Abstract
Introduction
In 2004, Patricia Skilling developed a new squatting-based pelvic floor rehabilitation method based on strengthening the three reflex pelvic muscles and ligaments hypothesized to control the closure and micturition reflexes. We adapted these methods to test our hypothesis that day/night enuresis was due to the inability of these muscles/ligaments to control an inappropriately activated micturition reflex.
Material and methods
The trial commenced as a randomized control trial to be conducted over 4 months, but was converted to a prospective trial at 4 weeks by order of the Ethics Committee. A total of 48 children, 7.6 ±2.5 years, 34 females, 14 males, had strictly supervised exercises twice daily, 10 squats, 10 bridge, fitball exercises involving proprioception exercises with surface perineal electromyogram (EMG) once a week.
Eligibility criteria were daytime urine leakage plus night-time bedwetting. Exclusion criterion was refusal to sign consent forms. Assessment was done by intention to treat. The criterion for cure was complete dryness.
Results
At 1st review (4 weeks) 12/24 in the treatment group reported total cure of wetting; 41/48 children (86%) were cured of both daytime/nighttime enuresis (p <0.001) at 4 months. There were no adverse events. Secondary outcomes were concomitant cure of constipation, fecal incontinence, urinary retention as predicted by the underlying integral theory of incontinence.
Conclusions
We believe our methods accelerated normal childhood strengthening of muscles/ligaments which control inappropriate activation of the micturition reflex which we hypothesize is the basis for daytime/nighttime enuresis. This is a simple treatment, needs diligent application and validation by others.
Keywords: bedwetting, daytime/nighttime enuresis, urinary retention, constipation, fecal incontinence
INTRODUCTION
Nocturnal enuresis or ‘bedwetting’ syndrome represents an important percentage of the daily consultation of the pediatrician/pediatric urologist. An estimated 15–20% of children at 5 years of age wet the bed [1]. Little is known about the pathophysiology or how to treat it [1], other than it may be a genetic and heterogeneous disorder [2, 3, 4]. Different specialties consider the topic from their own viewpoint, particularly psychologists and psychiatrists who see the problem as a behaviour disorder.
The Standardization Committee of the International Society for Pediatric Continence [5] specifically avoided pathogenesis and treatment in its 2016 publication. The committee separated day and night incontinence thus: “Intermittent incontinence that occurs while awake is termed daytime incontinence. When intermittent incontinence occurs exclusively during sleeping periods, it is termed enuresis”; and “Symptoms are classified according to their relation to the storage and/or voiding phase of bladder function, but terminology used for lower urinary tract (LUT) symptoms will focus on descriptive rather than quantitative language.”
Another vision and the basis of this paper, is the 1990 Integral Theory of Female Urinary Incontinence which states that bladder incontinence is a consequence of lax suspensory ligaments due to collagen changes therein [6]; symptom control is by three involuntary directional muscle forces which act against pubourethral and uterosacral/cardinal ligaments (CL/USL) to close urethral and anal tubes, Figure 1, Video 1; to open them for micturition by selective relaxation of a forward muscle, (arrow, Figure 2), and control of the micturition reflex by a central and peripheral neurological feedback system [7], Figure 2. In this context, ‘overactive bladder’ (OAB) is mainly an uncontrolled activation of the micturition reflex [8] expressed as urge incontinence during the day and nocturia at night. If ligaments are loose, the directional muscles which contract against them weaken; the muscles can no longer stretch the organs sufficiently to support the hydrostatic pressure of the urine (and feces) acting on the stretch receptors ‘N’, Figure 2; ‘N’ fire off afferents to the cortex at a lower bladder volume; if central control of the afferents (white arrow, Figure 2) cannot stem the afferent flow, the micturition or defecation reflexes are activated and the adult (and child) perceives this as an urge to empty the bladder (or bowel) during the day; at night, nocturia. A fundamental aspect of pelvic symptoms is the ‘iceberg phenomenon’ [9] where there is one main presenting symptom, in this work, nocturnal enuresis; the other symptoms such as daytime wetting, constipation, bladder emptying problems are ‘below the surface’ and have to be specifically sought out by direct questioning.
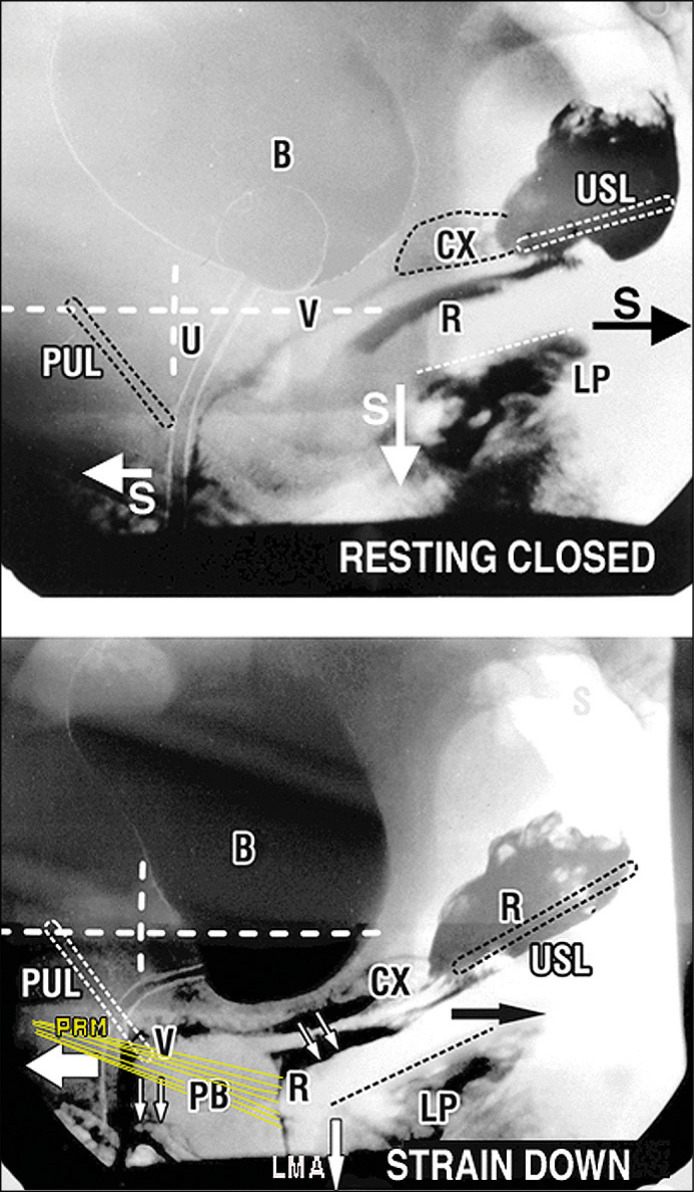
Figure 1.
Three directional muscle actions pull against pubourethral (PUL) and uterosacral (USL) suspensory ligaments. Broken lines represent bony vertical and horizontal co-ordinates . Radioactive dye has been inserted into the bladder ‘B’, vagina ‘V’, rectum ‘R’ and levator plate ‘LP’.
Upper xray image. Three slow twitch muscle forces ‘S’ maintain continence.
Lower xray image Urethral closure On straining, three fast twitch muscles pull forwards and backwards against the puborethral ligaments ‘PUL’ (arrows) and downwards against the uterosacral ligaments ‘USL’ (downward arrow). The downward vector ‘LMA’ pulls down the anterior border of LP to ‘kink’ the urethra at bladder neck.
Anorectal closure PRM contracts forwards. The backward vector LP stretches the rectum ‘R’ back to tension it; the downward vector ‘LMA’rotates ‘R’ to close the anorectal angle. Forward vector = m.pubococcygeus; backward vector = m.levator plate ‘LP’; downward vector = m. conjoint longitudinal muscle of the anus ‘LMA’.
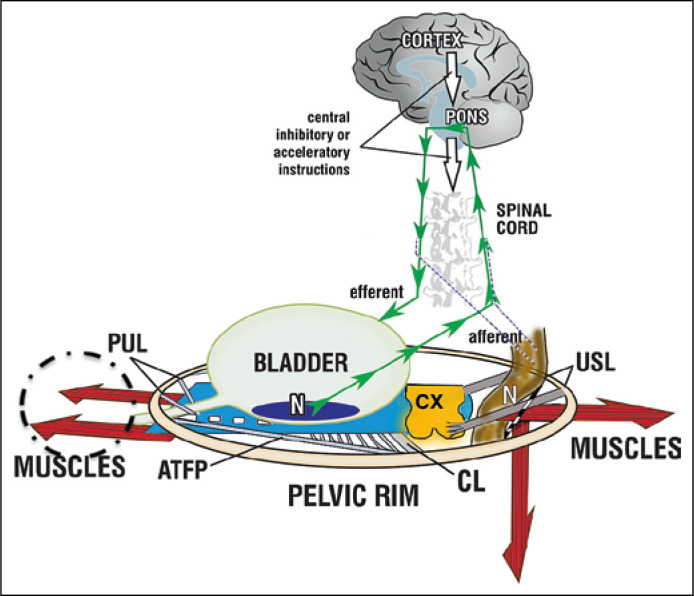
Figure 2.
Binary control of bladder & bowel. Schematic 3D sagittal view. System in normal closed mode. Like a trampoline, the organs are stretched and balanced by 3 opposite muscle forces (red arrows), contracting against PUL (pubourethral ligaments) and USL (uterosacral ligaments). Afferent impulses (small green arrows) originating from stretch receptors ‘N’ travel to the cortex. They are routinely reflexly suppressed cortically (white arrows). When required, the cortex activates the defecation and micturition reflexes for evacuation: the forward muscles relax, pubococcygeus for urethra (broken circle), puborectalis for anus (not shown); this allows the posterior muscles (arrows) to unrestrictedly open out the posterior wall of anus and urethra (broken white lines) just prior to bladder/ rectal evacuation by smooth muscles contraction (spasm). If PUL or USL are loose, the muscles contracting against them (red arrows) weaken. Urethra/anus cannot be closed (incontinence), opened (emptying problems) or organs stretched to support ‘N’, (‘urge incontinence).
CX – cervix; CL – cardinal ligament; ATFP – arcus tendineus fascia pelvis
Proofs of the theory to date have been largely surgical: observation of symptom fate following ligament repair. Examples: cure of stress urinary incontinence (SUI), by the midurethral sling [10] with a tape placed in the position of the pubourethral ligament (estimated 10,000,000 operations to date). Not so well known is cure of organ prolapse and pelvic symptoms by tapes placed in the cardinal and uterosacral ligaments [11–16]. Even less well known are Patricia Skilling’s squatting-based pelvic floor exercises (PFE) in a premenopausal adult population [17, 18]. These work by strengthening the 3 involuntary pelvic muscles and the ligaments they contract against; the PFEs achieved a greater than 50% improvement in urge, nocturia, stress urinary incontinence and bowel symptoms in 70–90% of premenopausal women [17, 18]. Some women were nulliparous and had nocturnal enuresis as children, suggesting, perhaps, a congenital etiology. It was this part of her results which inspired this study in children.
Our hypotheses
Nocturnal enuresis and daytime incontinence in children may be caused by congenital muscle/ligament weakness destabilizing control of the micturition reflex.
Nocturnal enuresis is the adult equivalent of nocturia, except that the children do not wake.
As children are in a collagen creation phase for their tissues, ligaments and bones, the squatting-based exercises would strengthen the 3 directional forces which open and close bladder and bowel, Figures 1&2, and create new collagen to reinforce pubourethral and cardinal/uterosacral ligaments to reverse the urinary and fecal dysfunctions as per the pelvic floor exercise studies [17, 18].
The primary aim was to test these hypotheses with a randomized control trial (RCT) with squatting-based exercises against placebo. The secondary aim was to test the ‘iceberg’ concept of co-occurrence of other bladder and bowel symptoms such as constipation, fecal incontinence, emptying symptoms by monitoring their fate.
Material and methods
The study was carried out at the Integral Institute of Pelvic Floor in the city of Córdoba – Argentina, after approval of the work plan by the Ethics Committee of CEIS Oulton, Instituto Oulton, affiliation, Faculty of Medical Sciences of the UNC under the supervision of the first author AFG. IRB approval by the ACTA B-345 Registro Provincial De Investigacion En Salud.
Initial study design. A randomized control study with two arms, squatting-based pelvic floor exercises and a placebo arm. The study was performed at the Instituto Integral de Piso Pélvico Cordoba Argentina.
Declaration of Helsinki and CONSORT guidelines were followed. Recruitment period: 26.8.2019 to 26.12.2019.
Participants. Forty-eight children were entered into the study by their parents.
Inclusion criteria were male and female patients from 6 to 10 years of age with night-time enuresis (bed-wetting) plus daytime wetting. Written informed consent from parents for the patients included in the study including permission to publish the results.
Exclusion criteria were patients whose parents did not accept informed consent.
The presenting symptom in all 48 children was nocturnal enuresis. Other symptoms recorded were daytime wetness, constipation, consistency and frequency of stools (Bristol classification), urinary tract infection, urge symptoms during the day, bladder emptying problems. Also recorded were age; residence (urban/rural); family situation: couples with stable union or unstable unions; change of residency in the previous 6 months; socio-economic level: low, medium, high; retention and urgency: whether the child was undergoing perineal maneuvers to retain urine and if urine was urgent to urinate; medication: none, past treatment with desmopressin and / or imipramine. No medication was administered during the study, except antibiotics if urinary infection was detected.
Urinary infection was diagnosed with positive urine culture to determine causal germ and treatment.
Constipation was defined as periods of 2 or more days without evacuation, as well as quality of the stools on the (hard or soft) Bristol scale.
Bladder emptying symptoms were confirmed by urine flowmetry and simultaneous computerized urine volume per second, duration of urination and activity of perineal floor with EMG perineal contact electrodes connected to an electromyograph (Medware®) brand with Ecud XP 5.0® and Ace XP 5.0® software.
The 3rd exercise, kinesiotherapy was carried out in the laboratory, the objective being for the child to identify the muscles that contract during exercises.
Psychological evaluation was performed if considered relevant. It provided information about the different profiles of children and their families to achieve a better approach to each patient. The nutritionist’s analysis delved into the hygienic-dietary aspects necessary to contribute to the improvement of constipation.
Randomization and masking. All 48 children in the study had daytime and nightly bedwetting (Table 1). Details were taken by a nurse who explained there was a new treatment and asked if they would participate in a trial which was explained. On agreement a consent form was signed. Meanwhile, 24 printed copies of each treatment were randomly placed into sealed opaque envelopes gathered into a box and shuffled thoroughly by a 2nd (blinded) person. The box was taken to the outpatient clinic. As each child entered the trial, two envelopes were taken from the box and placed on the desk. One envelope was chosen by the parent and the child was assigned to the trial arm indicated in the envelope. The next child was assigned according to the remaining envelope and so on. Care was taken so every step of the trial, randomization, intervention and assessment, was carried out by a different person, each person blinded from the other.
Table 1.
Questionnaire and results in the different moments in which the study was carried out (% in brackets)
| Questions | Entry | 2° week | 1° month | 4° month |
|---|---|---|---|---|
| Voiding daytime | 3.12 ±0.9 | 6.06 ±1.3 | 6.78 ±1.1 | 6.7 ±1.1 |
| Bedwetting days per week Yes |
6,44 ±1 48 (100) |
3.06 ±1.6 24 (50) |
0.98 ±1.6 7 (14.5) |
0.38 ±1 7 (14) |
| Daytime leak days per week Sometimes |
7.22 ±2.9 | 2.28 ±1.6 12 (25) |
0.64 ±1.2 12 (25) |
0.36 ±1.2 0 (0) |
| Fecal soiling number of patients | 9 (19) | 0 (0) | ||
| Bladder emptying difficulty number of patients Yes Post-void residual |
15 (31) 15 (31) |
0 (0) 0 (0) |
||
| Urge number of patients Yes No |
46 (98) 2 (2) |
32 (68) 16 (32) |
6 (12) 42 (88) |
4 (8) 44 (92) |
| Squatting exercises total number of patients completed Yes No |
0 (0) 48 (100) |
46 (96) 2 (4) |
46 (96) 2 (4) |
48 (96) 2 (4) |
| Number of defecations by a week | 4.34 ±1.9 | 5.82 ±1.1 | 6.34 ±0.9 | 6.44 ±0.8 |
| Characteristics of stools – Bristol Scale Soft Hard |
15 (30) 33 (70) |
25 (52) 23 (47.9) |
40 (80) 8 (20) |
46 (92) 2 (8) |
Treatment arm protocol: involved 3 types of exercises. The parents were directly instructed how to do the exercises at the clinic and were also given explanatory videos.
Ten squats morning and evening at home.
Ten bridge exercises morning and evening at home.
Fitball exercises involving pelvic anteversion and retroversion once a week in the clinic laboratory which involved proprioception exercises with surface perineal EMG. The rationale for this was that surface EMG helped compliance of the children to the exercises. It improved the proprioception and they assumed it as something playful.
The placebo arm protocol: the children ran 50 meters in the morning and also at night.
Monitoring was with diaries.
Outcomes, Table 1
Forty-eight children were studied; 96% carried out 4 months of exercises and completed the follow-up. Two were lost to the study. There were no adverse events.
Primary outcomes (intention to treat)
A total of 41/48 children were cured of both daytime/night-time enuresis (p <0.001).
Criterion for cure was complete dryness at 4 months review.
Secondary outcomes
A total of 32 (68%) children with constipation 92% cured (P<0.001); 9 (19%) soiling (all cured), 6 females (12%) a history of urinary tract infection, 15 (31%) had bladder emptying difficulties confirmed by ‘staccato wave’ on fluometry and post-void residual urine (PVR). Cure was confirmed in all 15 by ultrasound (PVR).
Mean age was 7.6 ±2.5 years, 34 females and 14 males. The vast majority of these children were from urban areas (78%) and the family situation was stable in 96% of the children. These children, mostly, had a medium socio-economic level (64%), an 18% lower class and 18% upper class. Demographics had no influence on outcomes.
The presenting symptom in every case was bedwetting. All other symptoms were obtained by specific interrogation. The main symptomatic results are detailed in Table 1.
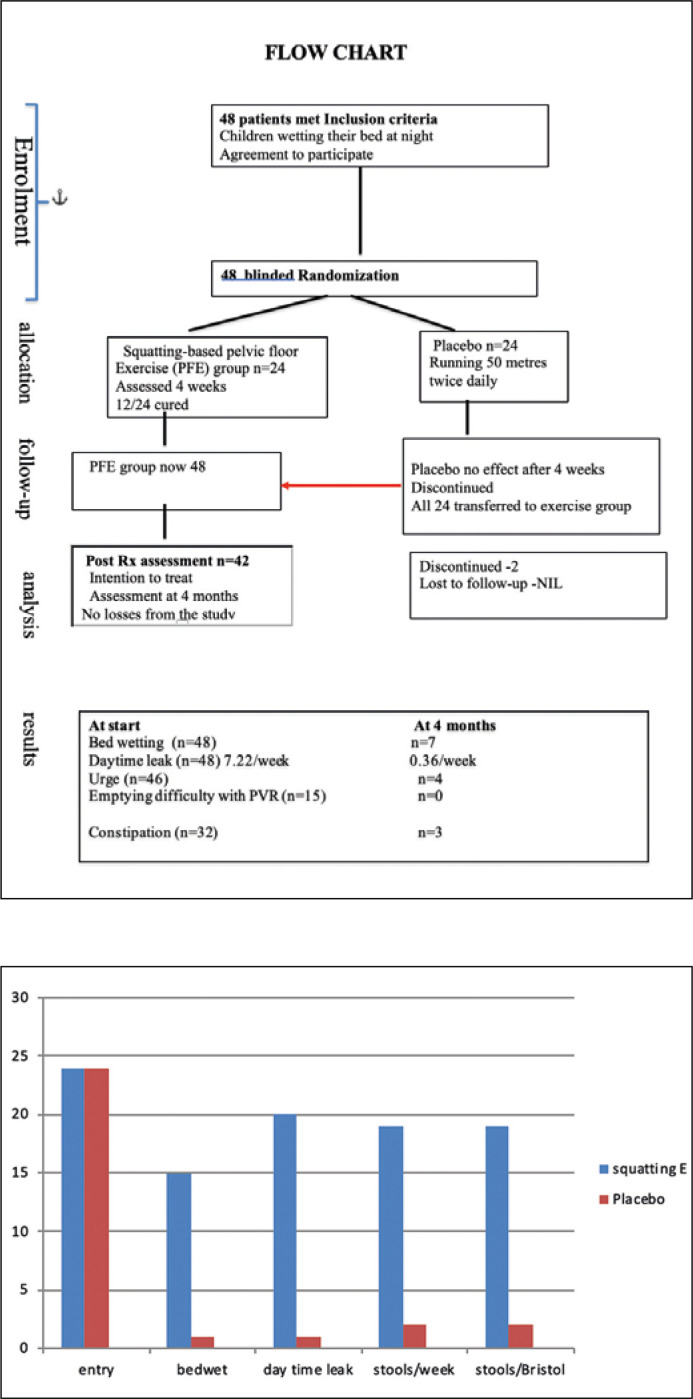
Both arms of the RCT results were assessed at 4 weeks by an external assessor whose opinion was validated by the parent of the child and entered into the clinical notes, stamped and dated (Figure 3). In the exercise group, 12/24 were entirely dry. In the control arm, there was no change. All children remained wet. At this point, the IRB committee ordered that the RCT be stopped, the placebo arm transferred to the exercise arm and the trial continued as a prospective trial. No child complained of pelvic pain and there was no stress urinary incontinence. Transperineal ultrasound did not show any abnormal perineal descent or any bladder neck funnelling.
Figure 3.
Graph of the first part of the trial. Symptom improvement at one month.
Treatment prior to the trial. Fourteen patients had some medication (desmopressin: 10, imipramine: 3, oxybutynin: 1), with no significant effect. 19 consulted with psychologists. Only some found some degree of impact on their self-esteem. There was no depression. There was no medication given.
10% of patients had urinary infections and 68% were considered constipated.
Gathering and assessment of the results
Each of the variables obtained upon admission (Table 1) were followed for a period of 4 months: at 2 weeks, 4 weeks and 4 months, each stage by a separate blinded assessor. At 4 months, the results were assessed again by a separate blinded assessor and validated in writing on the clinical notes by the parent with a signed signature and a dated hospital stamp. Analysis was separately carried out. We found a statistically significant difference (p <0.001), when comparing the number of urine samples per day at the beginning of the study, with those observed at 4 months of follow-up. The difference between study entry and after 2 weeks of treatment was also significant (p <0.001).
Wetting during the day was another variable studied. We found differences between the beginning of the study (p <0.001) and at two weeks; differences between the 2 weeks of the study and one month (p <0.001). There were no differences between the month of the study and the end (0.99).
Bedwetting at night: difference was significant with respect to the start parameters and the subsequent observations (p <0.001). Differences were found between the data obtained after 2 weeks of treatment and the month of treatment (p = 0.022) and between the month of treatment and follow-up after 4 months (0.003).
Evacuation habit: we observed that the number of depositions per week was increasing according to the progress of the treatment, there being significant differences between the beginning of the study and the first 2 weeks of the same (p <0.001), between the 2 weeks of the study and the month of the same (p <0.001) with no differences between the 1 and 4 months of follow-up (p = 0.19).
Consistency of the stool: we found that significantly (p <0.001), the feces became softer between the beginning and the 2 weeks of treatment and this stool softening continued during the study, observing differences between the 2 weeks of treatment and the month of treatment (p = 0.006) and between the month of treatment and 4 months of follow-up (p <0.001).
Statistics
The statistical analysis for the evaluation of patients with enuresis and its treatment was carried out with SAS software (SAS Institute, Inc., Cary, NC). The numerical variables were presented as means ± standard deviation and the continuous ones as percentages, the comparisons of the numerical variables were made with the student or Wilcoxon test, as appropriate and the nominal variables with chi-square or exact test of Fisher according to the characteristics of the population. The analysis of all the variables was done individually with simple and logistic regressions and jointly by means of multiple and logistic regressions. When the comparison was made in more than two groups, the analysis of variance (ANOVA) was used. Participants were included in primary analyses by intention to treat (n = 48).
Determination of the sample
It was obtained with an alpha of 0.05 and a beta of 0.30. The delta observed in previous studies was quite broad, which allowed us to obtain a power delete or power of 90% with the study of 48 patients.
DISCUSSION
Though started as an RCT, the transfer of the placebo arm to the experimental arm effectively altered this work to a one arm prospective trial. The muscle/ligament concepts driving this study are well outside the normal conceptual thinking and treatments of learned societies in the pediatric field [5]. The results were well beyond our expectations: 86% cure of nocturnal enuresis and daytime incontinence. We expected results similar to Patricia Skilling’s reports in adults, 50% improvement in 60–70% of children at most. The secondary outcomes, Table 1, demonstrated the importance of understanding that pelvic symptoms in the child occur in predictable groupings, and like the ‘iceberg’ concept [9], one symptom is pre-eminent. Other symptoms are ‘under the surface’ and need to be exposed by specific interrogation, as they were in our study protocol.
Analysis of hypothesis validity
Hypothesis 1 “Nocturnal enuresis and daytime incontinence in children may be caused by congenital ligament weakness destabilizing control of the micturition reflex.” It is clear from Figure 1 and Video 1 https://www.youtube.com/watch?v=3vJx2OvUYe0, that squatting -based exercises will strengthen the three directional muscle forces and the ligaments they contract against, pubourethral ‘PUL’ and uterosacral ‘USL’ ligaments. During micturition and defecation, the backward/downward posterior muscle forces (large arrows), Figure 2, contract against USL to pull open out the posterior wall of urethra and anorectum, broken lines. Opening the urethra Video 2 https://www.youtube.com/watch?v=eiF4G1mk6EA&feature=youtu.be or rectum Video 3 https://youtu.be/MS82AZoWn7U exponentially decreases the resistance to flow of urine and feces inversely by the 4th power of the tube radius (Poiseuille’s Law) [19–22]. This law is essential to understanding why children cannot close their emptying tubes (incontinence) or open them (constipation, bladder emptying difficulties): even a minor degree of muscle/ligament weakness is sufficient to cause bladder and bowel symptoms. Conversely, even a minor degree of strengthening will have an exponentially positive effect on the symptoms, as noted in our study.
The videos show the directional muscle movements of the muscles activated by the closure and evacuation reflexes.
Video 1. (Adult) 2D transperineal ultrasound showing the 3 directional movements activated by straining down. What to look for: involuntary forward movement acting against PUL position at midurethra; backward movement acting against PUL; downward angulation of the anterior border of the levator plate (white) against position of USL.
Video 2. Micturition (Adult) What to look for: involuntary backward movement acting against PUL; downward angulation of the anterior border of the levator plate against position of USL. ‘Spasm’ of detrusor throughout the emptying.
Video 3. Defecation (Adult) What to look for: downward angulation of the anterior border of the levator plate against position of USL exactly as occurs during micturition. Opening out of the anorectal angle; feces ‘sliding’ down the posterior rectal wall.
Hypothesis 2 “Nocturnal enuresis is the adult equivalent of nocturia, except that the children do not wake”. It was not possible to objectively test an activated micturition reflex in children while they were asleep. However, on the basis that an 86% cure of nocturnal enuresis by muscle/ligament strengthening gives a similar result to nocturia, cure rates achieved in adults by surgical and non-surgical ligament strengthening [17, 18], we felt the hypothesis was validated: strengthening the dynamic supports for the peripheral stretch receptors ‘N’, Figure 2. restores normality to the feedback control system to prevent inappropriate activation of the micturition reflex, expressed as daytime urge, nocturia, bedwetting.
Hypothesis 3 “Children are in a collagen creation phase for their tissues, ligaments and bones, the squatting-based exercises would strengthen the 3 directional forces which open and close bladder and bowel, Figures 1 and 2, and create new collagen to reinforce PUL and CL/USL ligaments to reverse the urinary and fecal dysfunction.” There is ample evidence in the literature of collagenotrophic activity during exercise for both muscles and connective tissue [23, 24]. Type I collagen is known to adapt to physical activity, and biomarkers of collagen turnover indicate that synthesis can be influenced by a single intense exercise bout [25]. Our findings were consistent with such evidence, but they did not prove hypothesis.
Strengths of the study. Its simplicity and virtually zero cost. If validated by others, it will change the management of nocturnal enuresis and other symptoms in children forever. It will also change the science away from the organ itself, to the muscles and ligaments which act coordinately to open and close the outlet tubes.
Weakness of the study. Data from a single study location. Stopping of the RCT after one month.
It seems likely that the limitation to the pathway to cure is collagenopoiesis and so it follows that these exercises must be diligently performed, preferably for life.
CONCLUSIONS
We believe our methods accelerated normal childhood strengthening of muscles/ligaments which control premature activation of the micturition reflex which we hypothesize is the basis for daytime/night-time enuresis. This is a simple treatment, but it needs validation by others.
Acknowledgments
We would like to thank Dr. Patricia Skilling for her assistance in adapting her adult pelvic floor protocols to needs of the children.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Moffat M. Nocturnal enuresis. Is there a rationale for treatment? Scan J Urol Nephol Suppl. 1994;163:55–67. [PubMed] [Google Scholar]
- 2.Hublin C, Kaprio J, Partinen M, Koskenvuo M. Nocturnal enuresis cohort. Sleep. 1998;21:579. doi: 10.1093/sleep/21.6.579. [DOI] [PubMed] [Google Scholar]
- 3.Bakwin H. The genetics of enuresis. In: Kolvin I, Mac Keith R.C, Meadow S.R, editors. Bladder Control and Enuresis. 1973. pp. 73–77. [Google Scholar]
- 4.Hjalmas K, Arnold T, Bower W, et al. Nocturnal enuresis: an international evidence-based management strategy. J Urol. 2004;171:2545–2561. doi: 10.1097/01.ju.0000111504.85822.b2. [DOI] [PubMed] [Google Scholar]
- 5.Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children's Continence Society. Neurourol Urodyn. 2016;35:471–448. doi: 10.1002/nau.22751. [DOI] [PubMed] [Google Scholar]
- 6.Petros PE, Ulmsten U. An Integral Theory of female urinary incontinence. Acta Obst Gynecolo Scand. 1990;69(Suppl 153):1–79. doi: 10.1111/j.1600-0412.1990.tb08027.x. [DOI] [PubMed] [Google Scholar]
- 7.Petros PE. Detrusor instability and low compliance may represent different levels of disturbance in peripheral feedback control of the micturition reflex. Neurourol Urodyn. 1999;18:81–91. doi: 10.1002/(sici)1520-6777(1999)18:2<81::aid-nau3>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Petros PE, Ulmsten U. Bladder instability in women: A premature activation of the micturition reflex. Neurourol Urodyn. 1993;12:235–239. doi: 10.1002/nau.1930120305. [DOI] [PubMed] [Google Scholar]
- 9.Goeschen K. Role of uterosacral ligaments in the causation and cure of chronic pelvic pain syndrome. Pelviperineology. 2015;34:2–20. [Google Scholar]
- 10.Ulmsten U, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol. 1995;29:75–82. doi: 10.3109/00365599509180543. [DOI] [PubMed] [Google Scholar]
- 11.Petros PE, Swash M. The Musculoelastic Theory of anorectal function and dysfunction. J Pelviperineology. 2008;27:89–121. [Google Scholar]
- 12.Liedl B, Inoue H, Sekiguchi Y, et al. Update of the Integral Theory and System for Management of Pelvic Floor Dysfunction in Females European J of Urology EURSUP-738. Eur Urol Suppl. 2018;17:100–108. [Google Scholar]
- 13.Wagenlehner F, Muller-Funogea l, Perletti G, et al. Vaginal apical prolapse repair using two different sling techniques improves chronic pelvic pain, urgency and nocturia - a multicentre study of 1420 patients. Pelviperineology. 2016;35:99–104. [Google Scholar]
- 14.Petros P, Lynch W, Bush M. Surgical repair of uterosacral/cardinal ligaments in the older female using the tissue Fixation system improves symptoms of obstructed micturition and residual urine. Pelviperineology. 2015;34:112–116. [Google Scholar]
- 15.Inoue H, Kohata Y, Sekiguchi Y, Kusaka T, Fukuda T, Monnma M. The TFS minisling restores major pelvic organ prolapse and symptoms in aged Japanese women by repairing damaged suspensory ligaments - 12-48 month data. Pelviperineology. 2015;34:79–83. [Google Scholar]
- 16.Liedl B, Goeschen K, Yassouridis A, et al. Cure of Underactive and Overactive Bladder Symptoms in Women by 1,671 Apical Sling Operations Gives Fresh Insights into Pathogenesis and Need for Definition Change. Urol Int. 2019;103:228–234. doi: 10.1159/000500329. [DOI] [PubMed] [Google Scholar]
- 17.Petros PE, Skilling PM. Pelvic floor rehabilitation according to the Integral Theory of Female Urinary Incontinence. First report. Eur J Obstet Gynecol Reprod Biol. 2001;94:264–269. doi: 10.1016/s0301-2115(00)00313-4. [DOI] [PubMed] [Google Scholar]
- 18.Skilling PM, Petros PE. Synergistic non-surgical management of pelvic floor dysfunction: second report. Int J Urogyne. 2004;15:106–110. doi: 10.1007/s00192-004-1122-3. [DOI] [PubMed] [Google Scholar]
- 19.Bush MB, Petros PEP, Barrett-Lennard BR. On the flow through the human urethra. Biomechanics. 1997;30(9):967–969. doi: 10.1016/s0021-9290(97)00050-x. [DOI] [PubMed] [Google Scholar]
- 20.Petros PE, Swash M. Directional muscle forces activate anorectal continence and defecation in the female. J Pelviperineology. 2008;27:94–97. [Google Scholar]
- 21.Bush M, Petros P, Swash M, Fernandez M, Gunnemann Defecation 2: Internal anorectal resistance is a critical factor in defecatory disorders. Tech Coloproctol. 2012;16:445–450. doi: 10.1007/s10151-012-0860-3. [DOI] [PubMed] [Google Scholar]
- 22.Petros PEP, Bush M. A Feedback Control System Explains Clinical and Urodynamic Bladder Instability in The Female. Pelviperineology. 2016;35:90–93. [Google Scholar]
- 23.Miller BF, Hansen M, Olesen JL, et al. Tendon collagen synthesis at rest and after exercise in women. J Appl Physiol. 2007;102:541–546. doi: 10.1152/japplphysiol.00797.2006. [DOI] [PubMed] [Google Scholar]
- 24.Miller BF, Olesen JL, Hansen M, et al. Coordinated collagen and muscle protein synthesis in human patella tendon and quadriceps muscle after Exercise. J Physiol. 2005;567:1021–1033. doi: 10.1113/jphysiol.2005.093690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langberg H, Skovgaard D, Asp S, et al. Time pattern of exercise-induced changes in type i collagen turnover after prolonged endurance exercise in humans. Calcif Tissue Int. 2000;67:41–44. doi: 10.1007/s00223001094. [DOI] [PubMed] [Google Scholar]