Abstract
Rotator cuff tears are among the most common orthopaedic conditions, with a very high social impact. A major concern is failure rates. To reduce these rates, recent years have seen increased attention to the biological augmentation of rotator cuff tears repairs, with a special focus on the application of mesenchymal stem cells (MSCs). Among the many tissues recognized as a source of MSCs, subacromial bursa recently has emerged. Another promising cell source was found to be the long head of the biceps tendon. Both those local MSC sources, unfortunately, are commonly considered discharge material. The purpose of this paper is to describe a simple yet fast arthroscopic technique of biological augmentation for rotator cuff repairs by mechanical harvesting and deployment of local MSCs sources, called LASCA (local autologous stem cells application), a feasible technique accessible to every shoulder surgeon and adaptable to many different techniques.
Rotator cuff tears are among the most common orthopaedic conditions, with a very high social impact. A major concern is a high rate of retear.1 To reduce these rates, recent years have seen increased attention to the biological augmentation of rotator cuff tears repairs, with a special focus on the application of mesenchymal stem cells (MSCs),2 multipotent cells able to differentiate along bony, chondral, and tendinous lineages. Among the many tissues recognized as a source of MSCs, subacromial bursa (SB) recently has emerged, revealing a superior potential in terms of engraftment to host tendon, survival, and proliferation.3,4 Moreover, it showed a superior chondrogenic potential over MSCs harvested from the enthesis and even compared with bone marrow–derived MSCs.5 Another promising cell source was characterized by Randelli et al. in 2013,1 the tendon-derived MSCs, by investigating samples from human supraspinatus and long head of the biceps tendon (LHBT). They confirmed that those tendons possess cells able to differentiate into osteoblasts, chondroblasts, and muscle cells, appearing potentially superior to bone marrow–derived MSCs as well. Those local MSC sources, unfortunately, are commonly considered discharge material: SB is always partially removed to increase visualization on the surgical field, whereas LHBT is more often tenotomized than repaired or conserved. The few published results on their possible application in rotator cuff tear repairs, however, suggest a possible positive effect at the repair site1, 2, 3, 4, 5 by providing a superior cell population able to enhance enthesis formation.
The purpose of this paper is to describe a simple yet fast arthroscopic technique of biological augmentation for rotator cuff repairs by mechanical harvesting and deployment of local MSCs sources, called LASCA (local autologous stem cells application).
Surgical Technique (With Video Illustration)
The LASCA technique is indicated for every reparable rotator cuff tear. It was ideated as an injection-like form of augmentation during a single-row arthroscopic repair with a triple-loaded anchor, but it can be applied to open repairs, transosseous repairs, and double rows, despite the preferred type of anchor or any other variable, such as the patient’s position, age at surgery, or revision surgeries. No vspecial preoperative imaging is therefore required, apart from what may be needed for the index diagnosis of each particular case.
Preparation
An ultrasound-guided brachial plexus block is performed by the anesthesiologist in a presurgical room. The patient is then moved into the surgical room and placed into a lateral decubitus position. Deep sedation in the patient is performed to maintain a lower blood pressure and better pain control. Sterile draping is performed as standard, and the arm is positioned at about 40° of abduction and 15° of anterior elevation for increased visualization, using a sterile skin traction.
While the first surgical steps of the arthroscopy are carried out, the scrub nurse will set up specific tools for LASCA: a dedicated “out-of-the-box” shaver’s filter and a “homemade” delivery system. The former is called GraftNet (Arthrex, Naples, FL); it is a suction-activated device designed to collect autologous tissue once it is connected to the shaver, which will be gathered in an easily accessed sterile filtered chamber (Fig 1). The latter is a construct made of a sterile syringe connected to a standard nasogastric tube, which will be cut short according to the length needed to reach the footprint by the lateral portal.
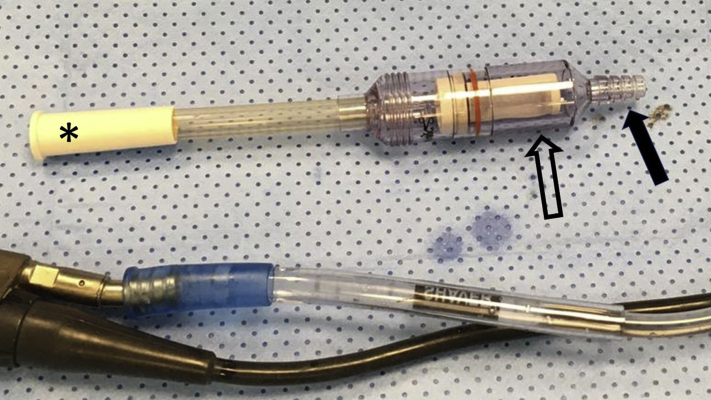
Fig 1.
The GraftNet (Arthrex, Naples, FL) used in the LASCA (local autologous stem cells application) technique. It is a filtering device to be connected to the shaver (by the white connector, shown by ∗) and to the suction mechanisms (by the transparent connector, shown by the filled arrow). It has a sterile chamber with a filtered basket of 3 cc of max volume to harvest the tissues debrided with the shaver (empty arrow).
Articular Phase: Portal Placement, Diagnostics, and LHBT Management
A standard posterior arthroscopic portal is produced first, which will serve as viewing portal. A diagnostic routine is performed and a working portal is produced laterally, trough the tendon tear, in an out-in fashion. A motorized shaver is introduced into the joint, the lesion is debrided down to healthy tendon, and the footprint is prepared. At this stage, the LHBT is evaluated for treatment: conservation, tenotomy, or tenodesis according to the intraoperative findings, patient’s characteristics and requests, and surgeon preferences.
Subacromial Phase: SB Harvesting, Cuff Repair, and LASCA
The second phase of the surgery is carried out in the subacromial space, viewing from the posterior portal and working from the lateral one. Before this phase starts, it is mandatory to have the GraftNet connected to the shaver. Soon as the subacromial space is accessed, in fact, a partial/total bursectomy is required to clear the surgical field and ensure an appropriate vision, and that tissue needs to be harvested for the LASCA to be applied. Once the device is filled completely (3 cc of harvested tissue) it can be removed, and the SB can be collected in a sterile fashion and put into a sterile cup with saline by the assistant surgeon (Fig 2). Harvested bursa will appear like a sort of gelatinous paste (Fig 3).
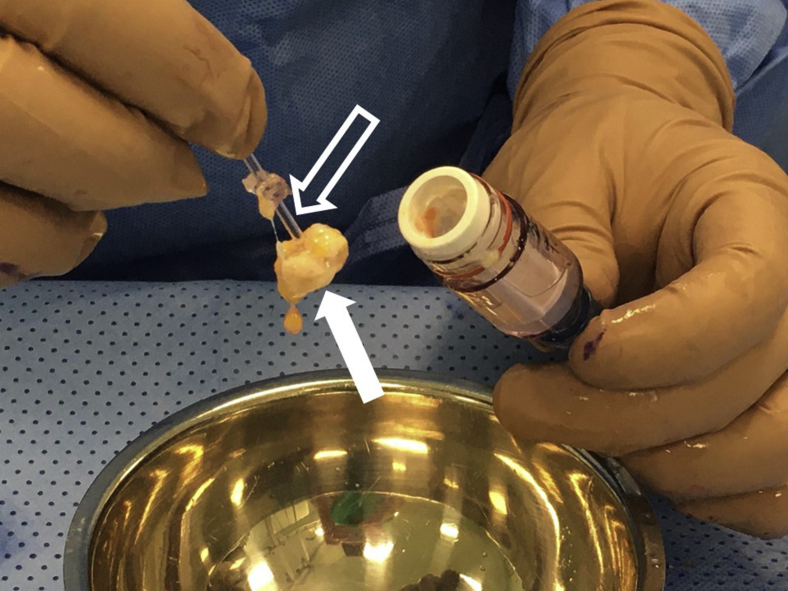
Fig 2.
Collection of the tissue. When the filter is completely filled with harvested subacromial bursa, it can be easily unscrewed and opened to collect the tissue. A little plastic piston (empty arrow) needs to be removed to take the tissue out (filled arrow).
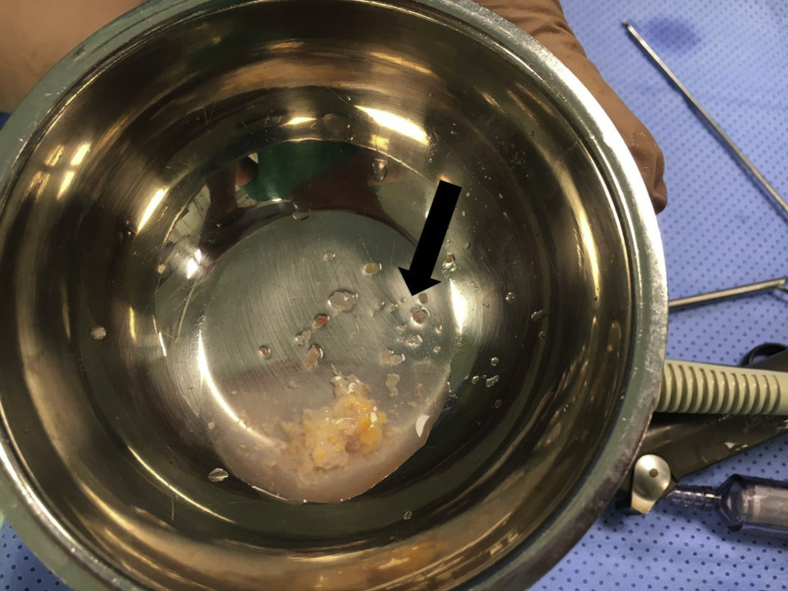
Fig 3.
Harvested subacromial bursa. Once harvested, the tissue has a paste-like appearance, not homogeneous, made of several chopped small pieces (filled arrow).
Meanwhile, the primary surgeon will carry on with the repair. The lesion is assessed with a grasper for reduction and repairability and a triple-loaded anchor is implanted. Each suture strand is then recovered and passed through the rotator cuff with a suture passer. In case of an LHBT soft-tissue tenodesis, the most anterior suture will be passed through the cuff by a shuttle suture previously positioned so to include the LHBT in the repair. Sutures can now be retrieved and secured with sliding knots, starting from the most posterior one, then securing the most anterior one, and lastly the middle suture, which will be not completely tied yet. At this point, the homemade delivery system, assembled beforehand, will be loaded with the harvested tissue and introduced in the subacromial space trough the lateral accessory portal (Fig 4). The free end of the nasogastric tube will be placed underneath the repaired tendon, and the augmentation will be performed by injecting the SB paste right before tying the last knot (Fig 5). Securing the middle suture at last will reduce the possibility for the paste to displace. Acromion will be assessed for acromioplasty, and the whole procedure will be over (Video 1).
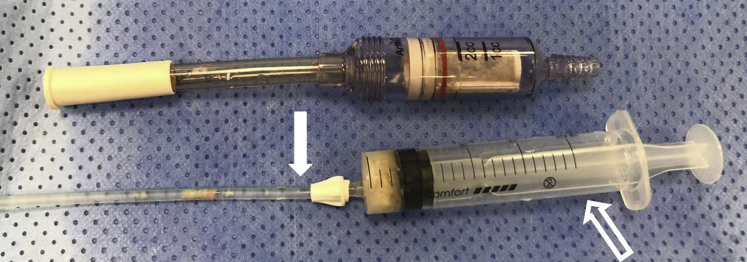
Fig 4.
Tools for LASCA. On the upper side, the GraftNet device is shown. Underneath, the home-made delivery systems created by connecting a sterile syringe (empty arrow) with a nasogastric tube cut at an appropriate length (filled arrow) is shown. Note that harvested tissue was loaded into the system, ready to be deployed at the repair site. (LASCA, local autologous stem cells application.)
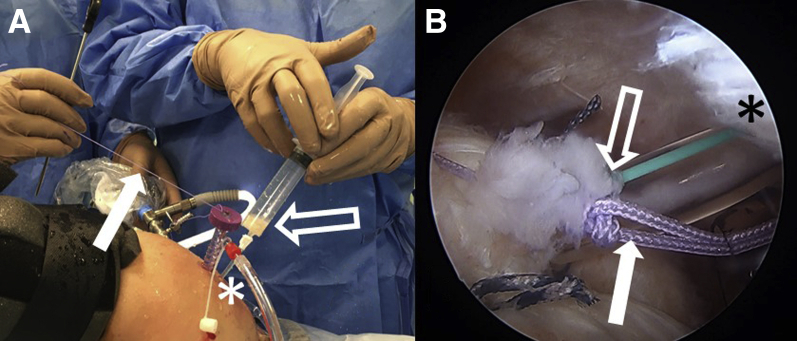
Fig 5.
Right shoulder, lateral decubitus. (A) Intraoperative external view. (B) Intraoperative arthroscopic view from the posterior portal. The harvested tissue is being deployed into the repair (empty arrow) through the accessory lateral portal used to implant the anchor (∗), whereas the “post-strand” or the middle suture is being pulled to tie the last knot (filled arrow).
Rehabilitation
Postoperative care protocol covers a 5-week-long time span, divided in 3 phases. Phase 1 (weeks 0-6) aims at the repair’s protection, pain, and inflammation control. The first 3 weeks consist of immobilization only, using a shoulder sling at about 15° of abduction and neutral rotation. Phase 2 begins at the seventh week, introducing progressive active movements and rotator strengthening. The last phase, from weeks 12 to 20, is aimed at muscular strengthening and coordination, to recover full force and functionality.
Discussion
This paper describes a simple and reproducible Technical Note called “LASCA” to be used for biological augmentation of rotator cuff repairs using subacromial bursa. The only similar paper was published recently by Freislederer et al.,6 in which the authors proposed a technique to sew the mobilized parietal sheet of the SB above a double-row rotator cuff repair. Frailty of the bursal tissue, which may result in the suture’s pull out, and potential formation of adhesions in the subdeltoid recess resulting in secondary stiffness were described as potential risks.6 LASCA presents even less-specific risks and limitations. In a few cases, in fact, the SB tissue may be insufficient or absent, and the technique may require modification. It is possible, for example, to check for the presence and quality of SB during the described articular phase, just before LHBT tenotomy. Eventually, the tenotomy can be performed with the shaver, with the GraftNet connected to it, to harvest LHBT’s tissue that was similarly demonstrated to be a promising MSCs source.1,5 The absence of the LHBT in the articular space, along with a low representation of the SB, is a limitation precluding LASCA. A second limitation is the dependence on the harvesting device, without which the technique would be extremely difficult to perform. Moreover, an aggressive bursectomy may result in larger bursal fragments, which may clog the filtering device. Lastly, displacement of the harvested SB may happen during its deployment if this surgical step is not carefully performed. It must be synced with the suture closure.
LASCA offers many more practical advantages due to its simplicity. First of all, it is extremely reproducible, as the SB removal with a shaver (and therefore its harvesting) is a surgical act with which all shoulder arthroscopists are familiar. The deployment of the harvested tissue with the proposed homemade system is another simple act, only requiring the ability to triangulate. It does not extend surgical time, and does not need to be planned in advance, as it relies on one “out of the box device,” and one construct made from items always available in every surgical room. Lastly, it is applicable to every surgical technique used for rotator cuff repairs, from open to arthroscopic procedures. LASCA, therefore, is accessible even to beginner shoulder arthroscopists.
Advantages are also present from a biological standpoint. This augmentation, in fact, involves harvesting of a local autologous tissue, avoiding host-to-graft reactions and donor-site morbidity. It has all the advantages of arthroscopic procedures in terms of fast recovery and reduced invasiveness. It uses an MSC source that appears successful in improving the rate of tendon healing,7 and harvests it by mechanical chopping, methodology that resulted in a superior count of cells able to proliferate, compared with whole bursal tissue or enzymatic digestion.3
In conclusion, LASCA is a feasible technique for biological augmentation of rotator cuff tears, accessible to every shoulder surgeon, and adaptable to many different techniques. Advantages are discussed in Table 1. Properly conducted outcomes study are needed, however, to assess its beneficial effects.
Table 1.
Main Advantages of LASCA
| Technical |
| Applicable to any type of repair |
| Easy and reproducible |
| No influence on standard surgical times |
| No planning required |
| Minimal costs |
| Beginner friendly |
| Biological |
| No host to graft reactions |
| No donor-site morbidity |
| MSCs with greater potential than other common sources3,4,7 |
| Arthroscopy: minimal invasiveness |
| Arthroscopy: faster recovery |
LASCA, local autologous stem cells application; MSC, mesenchymal stem cell.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This is a right shoulder in lateral decubitus. A posterior portal is used for the camera and the joint is assessed. A lateral working portal is performed and used to refresh the lesion and to prepare the footprint. In this case, a shuttle suture is applied on the long head of the biceps tendon for a subsequent soft-tissue tenodesis, then tenotomy is performed with radiofrequencies. Subacromial phase starts. It is mandatory to connect the filter device to the shaver to harvest the bursal tissue. It can be noted that no extra time is wasted during the bursectomy, and only the amount of bursa needed to clear the surgical field is removed and therefore harvested. Rotator cuff tear is assessed for reduction and repairability, and a triple-loaded anchor is implanted. The most anterior suture is passed with the shuttle suture trough the cuff and the biceps tendon; other sutures are passed with a suture passer. All sutures are tied apart from the middle one. The delivery system is introduced in the joint and its tip is positioned under the rotator cuff. Lastly, the harvested tissue is injected while the last knot is secured. Only minimal displacement of the injected tissue occurs during deployment.
References
- 1.Randelli P., Conforti E., Piccoli M. Isolation and characterization of 2 new human rotator cuff and long head of biceps tendon cells possessing stem cell-like self-renewal and multipotential differentiation capacity. Am J Sports Med. 2013;41:1653–1664. doi: 10.1177/0363546512473572. [DOI] [PubMed] [Google Scholar]
- 2.Randelli P., Randelli F., Ragone V. Regenerative medicine in rotator cuff injuries. Biomed Res Int. 2014;2014:129515. doi: 10.1155/2014/129515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morikawa D., Muench L.N., Baldino J.B. Comparison of preparation techniques for isolating subacromial bursa-derived cells as a potential augment for rotator cuff repair. Arthroscopy. 2020;36:80–85. doi: 10.1016/j.arthro.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Song N., Armstrong A.D., Li F., Ouyang H., Niyibizi C. Multipotent mesenchymal stem cells from human subacromial bursa: Potential for cell based tendon tissue engineering. Tissue Eng Part A. 2014;20:239–249. doi: 10.1089/ten.tea.2013.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Utsunomiya H., Uchida S., Sekiya I., Sakai A., Moridera K., Nakamura T. Isolation and characterization of human mesenchymal stem cells derived from shoulder tissues involved in rotator cuff tears. Am J Sports Med. 2013;41:657–668. doi: 10.1177/0363546512473269. [DOI] [PubMed] [Google Scholar]
- 6.Freislederer F., Dittrich M., Scheibel M. Biological augmentation with subacromial bursa in arthroscopic rotator cuff repair. Arthrosc Tech. 2019;8:e741–e747. doi: 10.1016/j.eats.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hernigou P., Flouzat Lachaniette C.H., Delambre J. Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: A case-controlled study. Int Orthop. 2014;38:1811–1818. doi: 10.1007/s00264-014-2391-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This is a right shoulder in lateral decubitus. A posterior portal is used for the camera and the joint is assessed. A lateral working portal is performed and used to refresh the lesion and to prepare the footprint. In this case, a shuttle suture is applied on the long head of the biceps tendon for a subsequent soft-tissue tenodesis, then tenotomy is performed with radiofrequencies. Subacromial phase starts. It is mandatory to connect the filter device to the shaver to harvest the bursal tissue. It can be noted that no extra time is wasted during the bursectomy, and only the amount of bursa needed to clear the surgical field is removed and therefore harvested. Rotator cuff tear is assessed for reduction and repairability, and a triple-loaded anchor is implanted. The most anterior suture is passed with the shuttle suture trough the cuff and the biceps tendon; other sutures are passed with a suture passer. All sutures are tied apart from the middle one. The delivery system is introduced in the joint and its tip is positioned under the rotator cuff. Lastly, the harvested tissue is injected while the last knot is secured. Only minimal displacement of the injected tissue occurs during deployment.