Abstract
Injuries to the acromioclavicular (AC) joint are common and comprise ∼12% of shoulder injuries. Stability to the AC joint depends on the coracoclavicular (CC) ligaments for vertical stability and AC ligaments and capsular structures for horizontal stability. Injuries to the AC ligaments can lead to horizontal instability of the AC joint. There is no gold standard technique for treating these injuries surgically, and many of the described procedures focus on vertical instability rather than horizontal instability. This article describes an open AC ligament reconstruction with semitendinosus allograft to restore horizontal stability of the AC joint.
The acromioclavicular (AC) joint is a diarthrodial joint connecting the acromion and the clavicle. Injuries to the AC joint are common and comprise ∼12% of shoulder injuries.1, 2, 3 Stability of the AC joint depends on contributions from both the coracoclavicular (CC) ligaments and AC ligament and capsular structures.4 The CC ligaments include the conoid and trapezoid ligaments, of which the conoid is stronger, and attach the clavicle to the coracoid process of the scapula, thereby providing vertical (superior-inferior) stability. The AC ligament comprises 4 components, of which the posterior and superior components are the strongest and attach the acromion to the distal clavicle, providing horizontal (anterior-posterior) stability to the AC joint.2,5 Injuries to this ligament lead to horizontal instability of the AC joint, which can cause chronic AC joint injuries, pain, and disability.6, 7, 8, 9
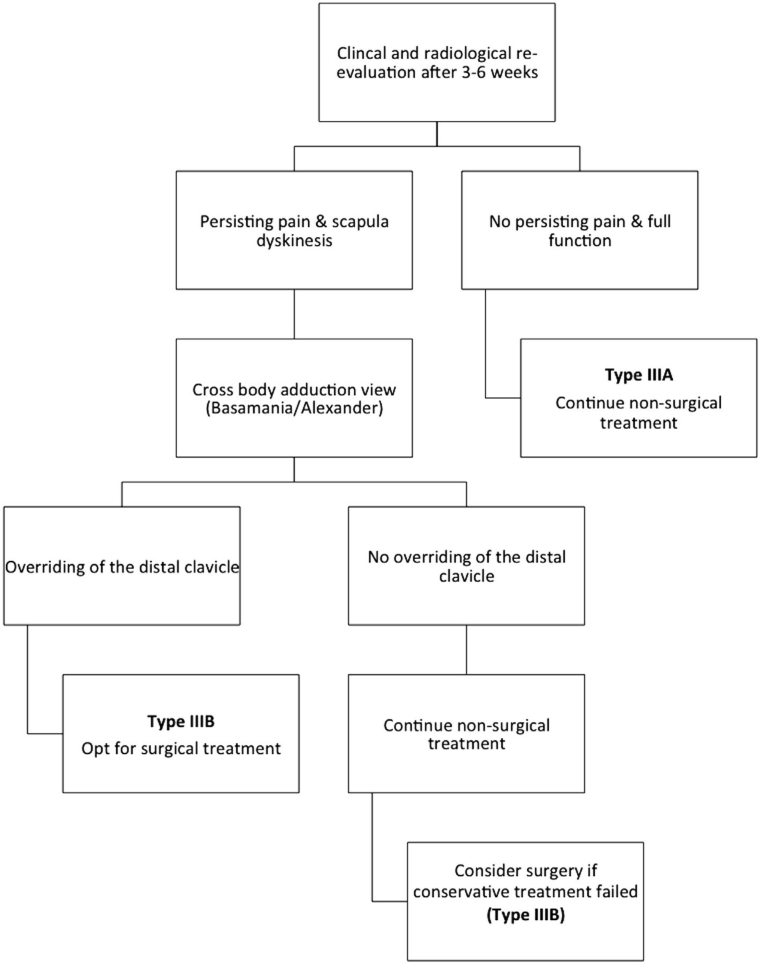
Acromioclavicular joint separations are classified using the modified Rockwood classification (Table 1; Figure 1).10,11 Type II injuries are often successfully treated nonoperatively with a short period of immobilization in an abduction sling, followed by shoulder rehabilitation focusing on scapular retraction. Rarely, isolated horizontal instability persists after failure of nonoperative management. Persistent horizontal instability can cause pain and functional impairment, especially with cross-body adduction. In these cases, surgery may be necessary to stabilize the AC joint.
Table 1.
Modified Rockwood Classification
| Type | Rockwood | Modification |
|---|---|---|
| I | Sprain of the AC ligament without radiographic abnormality; No CC ligament damage | |
| II | AC ligament and joint capsule disruption; Sprained, but intact, CC ligaments; 50% vertical subluxation of the distal clavicle | |
| III | AC ligament and joint capsule disruption; Disruption of the CC ligaments; 100% superior displacement of the distal clavicle | IIIA (stable) – Stable AC joint without overriding of the clavicle on the cross-body adduction view and without significant scapular dysfunction |
| IIIB (unstable) – Therapy-resistant scapular dysfunction and an overriding clavicle on cross-body adduction view | ||
| IV | Posterior displacement of the distal clavicle into the trapezius | |
| V | Injury to the AC and CC ligaments with >100% superior displacement of the clavicle | |
| VI | Subacromial or subcoracoid displacement of the clavicle |
Abbreviations: AC, acromioclavicular; CC, coracoclavicular.
Fig 1.
Modified Rockwood classification. The original Rockwood classification describes 6 types of acromioclavicular (AC) joint injuries. The modified Rockwood classification expands on Rockwood's original classification by separating type III injuries into stable (IIIA) and unstable (IIIB). Type IIIA injuries involve a stable AC joint without overriding of the clavicle on cross-body adduction view and without significant scapular dysfunction, whereas type IIIB injuries involve therapy-resistant scapular dysfunction and an overriding clavicle on cross-body adduction view.
There is no gold standard in the surgical treatment of AC joint injuries, particularly with regard to managing horizontal instability.3,12 More than 150 procedures for AC reconstruction have been described.13 Many of these procedures focus on CC ligament reconstruction (vertical instability) rather than AC ligament reconstruction (horizontal instability).12 This article describes an open technique for AC ligament repair and allograft reconstruction with semitendinosus allograft to restore horizontal stability of the AC joint (Video).
Surgical Technique
Indications for this procedure include any type II AC joint injury with attenuation of the AC joint ligament and capsule in a patient who failed extensive conservative treatment and has continued horizontal instability, pain, and poor shoulder function. Horizontal instability is confirmed on physical exam with tenderness over the AC joint and palpable instability and crepitus of the AC joint with digital manipulation and cross-body adduction against resistance. There is no vertical instability. MRI confirms the diagnosis of type II AC separation with tearing of the AC ligaments and intact coracoacromial (CA) ligaments with no rotator cuff tear.
The patient receives an interscalene nerve block to the affected shoulder before surgery. After induction of general endotracheal anesthesia, the patient is placed in the beach chair position, and all bony prominences are well padded. Examination under anesthesia confirms full passive range of motion of the operative shoulder with horizontal instability of the AC joint. The upper extremity is prepped and draped in the usual sterile fashion, and the patient receives antibiotic prophylaxis before an incision is made.
A 4-cm longitudinal incision is made on the superior aspect of the operative shoulder overlying the AC joint, and dissection is taken sharply down to the level of the fascia. Full-thickness skin flaps are raised both anterior and posterior to the clavicle and AC joint. The AC joint capsule is sharply incised in line with the clavicle to gain access to the AC joint. Visualization of the AC joint shows attenuation of the AC ligaments and disruption of the deep fibers on the distal clavicle, further confirming horizontal instability of the AC joint (Figure 2).
Fig 2.
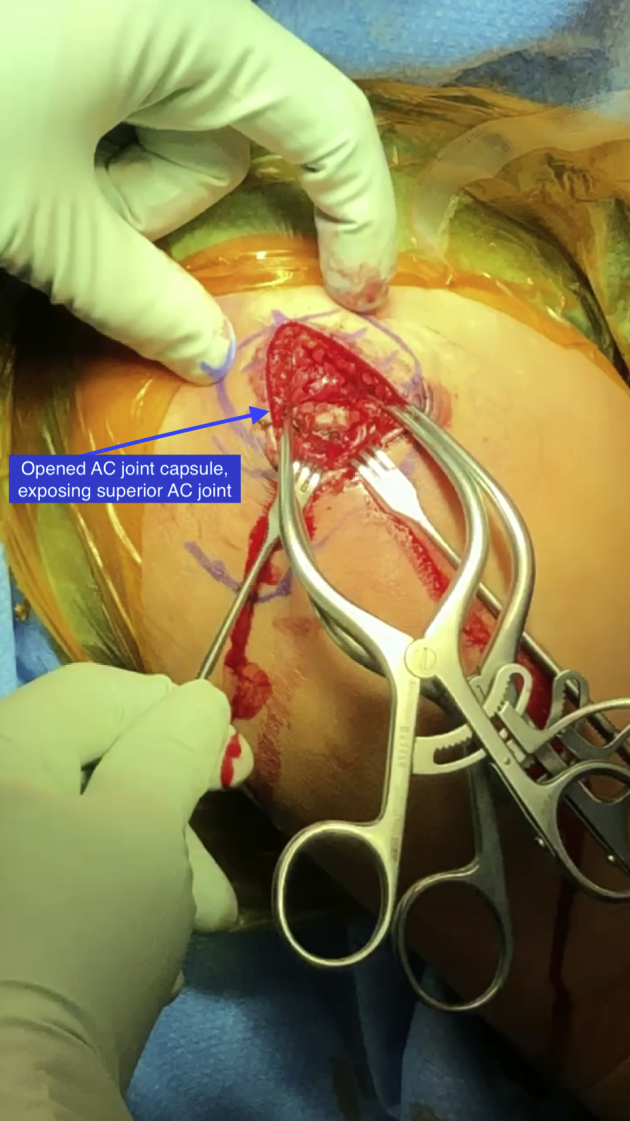
The right shoulder of a patient diagnosed with a type II acromioclavicular (AC) joint separation confirmed by magnetic resonance imaging is exposed while the patient is in the beach chair position. The AC joint is exposed through a superior incision in line with the clavicle. Here, the AC joint capsule has been opened, exposing the superior AC joint.
A semitendinosus or gracilis allograft is selected, and a running locked Krackow suture with #2 Ethibond is placed in each end of the tendon. The tendon is sized to determine the thickness of the allograft and diameter of interference screw for fixation. Typically, PEEK 5.5-mm interference screws (Arthrex, Naples, FL) are selected. A guidepin is inserted in the center of the distal clavicle 1 cm medial to the distal end, and a second guidepin is inserted in the acromion 1 cm lateral to the AC joint. A cannulated reamer is advanced over the guidepin to drill bicortical holes in the distal clavicle and the acromion. The drill holes are thoroughly irrigated to remove all bony debris.
The allograft tendon is then passed across the AC joint in a figure-8 fashion using a Hewson suture passer (Figure 3). The tail of the graft is placed posterior to the AC joint to reconstruct the posterior AC capsule. Superior pressure is applied to the elbow, and simultaneous downward pressure is applied to the clavicle to reduce the AC joint. While the AC joint is held, the graft is tensioned and secured by two 5.5 × 8-mm PEEK interference screws (Arthrex), 1 in the distal clavicle and 1 in the acromion (Figure 4). The graft is then sutured to itself with figure-8 sutures using #2 Ethibond (Figure 5). The AC joint native capsule and ligaments are repaired with a figure-8 suture over the top of the allograft reconstruction. Sutures are passed through the native AC joint capsule and through the allograft tendon, which provides excellent fixation of the allograft ligament and restores horizontal stability of the AC joint (Fig 6, Fig 7 through 8). The wound is irrigated, and the skin is closed in a layered fashion.
Fig 3.
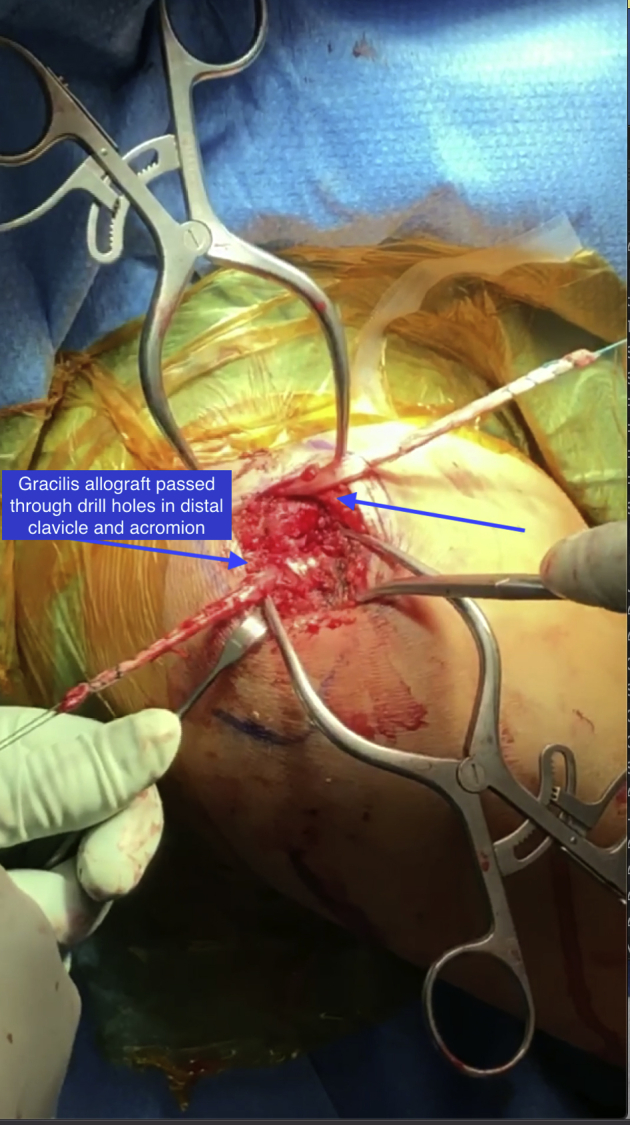
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position. The gracilis allograft has been passed through drill holes in the distal clavicle and acromion.
Fig 4.
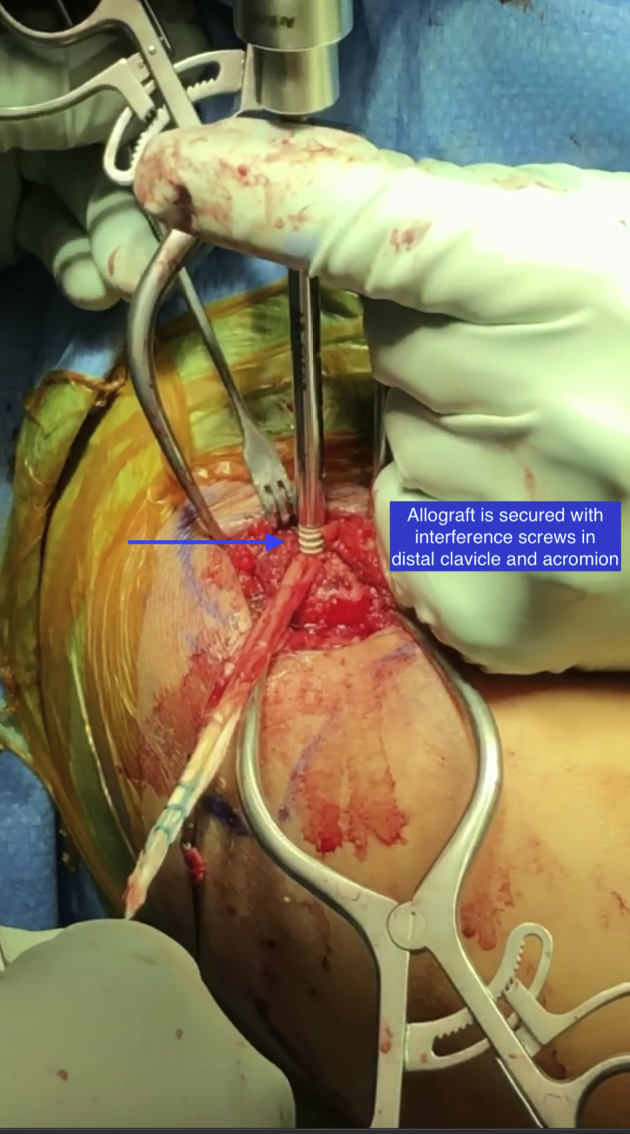
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position. After reducing the AC joint, the allograft is secured with 2 interference screws, 1 in the distal clavicle and 1 in the acromion.
Fig 5.
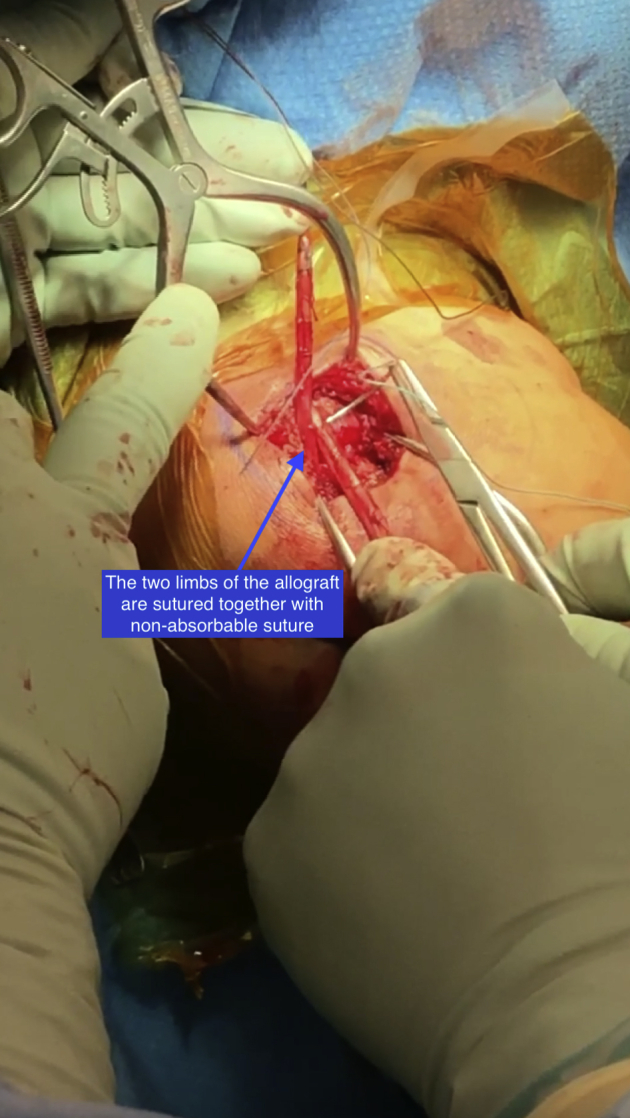
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position. The 2 limbs of the allograft are sutured together with nonabsorbable suture.
Fig 6.
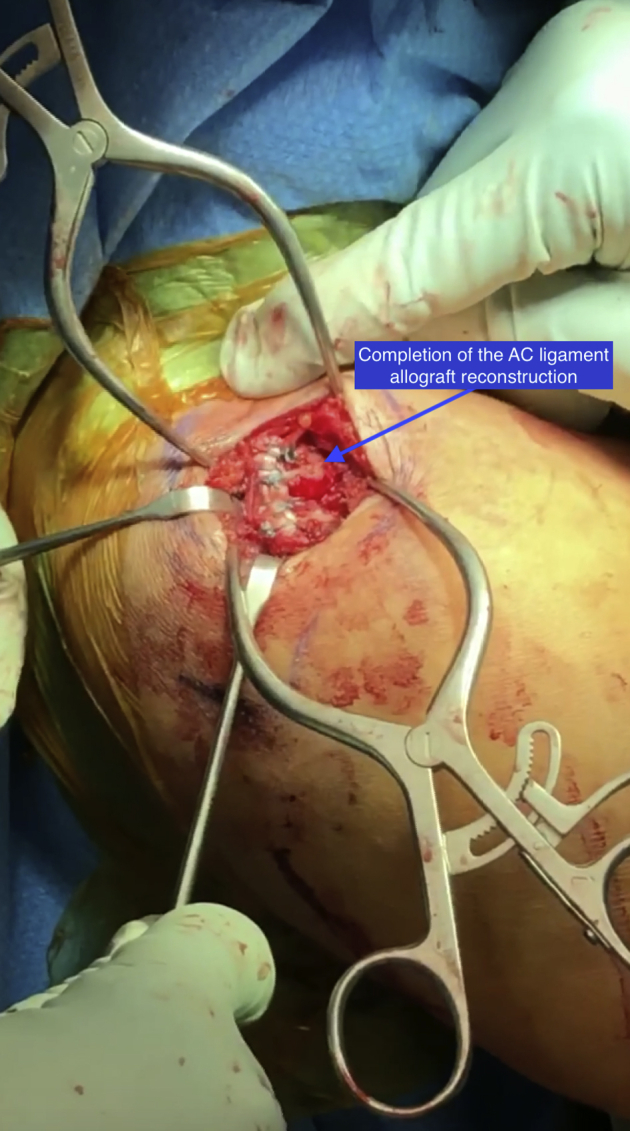
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position, depicting completion of the AC ligament allograft reconstruction. The horizontal stability of the AC joint can be assessed at the completion of the reconstruction.
Fig 7.
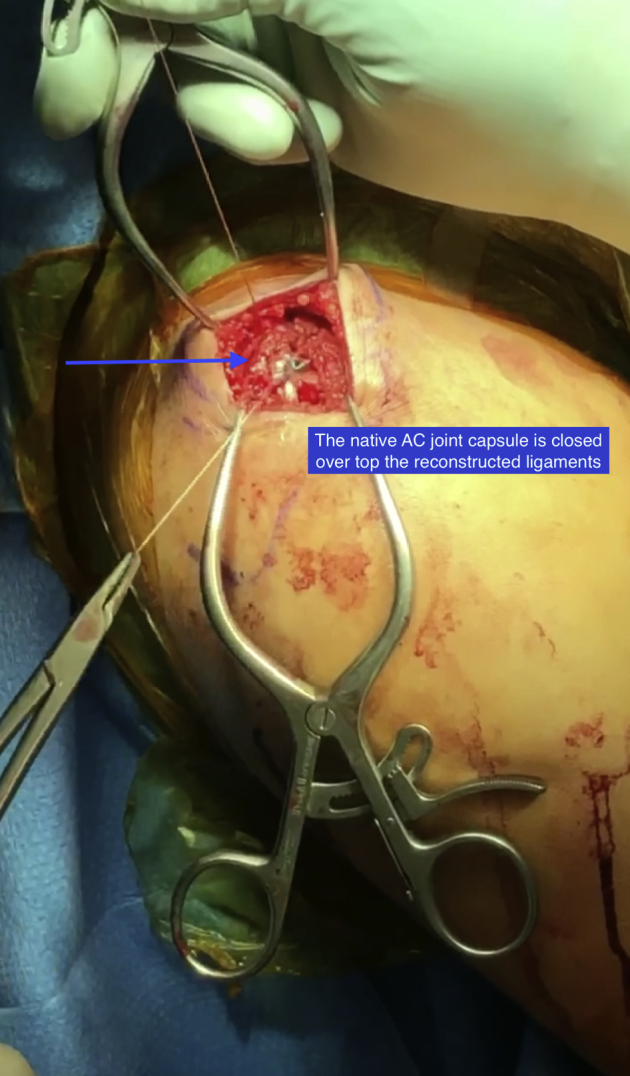
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position. The native AC joint capsule is closed over the top of the reconstructed ligaments.
Fig 8.
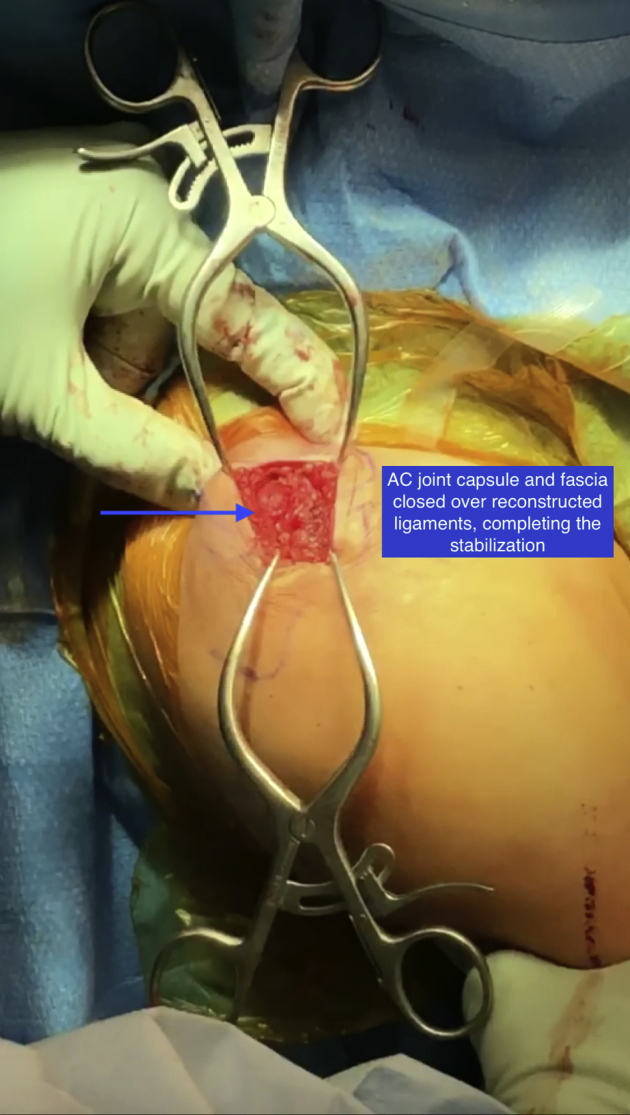
Superior view of the acromioclavicular (AC) joint in a right shoulder, with the patient in the beach chair position. The AC joint capsule and fascia have been closed over the reconstructed ligaments, completing the stabilization. The wound is thoroughly irrigated, closed, and dressed, and the patient is placed into an abduction pillow sling at the completion of the case.
Postoperatively, the upper extremity is maintained in an abduction pillow sling for 6 weeks. At the first postoperative visit, passive range of motion is initiated with forward elevation to 90° and external rotation to neutral. The patient begins scapular retraction exercises and posture training. Scapular retraction helps to reduce the AC joint. Cross-body adduction is avoided for the first 6 weeks. Active range of motion is initiated at 6 weeks, with progression to strengthening at 10 to 12 weeks.
Discussion
There is currently no consensus for the best surgical procedure to treat horizontal instability of the AC joint, and many of the described procedures for AC joint reconstruction focus on treating vertical instability rather than horizontal instability.12,14 The authors present a surgical technique for AC ligament reconstruction with a semitendinosus allograft with primary repair of the AC joint capsule for a type II AC joint separation with horizontal instability. The main advantage of our technique is the restoration of horizontal stability of the AC joint. Grade II AC separations are typically managed conservatively (e.g. nonsteroidal anti-inflammatory drugs, immobilization, physical therapy), but several studies have reported poor long-term outcomes in terms of pain and disability.15, 16, 17 In 2003, Mouhsine et al.17 evaluated 33 patients with grade I and II AC separations treated by conservative measures, including ice application, analgesics, and immobilization. The authors reported 27% of patients (9 of 33; 7 grade II and 2 grade I) failing conservative treatment and requiring subsequent surgery an average of 26 months after injury.17 The patients with grade II injuries were also found to have increased anterior-to-posterior (AP) laxity, suggesting residual horizontal instability of the AC joint.17 An overview of pearls and pitfalls as well as advantages and disadvantages of our technique are presented in Tables 2 and 3, respectively.
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Completely release the AC joint capsule to ensure anatomic reduction is achievable. | Keep drill holes centered in the clavicle and acromion to prevent fractures and avoid stress risers. |
| Distal clavicle resection can be performed in the setting of AC joint arthritis or distal clavicle osteophytes. | Use caution while drilling holes with the reamers to avoid damage to underlying rotator cuff and neurovascular structures. |
| Push up on the arm to aid in AC joint reduction during graft tensioning and graft fixation. | Place a Cobb elevator under the guide wire before reaming tunnels to prevent plunging or overdrilling. |
| Repair the native AC joint capsule to the allograft during closure. | Whipstitch the allograft tendon with a running, locked Krackow suture to prevent graft damage by the interference screw. |
Abbreviations: AC, acromioclavicular.
Table 3.
Advantages and Disadvantages
| Advantages |
|
|
|
| Disadvantages |
|
|
|
Abbreviations: AC, acromioclavicular.
Surgical procedures that treat horizontal instability of the AC joint have shown improved patient outcomes.1, 2, 3,18, 19, 20, 21 A recent study by Saier et al.19 evaluated whether isolated anatomic CC ligament reconstruction with 2 button devices provided equal horizontal stability compared with CC reconstruction with additional AC joint suture tape cerclage. After 5000 cycles of dynamic anteroposterior directed loading, only combined AC and CC reconstruction adequately achieved horizontal stability of the AC joint, highlighting the importance of reconstructing the AC ligament as well as the CC ligaments in patients with AC separations.19 In 2014, Beitzel et al.22 performed a cadaveric study to evaluate and directly compare the biomechanical performance of previously published AC ligament reconstruction techniques with anatomic CC reconstructions. The authors found that reconstruction of the AC ligament by direct wrapping and suturing of the graft around the AC joint was the most stable method, showing anterior rotation comparable with the native joint, whereas the transacromial technique in which a graft was passed over the acromion and into an acromial tunnel showed the most translation and rotation. The authors emphasized the importance of including AC ligaments as part of an anatomic reconstruction of the AC joint to better restore control of clavicle translation and rotation.22
Another beneficial feature of our technique includes the use of an allograft. Lee et al.23 investigated the strength of repair with tendon graft reconstruction (semitendinosus, gracilis, extensor hallucis longus) of the CC ligaments compared with the intact CC ligament complex and CA ligament transfer in a controlled laboratory study of 11 fresh-frozen human cadaver shoulders. The authors found that tendon graft reconstruction may provide improved biomechanical properties and a potential permanent biologic reconstruction, with an ultimate failure load equivalent to that of the native CC ligaments.23 In 2018, Moatshe et al.24 performed a systematic review to evaluate clinical and radiographic outcomes after surgical treatment for AC joint instability. The authors found that all techniques for surgical treatment of AC joint instability (i.e. free tendon graft, suspensory devices, synthetic ligament devices, and modified Weaver-Dunn, and hook plate/Kirschner wire techniques) improved patient outcomes and had relatively low reoperation rates (0.9% to 5.4%). The use of a free tendon graft was found to have an unplanned reoperation rate of 1.2%; however, these data were specific to isolated CC ligament reconstruction.24
It is important to consider some disadvantages or limitations. A recent systematic review and meta-analysis25 comparing open versus arthroscopic AC joint reconstruction demonstrated that there were no significant differences in outcomes after either approach, suggesting no superiority in the use of an open technique. Another recent systematic review and meta-analysis26 showed no significant differences in loss of reduction, complication rate, or revision rate for open versus arthroscopic AC joint reconstruction techniques; however, open procedures had significantly (P = .48) more clavicle fractures than arthroscopic repairs, and there was a significantly (P = .024) greater clavicle fracture rate with the use of tendon grafts compared with synthetic ligament grafts.
There is a paucity of literature on isolated reconstruction of the AC ligament to treat horizontal instability of the AC joint, and thus there is no gold standard for surgical management of such injuries. Our surgical technique for reconstruction of the AC ligament leads to excellent restoration of horizontal stability of the AC joint.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.J.O. reports board or committee member, American Shoulder and Elbow Surgeons, Arthroscopy Association of North America, Association of American Colleges, Southern Orthopaedic Association; paid consultant, research support, and other, DePuy, A Johnson & Johnson company, Mitek, Smith & Nephew; paid consultant, Stryker. M.K.M. reports personal fees, Arthrex; board or committee member, AAOS, American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America; editorial or governing board, ACSM Translational Journal, Ortho Info, Jackson Orthopaedic Society, The Forum; paid presenter or speaker, Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video illustrates an open technique for acromioclavicular (AC) ligament repair and allograft reconstruction with semitendinosus allograft to restore horizontal stability of the AC joint. This is a type II AC joint injury with attenuation of the AC joint ligament and capsule in a patient who failed extensive conservative treatment and had continued horizontal instability, pain, and poor shoulder function.
References
- 1.Braun S., Imhoff A.B., Martetschlaeger F. Primary fixation of acromioclavicular joint disruption. Oper Tech Sports Med. 2014;22:221–226. [Google Scholar]
- 2.Li X., Ma R., Bedi A., Dines D.M., Altchek D.W., Dines J.S. Management of acromioclavicular joint injuries. J Bone Joint Surg Am. 2014;96:73–84. doi: 10.2106/JBJS.L.00734. [DOI] [PubMed] [Google Scholar]
- 3.Martetschläger F., Tauber M., Habermeyer P., Hawi N. Arthroscopically assisted acromioclavicular and coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arthrosc Tech. 2016;5:e1239–e1246. doi: 10.1016/j.eats.2016.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dyrna F.G.E., Imhoff F.B., Voss A. The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med. 2018;46:1432–1440. doi: 10.1177/0363546518758287. [DOI] [PubMed] [Google Scholar]
- 5.Saccomanno M.F., De Ieso C., Milano G. Acromioclavicular joint instability: Anatomy, biomechanics and evaluation. Joints. 2014;2:87–92. doi: 10.11138/jts/2014.2.2.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gastaud O., Raynier J.L., Duparc F. Reliability of radiographic measurements for acromioclavicular joint separations. Orthop Traumatol Surg Res. 2015;101:S291–S295. doi: 10.1016/j.otsr.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Mazzocca A.D., Arciero R.A., Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–329. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 8.Minkus M., Hann C., Scheibel M., Kraus N. Quantification of dynamic posterior translation in modified bilateral Alexander views and correlation with clinical and radiological parameters in patients with acute acromioclavicular joint instability. Arch Orthop Trauma Surg. 2017;137:845–852. doi: 10.1007/s00402-017-2691-1. [DOI] [PubMed] [Google Scholar]
- 9.Tauber M. Management of acute acromioclavicular joint dislocations: Current concepts. Arch Orthop Trauma Surg. 2013;133:985–995. doi: 10.1007/s00402-013-1748-z. [DOI] [PubMed] [Google Scholar]
- 10.Beitzel K., Mazzocca A.D., Bak K. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30:271–278. doi: 10.1016/j.arthro.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Ulucay C., Ozler T., Akman B. Treatment of acromioclavicular joint injuries in athletes and in young active patients. J Trauma Treat. 2016;5:1000344. [Google Scholar]
- 12.Ma R., Smith P.A., Smith M.J., Sherman S.L., Flood D., Li X. Managing and recognizing complications after treatment of acromioclavicular joint repair or reconstruction. Curr Rev Musculoskel Med. 2015;8:75–82. doi: 10.1007/s12178-014-9255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beitzel K., Cote M.P., Apostolakos J. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29:387–397. doi: 10.1016/j.arthro.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Aliberti G.M., Kraeutler M.J., Trojan J.D., Mulcahey M.K. Horizontal instability of the acromioclavicular joint: A systematic review. Am J Sports Med. 2019 doi: 10.1177/0363546519831013. 363546519831013. [DOI] [PubMed] [Google Scholar]
- 15.North A.S. Rockwood grade I and II acromioclavicular injuries: As benign as commonly believed? Joints. 2016;4:171–173. doi: 10.11138/jts/2016.4.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaw M.B.K., McInerney J.J., Dias J.J., Evans P.A. Acromioclavicular joint sprains: The post-injury recovery interval. Injury. 2003;34:438–442. doi: 10.1016/s0020-1383(02)00187-0. [DOI] [PubMed] [Google Scholar]
- 17.Mouhsine E., Garofalo R., Crevoisier X., Farron A. Grade I and II acromioclavicular dislocations: Results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599–602. doi: 10.1016/s1058-2746(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 18.Cano-Martínez J.A., Nicolás-Serrano G., Bento-Gerard J., Picazo-Marín F., Andrés-Grau J. Acute high-grade acromioclavicular dislocations treated with triple button device (MINAR): Preliminary results. Injury. 2016;47:2512–2519. doi: 10.1016/j.injury.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 19.Saier T., Venjakob A.J., Minzlaff P. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: A biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1498–1505. doi: 10.1007/s00167-014-2895-7. [DOI] [PubMed] [Google Scholar]
- 20.Nüchtern J.V., Sellenschloh K., Bishop N. Biomechanical evaluation of 3 stabilization methods on acromioclavicular joint dislocations. Am J Sports Med. 2013;41:1387–1394. doi: 10.1177/0363546513484892. [DOI] [PubMed] [Google Scholar]
- 21.Tauber M., Valler D., Lichtenberg S., Magosch P., Moroder P., Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: Triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44:482–489. doi: 10.1177/0363546515615583. [DOI] [PubMed] [Google Scholar]
- 22.Beitzel K., Obopilwe E., Apostolakos J. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med. 2014;42:2141–2148. doi: 10.1177/0363546514538947. [DOI] [PubMed] [Google Scholar]
- 23.Lee S.J., Nicholas S.J., Akizuki K.H., McHugh M.P., Kremenic I.J., Ben-Avi S. Reconstruction of the coracoclavicular ligaments with tendon grafts. Am J Sports Med. 2003;31:648–654. doi: 10.1177/03635465030310050301. [DOI] [PubMed] [Google Scholar]
- 24.Moatshe G., Kruckeberg B.M., Chahla J. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: A systematic review of clinical and radiographic outcomes. Arthroscopy. 2018;34:1979–1995.e1978. doi: 10.1016/j.arthro.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 25.Hohmann E., Tetsworth K., Glatt V. Open versus arthroscopic acromioclavicular joint resection: A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2019;139:685–694. doi: 10.1007/s00402-019-03114-w. [DOI] [PubMed] [Google Scholar]
- 26.Gowd A.K., Liu J.N., Cabarcas B.C. Current concepts in the operative management of acromioclavicular dislocations: A systematic review and meta-analysis of operative techniques. Am J Sports Med. 2019;47:2475–2758. doi: 10.1177/0363546518795147. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video illustrates an open technique for acromioclavicular (AC) ligament repair and allograft reconstruction with semitendinosus allograft to restore horizontal stability of the AC joint. This is a type II AC joint injury with attenuation of the AC joint ligament and capsule in a patient who failed extensive conservative treatment and had continued horizontal instability, pain, and poor shoulder function.