicity profile and treatment tolerance in comparison to 3D-conformal radiotherapy and VMAT.
Figure 2.
Grade of gastrointestinal acute toxicity depending on radiotherapy technique.
Pearson's chi-square; p-value = 0.05
V-Mat – volume-modulated arc therapy; IGRT – image-guided radiation therapy, IMRT – intensity-modulated radiation therapy; 3D-conformal – 3-dimensional conformal radiotherapy
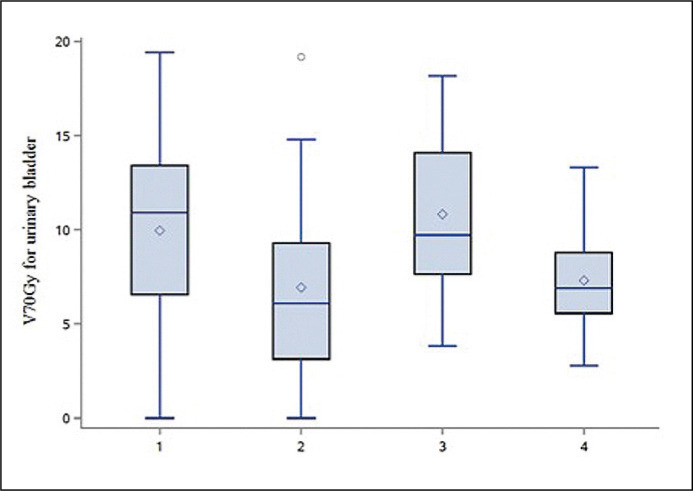
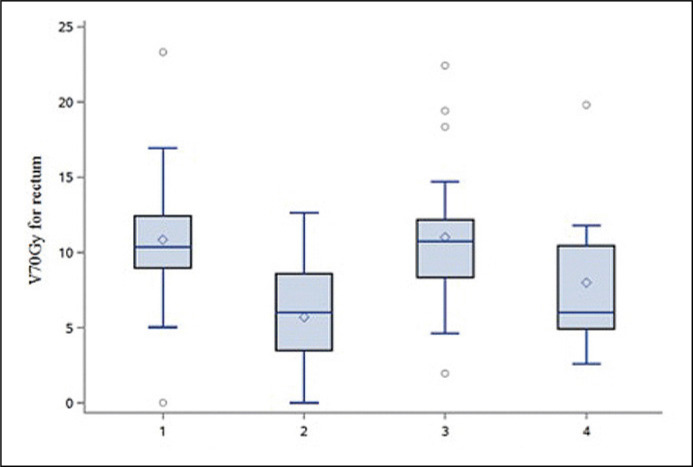
Furthermore, we analyzed the volume of the bladder and rectum covered by the 70Gy dose. On the Figure 3 and Figure 4 we presented those volumes, respectively for bladder and rectum. They depended on the treatment modality used. The results showed that IMRT and VMAT provided the opportunity to decrease the volume of irradiation of these organs.
Figure 3.
Distribution of the 70Gy dose of irradiation in the volume of urinary bladder depending on radiotherapy technique.
1 – 3-dimensional conformal radiotherapy; 2 – intensity-modulated radiation therapy; 3 – image-guided radiation therapy; 4 – volume-modulated arc therapy
Figure 4.
Distribution of the 70Gy dose of irradiation in the volume of rectum depending on radiotherapy technique.
Legend: 1 – 3-dimensional conformal radiotherapy, 2 – IMRT, 3 – IGRT, 4 – V-Mat
DISCUSSION
IMRT and VMAT remain the gold standard for definitive treatment of prostate cancer by external-beam radiation therapy [5]. Our results are in line with previous findings. Milecki et al. reported that 3D conformal radiotherapy is well tolerated. They examined 42 patients with localized and locally advanced prostate cancer. 80% of them experienced Grade 0 or 1 acute GU toxicity, such as urgency, nocturia or dysuria. The remaining group (20%) developed Grade 2 toxicity. Acute GI toxicity of Grade 0 or 1, such as rectal discomfort and mild diarrhea, was observed in 75% of patients while Grade 2 in 25% of them [6]. In our group, we reported Grade 2 acute toxicity in 18% (2/11), affecting both GU and as well GI. The remaining patients developed 0 or 1 Grade toxicity. Stankovic et al., described an influence of 3D conformal radiotherapy on lower GI system. They evaluated 94 patients with prostate cancer for acute toxicity and its predictive factors. 43.6% of them developed Grade 1 GI acute toxicity. There was a higher risk of this reactions when hemorrhoids the GI co-morbidities were present [7]. Chou et al., presented that 29% and 27% of patients developed Grade 1 and 2 acute GI toxicity while GU toxicity of that level was 40% and 33% respectively [8]. Wortel and colleagues compared 3D conformal radiotherapy and IGRT on a large group of patients (215 and 260 patients respectively). According to RTOG scale Grade 2 or higher acute GI toxicity occurred in 49% and 29% of patients in mentioned groups. GU toxicity was 48% and 38% respectively. The significant reduction of a risk of acute toxicity characterized IGRT in comparison to 3DCRT [9].
Fonteyne presented the report on acute toxicity after IMRT treatment in 230 patients. According to the results no Grade 3 or 4 acute GI toxicity was observed and Grade 2 in 11% of patients. Acute GU toxicity of Grade 3 appeared in 7% and Grade 2 in 41% of patients. Additionally, a simultaneous integrated boost to intraprostatic lesion did not have an influence on acute toxicity. Our results show similar tendency but better outcomes. GI toxicity occurs less often than GU toxicity. However, we did not reported any Grade 2 complications, probably because of treating only 20 patients with IMRT. There was also no Grade 3 GU toxicity and only 15% of patients developed Grade 2 GU toxicity [10].
Fang and colleagues described observation of 94 patients who underwent IMRT. 13.8% of them suffered from Grade 2 acute GI toxicity while 28.7% experienced that level of GU toxicity. Also no patient had Grade 3 acute GI and GU toxicity. They stated that hypertension increases the risk of acute GI toxicity and androgen-deprivation therapy (ADT), similarly to International Prostate Symptom Score (IPSS), increases acute GU toxicity [11].
De Meerleer et al., assessed the adverse effects of IMRT in a group 114 patients. According to RTOG scale they observed 39% and 27% of Grade 1 and 2 GI toxicity respectively. 34% of patients were free from side effects. Grade 3 GU toxicity was experienced by 7% and Grade 2 and 1 by 36% and 47% respectively. There were 10% of individuals that were free from GU toxicity [12].
Choong et al., assessed the toxicity of IGRT using fiducial markers. Acute GU toxicity of Grade 1 was observed in 62% and Grade 2 in 21% and GI toxicity in 29% and 11% respectively. Whereas Grade 3 was described in 1% of treated individuals [13].
Ishii et al., compared toxicity rates between whole-pelvic and prostate-only VMAT. No statistical difference was observed. Grade 2 GI toxicity was 10.1% and 6.7% while GU 12.6% and 10.5% respectively. Only an increased frequency of diarrhea in whole-pelvic VMAT was significant [14]. The above findings indicate that all of mentioned methods of radiotherapy are well tolerated. Grade 3 of acute toxicity appears rarely. In our study, irrespective of the irradiation technique used, neither Grade 3 nor 4 acute toxicity was observed. Generally, adverse reactions from genitourinary system are observed more frequently than from gastrointestinal system. The selection of the most optimal treatment method belongs to decision of the multidisciplinary team. Importantly, contrary to brachytherapy [15] external beam radiotherapy does not require anesthesia and it is not limited by prostate size.
The major limitation of our study is the relatively small number of patients analyzed, its retrospective nature and the fact that only (short-term) acute toxicity of radiotherapy was assessed. Although the described techniques are generally very well tolerated, the radiation therapy is time-consuming (generally lasts for seven to eight weeks). Furthermore, in contrast to surgery, patients are treated with hormonal therapy with its known side effects.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Bogers JA, van der Maazen RWM, Visser AG. Conformal Photon-Beam Radiotherapy of Prostate Carcinoma. Eur Urol. 2002;41:515–522. doi: 10.1016/s0302-2838(02)00017-9. [DOI] [PubMed] [Google Scholar]
- 2.Jereczek-Fossa B. A. Role of radiotherapy in the treatment of prostate carcinoma. Contemporary Oncology. 2003;7:176–182. [Google Scholar]
- 3.Quan EM, Li X, Li Y, et al. A comprehensive comparison of IMRT and VMAT plan quality for prostate cancer treatment. Int J Radiat Oncol Biol Phys. 2012;83:1169–1178. doi: 10.1016/j.ijrobp.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward MC, Tendulkar RD, Ciezki JP, Klein EA. Future Directions From Past Experience: A Century of Prostate Radiotherapy. Clin Genitourin Cancer. 2014;12:13–20. doi: 10.1016/j.clgc.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Ling CC, Yorke E, Fuks Z. From IMRT to IGRT: frontierland or neverland? Radiother Oncol J Eur Soc Ther Radiol Oncol. 2006;78:119–122. doi: 10.1016/j.radonc.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Milecki P, Stryczyńska G, Stachowski T, Kwias Z. Early toxicity of combined treatment in localised and locally advanced prostate cancer: hormone therapy with conformal radiotherapy. Urol Pol. 2002;55:48–52. [Google Scholar]
- 7.Stankovic V, Nikitovic M, Pekmezovic T, et al. Toxicity of the lower gastrointestinal tract and its predictive factors after 72Gy conventionally fractionated 3D conformal radiotherapy of localized prostate cancer. J BUON. 2016;21:1224–1232. [PubMed] [Google Scholar]
- 8.Chou RH, Wilder RB, et al. Acute toxicity of three-dimensional conformal radiotherapy in prostate cancer patients eligible for implant monotherapy. Int J Radiat Oncol Biol Phys. 2000;47:115–119. doi: 10.1016/s0360-3016(00)00422-3. [DOI] [PubMed] [Google Scholar]
- 9.Wortel RC, Incrocci L, Pos FJ, et al. Acute toxicity after image-guided intensity modulated radiation therapy compared to 3D conformal radiation therapy in prostate cancer patients. Int J Radiat Oncol Biol Phys. 2015;91:737–744. doi: 10.1016/j.ijrobp.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Fonteyne V, Villeirs G, Speleers B, et al. Intensity-Modulated Radiotherapy as Primary Therapy for Prostate Cancer: Report on Acute Toxicity After Dose Escalation With Simultaneous Integrated Boost to Intraprostatic Lesion. Int J Radiat Oncol Biol Phys. 2008;72:799–807. doi: 10.1016/j.ijrobp.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 11.Fang P, Mick R, Deville C, et al. A case-matched study of toxicity outcomes after proton therapy and intensity-modulated radiation therapy for prostate cancer. Cancer. 2015;121:1118–1127. doi: 10.1002/cncr.29148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Meerleer G, Vakaet L, Meersschout S, et al. Intensity-modulated radiotherapy as primary treatment for prostate cancer: Acute toxicity in 114 patients. Int J Radiat Oncol Biol Phys. 2004;60:777–787. doi: 10.1016/j.ijrobp.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Choong ES, Hruby G, Yang J, Kwong C, Patanjali N. 78Gy with Fiducial Marker Image--Guided Radiotherapy in Prostate Cancer: Single Center Analysis of 301 Patients. Asia Pac J Clin Oncol. 2017;13:e356–363. doi: 10.1111/ajco.12637. [DOI] [PubMed] [Google Scholar]
- 14.Ishii K, Ogino R, Hosokawa Y, et al. Comparison of dosimetric parameters and acute toxicity after whole-pelvic vs prostate-only volumetric-modulated arc therapy with daily image guidance for prostate cancer. Br J Radiol. 2016;89:20150930. doi: 10.1259/bjr.20150930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’hulst P, Mattelaer P, Darras J, Staelens L, Pottel H, Ponette D. Low-dose-rate brachytherapy as a minimally invasive curative treatment for localised prostate cancer has excellent oncological and functional outcomes: a retrospective analysis from a single centre. Cent European J Urol. 2018;71:270–275. doi: 10.5173/ceju.2018.1749. [DOI] [PMC free article] [PubMed] [Google Scholar]