Abstract
Lipids are essential components of cell structure and play important roles in signal transduction between cells and body metabolism. With the continuous development and innovation of lipidomics technology, many studies have shown that the relationship between lipids and cancer is steadily increasing, involving cancer occurrence, proliferation, migration, and apoptosis. Breast cancer has seriously affected the safety and quality of life of human beings worldwide and has become a significant public health problem in modern society, with an especially high incidence among women. Therefore, the issue has inspired scientific researchers to study the link between lipids and breast cancer. This article reviews the research progress of lipidomics, the biological characteristics of lipid molecules, and the relationship between some lipids and cancer drug resistance. Furthermore, this work summarizes the lipid molecules related to breast cancer diagnosis and prognosis, and then it clarifies their impact on the occurrence and development of breast cancer The discussion revolves around the current research hotspot long-chain non-coding RNAs (lncRNAs), summarizes and explains their impact on tumor lipid metabolism, and provides more scientific basis for future cancer research studies.
Keywords: lipids, breast cancer, lipidomics, diagnosis, prognosis, drug resistance, lncRNAs
1. Introduction
Breast cancer is a malignant disease that occurs in breast tissue. It occurs more frequently in women. It is also the second leading cause of female mortality. According to the breast cancer report updated by the American Cancer Society in 2019, the incidence of breast cancer in women increased by 0.3% annually from 2012 to 2016 [1]. In contrast, the mortality rate declined 40% from 1989 to 2017, reducing by a total of 375,900 deaths from breast cancer-related diseases. Studies have shown that this result was significantly linked with the widespread promotion of early breast cancer screening [2]. The early diagnosis and proper treatment of breast cancer through early screening is a crucial way to improve the survival rate of patients [3]. Improvements in screening and treatment have significantly reduced breast cancer mortality. Standard clinical screening techniques include mammography [4], ultrasound [5], and magnetic resonance imaging (MRI) [6]. Mammography is not very sensitive to breast tissue that contains a large number of fibrous structures. This type of tissue accounts for most of the examined cases, which causes one-third of missed diagnoses [7,8]. Ultrasound examination is a supplementary assessment to an X-ray examination. Image quality is primarily affected by the skill of the operator, and the examination results are unstable [9]. MRI detection is expensive, not suitable for large-scale early screening, and has a high false-positive rate that makes its detection result unsatisfactory [10,11]. Therefore, it is particularly important to find an early diagnosis method that is easy to operate, affordable, and suitable for detection in a large-sized population.
The evidence from many studies has confirmed that the metabolism of proliferating tumor cells is different from the cells in normal tissues [12]. The occurrence and development of tumors have specific metabolic processes, and the malignant transformation of tumor cell phenotypes mainly occurs in the lipid metabolism process [13]. Previous studies have shown that lipid molecules are closely related to the prognosis and development of diseases, e.g., prostate cancer [14], breast cancer [15], and colorectal cancer [16]. Especially in recent years, with the development of MS technology, it has become more feasible to achieve an early diagnosis for breast cancer patients [17,18], metabolic reprogramming [11,19], cancer staging [20], and a therapeutic intervention response [21]. This technology also provides convenience for obtaining lipid molecules with research value. Generally, MS and NMR spectroscopy techniques are used to identify tumor metabolites [22]. Since MS requires the use of chromatography for the preliminary separation of metabolites, it is usually combined with gas chromatography (GC) or liquid chromatography (LC) [23]. GC/LC–MS and other technologies for the metabolomics analysis of breast cancer patients’ tissues, blood, urine, and other biological tissues are important ways to discover lipid biomarkers and explore new metabolites.
In this paper, we review the literature on lipid and its metabolites in various experimental models in recent years, and then we summarize the valuable and potential lipid biomarkers to provide the basis for further study on the pathogenesis, diagnostic methods, and adverse clinical prognosis.
2. Biological Characteristics of Lipids
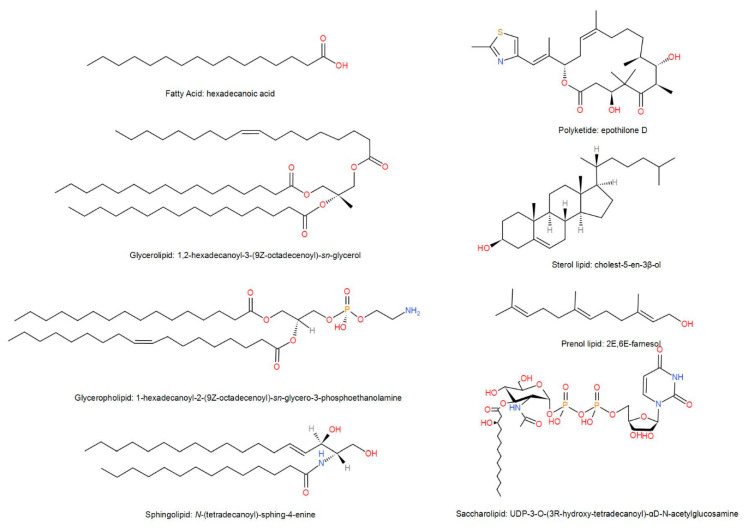
Lipids are means as small hydrophobic or amphiphilic molecules that are perhaps derived wholly or partially from the condensation of carbocation groups of thioesters and/or the condensation of carbocation groups of isoprene units [24,25]. Because lipids undergo many different biochemical changes during the biosynthesis process, their structure is more complicated than carbohydrates and proteins. Lipids form a variety of molecules through the combination of different types of building blocks, producing an extremely heterogeneous collection of molecules. In order to unify the classification and naming rules of lipid molecules, the LIPID MAPS Alliance [26] has developed a complete lipid classification system where the lipids are divided into eight categories that include fatty acids (FAs), glycerolipids (GLs), glycerophospholipids (GPs), sphingolipids (SPs), saccharolipids (SLs), polyketides (PKs), sterol lipids (STs), and prenol lipids (PRs). Due to the numerous and complex structures of lipids, we selected representative molecules from each category to represent the structure of lipids (Figure 1).
Figure 1.
Representative structure of lipids.
The chain extension of acetyl Coenzyme A (acetyl-CoA) primer and malonyl-CoA (or methyl malonyl-CoA) group synthesizes FAs. The functional groups are replaced by other atoms to form various molecular groups [27]. Some common FAs are stearic acid, soft acid, and arachidonic acid. GLs are composed of glycerol groups, and the fatty acids also include alkyl and 1Z-alkenyl variants [28]. Another lipid-containing glycerol group is that of GPs. In its molecular structure, the hydroxyl groups at the first and second positions of glycerol are replaced by FAs to form esters. The two fatty acids are nonpolar chains, so they have hydrophobic properties [29]. The hydroxyl group at position three is replaced by a phosphorus-containing group, and the third carbon atom of the phosphate group connected to a glycerol molecule is hydrophilic [30], which leads to GPs being both hydrophilic and hydrophobic. SPs take long-chain nitrogenous bases as their core structures, and they are ubiquitous in eukaryotic membranes, especially in central nervous system tissues. The in-depth study on sphingolipid metabolism and function by an SP reveals its family members, including ceramide (Cer), sphingosine (Sph), sphingosine-1-phosphate (S1P), and ceramide-1-phosphate (C1P) [31]. Unlike the definition of "glycolipids" by the International Union of Pure and Applied Chemistry (IUPAC) [32], an SL is a compound in which the fatty acyl groups are directly connected with a sugar skeleton. STs and PRs share a biosynthetic pathway through the polymerization of dimethylallyl pyrophosphate, but there are vital differences in their final structure and function. A PK is derived from the polymerization of acetyl and propionyl and belongs to the secondary metabolites of animals, plants, and microorganisms [33].
Significant changes in the lipid molecular structure have created a diversity of biological functions [34]. The complex lipid metabolism system is formed by lipid–lipid, lipid–protein, and lipid and other biomolecule interactions [35,36,37]. Lipids, as the medium of cell signal transmission, affect the metabolic behavior of tumor growth, play a role in invasion and metastasis, reshape the metabolic mechanism of cells, and transform the metabolic program from glycolysis to lipid-dependent energy supply [38]. One of the characteristics of cancer is metabolic reprogramming [39,40]. Unlike normal cells, cholesterol in cancer cells mainly exists in the inner layer, and external stimuli change the cholesterol content in the inner and outer layers. Based on this, it has been found that treating cells with a statin can reduce the cholesterol level in the inner layer of a cell membrane, leading to the inhibition of cell growth, which suggests a new method to treat cancer by regulating the cholesterol level of cells with drugs [41]. Secondly, lipids are involved in cell regulation including cell proliferation, apoptosis, and development. Comprehensive lipidomic research of breast has shown that some genes regulating the metabolism of lipids are highly expressed, suggesting that phospholipids perhaps have diagnostic function and the regulation of their metabolism can provide treatment changes for breast cancer [42].
3. Research Progress of Lipidomics
In 2003, Han and Gross and others initiated the concept of “lipidomics” [43]. Lipidomics belongs to the category of metabolomics, which is a science that studies the biological characteristics of all lipid molecules in organisms. It has an alternative subject in proteomics and genomics. The formal presentation of the concept means that the study of lipids in organisms has risen from a single level to a systematic level. Therefore, it is possible to achieve efficient and accurate lipidomics research [44].
The research content of lipid metabolomics mainly includes four parts: lipid extraction, separation, analysis and detection, and related bioinformatics analysis [45]. Because lipids are insoluble in water, organic solvents are usually used to extract lipids from biological tissues. Commonly used extractants include a methanol–chloroform mixture, methyl tert-butyl ether (MTBE) and solid phase extraction (SPE) [46,47]. The extracted lipid mixture is separated by a chromatographic adsorption method. With the improvement of this separation equipment, scientists have adopted HPLC [48] in recent years to achieve the rapid separation of lipids. However, this separation method is time-consuming, and the UV identification requires π–π * numerical conversion, which cannot achieve a strict proportional analysis with the molecular weight of lipid molecules, resulting in a great reduction in lipid detection accuracy.
High-resolution bio-mass spectrometry is the core tool of lipidomics analysis at present that can close the gap between lipid metabolism and clinical disease manifestations. There are several commonly used methods. The first is electrospray ionization mass spectrometry (ESI) [49]. ESI is a form of mass spectrometry with an electrospray ionization system that has a high sensitivity and is usually used in conjunction with liquid chromatography devices. It is suitable for the analysis of simple FAs and lipids with massive molecular weights. The second is matrix-assisted laser ionization mass spectrometry (MALDI) [50], which is suitable for the blood lipids and highly hydrophobic and nonpolar lipids, (phospholipids, for example). The third method is GC/LC–MS [51], which needs to transform lipid molecules into a gaseous state by derivatization before they can be studied. The most common application is to derivatize a lipid with methanol-forming FA methyl ester (FAME) for downstream analysis. The fourth method is nonaqueous capillary electrophoresis/mass spectrometry (NACE), which has a high separation efficiency. This technique does not require the preparation of a complicated sample, it is relatively low cost, and it is suitable for inactivated fatty acids [52] and phospholipids [53]. The fifth is MALDI imaging [54], which can be utilized to determine the spatial distribution of lipids in tissue samples; it displays the density of various lipid molecules as a heat map and retains their anatomical structures. This method is hypothesis-free and is expected to achieve a higher throughput lipid analysis [55].
Lipidomics, as a new research field, represents a new approach for diagnosis and treatment innovation in the next generation. Mass spectrometry, as a powerful analytical technique, provides convenience for lipidomics to explain disease mechanisms.
4. Lipids and Drug Resistance in Cancers
Drug action (chemotherapy, targeted drugs, and immune drugs) is an important treatment for cancer patients. However, long term use results in drug resistance that reduces the treatment’s efficacy and accelerates the progress of cancer, ultimately leading to the death of patients. Though the proper combination of anti-cancer drugs has dramatically improved the treatment of malignant tumors, drug resistance to chemotherapy often occurs, and the resistance of cancer to chemotherapy drugs remains the main clinical problem in preventing a recurrence. The ATP-binding cassette (ABC) transporter superfamily is a group of transmembrane proteins. The ABC transporter uses ATP to hydrolyze energy to transport a series of ionic compounds (carbohydrates, lipids, proteins, etc.) into the cell in the opposite direction. In addition, the ABC transporter has the ability to transport heterologous biological substances and drug-conjugated compounds. P-glycoprotein, multidrug resistance-related protein (MRP1), adenosine triphosphate binding transporter G superfamily member 2 antibody (ABCG2), mitoxantrone resistance protein (MXR), and breast cancer resistance proteins 1 (BCRP1) can help the body block the transport of drug molecules, expel anti-cancer drugs from cells, and reduce the effective concentration in cells, thus leading to acquired multidrug resistance. Drugs targeting tumor vessels have a limited effect on the survival rate of patients, which remains attributed to the patient’s resistance to anti-angiogenic drugs (AADs) [56,57]. What is even more surprising is that tumors such as breast cancer, cervical cancer, and gastric cancer growing around adipose tissue have lower benefits [56].
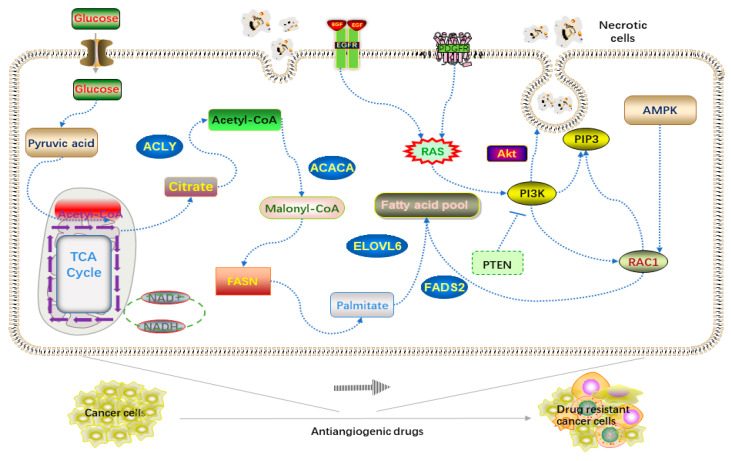
The rapid growth and expansion of a tumor depends on large angiogenesis [58]. Blood vessels provide nutrients, hormones, and sugar for cancer cells. The use of AADs reduces angiogenesis and energy supply, which leads to hypoxia in the intracellular environment, triggering fat cells to decompose and store excessive lipids, as well as causing reprogramming of lipid metabolism [38,59]. Further research has shown that the phosphorylation level of an AMP-activated protein kinase in tumor cells increases after AAD treatment, and the increase of carnitine palmitoyl transferase 1 (CTP1) activates fatty acid biosynthetic cells to provide ATP, all of which are caused by hypoxia. CTP1 is the rate-limiting enzyme of FA β-oxidation, which is the core process of fatty acid decomposition. The magical thing is that when CTP1 is knocked down, the drug resistance of hepatic cell carcinoma (HCC) is reversed by using AADs again. Therefore, CTP1 inhibitors can be used to both reduce lipid decomposition and reduce energy support for tumors. Moreover, another energy supply method called the giant cell drinking process has been found to be resistant to drug action [60]. Macrophages take up necessary biological materials from dead tumor cell fragments through endocytosis. Amino acids, sugars, and lipids can be reused to maintain their own expansion. Blocking the process of endocytosis can restore the drug sensitivity of cancer cells. Thus, in many cancer types, the Ras pathway activates downstream effector by stimulating platelet-derived growth factor receptor (PDGFR) and epidermal growth factor receptor (EGFR) [61], e.g., phosphatidylinositol 3-kinase (PI3K), inositol triphosphate (PIP3), and Rac1. PI3K regulates the actin cytoskeleton through Rac1 and promotes the closure of a large body through phosphoinositide signal [62]. The phagocytized necrotic cells are decomposed and metabolized to provide energy for tumor cell proliferation (Figure 2) [38,58,59,60,61,62].
Figure 2.
Mechanism of drug resistance of tumor cells induced by anti-angiogenic drugs (AADs).
It is widely known that the reduction of glycoproteins and the increase of alpha-fetoproteins and carcinoembryonic antigens on the surface of cancer cells also promote the spread and metastasis of tumor cells. However, the role of lipid molecules in tumor drug resistance is often neglected. In fact, lipid metabolism plays an essential role in regulating tumor sensitivity to anticancer drugs. However, it should be noted that whether it is a CTP1 inhibitor or a macrosomia blocker, it may not be sufficient for cancer treatment alone because this release may not eliminate malignant cells. Clinically, the combination of a cell inhibitor, targeted therapy, and a lipid metabolism inhibitor is more effective in treating cancer [59]. This new mechanism of tumor drug resistance will provide exciting opportunities for the development of new therapies for lipid metabolism in the future.
5. Role of Lipid in the Diagnosis of Breast Cancer
Lipids widely exist in human blood, urine, hair, and other tissues with convenient accessibility. Therefore, there have been many valuable lipid molecular screening experiments using lipidomics technology. Experiments have shown that a lipid is a useful biomarker for cancer diagnosis [63,64], especially in breast cancer. Therefore, the authors of this paper summarize the lipid molecules with diagnostic potential related to breast cancer in patients (Table 1) [11,42,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80].
Table 1.
Lipids with the ability of early diagnosis in breast cancer.
| Diagnosis Biomarker | Sample Type | Lipidomics Technique | Reference |
|---|---|---|---|
| PCs, ePC (38:3) and ePC (32:2), PC ae C42:5 and PC aa C42:2 | Urine, Plasma, Tissue | nLC-ESI-MS-MS, ESI-MS/MS, UPLC-MS | [11,42,65,66] |
| PC (32:1), (34:4), (38:3), (40:5), (40:3), (44:11) | Plasma, Tissue | ESI-MS/MS, MALDI-IMS | [11,67] |
| PC (30:0), (34:0), (34:1), (36:0), (36:1), (36:2), (38:4), (40:6), (42:6) | Tissue | MALDI-IMS, probe electrospray ionization-MS | [67,68] |
| PC (20:2/20:5) and PC (20:0/24:1;) | Plasma | UPLC-quadrupole time-of-flight tandem/MS | [69] |
| LPC (18:0), (18:3), (20:0), (20:1), (20:2) and a C (16:0) | Plasma, Urine, Tissue | ESI-MS/MS, MALDI-IMS, nLC-ESI-MS-MS |
[11,65,67] |
| PEs and PE (15:0/19:1) | Plasma, Tissue, Urine | UPLC-quadrupole time-of-flight tandem/MS, HILIC-HPLC/ ESI-MS, nLC-ESI-MS-MS |
[66,69,70] |
| Triglyceride, Triglyceride (12:0/14:1) | Plasma | UPLC-quadrupole time-of-flight tandem/MS | [69,71,72,73] |
| Diglyceride (18:1/18:2) | Plasma | UPLC-quadrupole time-of-flight tandem/MS | [69] |
| C19:0 CE, C19:1 CE, C19:2 CE | Plasma | ESI-MS/MS | [11] |
| PI (16L:0/16:1) and PI (18:0/20:4) | Plasma | normal-phase/reversed-phase two-dimensional LC-MS | [74] |
| Docosahexaenoic acid | Plasma, Tissue | LC-MS, Raman spectroscopy | [75,76] |
| Fatty acids: C14:0, C16:0, C16:1, C18:0, C18:3, C18:2, C20:4, and C22:6 | Serum | Chip-based direct-infusion nano-electrospray ionization-Fourier transform ion cyclotron resonance mass spectrometry, GC–MS | [76,77,78] |
| HDL-C, VLDL-C, LDL-C, TC | Plasma | NA | [72,79,80] |
| N-palmitoyl proline | Plasma | UPLC-quadrupole time-of-flight tandem/MS | [69] |
PC: phosphatidylcholine; ePC: ether-linked phosphatidylcholine; LPC: lysophosphatidylcholine; PE: phosphatidylethanolamine; CE: cholesteryl esters; PI: phosphatidylinositol; NA: not applicable; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; VLDL-C: very low-density lipoprotein cholesterol; TC: total cholesterol; UPLC: ultra-HPLC; IMS: imaging mass spectrometry; HILIC: hydrophilic interaction liquid chromatography.
In some studies, changes of phospholipids in plasma, serum [74,81], and urine [66,82] of breast cancer patients have been reported. For example, compared with normal tissues, the content of linoleic acid in patients’ tissues is higher. In contrast, the content of oleic and stearic acid is lower [11], especially in tertiary and estrogen receptor (ER)-negative breast cancer [25]. Under the action of the desaturase system, monounsaturated fatty acids introduce unsaturated bonds at precise positions in the fatty chain to form a bend, which changes the biophysical properties of the molecule [83]. The occurrence of tumor cells depends on the fluidity, functionality, and flexibility of monounsaturated fatty acids, which also involves the action of stearoyl-CoA desaturase (SCD-1). Studies have shown that most of the monounsaturated fatty acids in fat are in the form of oleic acid, which is completely obtained through endogenous processes, and the long-term large-scale intake of cis-monounsaturated oleic acid can reduce the risk of breast cancer [84,85]. Linoleic acid is a significant breast cancer cell-stimulating factor. Another finding from population diet control experiments is that linoleic acid has anti-cancer effects [27]. Docosahexaenoic acid (DHA) [75] also has anti-cancer functions. DHA inhibits the growth of breast cancer cells and increases apoptosis [86,87,88]. It induces apoptosis through lipid peroxidation by increasing the level of reactive oxygen species (ROS) and activating the caspase pathway [89]. Lipids such as phosphocholine, choline, and glycerophosphocholine in tumors will also increase, and non-invasive detection by magnetic resonance spectroscopy can be used to separate benign and malignant tumors [90]. Phosphatidylcholine (PC) (32:1) can be used as a diagnostic substance for benign and malignant breast tissue [74], as well as a prognostic marker for triple-negative breast cancer [91]. Serum-free fatty acids (FFAs) are important biologically active molecules. In vitro culture experiments have shown that FFAs have an anti-proliferative effect on breast cancer cells [92]. Chen et al. found that the combination of 15 lipid compounds can be used as both plasma biomarkers to distinguish early cancer and benign lesions and for an auxiliary and mammography examination to avoid the unnecessary follow-up of an incredibly invasive biopsy [11]. Park et al. reported that the four candidate markers (L-octanoylcarnitine, 5-oxoproline, hypoxanthine, and docosahexaenoic acid) found in the plasma of patients can effectively distinguish healthy subjects from malignant breast tumors, and it is expected to reach an early stage by only collecting blood samples [75]. Li et al. found that blood lipids in breast cancer patients after chemotherapy will increase. However, it should be noted that plasma contains a variety of lipoprotein libraries, and each lipoprotein constitutes thousands of different types according to different dietary sources [21]. For example, Meikle et al. pointed out that many phospholipids related to breast cancer have changed after eating soybeans and dairy products [93]. Therefore, when trying to determine the link between blood lipids, breast cancer, and other diseases, it is necessary to consider the impact of dietary intake on the disease.
Changes in the concentration of lipid metabolites reflect changes in the disease state. Monitoring the fluctuations of metabolites in organisms is an innovation in the early detection of breast cancer, but it is still in its infancy. Both the separation and analysis of metabolites require more mature technical and theoretical support. While researching lipid markers, we must also develop new and more valuable lipid molecules to detect early breast cancer.
6. Effects of Lipid Metabolism on Proliferation, Migration, and Apoptosis in Breast Cancer
The metabolism of most tumor cells differs from that of healthy cells. In cancer cells, in addition to changes in glucose metabolism, lipid metabolism also undergoes adaptive changes [94,95]. During the rapid proliferation of malignant cells, excess lipids are needed to synthesize biofilms, organelles, and important signal molecules [96,97]. The sources of lipids in the human body include dietary intake and the de novo synthesis of liver cells. The supply of lipids is essential for cell growth, but changes in epigenetics and the local microenvironment of tumors can cause disorders of lipid metabolism and activate cholesterol synthesis [39]. The lipid biosynthesis process can not only provide a large number of necessary bio-membrane components for the rapid division and proliferation of tumor cells but also promote the development of cancer by synthesizing a series of sphingomyelin, phosphatidylinositol, and other oxide signaling molecules [98].
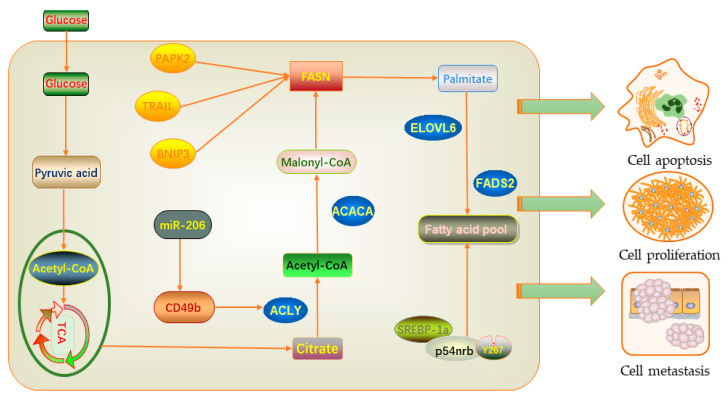
The conserved nuclear protein 54 kD Nuclear RNA-and DNA-binding protein (p54nrb) plays a role in RNA splicing and editing, DNA repair, and gene transcription [99]. These functions are essential for maintaining normal cell growth. When the protein structure is lost or changed, it may lead to the development of cancer [100]. Sterol regulatory element-binding proteins (SREBPs) can activate key enzymes in fatty acid and cholesterol biosynthesis, such as fatty acid synthase (FASN), citrate lyase (ACLY), and acetyl-CoA carboxylase 1 (ACC1). [101]. Some studies have shown that tumor cells can activate the de novo synthesis of fatty acids, which mainly depends on the SREBP transcription factor to increase the expression of adipogenic genes [102]. After experiments, it was determined that p54nrb is a new interacting protein of SREBP-1a [103]. SREBP-1a binds to p54nrb through residue Y267 to control target gene expression and lipid synthesis in breast cancer cells. In the process of fatty acid synthesis, various enzymes play a critical regulatory role. Since the discovery of FASN, its role in tumor growth and intracellular signal transmission has been extensively studied. Further studies have found that the use of FASN drug inhibitors can cause breast cancer cells to undergo apoptosis or tumor cell shrinkage, which indicates that FASN has a protective effect on breast cancer cells [104,105,106]. The reason for this is that the inhibition of fatty acid synthase leads to the aggregation of malonyl-CoA, which increases the expression of ceramide. It induces the pro-apoptotic gene bcl-2 and adenovirus E1B 19 kDa-interacting protein 3 (BNIP3), tumor necrosis factor-related apoptosis-inducing ligand (TRAIL), and death-related protein kinase 2 (DAPK2), thus significantly up-regulating and promoting cell apoptosis [105]. In addition, ACLY plays an important role in fatty acid biosynthesis and is the main enzyme-producing acetyl-CoA. A study has shown that microRNA-206 can encode the cell membrane surface integrin receptor CD49b, which acts on ACLY to cause breast cancer cell metastasis [107] (Figure 3).
Figure 3.
Lipid-related regulatory factors promoting the occurrence and development of breast cancer.
In addition, the development and metastasis of cancer are also closely related to the imbalance of the body’s redox balance [108]. This imbalance has been shown to be caused by an increase in free radicals (mainly ROS) [109]. ROS are a byproduct produced during aerobic metabolism [110]. They react with polyunsaturated fatty acids in biomembrane phospholipids to trigger lipid peroxidation and generate a series of complex products such as oxygen free radicals under peroxidation conditions. Many studies have shown that lipid peroxidation products may be involved in inducing cell apoptosis [111] because lipid peroxidation mainly acts on biological membranes and mitochondria-containing DNA. As the engine of the body, mitochondria participate in the physiological process of diseases such as aging, new blood vessels, and cancer. Its damage has a significant impact on the organism [112]. In addition, the role of ROS in tumorigenesis and development is also complicated [113], triggering various effects at different concentrations. On the one hand, accumulated ROS can cause irreversible oxidative damage to lipids, proteins, and DNA, and they can activate the ROS-mediated NF-κB pathway to cause chronic inflammation [31,114]; on the other hand, it can regulate intracellular ROS level to kill tumor cells. ROS open the mitochondrial permeability transition pore (PTP), increases the permeability of the inner membrane, interferes with the mitochondrial membrane potential, and induces the release of cytochrome c. Cytochrome c, apoptosis protease activator 1, and caspase 9 form an "apoptotic body" that initiates changes in the downstream process of the apoptosis cascade [109,115]. Therefore, targeted research on the dual effects of ROS is a potential direction for the treatment of malignant tumors.
7. Lipids as Predictors of Breast Cancer Risk and Prognosis
For breast cancer patients, lymph node status is the most accurate and important survival predictor. In addition, tumor size, the degree of differentiation, and histological type can also be used as prognostic factors. With the in-depth study of lipid molecules, people have discovered changes in lipid levels in the prognosis of different types of cancer. This abnormal change is associated with the survival risk of a variety of cancers, including breast cancer [116,117,118]. The negative correlation between lipid levels and the poor prognosis of cancer seems to be due to tumor type and the characteristics and pathophysiological effects of lipid molecules.
Triglycerides (TGs) and cholesterol (CHO) play important functions in biofilm composition and energy storage; 27-hydroxycholesterol (27HC) is the main metabolite of high cholesterol and is also a ligand for the estrogen receptor and liver X receptor (LXR) [119]. It is composed of sterol 27 hydroxylase (CYP27A1) and cytochrome P450 oxidase. Compared with normal tissues, the expression of 27HC in malignant breast tissues is significantly higher, and the increase of synthase CYP27A1 can improve the tumor grade [120]. When the production of CYP27A1 is cut off, it can significantly reduce the distant metastasis of tumor cell-related models [121]. 27HC can regulate the activity of estrogen receptor alpha (ERα)-positive breast cancer and directly act on immune cells to affect tumor growth and metastasis [122]. In addition, estrogen produced by adipose tissue also increases the risk of ERα-positive breast cancer. A number of epidemiological investigations and studies have found that the estrogen and progesterone levels of postmenopausal women increase the incidence and mortality of breast cancer [123,124]. A retrospective investigation on the relationship between blood lipid levels and breast cancer in patients found that low preoperative TG and high-density lipoprotein cholesterol (HDL-C) levels are risk factors. They may be independent predictors in the prognosis of breast cancer [125]. It is hypothesized that TGs cause a decrease in the sex hormone binding globulin and an increase in free estradiol, thereby increasing the risk of breast cancer recurrence. Nevertheless, another study showed that after excluding the confounding effects of insulin and body mass index, there was a failure to prove that blood lipids (TG and low-density lipoprotein cholesterol (LDL-C)) levels and breast cancer prognosis have any statistically significant correlation [126]. Blood lipid levels are potentially affected by menopausal status and fat intake. HDL-C can prevent lipid peroxidation by inhibiting the oxidative damage produced by LDL-C [127]. HDL-C is related to the incidence of breast cancer in postmenopausal women and is regarded as a marker of androgenic status [128]. When the body ingests a large amount of fat for a short time, it stimulates the increase of circulating estrogen, causing cell damage and affecting the growth of cancer cells. A Mendelian randomized grouping experiment proved that genetically elevated LDL-C due to proprotein convertase subtilisin/kexin type 9 (PCSK9) gene mutations could increase the incidence of estrogen receptor-positive breast cancer. The use of statins to target and repair mutant genes resulted in a finding that the mutation effect is not apparent [129].
Triple-negative breast cancer (TNBC) is one of the subtypes of breast cancer with a high risk of early recurrence and a low survival rate. A study found that the content of PC (32:1) in recurrent TNBC was significantly higher than that in non-recurrent TNBC. Compared with estrogen receptor-positive and human epidermal growthfactor receptor 2 (HER2) breast cancer, TNBC contained more PC (32:1) and PC (30:0) [130], suggesting the potential of phospholipids as candidate predictors [42,91]. In addition, PC is also considered to be a lipid metabolite that promotes cancer metastasis and malignant transformation [131]. On the other hand, dyslipidemia caused by high-fat diet and obesity can increase women’s risk of disease and adversely affect the prognosis of breast cancer patients [132,133]. An exogenous diet consumes much fat. Breast cancer cells absorb fat particles floating in the blood to promote their proliferation. This is an unexpected fat particle absorption mechanism that recently discovered and that revealed the connection between cancer cells and dietary fat [134]. Lipid metabolism is interfered by both exogenous and endogenous processes, and the mechanism of influence on breast cancer risk and prognosis is still unclear, so further prospective studies and experimental proof are needed.
8. LncRNA Related to Lipid Metabolism in Cancer
Long-chain non-coding RNAs (lncRNAs) have shown immeasurable potential value as a hotspot in molecular research, especially in the rapid development of tumor metabolic reprogramming. Some studies have shown that lncRNA can affect cancer migration, invasion, and other pathological processes [135].
lncRNAs are defined as transcripts of more than 200 nucleotides in length without a coding ability [136]. LncRNAs can participate in the regulation of a variety of lipid metabolism-related genes. Hepatocellular carcinoma up-regulated long non-coding RNA (HULC) [137,138] was the first reported liver-specific lncRNA that is highly expressed in liver cancer. HULC induces methylation at the CpG site at the miR-9 promoter. The methylation level of miR-9-1 is highly correlated with the increased risk of recurrence, resulting in a significantly shorter survival time for clear cell renal cell carcinoma [139]. HULC has been found to eliminate the miR-9-mediated inactivation of the transcription factor PPARA (proliferator-activated receptor alpha), up-regulated the same transcription factor [140,141], and activated liver cancer cell Acyl-CoA synthetase long-chain1 (ACSL1) [142,143], which promotes the expression of triglycerides and cholesterol accumulation in cells. According to reports, long non-coding hepatitis C virus (HCV) regulated 1 (lncHR1) is involved in tumor lipid metabolism, and the expression of SREBP-1c has been maintained by regulating the phosphorylation level of PDK1 upstream of AKT. SREBP-1c is an important regulator that regulates the dynamic balance of lipid metabolism and encodes the transcription of a variety of enzymes related to the synthesis of TG and FA to accelerate lipid synthesis. In addition, lncRNA related to cervical cancer lymph node metastasis promotes fatty acid metabolism reprogramming by regulating fatty acid binding protein 5 (FABP5) and promoting cervical cancer lymph node metastasis [144] (Table 2).
Table 2.
Long-chain non-coding RNAs (lncRNAs) related to lipid metabolism in cancer.
| LncRNAs | Lipid Metabolism-Related Genes | Cancer Types | Influences | References |
|---|---|---|---|---|
| HC | hnRNPA2B1 | Hepatic carcinoma | TG and CHO decreased | [145] |
| HAGLROS | FASN, ACC, SCD1, CPT1, SREBP1, PPARγ | Intrahepatic cholangiocarcinoma |
Promote autophagy, improving lipid metabolism reprogramming |
[146] |
| MACC1-AS1 | ACS, CPT1A | Gastric cancer | Drug resistance | [147] |
| HULC | ACSL1, PPARA | Hepatic carcinoma | TG and CHO accumulated | [148] |
| LNMICC | FABP5 | Cervical cancer | Lymph node metastasis | [149] |
| LeXis | RALY | Hepatic carcinoma | CHO increased | [150] |
| HR1 | SREBP-1c, FASN | Hepatic carcinoma | TG and lipid droplet accumulated | [151] |
| HCP5 | CPT1 | Gastric cancer | Drug resistance | [152] |
| MALAT1 | SREBP-1c | Hepatic carcinoma | Hepatic steatosis and insulin resistance | [153] |
ACC: acetyl-CoA carboxylase; SCD1: stearoyl-CoA desaturase1; CPT1: carnitine palmitoyl transferase 1; ACS: acetyl-coenzyme A synthetase; RALY: heterogeneous ribonucleoprotein; CHO: cholesterol; TG: triglyceride; PPARA: proliferator-activated receptor alpha; FASN: fatty acid synthase; HULC: hepatocellular carcinoma up-regulated long non-coding RNA; SREBP: Sterol regulatory element-binding protein; FABP: fatty acid binding protein 5.
In short, lncRNAs participate in lipid metabolism in different ways to affect tumor progression. We have explored the effect of lncRNAs on lipid metabolism and understand the mechanism of tumor carcinogenesis. These all provide new ideas and strategies for tumor treatment.
9. Conclusions
Lipids play an important role in the occurrence and development of cancer. They transmit information through communication between cells, regulate cell metabolism, and maintain an internal stable state. Studies have shown that lipid molecules are potential biomarkers for biological diagnosis. Combined with mass spectrometry as an auxiliary detection tool for mammography, they are expected to realize non-invasive early screening of breast cancer. In addition, with the continuous development of lipidomics technology, combining lipidomics with other omics technologies can give full play to the role of lipidomics in understanding the molecular mechanisms of disease. Though there have been many studies on the relationship between lipids and various diseases at home and abroad, there have been few studies on how lipids and their metabolism are involved in the occurrence and development of breast cancer. This is caused by both the structural diversity of lipid types and the immaturity of separation technology, which are challenges that need to be overcome in lipidomics research. Therefore, it is necessary to combine the existing biological analysis technology and emerging interdisciplinary theory to make a breakthrough in the research of lipidomics.
Author Contributions
Content design, R.G., Y.C., H.B., M.J., M.N., M.H. and Y.D.; literature collection, R.G. and Y.C.; arrangement, R.G.; Figures and Tables, R.G. and Y.C.; writing-original draft, R.G.; writing—review and editing, R.G., Y.C., H.B., M.J., M.N., M.H. and Y.D.; writing—proofreading, H.B.; funding, Y.D. and M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This project was supported by a NIH grant (5R01CA230514) to Youping Deng. This work was also supported by the NIH Grants 5P30GM114737, P20GM103466, U54MD007584 and 2U54MD007601. This was also sponsored by the first-class discipline construction fund of the School of Public Health of Guangxi Medical University.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.DeSantis C.E., Ma J., Gaudet M.M., Newman L.A., Miller K.D., Goding Sauer A., Jemal A., Siegel R.L. Breast cancer statistics, 2019. CA Cancer J. Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 2.Paci E., Broeders M., Hofvind S., Puliti D., Duffy S.W., Group E.W. European breast cancer service screening outcomes: A first balance sheet of the benefits and harms. Cancer Epidemiol. Biomark. Prev. 2014;23:1159–1163. doi: 10.1158/1055-9965.EPI-13-0320. [DOI] [PubMed] [Google Scholar]
- 3.McGuire S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv. Nutr. 2016;7:418–419. doi: 10.3945/an.116.012211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pisano E.D., Gatsonis C., Hendrick E., Yaffe M., Baum J.K., Acharyya S., Conant E.F., Fajardo L.L., Bassett L., D’Orsi C., et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N. Engl. J. Med. 2005;353:1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 5.Zhi H., Xiao X.Y., Yang H.Y., Ou B., Wen Y.L., Luo B.M. Ultrasonic elastography in breast cancer diagnosis: Strain ratio vs 5-point scale. Acad. Radiol. 2010;17:1227–1233. doi: 10.1016/j.acra.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Lehman C.D., Gatsonis C., Kuhl C.K., Hendrick R.E., Pisano E.D., Hanna L., Peacock S., Smazal S.F., Maki D.D., Julian T.B., et al. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N. Engl. J. Med. 2007;356:1295–1303. doi: 10.1056/NEJMoa065447. [DOI] [PubMed] [Google Scholar]
- 7.Sechopoulos I., Teuwen J., Mann R. Artificial intelligence for breast cancer detection in mammography and digital breast tomosynthesis: State of the art. Semin. Cancer Biol. 2020 doi: 10.1016/j.semcancer.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Birdwell R.L., Ikeda D.M., O’Shaughnessy K.F., Sickles E.A. Mammographic characteristics of 115 missed cancers later detected with screening mammography and the potential utility of computer-aided detection. Radiology. 2001;219:192–202. doi: 10.1148/radiology.219.1.r01ap16192. [DOI] [PubMed] [Google Scholar]
- 9.Rotten D., Levaillant J.M. The value of ultrasonic examination to detect and diagnose breast carcinomas. Analysis of the results obtained in 125 tumors using radiographic and ultrasound mammography. Ultrasound Obstet. Gynecol. 1992;2:203–214. doi: 10.1046/j.1469-0705.1992.02030203.x. [DOI] [PubMed] [Google Scholar]
- 10.Olsen O., Gotzsche P.C. Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 2001 doi: 10.1002/14651858.CD001877. [DOI] [PubMed] [Google Scholar]
- 11.Chen X., Chen H., Dai M., Ai J., Li Y., Mahon B., Dai S., Deng Y. Plasma lipidomics profiling identified lipid biomarkers in distinguishing early-stage breast cancer from benign lesions. Oncotarget. 2016;7:36622–36631. doi: 10.18632/oncotarget.9124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menendez J.A., Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat. Rev. Cancer. 2007;7:763–777. doi: 10.1038/nrc2222. [DOI] [PubMed] [Google Scholar]
- 14.Li J., Ren S., Piao H.L., Wang F., Yin P., Xu C., Lu X., Ye G., Shao Y., Yan M., et al. Integration of lipidomics and transcriptomics unravels aberrant lipid metabolism and defines cholesteryl oleate as potential biomarker of prostate cancer. Sci. Rep. 2016;6:20984. doi: 10.1038/srep20984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merdad A., Karim S., Schulten H.J., Jayapal M., Dallol A., Buhmeida A., Al-Thubaity F., Gari I.M., Chaudhary A.G., Abuzenadah A.M., et al. Transcriptomics profiling study of breast cancer from Kingdom of Saudi Arabia revealed altered expression of Adiponectin and Fatty Acid Binding Protein4: Is lipid metabolism associated with breast cancer? BMC Genom. 2015;16(Suppl. S1):S11. doi: 10.1186/1471-2164-16-S1-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christensen L.L., True K., Hamilton M.P., Nielsen M.M., Damas N.D., Damgaard C.K., Ongen H., Dermitzakis E., Bramsen J.B., Pedersen J.S., et al. SNHG16 is regulated by the Wnt pathway in colorectal cancer and affects genes involved in lipid metabolism. Mol. Oncol. 2016;10:1266–1282. doi: 10.1016/j.molonc.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jasbi P., Wang D., Cheng S.L., Fei Q., Cui J.Y., Liu L., Wei Y., Raftery D., Gu H. Breast cancer detection using targeted plasma metabolomics. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2019;1105:26–37. doi: 10.1016/j.jchromb.2018.11.029. [DOI] [PubMed] [Google Scholar]
- 18.Huang M., Li H.Y., Liao H.W., Lin C.H., Wang C.Y., Kuo W.H., Kuo C.H. Using post-column infused internal standard assisted quantitative metabolomics for establishing prediction models for breast cancer detection. Rapid Commun. Mass Spectrom. 2020;34(Suppl. S1):e8581. doi: 10.1002/rcm.8581. [DOI] [PubMed] [Google Scholar]
- 19.Yamashita A., Hayashi Y., Nemoto-Sasaki Y., Ito M., Oka S., Tanikawa T., Waku K., Sugiura T. Acyltransferases and transacylases that determine the fatty acid composition of glycerolipids and the metabolism of bioactive lipid mediators in mammalian cells and model organisms. Prog. Lipid Res. 2014;53:18–81. doi: 10.1016/j.plipres.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Li L., Zheng X., Zhou Q., Villanueva N., Nian W., Liu X., Huan T. Metabolomics-Based Discovery of Molecular Signatures for Triple Negative Breast Cancer in Asian Female Population. Sci. Rep. 2020;10:370. doi: 10.1038/s41598-019-57068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X., Liu Z.L., Wu Y.T., Wu H., Dai W., Arshad B., Xu Z., Li H., Wu K.N., Kong L.Q. Status of lipid and lipoprotein in female breast cancer patients at initial diagnosis and during chemotherapy. Lipids Health Dis. 2018;17:91. doi: 10.1186/s12944-018-0745-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J., Bowers J., Liu L., Wei S., Gowda G.A., Hammoud Z., Raftery D. Esophageal cancer metabolite biomarkers detected by LC-MS and NMR methods. PLoS ONE. 2012;7:e30181. doi: 10.1371/journal.pone.0030181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunther U.L. Metabolomics Biomarkers for Breast Cancer. Pathobiology. 2015;82:153–165. doi: 10.1159/000430844. [DOI] [PubMed] [Google Scholar]
- 24.Fahy E., Cotter D., Sud M., Subramaniam S. Lipid classification, structures and tools. Biochim. Biophys. Acta. 2011;1811:637–647. doi: 10.1016/j.bbalip.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fahy E., Subramaniam S., Brown H.A., Glass C.K., Merrill A.H., Jr., Murphy R.C., Raetz C.R., Russell D.W., Seyama Y., Shaw W., et al. A comprehensive classification system for lipids. J. Lipid Res. 2005;46:839–861. doi: 10.1194/jlr.E400004-JLR200. [DOI] [PubMed] [Google Scholar]
- 26.Fahy E., Subramaniam S., Murphy R.C., Nishijima M., Raetz C.R., Shimizu T., Spener F., van Meer G., Wakelam M.J., Dennis E.A. Update of the LIPID MAPS comprehensive classification system for lipids. J. Lipid Res. 2009;50:S9–S14. doi: 10.1194/jlr.R800095-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aro A., Mannisto S., Salminen I., Ovaskainen M.L., Kataja V., Uusitupa M. Inverse association between dietary and serum conjugated linoleic acid and risk of breast cancer in postmenopausal women. Nutr. Cancer. 2000;38:151–157. doi: 10.1207/S15327914NC382_2. [DOI] [PubMed] [Google Scholar]
- 28.Lands W.E., Hart P. The control of fatty acid composition in glycerolipids. J. Am. Oil Chem. Soc. 1966;43:290–295. doi: 10.1007/BF02609676. [DOI] [PubMed] [Google Scholar]
- 29.Sankaram M.B., Thompson T.E. Interaction of cholesterol with various glycerophospholipids and sphingomyelin. Biochemistry. 1990;29:10670–10675. doi: 10.1021/bi00499a014. [DOI] [PubMed] [Google Scholar]
- 30.Montealegre C., Verardo V., Luisa Marina M., Caboni M.F. Analysis of glycerophospho- and sphingolipids by CE. Electrophoresis. 2014;35:779–792. doi: 10.1002/elps.201300534. [DOI] [PubMed] [Google Scholar]
- 31.Bartke N., Hannun Y.A. Bioactive sphingolipids: Metabolism and function. J. Lipid Res. 2009;50:S91–S96. doi: 10.1194/jlr.R800080-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chester M.A. IUPAC-IUB Joint Commission on Biochemical Nomenclature (JCBN). Nomenclature of glycolipids--recommendations 1997. Eur. J. Biochem. 1998;257:293–298. doi: 10.1046/j.1432-1327.1998.2570293.x. [DOI] [PubMed] [Google Scholar]
- 33.McDaniel R., Ebert-Khosla S., Hopwood D.A., Khosla C. Engineered biosynthesis of novel polyketides. Science. 1993;262:1546–1550. doi: 10.1126/science.8248802. [DOI] [PubMed] [Google Scholar]
- 34.Tsui-Pierchala B.A., Encinas M., Milbrandt J., Johnson E.M. Lipid rafts in neuronal signaling and function. Trends Neurosci. 2002;25:412–417. doi: 10.1016/S0166-2236(02)02215-4. [DOI] [PubMed] [Google Scholar]
- 35.Wenk M.R., De Camilli P. Protein-lipid interactions and phosphoinositide metabolism in membrane traffic: Insights from vesicle recycling in nerve terminals. Proc. Natl. Acad. Sci. USA. 2004;101:8262–8269. doi: 10.1073/pnas.0401874101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heringdorf D.M.Z., Jakobs K.H. Lysophospholipid receptors: Signalling, pharmacology and regulation by lysophospholipid metabolism. Biochim. Biophys. Acta. 2007;1768:923–940. doi: 10.1016/j.bbamem.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 37.Brinkmann V. Sphingosine 1-phosphate receptors in health and disease: Mechanistic insights from gene deletion studies and reverse pharmacology. Pharmacol. Ther. 2007;115:84–105. doi: 10.1016/j.pharmthera.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Beloribi-Djefaflia S., Vasseur S., Guillaumond F. Lipid metabolic reprogramming in cancer cells. Oncogenesis. 2016;5:e189. doi: 10.1038/oncsis.2015.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 40.Gandhi N., Das G. Metabolic Reprogramming in Breast Cancer and Its Therapeutic Implications. Cells. 2019;8:89. doi: 10.3390/cells8020089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu S.L., Sheng R., Jung J.H., Wang L., Stec E., O’Connor M.J., Song S., Bikkavilli R.K., Winn R.A., Lee D., et al. Orthogonal lipid sensors identify transbilayer asymmetry of plasma membrane cholesterol. Nat. Chem. Biol. 2017;13:268–274. doi: 10.1038/nchembio.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hilvo M., Denkert C., Lehtinen L., Muller B., Brockmoller S., Seppanen-Laakso T., Budczies J., Bucher E., Yetukuri L., Castillo S., et al. Novel theranostic opportunities offered by characterization of altered membrane lipid metabolism in breast cancer progression. Cancer Res. 2011;71:3236–3245. doi: 10.1158/0008-5472.CAN-10-3894. [DOI] [PubMed] [Google Scholar]
- 43.Han X., Gross R.W. Global analyses of cellular lipidomes directly from crude extracts of biological samples by ESI mass spectrometry: A bridge to lipidomics. J. Lipid Res. 2003;44:1071–1079. doi: 10.1194/jlr.R300004-JLR200. [DOI] [PubMed] [Google Scholar]
- 44.Wenk M.R. The emerging field of lipidomics. Nat. Rev. Drug Discov. 2005;4:594–610. doi: 10.1038/nrd1776. [DOI] [PubMed] [Google Scholar]
- 45.Myers V.H., Champagne C.M. Nutritional effects on blood pressure. Curr. Opin. Lipidol. 2007;18:20–24. doi: 10.1097/MOL.0b013e328012d911. [DOI] [PubMed] [Google Scholar]
- 46.Matyash V., Liebisch G., Kurzchalia T.V., Shevchenko A., Schwudke D. Lipid extraction by methyl-tert-butyl ether for high-throughput lipidomics. J. Lipid Res. 2008;49:1137–1146. doi: 10.1194/jlr.D700041-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruiz-Gutiérrez V., Pérez-Camino M.C. Update on solid-phase extraction for the analysis of lipid classes and related compounds. J. Chromatogr. A. 2000;885:321–341. doi: 10.1016/S0021-9673(00)00181-3. [DOI] [PubMed] [Google Scholar]
- 48.Puranik M., Bhawsar D.V., Rathi P., Yeole P.G. Simultaneous Determination of Ofloxacin and Ornidazole in Solid Dosage Form by RP-HPLC and HPTLC Techniques. Indian J. Pharm. Sci. 2010;72:513–517. doi: 10.4103/0250-474X.73937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taamalli A., Arraez-Roman D., Barrajon-Catalan E., Ruiz-Torres V., Perez-Sanchez A., Herrero M., Ibanez E., Micol V., Zarrouk M., Segura-Carretero A., et al. Use of advanced techniques for the extraction of phenolic compounds from Tunisian olive leaves: Phenolic composition and cytotoxicity against human breast cancer cells. Food Chem. Toxicol. 2012;50:1817–1825. doi: 10.1016/j.fct.2012.02.090. [DOI] [PubMed] [Google Scholar]
- 50.Rauser S., Marquardt C., Balluff B., Deininger S.O., Albers C., Belau E., Hartmer R., Suckau D., Specht K., Ebert M.P., et al. Classification of HER2 receptor status in breast cancer tissues by MALDI imaging mass spectrometry. J. Proteome Res. 2010;9:1854–1863. doi: 10.1021/pr901008d. [DOI] [PubMed] [Google Scholar]
- 51.Lubes G., Goodarzi M. GC-MS based metabolomics used for the identification of cancer volatile organic compounds as biomarkers. J. Pharm. Biomed. Anal. 2018;147:313–322. doi: 10.1016/j.jpba.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 52.Azab S., Ly R., Britz-McKibbin P. Robust Method for High-Throughput Screening of Fatty Acids by Multisegment Injection-Nonaqueous Capillary Electrophoresis-Mass Spectrometry with Stringent Quality Control. Anal. Chem. 2019;91:2329–2336. doi: 10.1021/acs.analchem.8b05054. [DOI] [PubMed] [Google Scholar]
- 53.Gao F., Zhang Z., Fu X., Li W., Wang T., Liu H. Analysis of phospholipids by NACE with on-line ESI-MS. Electrophoresis. 2007;28:1418–1425. doi: 10.1002/elps.200600533. [DOI] [PubMed] [Google Scholar]
- 54.Cornett D.S., Mobley J.A., Dias E.C., Andersson M., Arteaga C.L., Sanders M.E., Caprioli R.M. A novel histology-directed strategy for MALDI-MS tissue profiling that improves throughput and cellular specificity in human breast cancer. Mol. Cell Proteom. 2006;5:1975–1983. doi: 10.1074/mcp.M600119-MCP200. [DOI] [PubMed] [Google Scholar]
- 55.Wu Z., Bagarolo G.I., Thoroe-Boveleth S., Jankowski J. “Lipidomics”: Mass spectrometric and chemometric analyses of lipids. Adv. Drug Deliv. Rev. 2020 doi: 10.1016/j.addr.2020.06.009. [DOI] [PubMed] [Google Scholar]
- 56.Bergers G., Hanahan D. Modes of resistance to anti-angiogenic therapy. Nat. Rev. Cancer. 2008;8:592–603. doi: 10.1038/nrc2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Crawford Y., Kasman I., Yu L., Zhong C., Wu X., Modrusan Z., Kaminker J., Ferrara N. PDGF-C mediates the angiogenic and tumorigenic properties of fibroblasts associated with tumors refractory to anti-VEGF treatment. Cancer Cell. 2009;15:21–34. doi: 10.1016/j.ccr.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 58.Cao Y., Arbiser J., D’Amato R.J., D’Amore P.A., Ingber D.E., Kerbel R., Klagsbrun M., Lim S., Moses M.A., Zetter B., et al. Forty-year journey of angiogenesis translational research. Sci. Transl. Med. 2011;3:114rv113. doi: 10.1126/scitranslmed.3003149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Iwamoto H., Abe M., Yang Y., Cui D., Seki T., Nakamura M., Hosaka K., Lim S., Wu J., He X., et al. Cancer Lipid Metabolism Confers Antiangiogenic Drug Resistance. Cell Metab. 2018;28:104–117.e105. doi: 10.1016/j.cmet.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 60.Jayashankar V., Edinger A.L. Macropinocytosis confers resistance to therapies targeting cancer anabolism. Nat. Commun. 2020;11:1121. doi: 10.1038/s41467-020-14928-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Recouvreux M.V., Commisso C. Macropinocytosis: A Metabolic Adaptation to Nutrient Stress in Cancer. Front. Endocrinol. (Lausanne) 2017;8:261. doi: 10.3389/fendo.2017.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Amyere M., Payrastre B., Krause U., Van Der Smissen P., Veithen A., Courtoy P.J. Constitutive macropinocytosis in oncogene-transformed fibroblasts depends on sequential permanent activation of phosphoinositide 3-kinase and phospholipase C. Mol. Biol. Cell. 2000;11:3453–3467. doi: 10.1091/mbc.11.10.3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tautu C., Verazin G., Prorok J.J., Alhadeff J.A. Improved procedure for determination of serum lipid-associated sialic acid: Application for early diagnosis of colorectal cancer. J. Natl. Cancer Inst. 1988;80:1333–1337. doi: 10.1093/jnci/80.16.1333. [DOI] [PubMed] [Google Scholar]
- 64.Zeleznik O.A., Clish C.B., Kraft P., Avila-Pacheco J., Eliassen A.H., Tworoger S.S. Circulating Lysophosphatidylcholines, Phosphatidylcholines, Ceramides, and Sphingomyelins and Ovarian Cancer Risk: A 23-Year Prospective Study. J. Natl. Cancer Inst. 2020;112:628–636. doi: 10.1093/jnci/djz195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qiu Y., Zhou B., Su M., Baxter S., Zheng X., Zhao X., Yen Y., Jia W. Mass spectrometry-based quantitative metabolomics revealed a distinct lipid profile in breast cancer patients. Int. J. Mol. Sci. 2013;14:8047–8061. doi: 10.3390/ijms14048047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim H., Min H.K., Kong G., Moon M.H. Quantitative analysis of phosphatidylcholines and phosphatidylethanolamines in urine of patients with breast cancer by nanoflow liquid chromatography/tandem mass spectrometry. Anal. Bioanal. Chem. 2009;393:1649–1656. doi: 10.1007/s00216-009-2621-3. [DOI] [PubMed] [Google Scholar]
- 67.Ide Y., Waki M., Hayasaka T., Nishio T., Morita Y., Tanaka H., Sasaki T., Koizumi K., Matsunuma R., Hosokawa Y., et al. Human breast cancer tissues contain abundant phosphatidylcholine(36ratio1) with high stearoyl-CoA desaturase-1 expression. PLoS ONE. 2013;8:e61204. doi: 10.1371/annotation/63c5359c-b1d2-44d8-944f-7bde0d6ec946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Iwano T., Yoshimura K., Inoue S., Odate T., Ogata K., Funatsu S., Tanihata H., Kondo T., Ichikawa D., Takeda S. Breast cancer diagnosis based on lipid profiling by probe electrospray ionization mass spectrometry. Br. J. Surg. 2020;107:632–635. doi: 10.1002/bjs.11613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jiang N., Zhang G., Pan L., Yan C., Zhang L., Weng Y., Wang W., Chen X., Yang G. Potential plasma lipid biomarkers in early-stage breast cancer. Biotechnol. Lett. 2017;39:1657–1666. doi: 10.1007/s10529-017-2417-z. [DOI] [PubMed] [Google Scholar]
- 70.Cifkova E., Holcapek M., Lisa M., Vrana D., Gatek J., Melichar B. Determination of lipidomic differences between human breast cancer and surrounding normal tissues using HILIC-HPLC/ESI-MS and multivariate data analysis. Anal. Bioanal. Chem. 2015;407:991–1002. doi: 10.1007/s00216-014-8272-z. [DOI] [PubMed] [Google Scholar]
- 71.Laisupasin P., Thompat W., Sukarayodhin S., Sornprom A., Sudjaroen Y. Comparison of Serum Lipid Profiles between Normal Controls and Breast Cancer Patients. J. Lab. Physicians. 2013;5:38–41. doi: 10.4103/0974-2727.115934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Franky Dhaval S., Shilin Nandubhai S., Pankaj Manubhai S., Patel H.R., Prabhudas Shankerbhai P. Significance of alterations in plasma lipid profile levels in breast cancer. Integr. Cancer Ther. 2008;7:33–41. doi: 10.1177/1534735407313883. [DOI] [PubMed] [Google Scholar]
- 73.Akalanka H.M.K., Ekanayake S., Samarasinghe K. Could Anthropometric and Lipid Parameters Reflect Susceptibility to Breast Cancer? Comparison of Newly Diagnosed Breast Cancer and Apparently Healthy Women. Asian Pac. J. Cancer Prev. 2018;19:2475–2480. doi: 10.22034/APJCP.2018.19.9.2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang L., Cui X., Zhang N., Li M., Bai Y., Han X., Shi Y., Liu H. Comprehensive lipid profiling of plasma in patients with benign breast tumor and breast cancer reveals novel biomarkers. Anal. Bioanal. Chem. 2015;407:5065–5077. doi: 10.1007/s00216-015-8484-x. [DOI] [PubMed] [Google Scholar]
- 75.Park J., Shin Y., Kim T.H., Kim D.H., Lee A. Plasma metabolites as possible biomarkers for diagnosis of breast cancer. PLoS ONE. 2019;14:e0225129. doi: 10.1371/journal.pone.0225129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brozek-Pluska B., Musial J., Kordek R., Bailo E., Dieing T., Abramczyk H. Raman spectroscopy and imaging: Applications in human breast cancer diagnosis. Analyst. 2012;137:3773–3780. doi: 10.1039/c2an16179f. [DOI] [PubMed] [Google Scholar]
- 77.Zhang Y., Song L., Liu N., He C., Li Z. Decreased serum levels of free fatty acids are associated with breast cancer. Clin. Chim. Acta. 2014;437:31–37. doi: 10.1016/j.cca.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 78.Lv W., Yang T. Identification of possible biomarkers for breast cancer from free fatty acid profiles determined by GC-MS and multivariate statistical analysis. Clin. Biochem. 2012;45:127–133. doi: 10.1016/j.clinbiochem.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 79.His M., Zelek L., Deschasaux M., Pouchieu C., Kesse-Guyot E., Hercberg S., Galan P., Latino-Martel P., Blacher J., Touvier M. Prospective associations between serum biomarkers of lipid metabolism and overall, breast and prostate cancer risk. Eur. J. Epidemiol. 2014;29:119–132. doi: 10.1007/s10654-014-9884-5. [DOI] [PubMed] [Google Scholar]
- 80.Yeo W., Mo F.K.F., Pang E., Suen J.J.S., Koh J., Loong H.H.F., Yip C.C.H., Ng R.Y.W., Yip C.H.W., Tang N.L.S., et al. Profiles of lipids, blood pressure and weight changes among premenopausal Chinese breast cancer patients after adjuvant chemotherapy. BMC Womens Health. 2017;17:55. doi: 10.1186/s12905-017-0409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hammad L.A., Wu G., Saleh M.M., Klouckova I., Dobrolecki L.E., Hickey R.J., Schnaper L., Novotny M.V., Mechref Y. Elevated levels of hydroxylated phosphocholine lipids in the blood serum of breast cancer patients. Rapid Commun. Mass Spectrom. 2009;23:863–876. doi: 10.1002/rcm.3947. [DOI] [PubMed] [Google Scholar]
- 82.Min H.K., Kong G., Moon M.H. Quantitative analysis of urinary phospholipids found in patients with breast cancer by nanoflow liquid chromatography-tandem mass spectrometry: II. Negative ion mode analysis of four phospholipid classes. Anal. Bioanal. Chem. 2010;396:1273–1280. doi: 10.1007/s00216-009-3292-9. [DOI] [PubMed] [Google Scholar]
- 83.Chatgilialoglu C., Ferreri C., Melchiorre M., Sansone A., Torreggiani A. Lipid geometrical isomerism: From chemistry to biology and diagnostics. Chem. Rev. 2014;114:255–284. doi: 10.1021/cr4002287. [DOI] [PubMed] [Google Scholar]
- 84.Kotronen A., Seppanen-Laakso T., Westerbacka J., Kiviluoto T., Arola J., Ruskeepaa A.L., Yki-Jarvinen H., Oresic M. Comparison of lipid and fatty acid composition of the liver, subcutaneous and intra-abdominal adipose tissue, and serum. Obesity (Silver Spring) 2010;18:937–944. doi: 10.1038/oby.2009.326. [DOI] [PubMed] [Google Scholar]
- 85.Ferreri C., Sansone A., Ferreri R., Amezaga J., Tueros I. Fatty Acids and Membrane Lipidomics in Oncology: A Cross-Road of Nutritional, Signaling and Metabolic Pathways. Metabolites. 2020;10:345. doi: 10.3390/metabo10090345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kang K.S., Wang P., Yamabe N., Fukui M., Jay T., Zhu B.T. Docosahexaenoic acid induces apoptosis in MCF-7 cells in vitro and in vivo via reactive oxygen species formation and caspase 8 activation. PLoS ONE. 2010;5:e10296. doi: 10.1371/journal.pone.0010296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cao W., Ma Z., Rasenick M.M., Yeh S., Yu J. N-3 poly-unsaturated fatty acids shift estrogen signaling to inhibit human breast cancer cell growth. PLoS ONE. 2012;7:e52838. doi: 10.1371/journal.pone.0052838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xiong A., Yu W., Tiwary R., Sanders B.G., Kline K. Distinct roles of different forms of vitamin E in DHA-induced apoptosis in triple-negative breast cancer cells. Mol. Nutr. Food Res. 2012;56:923–934. doi: 10.1002/mnfr.201200027. [DOI] [PubMed] [Google Scholar]
- 89.Sun-yong Hwang T.-H.K. 2 Hae-Hyeog Lee,2 Heung Yeol Kim,3 and Juhyun Seo4. Effect of Docosahexaenoic Acid (DHA) on Breast Cancer Cells. Kosin Med. J. 2015;30:103. doi: 10.7180/kmj.2015.30.2.103. [DOI] [Google Scholar]
- 90.Oresic M., Hanninen V.A., Vidal-Puig A. Lipidomics: A new window to biomedical frontiers. Trends Biotechnol. 2008;26:647–652. doi: 10.1016/j.tibtech.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 91.Hosokawa Y., Masaki N., Takei S., Horikawa M., Matsushita S., Sugiyama E., Ogura H., Shiiya N., Setou M. Recurrent triple-negative breast cancer (TNBC) tissues contain a higher amount of phosphatidylcholine (32:1) than non-recurrent TNBC tissues. PLoS ONE. 2017;12:e0183724. doi: 10.1371/journal.pone.0183724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bougnoux P., Hajjaji N., Maheo K., Couet C., Chevalier S. Fatty acids and breast cancer: Sensitization to treatments and prevention of metastatic re-growth. Prog. Lipid Res. 2010;49:76–86. doi: 10.1016/j.plipres.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 93.Meikle P.J., Barlow C.K., Mellett N.A., Mundra P.A., Bonham M.P., Larsen A., Cameron-Smith D., Sinclair A., Nestel P.J., Wong G. Postprandial Plasma Phospholipids in Men Are Influenced by the Source of Dietary Fat. J. Nutr. 2015;145:2012–2018. doi: 10.3945/jn.115.210104. [DOI] [PubMed] [Google Scholar]
- 94.Corbet C., Feron O. Emerging roles of lipid metabolism in cancer progression. Curr. Opin. Clin. Nutr. Metab. Care. 2017;20:254–260. doi: 10.1097/MCO.0000000000000381. [DOI] [PubMed] [Google Scholar]
- 95.Corbet C., Pinto A., Martherus R., de Jesus J.P.S., Polet F., Feron O. Acidosis Drives the Reprogramming of Fatty Acid Metabolism in Cancer Cells through Changes in Mitochondrial and Histone Acetylation. Cell Metab. 2016;24:311–323. doi: 10.1016/j.cmet.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 96.Furuta E., Pai S.K., Zhan R., Bandyopadhyay S., Watabe M., Mo Y.Y., Hirota S., Hosobe S., Tsukada T., Miura K., et al. Fatty acid synthase gene is up-regulated by hypoxia via activation of Akt and sterol regulatory element binding protein-1. Cancer Res. 2008;68:1003–1011. doi: 10.1158/0008-5472.CAN-07-2489. [DOI] [PubMed] [Google Scholar]
- 97.Lu S., Archer M.C. Sp1 coordinately regulates de novo lipogenesis and proliferation in cancer cells. Int. J. Cancer. 2010;126:416–425. doi: 10.1002/ijc.24761. [DOI] [PubMed] [Google Scholar]
- 98.Zeng Y., Ren K., Zhu X., Zheng Z., Yi G. Long Noncoding RNAs: Advances in Lipid Metabolism. Adv. Clin. Chem. 2018;87:1–36. doi: 10.1016/bs.acc.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 99.Shav-Tal Y., Zipori D. PSF and p54nrb/NonO-multi-functional nuclear proteins. FEBS Lett. 2002;531:109–114. doi: 10.1016/S0014-5793(02)03447-6. [DOI] [PubMed] [Google Scholar]
- 100.Pavao M., Huang Y.H., Hafer L.J., Moreland R.B., Traish A.M. Immunodetection of nmt55/p54nrb isoforms in human breast cancer. BMC Cancer. 2001;1:15. doi: 10.1186/1471-2407-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shao W., Espenshade P.J. Expanding roles for SREBP in metabolism. Cell Metab. 2012;16:414–419. doi: 10.1016/j.cmet.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhao X., Zong H., Abdulla A., Yang E.S., Wang Q., Ji J.Y., Pessin J.E., Das B.C., Yang F. Inhibition of SREBP transcriptional activity by a boron-containing compound improves lipid homeostasis in diet-induced obesity. Diabetes. 2014;63:2464–2473. doi: 10.2337/db13-0835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhu Z., Zhao X., Zhao L., Yang H., Liu L., Li J., Wu J., Yang F., Huang G., Liu J. p54(nrb)/NONO regulates lipid metabolism and breast cancer growth through SREBP-1A. Oncogene. 2016;35:1399–1410. doi: 10.1038/onc.2015.197. [DOI] [PubMed] [Google Scholar]
- 104.Kuhajda F.P. Fatty-acid synthase and human cancer: New perspectives on its role in tumor biology. Nutrition. 2000;16:202–208. doi: 10.1016/S0899-9007(99)00266-X. [DOI] [PubMed] [Google Scholar]
- 105.Innocenzi D., Alo P.L., Balzani A., Sebastiani V., Silipo V., La Torre G., Ricciardi G., Bosman C., Calvieri S. Fatty acid synthase expression in melanoma. J. Cutan. Pathol. 2003;30:23–28. doi: 10.1034/j.1600-0560.2003.300104.x. [DOI] [PubMed] [Google Scholar]
- 106.Kusakabe T., Nashimoto A., Honma K., Suzuki T. Fatty acid synthase is highly expressed in carcinoma, adenoma and in regenerative epithelium and intestinal metaplasia of the stomach. Histopathology. 2002;40:71–79. doi: 10.1046/j.1365-2559.2002.01289.x. [DOI] [PubMed] [Google Scholar]
- 107.Adorno-Cruz V., Hoffmann A.D., Liu X., Dashzeveg N.K., Taftaf R., Wray B., Keri R.A., Liu H. ITGA2 promotes expression of ACLY and CCND1 in enhancing breast cancer stemness and metastasis. Genes Dis. 2020 doi: 10.1016/j.gendis.2020.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Saikolappan S., Kumar B., Shishodia G., Koul S., Koul H.K. Reactive oxygen species and cancer: A complex interaction. Cancer Lett. 2019;452:132–143. doi: 10.1016/j.canlet.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 109.Aggarwal V., Tuli H.S., Varol A., Thakral F., Yerer M.B., Sak K., Varol M., Jain A., Khan M.A., Sethi G. Role of Reactive Oxygen Species in Cancer Progression: Molecular Mechanisms and Recent Advancements. Biomolecules. 2019;9:735. doi: 10.3390/biom9110735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liao Z., Chua D., Tan N.S. Reactive oxygen species: A volatile driver of field cancerization and metastasis. Mol. Cancer. 2019;18:65. doi: 10.1186/s12943-019-0961-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rosa D., Catala A. Fatty acid profiles and non enzymatic lipid peroxidation of microsomes and mitochondria from bovine liver, kidney, lung and heart. Arch. Physiol. Biochem. 1998;106:33–37. doi: 10.1076/apab.106.1.33.4398. [DOI] [PubMed] [Google Scholar]
- 112.Choudhary S., Zhang W., Zhou F., Campbell G.A., Chan L.L., Thompson E.B., Ansari N.H. Cellular lipid peroxidation end-products induce apoptosis in human lens epithelial cells. Free Radic. Biol. Med. 2002;32:360–369. doi: 10.1016/S0891-5849(01)00810-3. [DOI] [PubMed] [Google Scholar]
- 113.Agostinelli E., Seiler N. Non-irradiation-derived reactive oxygen species (ROS) and cancer: Therapeutic implications. Amino Acids. 2006;31:341–355. doi: 10.1007/s00726-005-0271-8. [DOI] [PubMed] [Google Scholar]
- 114.Wu W.S. The signaling mechanism of ROS in tumor progression. Cancer Metastasis Rev. 2006;25:695–705. doi: 10.1007/s10555-006-9037-8. [DOI] [PubMed] [Google Scholar]
- 115.Guicciardi M.E., Gores G.J. Apoptosis: A mechanism of acute and chronic liver injury. Gut. 2005;54:1024–1033. doi: 10.1136/gut.2004.053850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kitahara C.M., Berrington de Gonzalez A., Freedman N.D., Huxley R., Mok Y., Jee S.H., Samet J.M. Total cholesterol and cancer risk in a large prospective study in Korea. J. Clin. Oncol. 2011;29:1592–1598. doi: 10.1200/JCO.2010.31.5200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Emaus A., Veierod M.B., Tretli S., Finstad S.E., Selmer R., Furberg A.S., Bernstein L., Schlichting E., Thune I. Metabolic profile, physical activity, and mortality in breast cancer patients. Breast Cancer Res. Treat. 2010;121:651–660. doi: 10.1007/s10549-009-0603-y. [DOI] [PubMed] [Google Scholar]
- 118.Eliassen A.H., Colditz G.A., Rosner B., Willett W.C., Hankinson S.E. Serum lipids, lipid-lowering drugs, and the risk of breast cancer. Arch. Intern. Med. 2005;165:2264–2271. doi: 10.1001/archinte.165.19.2264. [DOI] [PubMed] [Google Scholar]
- 119.Nelson E.R., Wardell S.E., Jasper J.S., Park S., Suchindran S., Howe M.K., Carver N.J., Pillai R.V., Sullivan P.M., Sondhi V., et al. 27-Hydroxycholesterol links hypercholesterolemia and breast cancer pathophysiology. Science. 2013;342:1094–1098. doi: 10.1126/science.1241908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kimbung S., Chang C.Y., Bendahl P.O., Dubois L., Thompson J.W., McDonnell D.P., Borgquist S. Impact of 27-hydroxylase (CYP27A1) and 27-hydroxycholesterol in breast cancer. Endocr.-Relat. Cancer. 2017;24:339–349. doi: 10.1530/ERC-16-0533. [DOI] [PubMed] [Google Scholar]
- 121.Baek A.E., Yu Y.A., He S., Wardell S.E., Chang C.Y., Kwon S., Pillai R.V., McDowell H.B., Thompson J.W., Dubois L.G., et al. The cholesterol metabolite 27 hydroxycholesterol facilitates breast cancer metastasis through its actions on immune cells. Nat. Commun. 2017;8:864. doi: 10.1038/s41467-017-00910-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baek A.E., Nelson E.R. The Contribution of Cholesterol and Its Metabolites to the Pathophysiology of Breast Cancer. Horm. Cancer. 2016;7:219–228. doi: 10.1007/s12672-016-0262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chlebowski R.T., Anderson G.L., Gass M., Lane D.S., Aragaki A.K., Kuller L.H., Manson J.E., Stefanick M.L., Ockene J., Sarto G.E., et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304:1684–1692. doi: 10.1001/jama.2010.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fuhrman B.J., Schairer C., Gail M.H., Boyd-Morin J., Xu X., Sue L.Y., Buys S.S., Isaacs C., Keefer L.K., Veenstra T.D., et al. Estrogen metabolism and risk of breast cancer in postmenopausal women. J. Natl. Cancer Inst. 2012;104:326–339. doi: 10.1093/jnci/djr531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Li X., Tang H., Wang J., Xie X., Liu P., Kong Y., Ye F., Shuang Z., Xie Z., Xie X. The effect of preoperative serum triglycerides and high-density lipoprotein-cholesterol levels on the prognosis of breast cancer. Breast. 2017;32:1–6. doi: 10.1016/j.breast.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 126.Bahl M., Ennis M., Tannock I.F., Hux J.E., Pritchard K.I., Koo J., Goodwin P.J. Serum lipids and outcome of early-stage breast cancer: Results of a prospective cohort study. Breast Cancer Res. Treat. 2005;94:135–144. doi: 10.1007/s10549-005-6654-9. [DOI] [PubMed] [Google Scholar]
- 127.Ray G., Husain S.A. Role of lipids, lipoproteins and vitamins in women with breast cancer. Clin. Biochem. 2001;34:71–76. doi: 10.1016/S0009-9120(00)00200-9. [DOI] [PubMed] [Google Scholar]
- 128.Ni H., Liu H., Gao R. Serum Lipids and Breast Cancer Risk: A Meta-Analysis of Prospective Cohort Studies. PLoS ONE. 2015;10:e0142669. doi: 10.1371/journal.pone.0142669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Nowak C., Arnlov J. A Mendelian randomization study of the effects of blood lipids on breast cancer risk. Nat. Commun. 2018;9:3957. doi: 10.1038/s41467-018-06467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kang H.S., Lee S.C., Park Y.S., Jeon Y.E., Lee J.H., Jung S.Y., Park I.H., Jang S.H., Park H.M., Yoo C.W., et al. Protein and lipid MALDI profiles classify breast cancers according to the intrinsic subtype. BMC Cancer. 2011;11:465. doi: 10.1186/1471-2407-11-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mao X., He J., Li T., Lu Z., Sun J., Meng Y., Abliz Z., Chen J. Application of imaging mass spectrometry for the molecular diagnosis of human breast tumors. Sci. Rep. 2016;6:21043. doi: 10.1038/srep21043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Escande C., Chini C.C., Nin V., Dykhouse K.M., Novak C.M., Levine J., van Deursen J., Gores G.J., Chen J., Lou Z., et al. Deleted in breast cancer-1 regulates SIRT1 activity and contributes to high-fat diet-induced liver steatosis in mice. J. Clin. Investig. 2010;120:545–558. doi: 10.1172/JCI39319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hilakivi-Clarke L., Clarke R., Onojafe I., Raygada M., Cho E., Lippman M. A maternal diet high in n-6 polyunsaturated fats alters mammary gland development, puberty onset, and breast cancer risk among female rat offspring. Proc. Natl. Acad. Sci. USA. 1997;94:9372–9377. doi: 10.1073/pnas.94.17.9372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lupien L.E., Bloch K., Dehairs J., Traphagen N.A., Feng W.W., Davis W.L., Dennis T., Swinnen J.V., Wells W.A., Smits N.C., et al. Endocytosis of very low-density lipoproteins: An unexpected mechanism for lipid acquisition by breast cancer cells. J. Lipid Res. 2020;61:205–218. doi: 10.1194/jlr.RA119000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Feng S., Yao J., Chen Y., Geng P., Zhang H., Ma X., Zhao J., Yu X. Expression and Functional Role of Reprogramming-Related Long Noncoding RNA (lincRNA-ROR) in Glioma. J. Mol. Neurosci. 2015;56:623–630. doi: 10.1007/s12031-014-0488-z. [DOI] [PubMed] [Google Scholar]
- 136.Mercer T.R., Dinger M.E., Mattick J.S. Long non-coding RNAs: Insights into functions. Nat. Rev. Genet. 2009;10:155–159. doi: 10.1038/nrg2521. [DOI] [PubMed] [Google Scholar]
- 137.Panzitt K., Tschernatsch M.M., Guelly C., Moustafa T., Stradner M., Strohmaier H.M., Buck C.R., Denk H., Schroeder R., Trauner M., et al. Characterization of HULC, a novel gene with striking up-regulation in hepatocellular carcinoma, as noncoding RNA. Gastroenterology. 2007;132:330–342. doi: 10.1053/j.gastro.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 138.Seyed Hosseyni M., Gholamin A., Roohollah F., Sadeghizadeh M. Evaluation of Expression Levels of Linc-ROR and HULC Genes in Breast Cancer Cells (MCF7) Following Treatment with Nanocurcumin. J. Hum. Genet. Genom. 2020;3 doi: 10.5812/jhgg.100080. [DOI] [Google Scholar]
- 139.Hildebrandt M.A., Gu J., Lin J., Ye Y., Tan W., Tamboli P., Wood C.G., Wu X. Hsa-miR-9 methylation status is associated with cancer development and metastatic recurrence in patients with clear cell renal cell carcinoma. Oncogene. 2010;29:5724–5728. doi: 10.1038/onc.2010.305. [DOI] [PubMed] [Google Scholar]
- 140.Phillips C.M., Goumidi L., Bertrais S., Field M.R., Cupples L.A., Ordovas J.M., Defoort C., Lovegrove J.A., Drevon C.A., Gibney M.J., et al. Gene-nutrient interactions with dietary fat modulate the association between genetic variation of the ACSL1 gene and metabolic syndrome. J. Lipid Res. 2010;51:1793–1800. doi: 10.1194/jlr.M003046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ong K.T., Mashek M.T., Bu S.Y., Greenberg A.S., Mashek D.G. Adipose triglyceride lipase is a major hepatic lipase that regulates triacylglycerol turnover and fatty acid signaling and partitioning. Hepatology. 2011;53:116–126. doi: 10.1002/hep.24006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Mashek D.G., Bornfeldt K.E., Coleman R.A., Berger J., Bernlohr D.A., Black P., DiRusso C.C., Farber S.A., Guo W., Hashimoto N., et al. Revised nomenclature for the mammalian long-chain acyl-CoA synthetase gene family. J. Lipid Res. 2004;45:1958–1961. doi: 10.1194/jlr.E400002-JLR200. [DOI] [PubMed] [Google Scholar]
- 143.Wang Y., Cai X., Zhang S., Cui M., Liu F., Sun B., Zhang W., Zhang X., Ye L. HBXIP up-regulates ACSL1 through activating transcriptional factor Sp1 in breast cancer. Biochem. Biophys. Res. Commun. 2017;484:565–571. doi: 10.1016/j.bbrc.2017.01.126. [DOI] [PubMed] [Google Scholar]
- 144.Lu W., Cao F., Wang S., Sheng X., Ma J. LncRNAs: The Regulator of Glucose and Lipid Metabolism in Tumor Cells. Front. Oncol. 2019;9:1099. doi: 10.3389/fonc.2019.01099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lan X., Yan J., Ren J., Zhong B., Li J., Li Y., Liu L., Yi J., Sun Q., Yang X., et al. A novel long noncoding RNA Lnc-HC binds hnRNPA2B1 to regulate expressions of Cyp7a1 and Abca1 in hepatocytic cholesterol metabolism. Hepatology. 2016;64:58–72. doi: 10.1002/hep.28391. [DOI] [PubMed] [Google Scholar]
- 146.Ma J., Feng J., Zhou X. Long non-coding RNA HAGLROS regulates lipid metabolism reprogramming in intrahepatic cholangiocarcinoma via the mTOR signaling pathway. Exp. Mol. Pathol. 2020;115:104466. doi: 10.1016/j.yexmp.2020.104466. [DOI] [PubMed] [Google Scholar]
- 147.He W., Liang B., Wang C., Li S., Zhao Y., Huang Q., Liu Z., Yao Z., Wu Q., Liao W., et al. MSC-regulated lncRNA MACC1-AS1 promotes stemness and chemoresistance through fatty acid oxidation in gastric cancer. Oncogene. 2019;38:4637–4654. doi: 10.1038/s41388-019-0747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cui M., Xiao Z., Wang Y., Zheng M., Song T., Cai X., Sun B., Ye L., Zhang X. Long noncoding RNA HULC modulates abnormal lipid metabolism in hepatoma cells through an miR-9-mediated RXRA signaling pathway. Cancer Res. 2015;75:846–857. doi: 10.1158/0008-5472.CAN-14-1192. [DOI] [PubMed] [Google Scholar]
- 149.Shang C., Wang W., Liao Y., Chen Y., Liu T., Du Q., Huang J., Liang Y., Liu J., Zhao Y., et al. LNMICC Promotes Nodal Metastasis of Cervical Cancer by Reprogramming Fatty Acid Metabolism. Cancer Res. 2018;78:877–890. doi: 10.1158/0008-5472.CAN-17-2356. [DOI] [PubMed] [Google Scholar]
- 150.Sallam T., Jones M.C., Gilliland T., Zhang L., Wu X., Eskin A., Sandhu J., Casero D., Vallim T.Q., Hong C., et al. Feedback modulation of cholesterol metabolism by the lipid-responsive non-coding RNA LeXis. Nature. 2016;534:124–128. doi: 10.1038/nature17674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Li D., Cheng M., Niu Y., Chi X., Liu X., Fan J., Fan H., Chang Y., Yang W. Identification of a novel human long non-coding RNA that regulates hepatic lipid metabolism by inhibiting SREBP-1c. Int. J. Biol. Sci. 2017;13:349–357. doi: 10.7150/ijbs.16635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wu H., Liu B., Chen Z., Li G., Zhang Z. MSC-induced lncRNA HCP5 drove fatty acid oxidation through miR-3619-5p/AMPK/PGC1alpha/CEBPB axis to promote stemness and chemo-resistance of gastric cancer. Cell Death Dis. 2020;11:233. doi: 10.1038/s41419-020-2426-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Yan C., Chen J., Chen N. Long noncoding RNA MALAT1 promotes hepatic steatosis and insulin resistance by increasing nuclear SREBP-1c protein stability. Sci. Rep. 2016;6:22640. doi: 10.1038/srep22640. [DOI] [PMC free article] [PubMed] [Google Scholar]