Abstract
Antimicrobial resistance (AMR) is an important threat to public health worldwide. Furthermore, different studies have demonstrated a close association between antibiotic use in animal production and AMR in humans. It is well known that it is necessary to reduce antibiotic administration in farms by finding effective alternative treatments, using more resistant breeds and improving animal welfare. However, to be able to assess the alternatives proposed, it is essential to study the epidemiology of AMR under production conditions. Hence, the aim of this study was to investigate the AMR dynamic in 2 genetic poultry breeds during the growing period. The study was performed in 2 experimental poultry houses to simulate real production conditions, and no antibiotics were administered during the growing period. In addition, 2 poultry breeds were used, fast-growing and slow-growing. To evaluate AMR evolution, Escherichia coli was selected as indicator bacterium. To this end, animals from each experimental group were sampled at different times: on day of arrival, at mid-period, and at slaughter day. In the laboratory, cecal content was removed and inoculated in selective media. Then, biochemical tests were performed to confirm E. coli. Finally, antibiotic susceptibility was assessed according to Decision 2013/653. At the onset of the cycle, significant differences were observed between breeds, as the E. coli strains isolated from fast-growing 1-day-old-chicks showed higher AMR rates. However, at the end of the period, no significant differences were found between breeds and their presence of resistant bacteria (above 95%). Therefore, although no antibiotics were administered during the growing period, a high level of AMR at slaughter day was demonstrated. Further studies are necessary to determine the main risk factors that increase the level of AMR throughout the productive cycle in broiler chickens. In conclusion, it is important to highlight that although it is crucial to control both antibiotic use and animal welfare during the growing period, measures should be taken at all levels of the production chain.
Key words: antimicrobial resistance, multidrug-resistance, broiler, growing period, Escherichia coli
Introduction
Antimicrobial resistance (AMR) has become a major threat for public health worldwide (WHO, 2014). One of the main factors contributing to the emergence of resistant bacteria has been the massive use of antimicrobials for growth promotion and disease prevention for several years in animal production (Guo et al., 2018, Mehdi et al., 2018). However, although nowadays the use of antibiotics in poultry is a controlled practice (ESVAC, 2017), different studies demonstrated a close association between the antibiotic use in animal production and AMR in humans (Marshall and Levy, 2011, Chang et al., 2015, Founou et al., 2016, Horigan et al., 2016, Liu et al., 2016, Sharma et al., 2018) by the transfer of resistance from animal products to humans (Chantziaras et al., 2013). As a result, commonly used antibiotics have become ineffective in the treatment of a wide variety of bacterial diseases (Khurana et al., 2017, EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control), 2018). For that reason, society is pressing for a reduction in antibiotic administration and greater efforts to find effective alternatives to control infectious diseases in farms (Alós, 2015, Gadde et al., 2017).
Consequently, several classes of alternatives have been proposed and tested in poultry production, including probiotics, prebiotics, symbiotics, organic acids, enzymes, phytogenics, metals, antibacterial vaccines, immunomodulatory agents, antimicrobial peptides, bacteriophages, and different broiler chicken growth systems (Hancock et al., 2012, Cheng et al., 2014, Castellini and Dal Bosco, 2017, Polycarpo et al., 2017, Alagawany et al., 2018, Sevilla-Navarro et al., 2018, Suresh et al., 2018).
In response to the social pressure to reduce antibiotic administration and find effective alternatives to control the presence of bacterial infections in farms (Alós, 2015, Gadde et al., 2017, Lusk, 2018a), the alternative poultry production system (organic, free-range) is founded on a different approach, keeping sustainability and animal welfare in consideration. Producers are therefore motivated to choose breeds selected for their ability to deal with the natural environment (Castellini and Dal Bosco, 2017).
However, to be able to assess the effectiveness of these alternatives, it is necessary to have better knowledge of the epidemiology of AMR throughout the growing period under animal production conditions (Sirri et al., 2011, Lusk, 2018b). For this purpose, commensal Escherichia coli has typically been selected as AMR sentinel, as it provides valuable data and constitutes a reservoir of resistance genes, which can spread horizontally to zoonotic and other bacteria (EFSA and ECDC, 2019).
Hence, the objective of this study was to investigate the AMR and multidrug resistance (MDR) dynamic in 2 genetic poultry breeds, fast-growing, and slow-growing, during the growing period, using commensal E. coli as sentinel bacterium.
Materials and methods
In this experiment, all animals were handled according to the principles of animal care published by Spanish Royal Decree 53/2013 (Spain, 2013).
Experiment Design
The study was performed in 2 poultry houses of an experimental poultry house in the Centre for Animal Research and Technology (in its Spanish acronym, Valencian Institute for Agrarian Research, IVIA, Segorbe, Spain) to simulate the real conditions of poultry production. Two commercial breeds were used, one fast-growing (Ross) and the other slow-growing (Hubbard), the latter being a more animal-friendly alternative and increasingly demanded by consumers. The fast-growing breed is characterized by efficient feed conversion and a good meat yield (Ross, 2019). In contrast, the slow-growing breed is focused on the criteria of animal welfare, meat quality, and absence of antibiotics (Valls, 2017).
To this end, 576 broilers (males and females) provided from the same hatchery were located in 2 identical poultry rooms (replica A and B), and 288 animals were housed in each room (144 of fast-growing and 144 for slow-growing). The animals were randomly housed in 24 pens (12 pens for each breed) of 1.3 m2 in a final stocking density of 35 kg/m2, with wood shavings as bedding material. The house was supplied with programmable electrical lights, automated electric heating, and forced ventilation. The environmental temperature was gradually decreased from 32°C (1 D) to 19°C (42 D) in line with common practice in poultry production. The experimental pelleted feed was commercial feed according to standard diets for broilers. Two different age diets were offered to the birds: starter (1 D to 21 D) and grower (21 D to 42 D/63 D). Only one batch of feed per age (starter and grower) was manufactured. The starter diet was the same for both breeds, while the grower feed was the standard diet specific for each breed. Nutritional and product analysis was assessed before the arrival of animals. Feed was weighed, manually distributed, and added ad libitum. Furthermore, the mortality and the presence of diarrhea were recorded daily. Finally, animals were weighed at weekly intervals, and feed consumption per pen was recorded.
Sample Collection
To assess the dynamic of AMR rates in the microbiota of broilers throughout the growing period, commensal E. coli was selected as sentinel (EFSA and ECDC, 2018). To this end, 30 animals from each experimental group were randomly selected and sampled at different points during the growing period: on arrival (one-day-old chicks), at the mid-period (21-day-old), and before slaughter (42 D of age in fast-growing, and 63 D in slow-growing). Cecum samples were taken individually and placed in sterile jars. The samples were processed within 24 h after collection.
E. coli Isolation
Cecal content was removed and homogenized. Afterward, pools of 6 animals from each replica were prepared (5 pools/treatment), and the pools content was cultured directly onto a nonspecific medium: blood agar (Scharlab, S.L., Barcelona, Spain) in aerobic and anaerobic conditions, and 2 gram-negative specific media: MacConkey agar (Scharlab, S.L.) and Coliform chromogenic agar (Scharlab, S.L.). Agar plates were incubated at 37°C ± 1°C for 24 h. After incubation, suspected colonies were streaked into a nutrient medium (Scharlab, S.L.) and incubated at 37°C ± 1°C for 24 h. Then, API-20E test (Biomerieux, S.L.) was performed to confirm E. coli.
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility was tested according to the European Committee on Antimicrobial Susceptibility Testing guidelines (Matuschek et al., 2014). The source for zone diameters used for interpretation of the test was http://www.eucast.org/clinical_breakpoints/. E. coli strains were inoculated into Mueller-Hinton agar (Scharlab, S.L.) to form a bacterial lawn, the antibiotic discs were added, and plates were incubated at 37°C for 24 h. The antibiotics selected were those set forth in Decision 2013/653 (European Union, 2013), including 2 quinolones: ciprofloxacin (CIP, 5 μg) and nalidixic acid (NAL, 30 μg); 3 b-lactams: ampicillin (AMP, 10 μg), cefotaxime (CTX, 30 μg), and ceftazidime (CAZ, 30 μg); one phenicol: chloramphenicol (CHL, 5 μg); one potentiated sulfonamide: trimethoprim-sulfamethoxazole (SXT, 1.25/23.75 μg); one polymyxin: colistin (CST, 10 μg); one macrolide: azithromycin (AZM, 15 μg); one glycylcycline: tigecycline (TGC, 15 μg); one aminoglycoside: gentamycin (GEN, 10 μg); and one pyrimidine: trimethoprim (TMP, 5 μg). MDR was defined as acquired resistance to at least one agent in 2 or more antimicrobial classes (EFSA and ECDC, 2016).
Statistical Analysis
A generalized linear model was used to compare the AMR rates between breeds (fast-growing vs. slow-growing breed) and between antibiotics throughout the growing period (beginning, mid-period, and slaughter day). A P-value < 0.05 was considered to indicate a statistically significant difference. Analyses were carried out using a commercially available software application (SPSS 24.0 software package; SPSS Inc., Chicago, IL, 2002).
Results
During this study, all the productive parameters obtained corresponded to the breed standards, and no clinical signs were observed. During growing, a total of 50 pools of cecal content were examined in 4 agar plates, of which 199 (n = 200) were culture positive for E. coli (100 for fast-growing breed and 99 for slow-growing breed).
Prevalence of Antibiotic Resistance
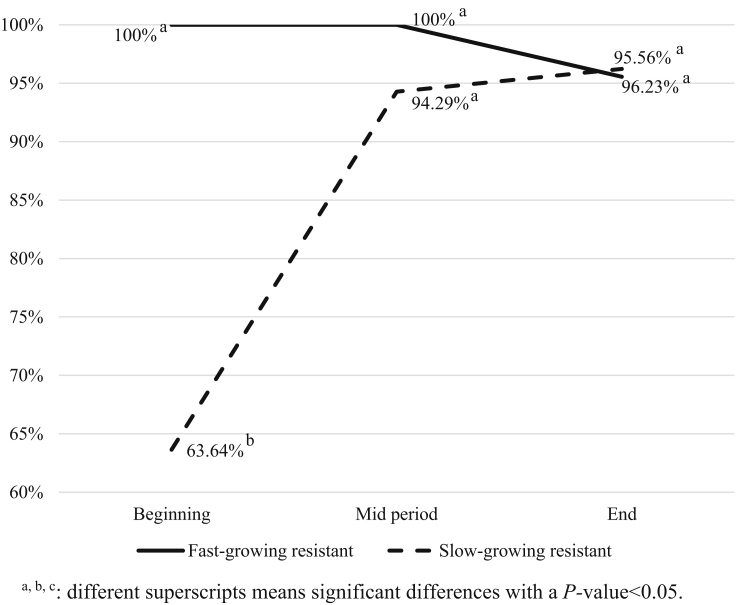
AMR rates of E. coli isolates from both breeds are presented in Figure 1. For all strains isolated, 98.0% (n = 98) and 91.9% (n = 91) from fast-growing and slow-growing breed, respectively, were resistant to at least one out of the 12 antibiotics tested. Moreover, statistically significant differences in AMR rates were shown throughout the growing period according to the breed studied (P-value < 0.05). At the onset of the growing period, 100.0% (n = 12) and 63.6% (n = 11) of the isolates from fast-growing and slow-growing breed were antibiotic resistant, and the strains isolated from fast-growing animals presented a higher AMR rate, with statistical differences between breeds (P-value < 0.05). However, by the end of the growth period, these differences disappeared; the fast-growing breed reached an AMR rate of 95.6%, and the slow-growing breed reached an AMR rate of 96.2%.
Figure 1.
Antimicrobial resistant E. coli strains dynamic in fast-growing and slow-growing breed throughout the growing period. a, b, c: different superscripts means significant differences with a P-value < 0.05.
For the fast-growing and slow-growing breed, E. coli AMR rates obtained against different antibiotics tested over time are summarized in Table 1.
Table 1.
Antibiotic resistance rates according to the antibiotic and the moment of the growing period in fast-growing and slow-growing breed.
| Breed | Sample moment | n | CIP | NAL | CTX | CAZ | AMP | CHL | SXT | CST | AZM | TGC | GEN | TMP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fast-growing breed | Beginning | 12 | 50b | 91.7 | 8.3 | 33.3c | 91.7b | 8.3 | 41.7 | 0 | 8.3a | 0 | 8.3 | 50 |
| Mid-period | 43 | 95.4c | 83.7 | 11.6 | 11.6b | 55.8a | 2.3 | 58.1 | 9.3 | 9.3a | 0 | 2.3 | 55.8 | |
| End | 45 | 20a | 71.1 | 0 | 0a | 53.3a | 4.4 | 35.6 | 8.9 | 82.2b | 0 | 0 | 51.1 | |
| Slow-growing breed | Beginning | 11 | 0a | 0a | 0 | 27.3 | 27.3a | 0 | 0 | 0 | 0a | 0 | 0 | 9.1 |
| Mid-period | 35 | 91.4b | 57.1b | 17.1 | 5.7 | 42.9a | 0 | 28.6 | 0 | 2.9a | 0 | 0 | 31.4 | |
| End | 53 | 11.3a | 86.8c | 7.6 | 9.4 | 66.9b | 5.7 | 26.4 | 9.4 | 41.5b | 0 | 1.9 | 45.3 |
a, b, c: different superscripts in each column means significant differences with a P-value<0.05.
Bold values indicate total number of strains per each sampling moment.
Abbreviations: AMP, ampicillin; AZM, azithromycin; CAZ, ceftazidime; CHL, chloramphenicol; CIP, ciprofloxacin; CST, colistin; CTX, cefotaxime; GEN, gentamycin; NAL, nalidixic acid; SXT, trimethoprim-sulfamethoxazole; TGC, tigecycline; TMP, trimethoprim.
Prevalence of Multidrug Resistance
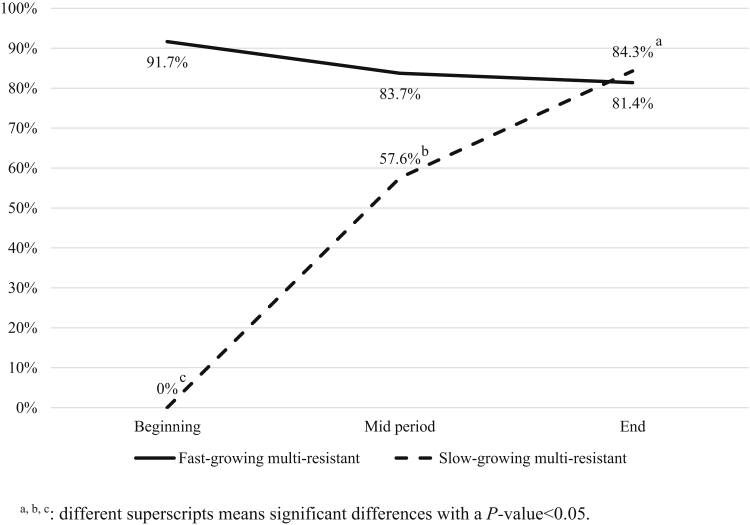
According to the MDR rates observed in fast-growing E. coli strains, on arrival day, 75.0% of the antibiotic resistant strains showed an MDR pattern, and this pattern was maintained until the end of the growing period (83.7%) (P-value>0.05).
Conversely, for slow-growing breed, none of the E. coli strains isolated at the start of the growth period showed an MDR pattern (0%), although this percentage increased to 84.3% (43/51) before slaughter (P-value < 0.05) (Figure 2).
Figure 2.
Multidrug-resistant E. coli strains dynamic in fast-growing and slow-growing breed throughout the growing period. a, b, c: different superscripts means significant differences with a P-value < 0.05.
Antibiotic Resistance Patterns
For the fast-growing breed, no AMR was observed in 2 (2.0%) of the isolates, and 12 E. coli strains were resistant to only one antibiotic, 18 (18.0%) to 2, 13 (13.0%) to 3, 21 (21.0%) to 4, 25 (25.0%) to 5, 3 (3.0%) to 6 and to 7, and 2 (2.0%) to 8. Only one isolate was resistant to 10 of the 12 antibiotics tested (Table 2).
Table 2.
Number of E. coli strains isolated resistant to the different number of antibiotics tested according to the sampling moment in fast-growing and slow-growing breeds.
| Breed | Sampling moment | Number of AMR to the indicated number of antibiotics |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total | ||
| Fast-growing breed | Beginning | 0 | 1 | 2 | 3 | 1 | 3 | 1 | 0 | 1 | 0 | 0 | 12 |
| Mid-period | 0 | 3 | 7 | 6 | 11 | 13 | 0 | 2 | 0 | 0 | 1 | 43 | |
| End | 2 | 8 | 9 | 4 | 9 | 9 | 2 | 1 | 1 | 0 | 0 | 45 | |
| Total | 2 | 12 | 18 | 13 | 21 | 25 | 3 | 3 | 2 | 0 | 1 | 100 | |
| Slow-growing breed | Beginning | 4 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 |
| Mid-period | 2 | 10 | 7 | 3 | 6 | 4 | 2 | 1 | 0 | 0 | 0 | 35 | |
| End | 2 | 8 | 6 | 18 | 12 | 3 | 1 | 2 | 0 | 1 | 0 | 53 | |
| Total | 8 | 25 | 13 | 21 | 18 | 7 | 3 | 3 | 0 | 1 | 0 | 99 | |
Abbreviation: AMR, antimicrobial resistance.
Bold values indicate E. coli strains isolated resistant to the different number of antibiotics.
For the slow-growing breed, 8 (8.1%) E. coli isolates were completely susceptible to all the antibiotics tested, 25 (25.3%) isolates were resistant to only one antibiotic and 13 (13.1%) to 2, 21 (21.2%) to 3, 18 (18.2%) to 4, 7 (7.1%) to 5, and 3 (3.0%) to 6 and to 7. Only one isolate was resistant to 9 of the 12 antibiotics tested (Table 2).
Overall, 59 different resistance patterns were observed. The combination of CIP-NAL-AMP-SXT-TMP (n = 21, 20%) was the most frequently observed pattern, followed by CIP alone (n = 13, 6.5%), the combination of NAL-AMP-SXT-TMP (n = 11, 6.5%) and NAL-AMP-TMP (n = 11, 6.5%).
AMR to the combination NAL-AMP was found in 56.0% and 46.5% of fast-growing and slow-growing E. coli strains, respectively, followed by resistance to the combination CIP-NAL (48.0% for fast-growing breed and 25.3% for slow-growing breed). Finally, it is important to highlight that 35.0% of fast-growing isolates and 18.2% of slow-growing isolates showed resistance to the combination CIP-AMP-NAL.
Discussion
The present study assessed the AMR dynamic in fast-growing and slow-growing breeds throughout the growing period under commercial farms conditions. To our best knowledge, this is the first study in the scientific literature to evaluate the relationship between both breeds on AMR evolution under the same production conditions.
Social pressure against intensive production systems demands the prohibition of antibiotic administration during the growing period and the use of new welfare-friendly breeds, which means chickens genetically adapted to less intensive production conditions (Castellini and Dal Bosco, 2017). However, our results demonstrated that although nonantibiotics were administered during the growing period, the same AMR rates were observed in both breeds (fast-growing and slow-growing) at the end of the growing period.
In 2016, the EFSA reported that 77.8% of E. coli isolated from broilers in European Union (EU) were resistant to antibiotics. However, there were large differences in AMR rates between EU Member States, being notably lower in Nordic countries and higher in Southern countries, especially Spain (EFSA and ECDC, 2018).
Regarding AMR rates obtained for the different antibiotics assessed, it is important to highlight the results obtained for TGC and CST, as they are the last-resort drugs used to treat human infectious diseases caused by multiresistant bacteria (Kern, 2018). On the one hand, in this study, the AMR to TGC was not detected in any isolate strain. This result agrees with that reported by the EFSA, in the EU, where only 4 countries presented AMR to this antibiotic (EFSA and ECDC, 2018). The total susceptibility to TGC might be explained by its restricted use to human hospital treatments (PRAN, 2018). On the other hand, resistance to CST was found in both breeds. These results are also similar to those reported by the EFSA, in which only 7 countries, including Spain, reported AMR to CST (EFSA and ECDC, 2018). Moreover, in other countries such as China, CST AMR rates reported were also very high (Zhang et al., 2019). This fact can be explained by its use in animal production for several years, especially in swine, to treat infectious diseases and as a growth promotor (ESVAC, 2017). Thus, the use of CST as a growth promoter has resulted in a high AMR to CST worldwide. It is important to highlight that the use of antibiotics as a growth promotor is a production technique that has been banned in the EU since 2006 (European Union, 2003).
The AMR rates shown in this study to CTX, CAZ, CHL, and GEN were low, in accordance with results obtained in previous studies in EU (EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control), 2018, MAPA (Ministry of Agriculture, Fishing and Food), 2018). However, Koga et al. (2015) recorded higher resistance rates in commercial broiler production in Brazil to all these antibiotics, except to CAZ.
It is important to highlight the high AMR obtained to CIP, NAL, AMP, SXT, AZM, and TMP in this study (Koga et al., 2015, Hussain et al., 2017, Ayandiran et al., 2018, EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control), 2018). Slight variations in AMR rates among isolates in these studies could be because of the different analysis methods employed, the different management systems set up, level of AMR in hatcheries, and use of antibiotics in the study areas (Okorafor et al., 2019). Specifically for AMP, TMP, and SXT, one hypothesis that could explain the results obtained in this study is that these antibiotics are permitted in Spain as therapeutic agents for bacterial infections, and as reported above for CST, they have been used as a growth promoter in animal production systems for several years (PRAN, 2018).
The results obtained in this study demonstrated the importance of AMR shedding from breeders to 1-day-old chicks. Several authors have shown that 1-day-old chicks are potential reservoirs of multiresistant enterobacteria obtained vertically from breeders (Jiménez-Belenguer et al., 2016, Projahn et al., 2017a, Projahn et al., 2017b, Okorafor et al., 2019). MDR bacteria could be transmitted through contaminated eggshells and/or from parent stock to hatchery (Projahn et al., 2017a, Daehre et al., 2017, Osman et al., 2018). Indeed, different reports have demonstrated that vertical transmission to chicks from the top of the production pyramid resulted in the introduction and spread of resistance genes in poultry (Borjesson et al., 2016, Osman et al., 2018).
On the other hand, horizontal transmission of AMR seems to be an important concern for the poultry industry (Szmolka and Nagy, 2013, Bengtsson-Palme et al., 2018, Agyare et al., 2018). Genomic analysis of the bacteria indicates that they could acquire their resistance profiles by incorporating different genetic elements through horizontal gene transfer (Agyare et al., 2018). For that reason, different scientific studies underline the importance of developing sanitary measures at the interface between the environment and livestock farming (Allen et al., 2010, Bengtsson-Palme et al., 2018, Westphal-Settele et al., 2018). However, it is important to highlight that in this study, the animals' origin is from the same hatchery. For this reason, further studies are necessary to compare the AMR dynamics from different companies.
In conclusion, the fact that the same AMR rates were observed, regardless of the breed studied, strongly suggests the possibility of vertical transmission from hatcheries and dissemination spread through the environment between flocks. Further studies are needed to confirm this hypothesis, and innovative-cost effective tools should be implemented at farm level to avoid antibiotic administration whenever possible throughout the broiler production chain.
Acknowledgments
The authors wish to thank the National Institute for Agricultural Research, Spain; Ministry of Economy, Industry and Competitiveness, Spain (RTA 2017-00013, Program: MINECO) and University CEU (INDI 19/32-18/28-17/25) for the financial support. Moreover, the authors wish to thank the “Improvement of Production System-related Food Safety and End Products” research group (Veterinary Faculty, University Cardenal Herrera-CEU) for their technical support. English text version was revised by N. Macowan English Language Service.
References
- Agyare C., Boamah V.E., Zumbi C.N., Osei F.B. Antibiotic use in poultry production and its effects on bacterial resistance. In: Kumar Yashwant., editor. Antimicrobial Resistance – A Global Threat. InTech Open Science; London, United Kingdom: 2018. pp. 1–20. [Google Scholar]
- Alagawany M., Abd El-Hack M.E., Farag M.R., Sachan S., Karthik K., Dhama K. The use of probiotics as eco-friendly alternatives for antibiotics in poultry nutrition. Environ. Sci. Pollut. Res. Int. 2018;25:10611–10618. doi: 10.1007/s11356-018-1687-x. [DOI] [PubMed] [Google Scholar]
- Allen H.K., Donato J., Wang H.H., Cloud-Hansen K.A., Davies J., Handelsman J. Call of the wild: antibiotic resistance genes in natural environments. Nat. Rev. Microbiol. 2010;8:251–259. doi: 10.1038/nrmicro2312. [DOI] [PubMed] [Google Scholar]
- Alós J. Resistencia bacteriana a los antibióticos: una crisis global. Enferm. Infecc. Microbiol. Clin. 2015;33:692–699. doi: 10.1016/j.eimc.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Ayandiran T.O., Falgenhauer L., Schmiede J., Chakraborty T., Ayeni F.A. High resistance to tetracycline and ciprofloxacin in bacteria isolated from poultry farms in Ibadan, Nigeria. J. Infect. Dev. Ctries. 2018;12:462–470. doi: 10.3855/jidc.9862. [DOI] [PubMed] [Google Scholar]
- Bengtsson-Palme J., Kristiansson E., Larsson D.G.J. Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiol. Rev. 2018;42 doi: 10.1093/femsre/fux053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borjesson S., Ny S., Egervarn M., Bergstrom J., Rosengren A., Englund S., Lofmark S., Byfors S. Limited dissemination of extended-spectrum beta-lactamase- and plasmid-encoded AmpC-producing Escherichia coli from food and farm animals, Sweden. Emerg. Infect. Dis. 2016;22:634–640. doi: 10.3201/eid2204.151142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellini C., Dal Bosco A. Animal Welfare and Poultry Meat in Alternative Production Systems (and Ethics of Poultry Meat Production) Woodhead Publishing Series in Food Science, Technology and Nutrition; Elservier Ltd.: 2017. Poultry quality evaluation: quality attributes and consumer values; pp. 335–357. [Google Scholar]
- Chang Q., Wang W., Regev-Yochay G., Lipsitch M., Hanage W.P. Antibiotics in agriculture and the risk to human health: how worried should we be? Evol. Appl. 2015;8:240–247. doi: 10.1111/eva.12185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chantziaras I., Boyen F., Callens B., Dewulf J. Correlation between veterinary antimicrobial use and antimicrobial resistance in food-producing animals: a report on seven countries. J. Antimicrob. Chemother. 2013;69:827–834. doi: 10.1093/jac/dkt443. [DOI] [PubMed] [Google Scholar]
- Cheng G., Hao H., Xie S., Wang X., Dai M., Huang L., Yuan Z. Antibiotic alternatives: the substitution of antibiotics in animal husbandry? Front. Microbiol. 2014;5:217. doi: 10.3389/fmicb.2014.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daehre K., Projahn M., Semmler T., Roesler U., Friese A. Extended-spectrum beta-lactamase-/AmpC beta-lactamase-producing Enterobacteriaceae in broiler farms: transmission dynamics at farm level. Microb. Drug Resist. 2017;24:511–518. doi: 10.1089/mdr.2017.0150. [DOI] [PubMed] [Google Scholar]
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control) ECDC; Stockholm: 2016. EU Protocol for Harmonised Monitoring of Antimicrobial Resistance in Human Salmonella and Campylobacter Isolates. [Google Scholar]
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control) The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2016. EFSA J. 2018;16:5182. doi: 10.2903/j.efsa.2018.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EFSA and ECDC (European Food Safety Authority and European Centre for Disease Control) Technical specifications on harmonised monitoring of antimicrobial resistance in zoonotic and indicator bacteria from food-producing animals and food. EFSA J. 2019;17:5709. doi: 10.2903/j.efsa.2019.5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESVAC (European Medicines Agency) 2017. Sales of Veterinary Antimicrobial Agents in 30 European Countries in 2015. Trends from 2010 to 2015. Seventh ESVAC Report. Accessed December 2019. https://www.ema.europa.eu/en. [Google Scholar]
- European Union . 2003. Regulation (EC) No 1831/2003 of the European Parliament and of the Council of 22 September 2003 on Additives for Use in Animal Nutrition (Text with EEA Relevance) Accessed December 2019. https://eur-lex.europa.eu/homepage.html?locale=en. [Google Scholar]
- European Union . 2013. Commission Implementing Decision 2013/653 of 12 November 2013 as Regards a Union Financial Aid towards a Coordinated Control Plan for Antimicrobial Resistance Monitoring in Zoonotic Agents in 2014 (Notified under Document C (2013) 7289) Accessed December 2019. https://eur-lex.europa.eu/homepage.html?locale=en. [Google Scholar]
- Founou L.L., Founou R.C., Essack S.Y. Antibiotic resistance in the food chain: a developing country-perspective. Front. Microbiol. 2016;7:1881. doi: 10.3389/fmicb.2016.01881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadde U., Kim W.H., Oh S.T., Lillehoj H.S. Alternatives to antibiotics for maximizing growth performance and feed efficiency in poultry: a review. Anim. Health Res. Rev. 2017;18:26–45. doi: 10.1017/S1466252316000207. [DOI] [PubMed] [Google Scholar]
- Guo X., Stedtfeld R.D., Hedman H., Eisenberg J.N.S., Trueba G., Yin D., Tiedje J.M., Zhang L. Antibiotic resistome associated with small-scale poultry production in rural Ecuador. Environ. Sci. Technol. 2018;52:8165–8172. doi: 10.1021/acs.est.8b01667. [DOI] [PubMed] [Google Scholar]
- Hancock R.E., Nijnik A., Philpott D.L. Modulating immunity as a therapy for bacterial infections. Nat. Rev. Microbiol. 2012;10:243–254. doi: 10.1038/nrmicro2745. [DOI] [PubMed] [Google Scholar]
- Horigan V., Kosmider R.D., Horton R.A., Randall L., Simons R.R. An assessment of evidence data gaps in the investigation of possible transmission routes of extended spectrum β-lactamase producing Escherichia coli from livestock to humans in the UK. Prev. Vet. Med. 2016;124:1–8. doi: 10.1016/j.prevetmed.2015.12.020. [DOI] [PubMed] [Google Scholar]
- Hussain A., Shaik S., Ranjan A., Nandanwar N., Tiwari S.K., Majid M., Baddam R., Qureshi I.A., Semmler T., Wieler L.H., Islam M.A., Chakravortty D., Ahmed N. Risk of transmission of antimicrobial resistant Escherichia coli from commercial broiler and free-range retail chicken in India. Front. Microbiol. 2017;8:2120. doi: 10.3389/fmicb.2017.02120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez-Belenguer A., Doménech E., Villagrá A., Fenollar A., Ferrús M.A. Antimicrobial resistance of Escherichia coli isolated in newly hatched chickens and effect of amoxicillin treatment during their growth. Avian Pathol. 2016;45:501–507. doi: 10.1080/03079457.2016.1168515. [DOI] [PubMed] [Google Scholar]
- Kern W.V. Multiresistant bacteria - antibiotic prescription and antibiotics of last resort. Dtsch. Med. Wochenschr. 2018;143:643–650. doi: 10.1055/s-0043-119958. [DOI] [PubMed] [Google Scholar]
- Khurana A., Shina R., Nagaraju M. Centre for Science and Environment; New Delhi: 2017. Antibiotic Resistance in Poultry Environment: Spread of Resistance from Poultry Farm to Agricultural Field. [Google Scholar]
- Koga V.L., Scandorieiro S., Vespero E.C., Oba A., de Brito B.G., de Brito K.C., Nakazato G., Kobayashi R.K. Comparison of antibiotic resistance and virulence factors among Escherichia coli isolated from conventional and free-range poultry. Biomed. Res. Int. 2015;2015:618752. doi: 10.1155/2015/618752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.Y., Wang Y., Walsh T.R., Yi L.X., Zhang R., Spencer J., Doi Y., Tian G., Dong B., Huang X., Yu L.F., Gu D., Ren H., Chen X., Lv L., He D., Zhou H., Liang Z., Liu J.H., Shen J. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 2016;16:161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- Lusk J.L. Food Marketing Institute Foundation, Animal Agriculture Alliance, and the Foundation for Food and Agriculture Research; 2018. Consumer Beliefs, Knowledge, and Willingness-To-Pay for Sustainability-Related Poultry Production Practices Broiler Survey Report. [Google Scholar]
- Lusk J.L. Consumer preferences for and beliefs about slow growth chicken. Poult. Sci. 2018;97:4159–4166. doi: 10.3382/ps/pey301. [DOI] [PubMed] [Google Scholar]
- Marshall B.M., Levy S.B. Food animals and antimicrobials: impacts on human health. Clin. Microbiol. Rev. 2011;24:718–733. doi: 10.1128/CMR.00002-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matuschek E., Brown D.F., Kahlmeter G. Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin. Microbiol. Infect. 2014;20:O255–O266. doi: 10.1111/1469-0691.12373. [DOI] [PubMed] [Google Scholar]
- Mehdi Y., Létourneau-Montminy M.P., Gaucher M.L., Chorfi Y., Suresh G., Rouissi T., Brar S.K., Côté C., Ramirez A.A., Godbout S. Use of antibiotics in broiler production: global impacts and alternatives. Anim. Nutr. 2018;4:170–178. doi: 10.1016/j.aninu.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAPA (Ministry of Agriculture, Fishing and Food) Informe JIACRA España. Primer análisis integrado del consumo de antibióticos y su relación con la aparición de resistencia. 2018. http://www.resistenciaantibioticos.es/es/publicaciones/informe-jiacra-espana
- Okorafor O.N., Anyanwu M.U., Nwafor E.O., Anosa G.N., Udegbunam R.I. Multidrug-resistant enterobacteria colonize commercial day-old broiler chicks in Nigeria. Vet. World. 2019;12:418–423. doi: 10.14202/vetworld.2019.418-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman K.M., Kappell A.D., Elhadidy M., ElMougy E., El-Ghany W.A.A., Orabi A., Mubarak A.S., Dawoud T.M., Hemeg H.A., Moussa I.M.I., Hessain A.M., Yousef H.M.Y. Poultry hatcheries as potential reservoirs for antimicrobial-resistant Escherichia coli: a risk to public health and food safety. Sci. Rep. 2018;8:5859. doi: 10.1038/s41598-018-23962-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polycarpo G.V., Andretta I., Kipper M., Cruz-Polycarpo V.C., Dadalt J.C., Rodrigues P.H.M., Albuquerque R. Meta-analytic study of organic acids as an alternative performance-enhancing feed additive to antibiotics for broiler chickens. Poult. Sci. 2017;96:3645–3653. doi: 10.3382/ps/pex178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRAN (Plan Nacional Resistencia Antibióticos) Antibióticos críticos. 2018. http://resistenciaantibioticos.es/es/profesionales/vigilancia/antibioticos-criticos
- Projahn M., Daehre K., Roesler U., Friese A. Extended-spectrum beta-lactamase and plasmid-encoded cephamycins-producing enterobacteria in broiler hatchery as a potential mode of pseudovertical transmission. Appl. Environ. Microbiol. 2017;83:e02364. doi: 10.1128/AEM.02364-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Projahn M., Daehre K., Semmler T., Guenther S., Roesler U., Friese A. Environmental adaptation and vertical dissemination of ESBL-/pAmpC-pro- ducing Escherichia coli in an integrated broiler produc- tion chain in the absence of antibiotic treatment. Microb. Biotechnol. 2017;11:1017–1026. doi: 10.1111/1751-7915.13040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross Ross 308/Ross 308 FF broiler: performance objectives. 2019. http://es.aviagen.com/assets/Tech_Center/Ross_Broiler/Ross308-308FF-BroilerPO2019-EN.pdf
- Sevilla-Navarro S., Marín C., Cortés V., García C., Vega S., Catalá-Gregori P. Autophage as a control measure for Salmonella in laying hens. Poult. Sci. 2018;97:4367–4373. doi: 10.3382/ps/pey294. [DOI] [PubMed] [Google Scholar]
- Sharma C., Rokana N N., Chandra M M., Singh B.P., Gulhane R.D., Gill J.P.S., Ray P P., Puniya A.K., Panwar H. Antimicrobial resistance: its surveillance, impact, and alternative management strategies in dairy animals. Front. Vet. Sci. 2018;8:237. doi: 10.3389/fvets.2017.00237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirri F., Castellini C., Bianchi M., Petracci M., Merluzzi A., Franchini A. Effect of fast-, medium- and slow-growing strains on meat quality of chickens reared under the organic farming method. Animal. 2011;5:312–319. doi: 10.1017/S175173111000176X. [DOI] [PubMed] [Google Scholar]
- Spain Royal Degree 53/2013, 1st of Febrary, por el que se establecen las normas básicas aplicables para la protección de los animales utilizados en experimentación y otros fines científicos, incluyendo la docencia. Boletín Oficial del Estado. 2013;34:11370–11421. [Google Scholar]
- Suresh G., Das R.K., Kaur Brar S., Rouissi T., Avalos Ramirez A., Chorfi Y., Godbout S. Critical Reviews in Microbiology Alternatives to antibiotics in poultry feed: molecular perspectives. Crit. Rev. Microbiol. 2018;44:318–335. doi: 10.1080/1040841X.2017.1373062. [DOI] [PubMed] [Google Scholar]
- Szmolka A., Nagy B. Multidrug resistant commensal Escherichia coli in animals and its impact for public health. Front. Microbiol. 2013;4:258. doi: 10.3389/fmicb.2013.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valls M. Reproductoras & pollos crecimiento lento. 2017. https://avicultura.info/reproductoras-y-pollos-de-crecimiento-lento/
- Westphal-Settele K., Konradi S., Balzer F., Schönfeld J., Schmithausen R. The environment as a reservoir for antimicrobial resistance: a growing problem for public health? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61:533–542. doi: 10.1007/s00103-018-2729-8. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization) Antimicrobial Resistance: Global Report on Surveillance 2014. 2014. https://www.who.int/drugresistance/documents/surveillancereport/en/
- Zhang X., Zhang B., Guo Y., Wang J., Zhao P., Liu J., He K. Colistin resistance prevalence in Escherichia coli from domestic animals in intensive breeding farms of Jiangsu Province. Int. J. Food Microbiol. 2019;291:87. doi: 10.1016/j.ijfoodmicro.2018.11.013. [DOI] [PubMed] [Google Scholar]