Abstract
Introduction
The COVID-19 pandemic has brought great challenges to the management of urological patients. Like most surgical specialties, urology has shifted towards an emergency mentality. Currently, the beginning of the de-escalation phase of the pandemic has been observed, which will certainly pose new challenges to the urological community.
Material and methods
A non-systematic search was conducted through the Medline and Web of Science databases. The main keywords used in the search were: ‘COVID-19’, ‘SARS-CoV-2’, ‘urology’. The search included articles without time and language limitation.
Results
During the peak of the COVID-19 pandemic urological services had to focus on maintaining urgent-oncological and emergency-trauma procedures. First adapted recommendations were released at the end of March 2020. Primarily, they included information regarding the prioritization of surgical procedures. Currently, the beginning of the de-escalation phase in many countries has forced the necessity of establishing new degrees of priority for surgical interventions.
During the COVID-19 pandemic, cancellations and rescheduling significantly extend the waiting time for outpatient appointments and surgical procedures. A network of expert high-volume centres, at every level of referentiality, should guarantee the continuity of oncological care, supported with telemedicine systems.
The COVID-19 pandemic has caused a substantial decrease in clinical activity of urology residents. There also is huge potential for remote technology to address and improve education and training continuation in this field.
Conclusions
Urological care has been severely impaired by the COVID-19 pandemic. Urologists must adapt to the dynamically changing reality, prioritizing the safety and well-being of their patients and their clinic workforce.
Keywords: COVID-19, SARS-CoV-2, urology
INTRODUCTION
The COVID-19 pandemic, caused by the novel coronavirus (SARS-CoV-2), has brought great challenges to the management of patients, including those with urological diseases. It has resulted in the significant reallocation of health resources, as well as changes in routine clinical activities. Urology, like most surgical specialties, has shifted towards an emergency mentality, with many elective procedures having been cancelled [1]. Currently, the beginning of the de-escalation phase of the pandemic has been observed, which will certainly pose new challenges to the whole urological community [2].
The main aim of this article was to provide a brief summary of changes in urological practice, which have occurred during the COVID-19 pandemic, and their potential future implications.
Evidence acquisition
A non-systematic search was conducted through the Medline and Web of Science databases. The main keywords used in the search were: ‘COVID-19’, ‘SARS-CoV-2’, ‘urology’. Auto alerts in Medline were considered and the reference lists of original articles and review articles were searched for further eligible sources. The search included articles without time and language limitation, however, we focused primarily on the most recent publications.
Surgical procedures
During the peak of the COVID-19 pandemic in March and April 2020, the increasing number of new COVID-19 cases resulted in reduced availability of medical resources and shortages in medical personnel. Urology services had to focus predominantly on maintaining urgent-oncological and emergency-trauma procedures [3]. To that effect, the first recommendations from national and international urological associations/societies were released at the end of March 2020, and since then, several other guidelines and recommendations have been published [4–11]. Main European guidelines/recommendations with present date are shown in Figure 1. Primarily, they included information regarding the triage of urological patients and the prioritization of surgical procedures. It has to be emphasized that the majority of available recommendations were based on expert opinions [4–8]. Among scientific societies, only the European Association of Urology (EAU) provided evidence based guidelines, however, most findings had a low level of evidence (3/4) [9]. In adapted EAU guidelines, general recommendations applicable during the COVID-19 pandemic were presented. Additionally, recommendations on specific urological conditions were provided and based on four different levels of priority: low priority (clinical harm very unlikely if postponed for 6 months); intermediate priority (clinical harm possible if postponed for 3–4 months, but unlikely); high-priority (clinical harm very likely if postponed for >6 weeks); emergency (life threatening situations, likely to have presented via emergency department despite the current pandemic) [9]. A summary of high priority and emergency oncological surgeries is presented in Table 1.
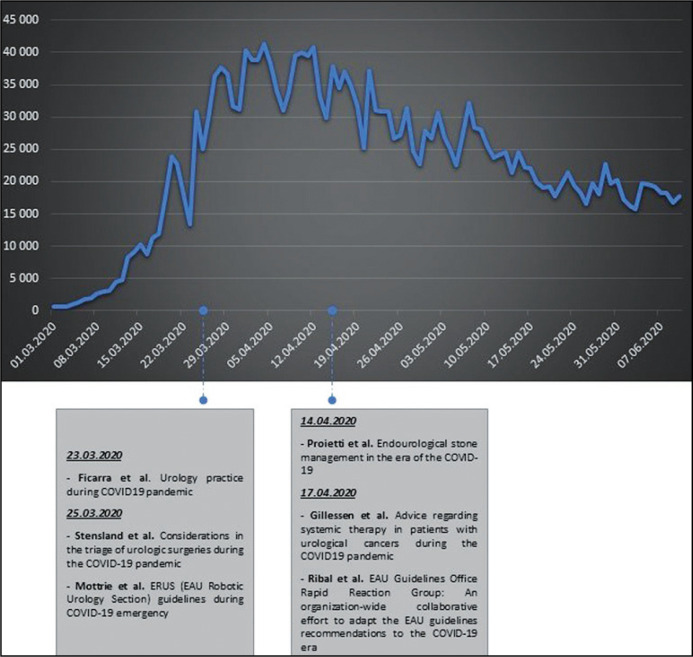
Figure 1.
Main European guidelines/recommendations regarding urological practice, released during the COVID-19 pandemic. The graph shows the number of daily cases of COVID-19 in Europe [4–9].
Table 1.
Summary of high priority and emergency oncological surgeries [9]
| Condition | Surgical procedure | Priority | |
|---|---|---|---|
| High-priority | Emergency | ||
| BC NMIBC | TURBT | In patients with bladder lesion and intermittent macroscopic haematuria or history of high-risk NMIBC | In patients with macroscopic haematuria with clot retention requiring bladder catheterisation |
| re-TURBT | In patients with visibly residual tumour after initial resection and large or multiple T1 high-grade at initial resection without muscle in the specimen | – | |
| MIBC | TURBT | In case of suspicion of an invasive tumour (identified on imaging) | – |
| RC | – | – | |
| UUTC | RNU | In patients with high-risk nonmetastatic UTUC | As a palliative treatment to symptomatic patients (eg. haematuria – clots) with resectable locally advanced tumours in patients with muscle – invasive UTUC |
| PCa | RP | In locally advanced PCa (including cN1) | – |
| RCC | Nephrectomy | In clinically advanced RCC cT2b-4, cN0-cN1 cM0 | – |
| TC | Orchidectomy | – | In all patients with suspicion of TC (pathological examination) |
BC – bladder cancer; NMIBC – non-muscle invasive bladder cancer; MIBC – muscle-invasive bladder cancer; TURBT – transurethral resection of bladder tumour; re-TURBT – restaging transurethral resection of bladder tumour; RC – radical cystectomy; UUTC – upper urinary tract carcinoma; RNU – radical nephroureterectomy; PCa – prostate cancer; RP – radical prostatectomy; RCC – renal cell carcinoma; TC – testicular cancer
Although a large consensus among various urological associations/societies regarding the prioritization of urological procedures exists, some differences are also present. Generally, the differences concern delays in some oncological conditions (i.e. priority of radical cystectomy), which is primarily related to various sociodemographic and healthcare system factors, as individual countries are at different stages of the pandemic [12]. Notably, available guidelines do not include modifications for a prolongation of the crisis [12]. Currently, the beginning of the de-escalation phase in many countries has forced the necessity of establishing a new degree of priority in surgical interventions. Most benign urological conditions can also be time-sensitive and can worsen over time, deeply affecting patients’ quality of life.
Until a vaccine for COVID-19 is developed, maintenance of a steady state of low-level transmission is crucial. Medical professionals working in the urological department are continuously at an elevated risk of a COVID-19 infection, thus they should adopt sufficient protection strategies. In compliance with national and international urologic associations/societies, it seems rational to continue the systematic use of high quality personal protective equipment (PPE), especially when COVID-19 is suspected (clinically or based on epidemiological interview) [3]. Testing of elective patients is highly recommended whenever possible within 48 h prior to surgery in an outpatient clinic setting, if the resources are available. The number of personnel attending the operating room during urgent urological surgery should be limited [9]. Whether SARS-CoV-2 can be transmitted by aerosols remains controversial. Thus, reducing the amount of surgical smoke and aerosol generated is reasonable as viruses like HIV, HCV, and papillomavirus, have been detected in surgical smoke in previous studies. Consequently, it is recommended to use the lowest intra-abdominal pressure during laparoscopic procedures in order to minimize the risk of aerosol infection [9, 13]. Although there is no proven evidence on the possibility of SARS-CoV-2 transmission via urine, endoscopic procedures should be performed with caution and full PPE protection. Evacuation of irrigation fluid during endourological procedures should be collected through a closed system [9].
Surgical and outpatient waiting time
Long waiting lists for outpatient appointments and surgical procedures have been a problematic issue already before the COVID-19 pandemic. During the COVID-19 pandemic common cancellations and rescheduling significantly extends this process [14]. In Italy, the European country with the highest number of confirmed COVID-19 cases, the observed decrease in urological oncological and non-oncological surgical activity was 35.9% and 89%, respectively [15]. The reorganization of surgical procedures has promoted the onset of a novel factor influencing the attempt to normalize surgical planning, namely the fear to contract COVID-19. For this reason, many patients failed and still fail to attend scheduled meetings and admissions. With increasing waiting or delay times, patients (especially oncological) may present with more advanced disease, which is associated with the implementation of more complex and harmful surgical procedures [14]. A network of expert high-volume centres, at every level of referentiality, should guarantee the continuity of oncological care in an appropriate way, ensuring the availability of hospital beds and timely management of new patients.
To ensure basic urological care and reduce the potentially avoidable treatment delays in the COVID-19 de-escalation scenario, telemedicine and telehealth systems seem to currently be a very encouraging option [16]. Telemedicine optimizes the safety of both the patients and medical professionals. The benefits for telemedicine in urology are continuing urological outpatient follow-up, providing recommendations and prescriptions, and the triage of patients who will need urgent procedures [14, 16]. Although many of the emergency provisions enacted during the crisis were temporary, many urological associations/societies supported the use of telemedicine in the upcoming months as a useful strategy to optimize resources in various contexts (including e.g. first clinical assessments, multidisciplinary meetings, control visits). Implementation of a remote consultation system and multidisciplinary team meetings can offer optimum therapeutic outcome [14, 16].
Education and residency training
The COVID-19 pandemic has caused a substantial decrease in assistance and academic activities in most medical residences, affecting urological residents too. The deprivation and difficulties in training were commonly reported in many countries [17, 18, 19]. The loss of clinical routine and daily activities, the cancellation of external internships, exams and numerous events, such as congresses, has impacted negatively on the annual planning for the specialization. Although the epidemic situation is currently changing, long-term action plans, given the possibility of multiple waves of infection, should not be neglected. There is a huge potential for remote technology, e-learning, webinars and online simulation courses to maintain, but also improve education and residency training. They might allow for the formation of new interactions and connections with people from all over the world, which might result in future internship opportunities and scientific collaboration.
CONCLUSIONS
Urological care has been severely impaired by the COVID-19 pandemic. Urologists must adapt to the dynamically changing reality, prioritizing the safety and well-being of their patients and their clinical workforce. During the de-escalation phase we need to establish a new degree of priority in surgical interventions. Telemedicine and virtual communication might offer great opportunity and value in the future for everyday reorganization of the whole diagnostic and therapeutic pathway of care, as well as improve medical education.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
FINANCIAL DISCLOSURE
None of the contributing authors have any conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
References
- 1.Puliatti S, Eissa A, Eissa R, et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int. 2020;125:E7–E14. doi: 10.1111/bju.15071. [DOI] [PubMed] [Google Scholar]
- 2.López-Fando L. De-escalation urology measures. COVID-19 pandemia stepwise recommendations. Arch Espl Urol. 2020;73:325–327. [PubMed] [Google Scholar]
- 3.Kunz Y, Horninger W, Pinggera GM. Are urologists in trouble by SARS-CoV-2? Reflexions and recommendations for specific interventions. BJU Int. 2020 doi: 10.1111/bju.15141. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. 2020;72:369–375. doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 5.Stensland KD, Morgan TM, Moinzadeh A, et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur Urol. 2020;77:663–666. doi: 10.1016/j.eururo.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mottrie A. ERUS (EAU Robotic Urology Section) guidelines during COVID-19 emergency. https://uroweb.org/wp-content/uploads/ERUS-guidelines-for-COVID-def.pdf.
- 7.Proietti S, Gaboardi F, Giusti G. Endourological Stone Management in the Era of the COVID-19 [published online ahead of print, 2020 Apr 14] Eur Urol. 2020;78:131–133. doi: 10.1016/j.eururo.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillessen S, Powles T. Advice Regarding Systemic Therapy in Patients with Urological Cancers During the COVID-19 Pandemic. Eur Urol. 2020;77:667–668. doi: 10.1016/j.eururo.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ribal MJ, Cornford P, Briganti A, et al. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation-wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur Urol. 2020;78:21–28. doi: 10.1016/j.eururo.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.USANZ Guidelines for urological prioritisation during COVID-19.
- 11.Goldman HB, Haber GP. Recommendations for Tiered Stratification of Urological Surgery Urgency in the COVID-19 Era. J Urol. 2020;204:11–13. doi: 10.1097/JU.0000000000001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heldwein FL, Loeb S, Wroclawski ML, et al. A Systematic Review on Guidelines and Recommendations for Urology Standard of Care During the COVID-19 Pandemic. Eur Urol Focus. 2020 doi: 10.1016/j.euf.2020.05.020. S2405-4569(20)30155-3 [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zampolli HC, Rodriguez AR. Laparoscopic and Robotic Urology Surgery during Global Pandemic COVID19. Int Braz J Urol. 2020;46:10. doi: 10.1590/S1677-5538.IBJU.2020.S113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hughes T, Ho HC, Shariat SF, Somani BK. Where do urologists stand in the era of novel coronavirus-2019 disease. Curr Opin Urol. 2020;30:610–616. doi: 10.1097/MOU.0000000000000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocco B, Sighinolfi MC, Sandri M, et al. The dramatic COVID-19 outbreak in italy is responsible of a huge drop in urological surgical activity: A multicenter observational study. BJU Int. 2020 doi: 10.1111/bju.15149. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGinley MP, Ontaneda D, Wang Z, et al. Teleneurology as a Solution for Outpatient Care During the COVID-19 Pandemic. Telemed J E Health. 2020:10. doi: 10.1089/tmj.2020.0137. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seguí-Moya E, González-Padilla DA, Ortega-Polledo LE, et al. Impact of COVID-19 in Spanish urology residents: Recommendations and perspective. Arch Esp Urol. 2020;73:471–478. [PubMed] [Google Scholar]
- 18.Fero KE, Weinberger JM, Lerman S, Bergman J. Perceived Impact of Urologic Surgery Training Program Modifications due to COVID-19 in the United States. Urology. 2020 doi: 10.1016/j.urology.2020.05.051. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pang KH, Carrion DM, Rivas JG, et al. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur Urol. 2020;78:6–8. doi: 10.1016/j.eururo.2020.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]